Back to Journals » International Journal of General Medicine » Volume 16
The Paradoxical Association of Lipids with Survival and Walking Ability of Hip Fractures in Geriatric Patients After Surgery: A 1-Year Follow-Up Study
Authors Zhao Z, Fan W, Wang L, Chu Q
Received 16 April 2023
Accepted for publication 7 July 2023
Published 28 August 2023 Volume 2023:16 Pages 3907—3919
DOI https://doi.org/10.2147/IJGM.S417499
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Zhibang Zhao, Wenliang Fan, Liqiang Wang, Qingbo Chu
Emergency Trauma Center, Nanyang Second People’s Hospital, Nanyang, Henan, People’s Republic of China
Correspondence: Qingbo Chu, Emergency Trauma Center, Nanyang Second People’s Hospital, No. 66 East Jianshe Road, Nanyang, Henan, 473000, People’s Republic of China, Email [email protected]
Background: We aimed to explore the association between lipids and the survival and walking ability of hip fractures in geriatric patients after surgery.
Methods: Restricted cubic spline (RCS) was established to explore the nonlinear relationship between lipids and 1-year mortality of hip fractures, and the cut-off points were also determined by RCS. Then, the patients were divided into three groups: low, middle, and high levels of LDL-c. Then, the survival and walking ability of patients from different groups were compared, and the Cox regression and Logistics regression were used to identify the relationships between lipids and the survival and walking ability of hip fractures.
Results: The patients with middle levels of LDL-c had a significantly high survival probability than those with low or high levels of LDL-c (p < 0.001). The patients with low levels of LDL-c and with high levels of LDL-c may have a poor prognosis compared with patients with middle levels of LDL-c in 6-month mortality, 6-month free walking ability, 1-year mortality, and 1-year free walking ability (All p < 0.05).
Conclusion: Low and high levels of LDL-c may both relate to the poor survival and walking ability of hip fractures.
Keywords: hip fractures, LDL-c, lipid, dyslipidemia, prognosis
Introduction
Hip fracture has become a severe health problem for older patients in the increasingly severe aging society due to its high mortality and disability.1 In most cases, the direct causes of hip fractures were low-energy injuries, such as falls and slips.2 However, the decrease in bone density mass (BMD) was the root cause of hip fractures in older adults.3 Osteoporosis may not only affect the incidence of fragility fracture but also the prognosis of fractures. The poor bone regeneration ability in older patients with osteoporosis may have a much longer stay in bed even after surgery, and this may contribute to the development of complications and even death.4
Many factors may associate with bone metabolism and the rehabilitation of hip fractures, such as nutrition status, oxidative status, muscle mass and function, and so on.5–7 These factors may predict the prognosis of hip fractures by indicating the bone metabolism ability and the status of the whole body. Blood lipids, one of the most comprehensive and common clinical biochemistry tests, were proven to reflect bone metabolism status and were widely used to evaluate body function.8–10 However, the relationship between lipids and bone metabolism was still controversial: many studies indicate that the increase of triglyceride (TG) and low-density lipoprotein cholesterol (LDL-c) may be related to decreasing of BMD, and this interaction may be achieved via regulating the vitamin D.11 On the contrary, many researchers believed that lipids may relate to nutritional status and then be a potentially protective factor against the decrease in BMD.12 Many studies reported that the association of lipids and incident bone fractures may be nonlinear, while few studies discussed the relationship between lipids and the outcomes of hip fractures.13 Lipids play significant roles in bone metabolism, immune responses, oxidative stress, and regulation of inflammation, and all these physiological and pathological processes have been proven to relate to the prognosis of hip fractures.14–16 Therefore, we hypothesize that lipids may be implicated in the prognosis of elderly patients with hip fractures through the mechanisms described above. In this study, we aimed to explore the relationship between lipids and the survival and walking ability of hip fracture in geriatric patients and identify the potential nonlinear relationship between them by establishing the restricted cubic spline (RCS).
Materials and Methods
Study Design
Our study was a retrospective study performed in Emergency Trauma Center, Nanyang Second People’s Hospital. We declare that this study, as an observational study, was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Nanyang Second People’s Hospital (ID: 2013 Research Review No. 21). All the information about patient privacy was well protected, and informed consent was obtained from patients or their direct relatives. The inclusion criteria in this study were set as below: A. 50 years of age or older; B. Hip surgeries conducted for hip fractures. The exclusion criteria were set as below: A. Hip fractures caused by high energy; B. Pathological fractures. All patients with hip fractures in our department between January 2014 and January 2021 who met the criteria mentioned above were enrolled in our study.
Variables
Baseline features, including sex, body mass index (BMI), type of fracture, fracture history, smoking history, alcoholism history, polytrauma, surgical procedures, anesthesia, and time from injury to surgery, were collected and summarized. The fracture types were summarized as femoral neck fracture and intertrochanteric fracture, and the surgical procedures were divided into internal fixation and arthroplasty. The hospital examination including electrocardiogram, chest radiograph, triglycerides (TG), low-density lipoprotein cholesterol (LDL-c), high-density lipoprotein cholesterol (HDL-c), red blood count (RBC), hemoglobin (Hb), blood glucose (GLU), and albumin (ALB) was also collected. According to the Chinese Expert Consensus on Management of Dyslipidemia in the Elderly, patients with hypertriglyceridemia, with abnormal levels of LDL-c, and with abnormal levels of HDL-c were identified (Hypertriglyceridemia: TG ≥ 2.3 mmol/L; Abnormal levels of LDL-c: LDL-c ≥ 4.1 mmol/L; Abnormal levels of HDL-c: HDL-c < 1.0 mmol/L). To evaluate the comorbidities of patients, the Charlson comorbidity index (CCI) according to the patient’s comorbidities data.17
Follow-Up and Outcomes
All the patients enrolled in our study were followed up for 1 year via telephone. Death in this study was identified as all-cause death, and the free walking ability was identified as the ability that patients were able to complete daily activities without assistance. The primary outcomes were mortality rates at 3 months, 6 months, and 1 year after surgery, and the second outcomes were the free walking abilities at 3 months, 6 months, and 1 year.
Nonlinear Analyses
To explore the nonlinear relationships between lipids and the survival and walking ability of hip fractures, RCSs with four knots based on different Cox models and adjusted for different variables were established. Based on the RCS for the relation between LDL-c and 1-year mortality, the LDL-c cutoff points were decided according to the intersection of the 95% confidence interval (CI) and the Hazard Ratio (HR) = 1. Then, the patients were divided into three groups: patients with low levels of LDL-c, patients with middle levels of LDL-c, and patients with high levels of LDL-c.
Statistical Analyses
Continuous variables were expressed as mean ± standard deviation and analyzed by Independent Student’s T-tests for normally distributed data and by Wilcoxon rank-sum tests for non-normally distributed data. Categorical variables were presented as count (percent) and assessed using Chi-squared tests or Fisher’s exact test. Bonferroni Correction was applied for multiple tests to control the probability of committing a type I error at α = 0.05. Kaplan–Meier curves were established and the Log rank test was used to compare the survival between groups. Then, the univariate Cox models were established and the significant variables were included in Cox model 1 and Cox model 2. Cox model 1 was adjusted for only one type of lipid variable (LDL-c, HDL-c, or TG), while Cox model 2 was adjusted for all types of lipid variables (LDL-c, HDL-c, and TG). To reduce the bias caused by co-variables, logistics analyses were also performed to identify the predictive value of LDL-c for 6-month and 1-year mortality and walking ability. All analyses were conducted using R software version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria), and some analyses were visualized using GraphPad Prism version 8.0.1 (GraphPad Software, San Diego, CA). The null hypothesis was rejected for values of P < 0.05.
Results
Baseline Characteristics
Finally, a total of 688 individuals who underwent hip surgeries in our department between January 2014 and January 2021 and met the inclusion criteria were included in our study. The detailed inclusion and exclusion number of patients could be found in Figure 1. Then, the baseline features of patients with different 1-year survival statuses were compared and summarized in Table 1. Of the overall 688 individuals, 122 died within 1 year, and in the comparison of baseline characteristics between patients with survival time ≤1 year and patients with survival time >1 year, patients who survived more than 1 year had significantly lower ages (70.90 ± 10.18 vs 81.19 ± 6.54, p < 0.001), while there was no significant difference in LDL-c, HDL-c, and TG (Table 1).
 |
Table 1 Baseline Chart of Our Study |
 |
Figure 1 Flowchart of our study. Abbreviation: LDL-c, low-density lipoprotein cholesterol. |
Nonlinear Analyses
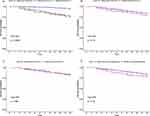
According to the results of the comparison of baseline characteristics, age as a co-variable was adjusted in RCS models. As shown in Figure 2, the nonlinear relationships between lipids (LDL-c, HDL-c, and TG) and 1-year mortality were calculated and visualized. There were significant U shapes between LDL-c and 1-year mortality in the unadjusted model (p < 0.001) and the model adjusted for age (p < 0.001), while there were no significant nonlinear relationships for HDL-c and TG.
To further explore the nonlinear relation between LDL-c and the prognosis of hip fractures, the patients were divided into three groups according to the results of RCS adjusted for age. The two cutoff points were decided: A: 3.49 mmol/L (95% CI: 0.998–0.999); B: 4.16 mmol/L (95% CI: 0.521–0.985). The three groups were identified as low levels of LDL-c: with levels of LDL-c < 3.49 mmol/L; middle levels of LDL-c: with levels of LDL-c between 3.49 mmol/L and 4.16 mmol/L; high levels of LDL-c: with levels of LDL-c > 4.16 mmol/L.
Outcomes
The survival and walking ability of patients were compared according to their lipid levels. The Kaplan–Meier curves showed that the patients with middle levels of LDL-c had a significantly high survival probability than those with low or high levels of LDL-c (p < 0.001, Figure 3A), while there was no significant difference between the patients with normal LDL-c and with abnormal LDL-c, as well as HDL-c and TG (all p > 0.05, Figure 3B-D). The relationships between lipids and mortality and walking ability are shown in Figure 4 and Table 2. The patients with middle levels of LDL-c may have a significantly better prognosis than those with low or high levels of LDL-c in both survival and free walking abilities (Figure 4A and B). Figure 4C and D showed the mortality and walking ability in patients with normal LDL-c and with abnormal LDL-c, and interestingly, the patients with abnormal LDL-c may have a significantly poor 3-month and 6-month free walking rate, while the other outcomes between them were not significantly different. The comparison of mortality and walking ability for patients grouped by levels of HDL-c and TG is shown in Table 2.
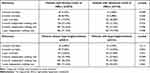 |
Table 2 Outcomes of Patients Grouped by Different Levels of HDL-c and TG |
Relationships Between Lipids and Prognosis
The direct comparison between survival and walking ability of patients in different groups may miss the impact of co-factors and lead to bias. Therefore, the Cox models and Logistics models were established to identify the relationships between lipids and prognosis. In both Cox models and Logistics models, Model 1 was adjusted by age, and all the lipid factors were included in the models independently, while Model 2 was adjusted by LDL-c, HDL-c, and hypertriglyceridemia together. To better explore the nonlinear relationships between LDL-c and prognosis, LDL-c was transformed into three types of variables: continuous LDL-c, normal or abnormal levels of LDL-c, and low, middle, or high levels of LDL-c. Each type of LDL-c was included in models independently. The results of Cox analyses are shown in Table 3, and in all models, compared to middle levels of LDL-c, the patients with low and high levels of LDL-c may have a significantly high risk of 1-year mortality. Moreover, in the Cox model 2, patients with hypertriglyceridemia may also face a higher risk of 1-year mortality than those without hypertriglyceridemia (Table 3).
 |
Table 3 Cox Models of 1-Year Mortality Adjusted for Different Factors |
The results of Logistics regression are summarized in Table 4. In both Model 1 and Model 2, the patients with low levels of LDL-c and with high levels of LDL-c may have a poor prognosis compared with patients with middle levels of LDL-c in 6-month mortality, 6-month free walking ability, 1-year mortality, and 1-year free walking ability (All p < 0.05). Moreover, the abnormal levels of LDL-c may also be a risk factor for 6-month free walking ability (Table 4).
 |
Table 4 Logistics Models of 6-Month and 1-Year Mortality and Free Walking Ability |
Discussion
Blood lipid is a general term for neutral fats (triglycerides) and lipids (phospholipids, glycolipids, sterols, steroids) in plasma, which are widely present in the human body and essential substances for the basic metabolism of cells.18 However, dyslipidemia, one of the most common chronic diseases featured by increased total cholesterol, increased LDL-c, increased TG, and decreased HDL-c in older adults, has been proven to relate to many diseases, especially to cardio-cerebral vascular diseases.19
In this study, we explored the relationships between blood lipids and the prognosis of hip fractures. Hip fracture is a common geriatric fracture with high mortality and disability, and in the clinic, many older patients may also face hip fracture and dyslipidemia.20 Therefore, identifying the associations between them may provide better sights and predictive tools in the treatment of hip fractures. To avoid the bias caused by co-factors, multi-variable regression analyses were performed and our study indicated that the LDL-c may relate to the survival and walking ability of hip fracture, while the other lipids, such as HDL-c and TG, were not significantly associated with the survival and walking ability of hip fractures. To calculate and visualize the relationships between LDL-c and the prognosis of hip fractures, the RCS was performed. RCS was one of the most common methods for analyzing nonlinear relationships and was widely used in many population studies.21,22 Interestingly, the relationships between LDL-c and the prognosis of hip fracture were fitted by RCS as a nonlinear U shape, which means both the low levels of LDL-c and high levels of LDL-c were the risk factors for geriatric hip fractures. Based on the results of RCS, the cutoff points of LDL-c were also generated, and the patients were divided into three groups according to the cutoff points for further tests. Compared with the two-groups-division by abnormal cutoff points, the three-groups-division may better indicate the U-shape associations. Moreover, to avoid the interaction between different lipids in the multivariable models, two kinds of models were established to better understand the association of lipids with the prognosis of hip fractures.
Consistent with our study, a population study that followed almost six thousand people showed the significantly nonlinear U-shaped relationships between LDL-c and hip fractures: the patients with the lowest and highest quintiles of LDL-c may have a significantly higher hip fracture risk, and similarly, the TG was not associated with the risk of hip fractures.23 Moreover, a retrospective study showed that patients with high levels of LDL may have a high risk of developing chronic non-malignant pain after the primary total hip arthroplasty for femoral neck fractures.24 Similarly, a study that reported the relationship between avascular necrosis of the femoral head and dyslipidemia for patients with low-energy femoral neck fractures after the treatment of cancellous screws showed that the patients with avascular necrosis of the femoral head tend to have a higher LDL-c and lower HDL-c than those without avascular necrosis of the femoral head.25 However, in the previous studies, the lipids were always studied and grouped by the abnormal values in the guidelines, which may ignore the nonlinear relationships between them. A more subdivided way of grouping may better reveal the association of lipids with outcomes of hip fractures.
Our study was an observational population study, and how to explain the findings was still a controversial question.26 Bone regeneration ability was one of the major factors for the rehabilitation of geriatric hip fractures: patients with strong bone regeneration abilities can get out of bed and exercise more quickly, reducing their bedridden time and consequently decreasing the risk of postoperative complications such as blood clots, pneumonia, and bedsores.27,28 As a result, they have a better prognosis. The LDL-c may relate to the mortality and walking ability of hip fractures by influencing bone metabolism. The negative relationship between LDL-c and BMD had been proved by a Mendelian randomization study.29 This conclusion was also reported in some population studies.30,31 However, some studies indicate that there might be no significant relationship between BMD and LDL-c.32 Many mechanisms might be used to understand the negative relationships between lipids and bone metabolism. In the most direct part, the increased cholesterol may inhibit the differentiation of osteoblasts and enhance the activity of osteoclasts, which may contribute to poor bone formation ability.33,34 Moreover, the LDL-c may promote arterial calcification, and their accumulation in the subendothelial space of skeletal bone arteries may inhibit bone formation.35 Dyslipidemia may also affect bone metabolism by increasing fat accumulation, reducing bone vascularization, and regulating oxidative stress which might cause a poor prognosis of fractures.36
These mechanisms linking the LDL-c and bone formation may explain the poor survival and walking ability of patients with high levels of LDL-c. However, low levels of LDL-c may also associate with poor prognosis of hip fractures by revealing the positive relation between LDL-c and all-cause mortality.37 A prospective study conducted in South Korea reported that patients with LDL-c < 1.81 mmol/L may face a higher risk of both all-cause mortality and cardiovascular disease mortality than those with LDL-c 2.59–3.34 mmol/L.38 Another cohort study showed similar results: for participants with a higher risk of coronary events, LDL-c <1.81 mmol/L is associated with increased all-cause mortality when compared with LDL-c ≥1.81 mmol/L.39 The association between LDL-c and all-cause mortality may also be in patients with hip fractures. LDL-c plays a significant role in the synthesis of cellular membranes and steroid hormones, and LDL-c is also one of the most sensitive predictors of malnutrition.40–42 These mechanisms may potentially explain why low levels of LDL-c were a protective factor for the prognosis of hip fracture.
Our study has several limitations. Firstly, due to the nature of the observational study, some data of patients and the follow-up may be lost, and this may cause bias in our study. Secondly, the results of the test of lipids were the first blood test when patients were admitted to our department, and the levels of lipids may be fluctuant, and the time of the test may affect the results of our study. Thirdly, as a retrospective study, our study was not able to establish the causality between lipids and the prognosis of fracture. Lastly, though most of the co-factors were included in our multivariable models, some of the variables, such as the use of lipid-lowering drugs, were not available, which might cause bias in our results.
In conclusion, the nonlinear U-shape relationships between LDL-c and the prognosis of hip fractures were observed in our study: the low and high levels of LDL-c may both relate to the poor survival and walking ability of hip fractures. Our findings may provide potential strategies for patients with hip fractures, especially those with dyslipidemia at the same time. The potential mechanism behind our findings was still controversial, and further experimental studies may be performed to provide more high-grade evidence.
Conclusion
Low and high levels of LDL-c may both relate to the poor survival and walking ability of hip fractures.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was a retrospective cohort study conducted in Emergency Trauma Center, Nanyang Second People’s Hospital. We declare that this study, as an observational study, was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Nanyang Second People’s Hospital (ID: 2013 Research Review No. 21). All the information about patient privacy was well protected. Informed consent was obtained from patients, and for those who had passed away during the follow-up, informed consent was obtained from their direct relatives. The use of informed consent obtained from direct relatives was approved by the Ethics Committee of Nanyang Second People’s Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Liu M, Yang C, Chu Q, Fu X, Zhang Y, Sun G. Superoxide Dismutase and Glutathione Reductase as Indicators of Oxidative Stress Levels May Relate to Geriatric Hip Fractures’ Survival and Walking Ability: a Propensity Score Matching Study. Clin Interv Aging. 2022;17:1081–1090. doi:10.2147/CIA.S370970
2. Kadri A, Binkley N, Daffner SD, Anderson PA. Fracture in Patients with Normal Bone Mineral Density: an Evaluation of the American Orthopaedic Association’s Own the Bone Registry. J Bone Joint Surg Am. 2023;105(2):128–136. doi:10.2106/JBJS.22.00012
3. Aude M, Jean-Jacques B, Laura I, et al. Fracture distribution in postmenopausal women: a FRISBEE sub-study. Arch Osteoporos. 2022;18(1):3. doi:10.1007/s11657-022-01191-w
4. McHugh MA, Wilson JL, Schaffer NE, et al. Preoperative Comorbidities Associated With Early Mortality in Hip Fracture Patients: a Multicenter Study. J Am Acad Orthop Surg. 2023;31(2):81–86. doi:10.5435/JAAOS-D-21-01055
5. Liu M, Ji S, Yang C, et al. Prealbumin as a nutrition status indicator may be associated with outcomes of geriatric Hip fractures: a propensity score matching and 1-year follow-up study. Aging Clin Exp Res. 2022;34(12):3005–3015. doi:10.1007/s40520-022-02243-4
6. Schroeder JD, Turner SP, Buck E. Hip Fractures: diagnosis and Management. Am Fam Physician. 2022;106(6):675–683.
7. Kobayashi H, Inoue T, Ogawa M, Abe T, Tanaka T, Kakiuchi M. Malnutrition diagnosed by the Global Leadership Initiative on Malnutrition criteria as a predictor of gait ability in patients with Hip fracture. Injury. 2022;53(10):3394–3400. doi:10.1016/j.injury.2022.08.004
8. Niu P, Li H, Liu D, Zhang YF, Liu Y, Liang C. Association Between HDL-C and Bone Mineral Density: an Cross-Sectional Analysis. Int J Gen Med. 2021;14:8863–8872. doi:10.2147/IJGM.S334972
9. Xie R, Huang X, Liu Q, Liu M. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011-2018. J Orthop Surg Res. 2022;17(1):92. doi:10.1186/s13018-022-02986-w
10. Sato Y, Hosonuma M, Sugawara D, et al. Cholesterol and fat in diet disrupt bone and tooth homeostasis in mice. Biomed Pharmacother. 2022;156:113940. doi:10.1016/j.biopha.2022.113940
11. Kim J, Ha J, Jeong C, et al. Bone mineral density and lipid profiles in older adults: a nationwide cross-sectional study. Osteoporos Int. 2023;34(1):119–128. doi:10.1007/s00198-022-06571-z
12. Ge B, Lu SQ, Lei SF. The obesity indices mediate the relationships of blood lipids and bone mineral density in Chinese elders. Mol Cell Probes. 2021;56:101705. doi:10.1016/j.mcp.2021.101705
13. Tohidi M, Barzegar N, Hasheminia M, Azizi F, Hadaegh F. Association of different lipid measures with incident bone fractures: Tehran lipid and glucose study. Postgrad Med. 2022;134(3):326–332. doi:10.1080/00325481.2022.2050980
14. Dwivedi A, Anggard EE, Carrier MJ. Oxidized LDL-mediated monocyte adhesion to endothelial cells does not involve NFkappaB. Biochem Biophys Res Commun. 2001;284(1):239–244. doi:10.1006/bbrc.2001.4955
15. Ghio M, Fabbi P, Contini P, et al. OxLDL- and HSP-60 antigen-specific CD8(+) T lymphocytes are detectable in the peripheral blood of patients suffering from coronary artery disease. Clin Exp Med. 2013;13(4):251–255. doi:10.1007/s10238-012-0205-6
16. Luegmayr E, Glantschnig H, Wesolowski GA, et al. Osteoclast formation, survival and morphology are highly dependent on exogenous cholesterol/lipoproteins. Cell Death Differ. 2004;11 Suppl 1:S108–18. doi:10.1038/sj.cdd.4401399
17. Asai N, Ohashi W, Sakanashi D, et al. Combination of Sequential Organ Failure Assessment (SOFA) score and Charlson Comorbidity Index (CCI) could predict the severity and prognosis of candidemia more accurately than the Acute Physiology, Age, Chronic Health Evaluation II (APACHE II) score. BMC Infect Dis. 2021;21(1):77. doi:10.1186/s12879-020-05719-8
18. Durstine JL, Grandjean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipid and lipoprotein adaptations to exercise: a quantitative analysis. Sports Med. 2001;31(15):1033–1062. doi:10.2165/00007256-200131150-00002
19. Noale M, Limongi F, Maggi S. Epidemiology of Cardiovascular Diseases in the Elderly. Adv Exp Med Biol. 2020;1216:29–38. doi:10.1007/978-3-030-33330-0_4
20. Choi HG, Lee YB, Rhyu SH, Kwon BC, Lee JK. Mortality and cause of death postoperatively in patients with a Hip fracture: a national cohort longitudinal follow-up study. Bone Joint J. 2018;100-B(4):436–442. doi:10.1302/0301-620X.100B4.BJJ-2017-0993.R2
21. Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944–953. doi:10.1016/S2213-8587(18)30288-2
22. Liu M, Chu Q, Yang C, et al. The paradoxical relation between serum uric acid and outcomes of Hip fracture in older patients after surgery: a 1-year follow-up study. Surgery. 2022;172(5):1576–1583. doi:10.1016/j.surg.2022.07.008
23. Barzilay JI, Buzkova P, Kuller LH, et al. The Association of Lipids and Lipoproteins with Hip Fracture Risk: the Cardiovascular Health Study. Am J Med. 2022;135(9):1101–1108 e1. doi:10.1016/j.amjmed.2022.05.024
24. Wang C, Xu B, Wang P, et al. Association of dyslipidemia with chronic non-malignant pain in elderly patients with femoral neck fractures treated by primary total Hip arthroplasty: a retrospective study. J Int Med Res. 2021;49(9):3000605211045224. doi:10.1177/03000605211045224
25. Zhang C, Zhu X, Pei G, et al. Dyslipidaemia for patients with low-energy femoral neck fractures after the treatment of cancellous screws: a retrospective study with a 3-year minimum follow-up. BMC Musculoskelet Disord. 2017;18(1):440. doi:10.1186/s12891-017-1804-x
26. Anagnostis P, Florentin M, Livadas S, Lambrinoudaki I, Goulis DG. Bone Health in Patients with Dyslipidemias: an Underestimated Aspect. Int J Mol Sci. 2022;23(3):56.
27. Yu Y, Wang Y, Hou X, Tian F. Recent advances in the identification of related factors and preventive strategies of Hip fracture. Front Public Health. 2023;11:1006527. doi:10.3389/fpubh.2023.1006527
28. Zuelzer DA, Weaver D, Zuelzer AP, Hessel EA. Current Strategies in Medical Management of the Geriatric Hip Fracture Patient. J Am Acad Orthop Surg. 2023;31(12):620–626. doi:10.5435/JAAOS-D-22-00815
29. Zheng J, Brion MJ, Kemp JP, et al. The Effect of Plasma Lipids and Lipid-Lowering Interventions on Bone Mineral Density: a Mendelian Randomization Study. J Bone Miner Res. 2020;35(7):1224–1235. doi:10.1002/jbmr.3989
30. Xiao F, Peng P, Gao S, Lin T, Fang W, He W. Inverse association between low-density lipoprotein cholesterol and bone mineral density in young- and middle-aged people: the NHANES 2011-2018. Front Med. 2022;9:929709. doi:10.3389/fmed.2022.929709
31. Xie R, Huang X, Zhang Y, Liu Q, Liu M. High Low-Density Lipoprotein Cholesterol Levels are Associated with Osteoporosis Among Adults 20-59 Years of Age. Int J Gen Med. 2022;15:2261–2270. doi:10.2147/IJGM.S353531
32. Jia L, Cheng M. Correlation analysis between risk factors, BMD and serum osteocalcin, CatheK, PINP, beta-crosslaps, TRAP, lipid metabolism and BMI in 128 patients with postmenopausal osteoporotic fractures. Eur Rev Med Pharmacol Sci. 2022;26(21):7955–7959. doi:10.26355/eurrev_202211_30147
33. Mandal CC. High Cholesterol Deteriorates Bone Health: new Insights into Molecular Mechanisms. Front Endocrinol (Lausanne). 2015;6:165. doi:10.3389/fendo.2015.00165
34. Pelton K, Krieder J, Joiner D, Freeman MR, Goldstein SA, Solomon KR. Hypercholesterolemia promotes an osteoporotic phenotype. Am J Pathol. 2012;181(3):928–936. doi:10.1016/j.ajpath.2012.05.034
35. Demer LL. Vascular calcification and osteoporosis: inflammatory responses to oxidized lipids. Int J Epidemiol. 2002;31(4):737–741. doi:10.1093/ije/31.4.737
36. Zeng X, Zhan K, Zhang L, et al. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J Orthop Surg Res. 2017;12(1):30. doi:10.1186/s13018-017-0532-0
37. Rong S, Li B, Chen L, et al. Association of Low-Density Lipoprotein Cholesterol Levels with More than 20-Year Risk of Cardiovascular and All-Cause Mortality in the General Population. J Am Heart Assoc. 2022;11(15):e023690. doi:10.1161/JAHA.121.023690
38. Sung KC, Huh JH, Ryu S, et al. Low Levels of Low-Density Lipoprotein Cholesterol and Mortality Outcomes in Non-Statin Users. J Clin Med. 2019;8(10). doi:10.3390/jcm8101571
39. Penson PE, Long DL, Howard G, et al. Associations between very low concentrations of low density lipoprotein cholesterol, high sensitivity C-reactive protein, and health outcomes in the Reasons for Geographical and Racial Differences in Stroke (REGARDS) study. Eur Heart J. 2018;39(40):3641–3653. doi:10.1093/eurheartj/ehy533
40. Cheng KH, Chu CS, Lin TH, Lee KT, Sheu SH, Lai WT. Lipid paradox in acute myocardial infarction-the association with 30-day in-hospital mortality. Crit Care Med. 2015;43(6):1255–1264. doi:10.1097/CCM.0000000000000946
41. Wang B, Guo Z, Li H, et al. Non-HDL cholesterol paradox and effect of underlying malnutrition in patients with coronary artery disease: a 41,182 cohort study. Clin Nutr. 2022;41(3):723–730. doi:10.1016/j.clnu.2022.01.027
42. Wang B, Liu J, Chen S, et al. Malnutrition affects cholesterol paradox in coronary artery disease: a 41,229 Chinese cohort study. Lipids Health Dis. 2021;20(1):36. doi:10.1186/s12944-021-01460-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.