Back to Journals » Clinical Ophthalmology » Volume 17
The Nictavi Tarsus Patch: A New Device for Achieving Temporary Eyelid Closure in Lagophthalmos
Authors Guo S, Borchert MS, Chang M, Nallasamy S, Reid MW , Zhang-Nunes S, Chang JR, Nguyen AM
Received 20 April 2023
Accepted for publication 23 June 2023
Published 3 July 2023 Volume 2023:17 Pages 1877—1884
DOI https://doi.org/10.2147/OPTH.S415766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Sarah Guo,1 Mark S Borchert,2,3 Melinda Chang,2,3 Sudha Nallasamy,1– 3 Mark W Reid,2,3 Sandy Zhang-Nunes,1,3 Jessica R Chang,1,3 Angeline M Nguyen1– 3
1Keck School of Medicine of University of Southern California, Los Angeles, CA, USA; 2The Vision Center at Children’s Hospital Los Angeles, Los Angeles, CA, USA; 3Roski Eye Institute at the University of Southern California, Department of Ophthalmology, Los Angeles, CA, USA
Correspondence: Angeline M Nguyen, Tel +1 323-361-2347, Fax +1 323-361-9812, Email [email protected]
Purpose: To evaluate the effectiveness, tolerability, and safety of the Nictavi Tarsus Patch™ (NTP) in inducing temporary eyelid closure for the management of lagophthalmos in the pediatric and young adult population.
Methods: We prospectively enrolled 20 patients < 21 years of age who had previously been managed for lagophthalmos to trial the NTP in clinic. Inter-palpebral fissure distance (IPFD) was compared before and after the placement of the NTP in the eyes-closed position using paired t-tests. Subjects then underwent a 3-night home trial with the NTP, and parent and subject perceptions of effectiveness, comfort, and complications with the patch were analyzed using Likert scale survey questions.
Results: Twenty subjects ages 2– 20 years with paralytic (65%) and non-paralytic (35%) lagophthalmos were enrolled. The NTP improved lagophthalmos from a mean pre-placement IPFD of 3.3 mm to post-placement IPFD of 0.4 mm (p < 0.01). Overall, 80% of subjects achieved successful eyelid closure defined as ≤ 1 mm of post-placement IPFD. When stratified by subtype, 100% of subjects with paralytic lagophthalmos achieved successful eyelid closure compared to 71% of subjects with non-paralytic lagophthalmos. On a scale of 1 (worst) to 5 (best), parents rated the NTP at 4.3± 0.7 for comfort while wearing, 4.3± 1.0 for comfort in removing, 4.6± 0.7 for ease of use, and 4.3± 0.9 for effectiveness. Ninety-three percent of parents reported preferring NTP to other eyelid closure methods previously tried and indicated that they would use it again.
Conclusion: The NTP is an effective, tolerable, and safe method of eyelid closure for children and young adults.
Keywords: lagophthalmos, eyelid closure, Nictavi Tarsus Patch, pediatric
Plain Language Summary
Lagophthalmos, or incomplete closure of the eyelids, can cause ocular surface dryness which results in significant discomfort and even vision loss. Lagophthalmos and its complications are difficult to manage, as current management methods are typically ineffective, uncomfortable, or involve invasive procedures for definitive treatment. Clinicians often recommend medical tape to induce eyelid closure, but this method is poorly tolerated. Our study evaluates the Nictavi Tarsus Patch™ (NTP), a new device designed to induce temporary eyelid closure with minimal discomfort. We enrolled 20 subjects < 21 years of age with lagophthalmos. Subjects underwent a study visit and 3-night trial of using NTP at home. During the study visit, severity of lagophthalmos was determined by measuring the distance (mm) between the upper and lower eyelids when the subject attempted to close their eyes. After the 3-night trial, parents of subjects (who were developmentally mature enough to answer questions) independently answered a series of survey questions over the phone.
In our study, we found that the NTP was safe and effective in inducing eyelid closure when in place and that the NTP was rated favorably in terms of comfort by our subjects and their parents. The majority of our subjects reported that they would want to use the device again and preferred it over previous methods tried. We anticipate that the NTP will address the current void for a tolerable, non-invasive management option for patients with lagophthalmos in both the outpatient and inpatient settings.
Introduction
Lagophthalmos, or the inability to completely close the eyelids, can result from a variety of paralytic and mechanical conditions in patients of all ages.1 The subsequent corneal exposure can lead to numerous sequelae, including severe ocular surface discomfort and vision loss from exposure keratopathy.
Therapy for lagophthalmos starts conservatively with frequent ocular surface lubrication. Depending on the severity of corneal disease, management may also require closure of the affected eyelid with external devices (such as medical tape) or definitive treatment with surgery (such as tarsorrhaphy or eyelid weight implantation).2,3
Despite the multitude of available management options, lagophthalmos still poses a therapeutic challenge, as available external devices are often ineffective or poorly tolerated.4 As a result, patients often fail conservative therapy with external devices and require surgical treatment, which is not only invasive but also potentially disfiguring and difficult to reverse.5,6
A more effective, comfortable, and non-surgical management option is needed to improve therapeutic outcomes. The Nictavi Tarsus Patch™ (NTP, Nictavi, Los Angeles, California) is a new, disposable, adhesive device that gently adheres to the upper eyelid. Given its semi-rigid material, when placed onto the upper eyelid in the eyes-closed position, the NTP immobilizes movement of the tarsus such that the upper eyelid remains closed even upon attempted upgaze. This study evaluates the effectiveness, tolerability, and safety of the NTP in lagophthalmos in children and young adults.
Methods
This prospective clinical trial (NCT05183282) adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Children’s Hospital Los Angeles. The study was HIPAA-compliant with protection of individually identifiable health information. Informed consent for participation in the trial was obtained from parents or legal guardians of subjects who were ≤17 years of age and was obtained directly from subjects who were ≥18 years of age. Subjects 7 to 17 years of age were asked to provide their assent to be included in the study. Photo consent for figures was also obtained and is archived at Children’s Hospital Los Angeles. The authors do not intend to share individual deidentified participant data or other study-related documents.
Study Population
Subjects were recruited from The Vision Center of Children’s Hospital Los Angeles between January 2018 and July 2022 who were identified from a list of patients coded as having an ICD-10 diagnosis of lagophthalmos (H02.2), exposure keratopathy (H16.21), and/or facial palsy (G51.0). Subjects were eligible if they were <21 years of age, had a diagnosis of lagophthalmos and had previously been recommended an eyelid closure method such as using medical tape, Steri-strips™, eye patches, temporary tarsorrhaphy, or any other temporary eyelid closure method. Subjects under the age of 18 were eligible for the study if their accompanying parent was 18 years of age or older. Subjects were excluded if they had an active corneal abrasion or ulcer, active use of a bandage contact lens, active dermatitis affecting the eyelids, an allergy to adhesive, inability to tolerate the NTP in clinic, or had an inability for complete mechanical closure of the eyelid by any means due to missing eyelid lamella.
Study Visit
The eye selected for study was the one with lagophthalmos (if unilateral) or, in bilateral cases, the one with more severe lagophthalmos. At the study visit, exophthalmometry was measured with a Hertel exophthalmometer. Lagophthalmos was measured as the pre-placement interpalpebral fissure distance (IPFD) in millimeters using a ruler held near the subject’s study eye in the relaxed eyes-closed position while subjects were seated upright with a chin up position to ensure adequate visualization of the eyelid margins. The NTP was then placed on the study eye by securing the adhesive side of the patch directly onto the upper eyelid so that its inferior edge was adjacent to the eyelid margin (Figure 1). Residual lagophthalmos was measured as the post-placement IPFD with the NTP in place. For subjects who were unable to follow commands to close their eyes, lagophthalmos was estimated during blinking or was deemed unmeasurable, and residual lagophthalmos was measured with the subjects’ eyes in primary gaze.
 |
Figure 1 Proper placement of the NTP is demonstrated on the subject’s left upper eyelid, with the inferior border of the patch adjacent to the upper eyelid margin and above the eyelashes. |
At-Home Trial Period and Survey
Parents and subjects >18 years of age were shown how to properly place the NTP and were given samples to trial for 3 nights on the study eye at home while asleep. Parents and subjects were instructed to continue using all routine ophthalmic ointment or gel into the lower eyelid fornix once the NTP was in place.
After completing the 3-night trial, parents of subjects were contacted by a research assistant to complete a phone survey consisting of 12 questions assessing their experience with the patch, including comfort, ease of use, and preference compared to other methods of eyelid closure they had previously tried (Supplemental Table 1). Subjects under 18 years of age who were developmentally mature enough to answer survey questions were separately asked a set of seven corresponding age-appropriate questions. Subjects ≥18 years of age who applied their own NTP for the 3-night-trial were administered the parent survey. A commentary section was available for further elaboration on both parent and child surveys.
Statistical Methods and Programming
For our power analysis, we estimated that there would be on average of 2 mm of lagophthalmos before placing the patch and 1 mm after placing the patch. Thus, with a standard deviation of 1 mm, an alpha of 5%, and a beta of 20%, the sample size we predicted would be needed was 10.
Descriptive statistics were used to characterize the study population’s demographic information (age, sex, race) and clinical characteristics (exophthalmometry and classification of lagophthalmos).
Wilcoxon signed-rank tests were used to determine whether there was a statistically significant change in IPFD before and after placing the NTP by lagophthalmos subtype (paralytic versus non-paralytic). Linear regression models with robust standard errors were also used to evaluate factors predictive of post-placement IPFD. These models were adjusted for age, sex, pre-placement IPFD, exophthalmometry, and lagophthalmos subtype. Next, the proportion of subjects who achieved successful eyelid closure was determined for each lagophthalmos subtype. Successful eyelid closure was defined as achieving complete eyelid closure (0 mm residual lagophthalmos) or near-complete eyelid closure (≤1 mm residual lagophthalmos) in the eyes-closed position with the NTP in place. Logistic regression models were attempted to determine factors predictive of having a successful eyelid closure; however, these models did not converge on a solution due to too few subjects having unsuccessful eyelid closure.
Subjective responses from parents and subjects were assessed for agreement using Cohen’s weighted kappa statistic. Linear regression models with robust standard errors were then used to determine factors predictive of parents responding that they would use the NTP again and whether they prefer to use the NTP over other methods previously used. These models were adjusted for objective successful eyelid closure, ratings of comfort, ease of use, and subjective ratings of effectiveness (answers to questions P4-P7, Supplemental Table 1).
All p-values less than 0.05 were considered statistically significant, and all p-values less than 0.10 were considered marginally significant. Analyses were performed using Stata/SE software version 14.2 (Stata Corp., College Station, TX).
Results
Study Population
Twenty subjects ages 2 to 20 years (median = 9 years, IQR = 7 years) were enrolled in this study (Table 1). Thirty-five percent were female, and 55% were Hispanic/Latinx. A variety of conditions were responsible for lagophthalmos and were categorized as paralytic (65%) or non-paralytic (35%) subtypes. Exophthalmometry measurements showed a median of 16mm (IQR = 15–19) in the study eye. Paralytic lagophthalmos was most commonly secondary to facial nerve palsy, which was isolated or part of a syndrome; less common causes of paralytic lagophthalmos included Cap myopathy, Krabbe’s disease, and Stuve-Wiedemann syndrome. Non-paralytic lagophthalmos was caused by variety of conditions, including post-surgical cicatricial changes, proptosis, and idiopathic etiologies (Table 2). Lagophthalmos was characterized as idiopathic if the limitation in eyelid closure was suspected to be due to nocturnal lagophthalmos or an unexplained mechanical cause, such as shortened eyelid lamellae, that was not associated with the subject’s syndrome.
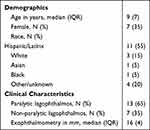 |
Table 1 Characteristics of Study Population |
 |
Table 2 Interpalpebral Fissure Distance with and without Nictavi Tarsus Patch ™ |
Subjects reported previously attempting management of their lagophthalmos with medical tape (65%), Steri-strips (™) (15%), patches (25%), moisture chambers (5%), and lateral tarsorrhaphy (10%). Thirty percent had attempted multiple modes of therapy.
Objective Measures of Eyelid Closure
Lagophthalmos improved from a mean pre-placement IPFD of 3.3 mm to a mean post-placement IPFD of 0.4 mm in subjects overall (P = 0.0009) (Table 3). When stratified by subtype, those with paralytic lagophthalmos improved from a mean pre-placement IPFD of 3.1 mm to a mean post-placement IPFD of 0.1 mm (P = 0.005). Subjects with non-paralytic lagophthalmos improved from a mean pre-placement IPFD of 3.6 mm to a mean post-placement IPFD of 1.2 mm, although this difference was only marginally significant (P = 0.09).
 |
Table 3 Mean Interpalpebral Fissure Distance with and without the Nictavi Tarsus Patch™ by Lagophthalmos Subtype |
Sixteen of the 20 subjects (80%) achieved successful eyelid closure with the NTP, defined as ≤1mm of post-placement IPFD. When stratified by subtype, 100% of subjects with paralytic lagophthalmos achieved successful eyelid closure compared to 71% of subjects with non-paralytic lagophthalmos.
In linear regression analyses adjusted for age, sex, pre-placement IPFD, exophthalmometry, and lagophthalmos subtype, having a paralytic subtype was associated with 1.65 mm less residual lagophthalmos compared to non-paralytic cases (P = 0.007), and every 1 mm increase in exophthalmometry measurement was associated with 0.21 mm less residual lagophthalmos (P = 0.005).
Parent and Child Survey Results
A majority of parents were reached by phone for the survey (n = 15), and 5 subjects were able to respond to the child survey. All subjects whose parents were surveyed completed the 3-night trial of NTP except for 1 who removed the patch himself one night and 2 other subjects who had their patches removed prematurely one night due to the subjects indicating discomfort.
On a scale of 1 (worst) to 5 (best), parents rated the NTP an average of 4.3±0.7 for comfort while wearing, 4.3±1.0 for comfort in removing, 4.6±0.7 for ease of use, and 4.3±0.9 for effectiveness. Of the 5 subjects who were able to answer survey questions (ages 10 to 20 years), they rated the NTP an average of 4.4±1.3 for comfort while wearing and 3.8±1.3 for comfort when removing. There was no significant difference between the responses of parents whose child was able to participate in the survey compared to those whose child was unable to participate. A majority of parents (93%) and subjects (80%) preferred the NTP over previous methods of eyelid closure with 93% of parents and 60% of subjects reporting willingness to use the NTP again.
In linear regression models adjusting for parents’ subjective responses to questions P4-P7 (Supplemental Table 1) and whether the subject achieved successful eyelid closure, parents were marginally more likely to report preference for using the patch again if they noted greater ease of use of the NTP (P = 0.08).
Additional comments about the NTP included that it was “painless”, “not sticky”, and that it “allowed [them] to sleep longer”.
Parent and Child Survey Response Agreement
For families in which both the parent and child participated in their respective surveys (n = 5), parent responses were largely representative of subject experiences, though interrater agreement varied by survey question. There was substantial agreement (90%, k = 0.62) regarding comfort wearing the NTP between parents and subjects, with 87% of parents and 80% of subjects rating it a 4 or 5. However, there was slightly less agreement (67%, k = 0.14) about comfort in removing the NTP, with 80% of parents and 60% of subjects rating the NTP a 4 or 5. Parents and subjects substantially agreed (90%, k = 0.62) on their preference to use the NTP over other methods and had moderate agreement (80%, k = 0.38) about using the device again.
Safety
One subject noted redness of the eye, and another subject complained of watery eyes during the trial. There were no reports of skin irritation.
Discussion
This study is the first to evaluate the use of the NTP for improving eyelid closure in patients with lagophthalmos. In our pediatric and young adult population, wearing the NTP resulted in complete or near-complete eyelid closure in 100% of subjects with paralytic lagophthalmos and 71% of subjects with non-paralytic lagophthalmos. After a 3-night home trial, parents and subjects rated the NTP highly in subjective effectiveness, comfort in use and removal, and ease of use. In addition, they reported preferring the NTP over previous methods tried and would use the NTP again.
It is generally accepted that the prevention of exposure keratopathy from lagophthalmos involves the combination of lubrication and coverage of the ocular surface through facilitating eyelid closure.7,8 Medical tape and Steri-strips™ are likely the most commonly recommended methods for non-invasive temporary eyelid closure because they are readily available in the clinic setting, but the Eyelocc™ and Sharn EyeGard® are commercially available devices designed for this purpose as well. There are no studies to our knowledge formally evaluating these devices for their effectiveness in improving eyelid closure or their tolerability.
In our experience, existing devices for eyelid closure are poorly tolerated by patients due to the discomfort of having adhesive on a large area of periorbital skin and eyelashes, thus resulting in poor treatment compliance. In our subjects who have all tried at least one device for eyelid closure (with 30% trying multiple methods of eyelid closure), the NTP was rated by parents and subjects as being comfortable to wear, comfortable to remove, and easy to use. As the NTP is designed for placement only on the upper eyelid, its sparing of the surrounding periorbita and eyelashes may allow it to be more comfortable than other devices. Additionally, its design allows for topical ocular medications to be instilled in the inferior fornix without having to remove and replace the patch as would be necessary with previous devices which cover both the upper and lower eyelid. Unlike other devices that require instillation of medications prior to placement of the device because they cover both the upper and lower eyelid simultaneously, the NTP can be placed on the eyelid while the skin is still dry for good adherence of the device to the skin. Finally, the NTP’s silicon-based adhesive,9 as opposed to acrylate as found in most medical tapes, allows for longer effective wear-time with minimal skin irritation as evidenced by the few adverse effects in our study.
The Stamler Lid Splint (SLS)10 and Temporary Eyelid Closure Applique (TLC)11 are two additional methods previously described for temporary eyelid closure which also spare the eyelashes in their design. The SLS comprises an oval piece of firm plastic that is coated on one side with stoma adhesive, while the TLC applique is made of weighted and adhesive ostomy material cut into a half circle to facilitate eyelid closure. Unlike the NTP, these methods were reported in previous studies to induce continuous eyelid closure over several days and thus may be more appropriate for treating temporary facial palsy or acute corneal epithelial disease rather than routine nightly use, such as in cases of chronic lagophthalmos. Additionally, there may be challenges to obtaining these devices, as there is no means for obtaining the SLS that we could identify through our search online, and the ostomy material for the TLC is not readily available in the ophthalmology clinic.
External eyelid weights of different sizes made of gold12 or tantalum13 are also available for placement on the upper eyelid to improve eyelid closure. While these devices have been shown to improve ocular comfort, the degree of eyelid closure achieved has not been reported, and their utility for nocturnal use has not been described.
We identified that the NTP was associated with greater success in eyelid closure in paralytic lagophthalmos than non-paralytic lagophthalmos. This relationship was expected, as anatomical abnormalities in non-paralytic lagophthalmos, such as post-surgical cicatricial eyelid changes, congenital or acquired insufficiency of eyelid lamellae, or proptosis might inhibit the upper eyelid from fully covering the ocular surface even with the placement of additional force. We interestingly found that greater proptosis was a predictor of greater success in eyelid closure, although the magnitude of this association was small. This counterintuitive finding in our study may be due to our small sample size resulting in outliers influencing this result. Studying a larger sample of patients would help to clarify this finding.
We demonstrated that parents and subjects were in general agreement in their survey responses about their subjective experience with the NTP. This suggests that parents who assisted their child in applying the device were largely aware of their child’s experience. However, given our small sample of paired parent and subject surveys, future studies would be needed to conclude if parent responses can be considered as a reliable substitute for those children who are unable to respond to survey questions.
Limitations of our study include the relatively small sample size, short study period, and response rate to our survey. Although there were no short-term adverse events, longer-term follow-up may better evaluate whether prolonged use, or use by those with more sensitive skin, may produce irritation. Additionally, variability in real-world use may be present when parents place the patch on their children or if patients place the patch on themselves. Parents subjectively reported that the patch was successful in closing their child’s eyelids during the trial, but there may be changes in the effectiveness of the NTP after sustained wear throughout the night. There may also be difficulty with achieving routine nightly use in younger children who have variable cooperativeness. Finally, we measured successful eyelid closure as a proxy for reducing exposure keratopathy, but we did not directly measure corneal health.
Conclusion
The NTP is a non-invasive management option for lagophthalmos that is effective, comfortable, and safe in children and young adults. Patients with paralytic lagophthalmos may have greater success in achieving complete eyelid closure than those with non-paralytic lagophthalmos, although both groups studied experienced an overall improvement in eyelid closure. While our cohort was limited primarily to children and young adults in the outpatient setting, we believe our results would be generalizable to patients of all ages and to hospital-based settings.
Acknowledgments
The authors thank Brianne Brown (clinical research coordinator) for her essential role in enrolling patients and Dr. Anthony Aldave for his advice on study design.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Correia Pereira MV, Firmato Glória AL. Lagophthalmos. Semin Ophthalmol. 2010;25(3):72–78. doi:10.3109/08820538.2010.488578
2. Wolkow N, Chodosh J, Freitag SK. Innovations in treatment of lagophthalmos and exposure keratopathy. Int Ophthalmol Clin. 2017;57(4):85–103. doi:10.1097/IIO.0000000000000185
3. Baum J. The advantages of partial patching or tarsorrhaphy over complete eyelid closure. Am J Ophthalmol. 1987;103(3):339–340. doi:10.1016/S0002-9394(21)00249-X
4. Latkany R, Lock B, Speaker M. Nocturnal lagophthalmos: an overview and classification. Ocul Surf. 2006;4(1):44–53. doi:10.1016/S1542-0124(12)70263-X
5. Howitt DA, Goldstein JH. Physiologic Lagophthalmos. Am J Ophthalmol. 1969;68(2):355. doi:10.1016/0002-9394(69)94086-0
6. Mancini R, Taban M, Lowinger A, et al. Use of Hyaluronic Acid Gel in the Management of Paralytic Lagophthalmos: the Hyaluronic Acid Gel “Gold Weight. Ophthal Plast Reconstr Surg. 2009;25(1):23–26. doi:10.1097/IOP.0b013e318192568d
7. Fu L, Patel BC. Lagophthalmos. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK560661/.
8. Gervasio KA, Godfrey KJ, Marlow ED, Lee MN, Lelli GJ. Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) Versus Standard of Care for Postsurgical Lagophthalmos and Exposure Keratopathy: trends in Visual Outcomes. Ophthal Plast Reconstr Surg. 2019;35(3):281–285. doi:10.1097/IOP.0000000000001233
9. Zeng LA, Lie SA, Chong SY. Comparison of medical adhesive tapes in patients at risk of facial skin trauma under anesthesia. Anesthesiol Res Pract. 2016;2016:1–6. doi:10.1155/2016/4878246
10. Mulhern MG, Rootman DS. The stamler lid splint: a new short-term technique for achieving therapeutic ptosis. Cornea. 2002;21(3):260–264. doi:10.1097/00003226-200204000-00005
11. Robinson C. Temporary eyelid closure appliqué. Arch Ophthalmol. 2006;124(4):546. doi:10.1001/archopht.124.4.546
12. Seiff SR, Boerner M, Carter SR. Treatment of facial palsies with external eyelid weights. Am J Ophthalmol. 1995;120(5):652–657. doi:10.1016/S0002-9394(14)72212-3
13. Shepler TR, Seiff SR. Use of isobutyl cyanoacrylate tissue adhesive to stabilize external eyelid weights in temporary treatment of facial palsies. Ophthal Plast Reconstr Surg. 2001;17(3):169–173. doi:10.1097/00002341-200105000-00004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
