Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
The Morbidity and Associated Factors of Depression in Caregivers of Patients with Depressive Disorder
Authors Lee Y, Lin PY , Huang YC , Chiu NM, Hung CF, Wang LJ
Received 5 April 2023
Accepted for publication 10 August 2023
Published 24 August 2023 Volume 2023:19 Pages 1853—1864
DOI https://doi.org/10.2147/NDT.S415881
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Yu Lee,1 Pao-Yen Lin,1 Yu-Chi Huang,1 Nien-Mu Chiu,1 Chi-Fa Hung,1 Liang-Jen Wang2
1Department of Psychiatry, Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Kaohsiung, Taiwan; 2Department of Child and Adolescent Psychiatry, Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Kaohsiung, Taiwan
Correspondence: Liang-Jen Wang, Department of Child and Adolescent Psychiatry, Kaohsiung Chang Gung Memorial, Hospital, No. 123, Ta-Pei Road, Kaohsiung City, Taiwan, Tel +886-7-7317123 ext. 8753, Fax +886-7-7326817, Email [email protected]
Objective: Depressive disorder significantly impacts patients’ daily living activities and quality of life. Caregivers of patients with depression may also suffer from psychological distress related to the chronic burden of caring for the patient’s mood changes. The purpose of this study was to evaluate the morbidity and associated factors of depression in caregivers of patients with depressive disorder.
Methods: In this study, we used a cross-sectional design with consecutive sampling. Study subjects were recruited from the psychiatric outpatient clinic of a medical center from August 2021 to June 2022. Caregivers of depressive disorder patients were enrolled and assessed using the Mini International Neuropsychiatric Interview, Hospital Anxiety and Depression Scale (HADS), Suicide Assessment Scale (SAS), Stigma Scale of the Explanatory Model Interview Catalogue (EMIC), and Family APGAR Index.
Results: Of the 120 caregivers that completed the study, 59.2% (n=71) were females. The most common psychiatric diagnosis was depressive disorders (25.8%), followed by anxiety disorders (17.5%) and insomnia disorder (15.8%); 54.2% of the caregivers had a psychiatric diagnosis. Using logistic regression analysis, we found that anxiolytics/hypnotics use (OR=5.58; 95% CI, 1.84– 16.96; p< 0.01), higher suicide risk (SAS) (OR=1.10; 95% CI, 1.05– 1.16; p< 0.001), and lower family support (APGAR scores) (OR=0.82; 95% CI, 0.71– 0.94; p< 0.01) were three significant associated factors.
Conclusion: Depression was the most prevalent psychiatric diagnosis in caregivers of patients with depressive disorder. Early psychiatric diagnosis for caregivers of patients with depression is crucial to offering suitable support and treatment and may improve caregivers’ quality of life.
Keywords: depression, morbidity, associated factor, caregiver
Introduction
Depressive disorder is a prevalent and seriously disabling public health problem worldwide. As of 2020, it has become the second most common debilitating disease, following only cardiovascular disease.1 Depressive disorder significantly impacts patients’ daily living activities, quality of life, cognitive function, and work productivity, and more than 13% of patients with depression attempt suicide during their worst episode.2–4
Lim et al5 studied one million participants from 30 countries from 1994 to 2014 by meta-analysis and found that the aggregate point prevalence, one-year, and lifetime prevalence of depression were 12.9%, 7.2%, and 10.8%, respectively. In another study from the US, the authors examined 89,037 people from 18 countries and found that the average lifetime and 12-month prevalence estimates of major depression were 11.1% and 5.9% in low- to middle-income countries and 14.6% and 5.5% in high-income countries.6 Based on the National Health and Nutrition Examination Survey, during 2013–2016, 8.1% of American adults had depression in a given two-week period. From 2007 to 2016, the morbidity of American adults with depression did not change significantly over time.7 Based on the aforementioned studies, the point prevalence of depression is quite high, ranging from 8% to 12%, and has shown a stable trend in recent decades.
Caregivers of patients with any disease may suffer from psychological distress or depressive disorders related to the chronic burden of caring for the patient’s physical condition or mood changes.8 Prior studies of depression in caregivers of patients primarily focused on patients with other physical diseases, eg, dementia and cancer.9,10 The purpose of these two studies was to investigate the relationship amongst caregiver burden, family functioning, and depression severity.9,10 Few studies have been done on caregiver depression in patients with depressive disorder. Marguerite et al11 performed a study to explore the influence of emotional intelligence (EI) and coping strategies on anxious and depressive symptoms in 79 MDD patients and their caregivers. The results demonstrated that coping strategies exhibited evidence of the actor and partner effect. However, this study did not examine the prevalence of depression in caregivers of depressive patients using the Beck Depression Inventory, a tool for detecting depression severity.11 Based on the above literatures review, we determined that studies on the morbidity of depression in caregivers of patients with depression was rare. Therefore, more studies on whether depression of caregivers in various clinical conditions (physical diseases vs depressive disorder) differ are warranted.
Previous research has indicated that caregiving in Taiwan is influenced by various factors such as culture, sociocultural aspects, religion, and gender. For instance, Wu et al (2016) examined the caregiver’s perspective and investigated the connections between attributions of schizophrenia, stigmatization, and caregiving experiences.12 Their findings revealed that biological attributions were positively associated with perceived family collaboration, while environmental attributions were linked to perceived informational support. Moreover, internalized stigma showed a negative association with perceived family collaboration. In the context of foreign caregivers in Taiwan, a study highlighted the differences in language, religion, culture, values, and expectations between foreign caregivers and stroke survivors influenced the caregiving experience.13 Additionally, another study demonstrated that being a foreign caregiver was not correlated with depression among older individuals in Taiwan.14 With respect to gender-related issues, two studies conducted in Taiwan found that female caregivers more frequently reported symptoms of diminished well-being, decreased psychosocial health, and lower overall self-rated health.15,16 Further research is needed to clarify the gender differences in depression among caregivers of individuals with depressive disorders.
Several studies have examined the associated factors of depression among caregivers of patients with different physical conditions, such as dementia, cancer, etc. Previous studies have detected associated factors for depressive disorder in caregivers of patients with dementia, included older age, low income, being a wife/female spouse, and hours spent caregiving.17,18 Prior studies have found that risk factors for depressive disorder in caregivers of patients with cancer included being female, with a younger age, a past history of depression, advanced cancer stage of the patients, having a lower educational level, poor family support, and impaired social functioning.19–21 Based on the abovementioned literature review, we hypothesized that lower family support, higher suicide risk, a past history of depression, and lower educational level were possible associated factors of depression in caregivers of depressive patients. To our knowledge, no study has yet been done on the associated factors of depression in caregivers of patients with depression. The aim of our study was to evaluate the morbidity and associated factors of depression in caregivers of patients with depressive disorder.
Methods
Participants
This study used a cross-sectional design with consecutive sampling. Participants were recruited from the psychiatric outpatient/inpatient departments at a general hospital from August 2021 to June 2022. The inclusion criteria were as follows: (1) individuals who are the depressive patient’s principal caregiver, which we defined as “living with the patient and taking care of his/her daily needs”; (2) individuals who have the ability to understand the study procedure and can provide written informed consent. The exclusion criteria were as follows: individuals who are too weak to complete the questionnaire or clinical interview.
Procedures
Ethical approval was obtained from the human research ethics committee of Chang Gung Memorial Hospital (202002316B0). Ethical standards formulated from the Helsinki Declaration of 1964 and revised in 2013 were followed. The study procedure consisted of the following steps: (1) depressive patients’ and their caregivers referred from the psychiatric outpatient clinic were asked to sign written informed consent. (2) Depressive patients and their caregivers attended an appointment and were identified as fulfilling the inclusion criteria; (3) the MINI was used by a senior psychiatrist (Dr. Y. Lee) to reach a psychiatric diagnosis; (4) one trained research assistant collected the depressive patients and their caregivers’ demographic and clinical data and clinical rating scales data, including the Hospital Anxiety and Depression Scale (HADS), Suicide Assessment Scale (SAS), Stigma Scale of the Explanatory Model Interview Catalogue (EMIC), and Family APGAR Index through in-person interview and reading out the questions.
Assessment
Hospital Anxiety and Depression Scale (HADS)
The HADS is a 14-item self-administered questionnaire for assessing the severity of anxiety and depression symptoms.22 The HADS is commonly used in hospital practice and primary care and for the general population.23 Seven items are used to assess anxiety, and the other seven items are used to assess depression. Each item has four possible responses (scored 0–3); the anxiety (HADS-A) and depression (HADS-D) subscales have independent measures.17 The Cronbach’s alpha for HADS in this study was 0.886. The sensitivity and specificity for both HADS-A and HADS-D of approximately 0.80 were similar to the sensitivity and specificity achieved by the General Health Questionnaire (GHQ).24
The Chinese version of the Hospital Anxiety and Depression Scale (HADS) was initially employed to identify depression in individuals with chronic headaches, and it demonstrated satisfactory validity.25 In our study, we aimed to evaluate the validity of the self-reported HADS as a screening tool for depression in patients diagnosed with head and neck cancer (HNC). Our sample consisted of 93 HNC patients, and we determined that a cutoff score of 8 on the HADS yielded good validity, as evidenced by the mean area under the receiver operating characteristic curve of 0.975±0.015.26
Suicide Assessment Scale (SAS)
The Suicide Assessment Scale (SAS) was developed by a prospective study on repeated suicide attempts among suicidal cases in a general hospital.27 The SAS was verified to have satisfactory reliability and validity and can be applied in the clinical setting to evaluate patients’ suicidal risk.28 The SAS is composed of four dimensions: negative ideation, positive ideation, impulsivity, and aggression. Each dimension has five items. Possible total scores on the SAS range from 0 to 80, with higher scores indicating more severe suicidal risk.28 The Cronbach’s alpha for the SAS in this study was within 0.663 to 0.943. The concurrent validity of the SAS was achieved by the SAS scores, which were significantly associated with the Beck Hopelessness Scale (g = 0.32, P < 0.001).
Stigma Scale of the Explanatory Model Interview Catalogue (EMIC)
The Explanatory Model Interview Catalogue (EMIC) is an anthropologically-based semi-structured interview schedule that systematically examines patients’ help-seeking behavior for quantitative and qualitative data information.29 EMIC was used as a study instrument and widely applied in the field of cultural psychiatry, which focused on patients’ illness behavior and stigma in the last 20 years.30,31 Possible total scores on the Stigma Scale of EMIC range from 0 to 24, with higher scores indicating greater stigma. The Cronbach’s alpha for EMIC in this study was 0.828. The convergent validity of both EMIC and the Participation Scale was confirmed by Spearman’ s rank order correlation, which showed a moderate to strong correlation (r = 0.48, p = 0.001).32
Family APGAR Index
The Family APGAR index assesses a family member’s perception of family functioning and family support by examining his/her satisfaction with family relationships.33 It is composed of five parameters: adaptation, partnership, growth, affection, and resolution with a three-point scale ranging from 0 (hardly ever) to 2 (almost always). The total scores range from 0 to 10, with higher scores representing higher levels of family functioning and family support. The Cronbach’s alpha for the Family APGAR Index in this study was 0.940. The construct validity of APGAR was yielded by an APGAR/ Pless-Satterwhite correlation of 0.80 and an APGAR/ therapist estimate correlation of 0.64~0.80.34
In a pioneering study conducted in Taiwan by Chau et al, the Chinese version of the Family APGAR was utilized. The study involved 113 participants from 45 Chinese families, and the results demonstrated a significant correlation between Family APGAR scores and the scores obtained from the Chinese Health Questionnaire. The authors suggested that the Family APGAR index is a valuable and straightforward tool for identifying patients with familial dysfunction in routine clinical settings.35
Mini International Neuropsychiatric Interview (MINI)
The MINI is a short, structured clinical interview designed for making an accurate psychiatric diagnosis based on the DSM-IV or ICD-10.36 It has good sensitivity and specificity and can be administrated by non-physicians. The validity and reliability of the MINI has been examined using the Structured Clinical Interview for DSM-III-R Patients (SCID-P) with satisfactory results.37 The sensitivity and specificity were good or very good for all diagnoses with the exception of generalized anxiety disorder (GAD) (kappa=0.36), agoraphobia (sensitivity=0.59), and bulimia (kappa=0.53).37 The Taiwanese version of the MINI was translated by a team of experienced psychiatrists and subsequently retranslated into English. The copyright for the Taiwan Society of Psychiatry was obtained from the original author. The Taiwanese version of the MINI underwent rigorous validation procedures, including specialist validity assessment. To evaluate interrater reliability, trained psychiatrists conducted interviews with residents, resulting in a k value of 0.75 and a Z score of 13.22.38,39 The assessment time is approximately 15–20 minutes. The kappa values of the MINI were within 0.90~0.43.
MINI Suicidal Scale
The MINI Suicidal Scale, one of the modules of the MINI, is a short structured diagnostic interview that was jointly developed and validated by psychiatrists and clinicians in the United States and Europe for the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Classification of Mental and Behavioural Disorders (ICD-10). This instrument can quantitatively evaluate suicide risk and differentiate suicide risk levels (high, moderate, low). In a retrospective study of patients admitted to a psychiatric emergency department, the MINI categorized suicide attempters and non-attempters with an area under the curve (AUC) of 0.84 by ROC analysis.40
Statistics
Descriptive and inferential statistics were analyzed using SPSS for Windows v. 24.0. We first used descriptive statistics (chi-square and t-tests) to determine differences in demographic data and clinical characteristics between subjects with and without depressive disorder. We used Bonferroni correction to adjust for multiple testing in the correlation matrix. A stepwise forward model of logistic regression was used to test the factors associated with depressive disorder.
Results
A total of 136 caregivers were initially recruited for this study; 10 declined to enter the study, and of the remaining 126 participating, six who had agreed did not complete the questionnaires. Data collection was completed with the remaining 120 patients, with a response rate of 88.2%. Out of the 120 caregivers included in the study, 50 (41.7%) were spouses, 36 (30.0%) were children, 18 (15.0%) were parents, 5 (4.2%) were siblings, and 11 (9.2%) comprised friends, grandparents, or daughter-in-law.
Of the 120 caregivers who successfully completed the study, 59.2% (n=71) were females. The average age of the subjects was 52.6 (±14.9) years. Their mean education level was 13.1 (±2.2) years, 67.5% were married, and 54.2% were currently employed. Fifty-three percent of caregivers had a co-morbidity of one or more physical illnesses, 5% had past suicide history, 15% had family suicide history, 51% had family psychiatric history, and 26.7% had hypnotic use history (Table 1). The demographic and clinical data of the 120 depressive patients who were being cared for are shown in Table S1.
 |
Table 1 Baseline Demographic and Clinical Characteristics in Caregivers of Depression Patients (N=120) |
The most common psychiatric diagnoses of the caregivers were depressive disorders (25.8%), followed by anxiety disorders (17.5%) and insomnia disorder (15.8%). Among the depressive disorders, the most prevalent was major depressive disorder (MDD) (12.5%), followed by other specified depressive disorder (8.3%) and persistent depressive disorder (5.0%). Fifty-four percent of caregivers had a psychiatric diagnosis (Table 2). Among the anxiety disorders, the most prevalent was other specified anxiety disorder (10.0%), followed by generalized anxiety disorder (5.8%), panic disorder (0.8%), and social phobia (0.8%).
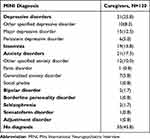 |
Table 2 Psychiatric Diagnoses in Caregivers |
In the univariate analyses of the 120 caregivers, factors significantly associated with depressive disorders included past psychiatric history (x2=19.59, p<0.001), past suicide history (x2=18.13, p<0.001), more habitual hypnotics use (48.4% vs 19.1%, p=0.001), higher anxiety scores (9.6±4.9 vs 3.9±3.1, p<0.001), lower APGAR scores (4.3±3.8 vs 7.3±3.1, p<0.001), and greater SAS suicide risk [20.9(1–57) vs 9.2(0–34), p<0.001] (Table 1). The HADS scores of depressive patients did not significantly differ between depressive caregivers and non-depressive caregivers (Table 1).
When the above significant factors were analyzed relative to depressive disorders using the stepwise forward model of logistic regression, anxiolytics/hypnotics use (OR=5.58; 95% CI, 1.84–16.96; p<0.01), higher suicide risk (SAS) (OR=1.10; 95% CI, 1.05–1.16; p<0.001), and lower family support (APGAR scores) (OR=0.82; 95% CI, 0.71–0.94; p<0.01) were discovered to be three significant associated factors (Table 3).
 |
Table 3 Associated Factors of Depressive Disorder Among Caregivers: Logistic Regression Analysis |
When comparing male caregivers to female caregivers of patients with depression, several notable differences emerged. Male caregivers were found to be older (57.8±12.9 vs 49.0±14.0, P=0.001), more likely to be married (85.7% vs 54.9%, P<0.001), and exhibited lower levels of depressive severity (7.4±5.4 vs 11.9±8.3, P<0.001) as well as anxiety severity (3.4±2.9 vs 6.7±4.8, P<0.001) in comparison to their female counterparts (Table 4).
 |
Table 4 Gender Difference of Demographic and Clinical Characteristics in Caregivers of Depression Patients (N=120) |
Discussion
To the best of our knowledge, this study is the first to focus on depression morbidity of caregivers in patients with depressive disorder. The most prevalent psychiatric diagnoses of the caregivers were depressive disorders (25.8%). Caregivers of patients with depression experience care burden, worry, and economic load and are vulnerable to developing such mental conditions as insomnia, anxiety, and depression. Compared to other diseases’ caregivers, the morbidity of depression of this study is about double that of head and neck cancer (14.7%)19 and Parkinson’s disease (PD) (11.1%).41 This finding suggests that when caring for psychiatric disorder, the risk of having depression in caregivers is higher than with physical diseases, which may be related to providing more mental care and perhaps an existing dyadic interaction. Furthermore, our morbidity of major depression (12.5%) was higher than a previous community study among the adult population in Taiwan (1.2%).42 Possible explanations for this discrepancy are (1) our sample was from a special population, caregivers of depressive patients, who might have more psychosocial stress than the general population, and (2) distress of having a depressed caregiver induces new, or worsens existing, psychiatric disorders.42
Although HADS scores of depressive patients did not significantly differ between depressive caregivers and non-depressive caregivers, patients’ depression severity (HADS) was positively correlated to caregivers’ depression severity (HADS) (r=0.294, p<0.01). This result suggests that patients’ depression severity may impact caregivers’ depression. It may also raise the hypothesis that some couples have some sort of shared depressive symptomology apart from the impact of depression. Further studies are warranted to test the above hypothesis.
In the present study, depression of caregivers may come from before taking care of depressive patients or after taking care of depressive patients. It relates the concept of pre-morbid depressive symptoms or diagnosis of partner-depression-induced-caregiver-depression. However, it cannot be differentiated in this study due to a lack of collecting data to separate those two stages. Further studies should be conducted to clarify this concept.
The highest associated factor for depressive disorder in this study was hypnotics use. Patients with habitual hypnotics use usually have the problem of chronic insomnia. A prior study supports the concept that insomnia is a risk factor for developing major depression.43 In a study of 591 young community adults, Buysse found that insomnia lasting two weeks or longer predicted major depressive episodes.43 Moreover, a previous study on depression in caregivers of head and neck cancer also found that hypnotic use was associated with depression.44 Based on the above results, the caregivers in our study who had habitual hypnotics use could have been more vulnerable to developing depressive disorder. However, it is important to note that insomnia can be one of the symptoms of depressive disorder, and the use of hypnotics may be a means of seeking relief from insomnia. Therefore, the relationship between hypnotic use and depressive disorder could be bidirectional.
Suicide risk was the third risk of depression among caregivers in our study. Lee et al41 investigated 101 PD patients’ caregivers and found that a high severity of suicide in caregivers was associated with severity of depression and with having depressive disorder. This notion supports our result that suicide risk is one of the risk factors for depression among caregivers. Suicide risk comprises four dimensions: suicidal ideation, suicidal plan, suicidal gestures, and suicide attempt. Few studies have focused on detecting suicide risk in caregivers. In a nationwide survey in Korea, Park et al found that family caregivers with anxiety or depression had higher rates of suicidal ideation and suicide attempts than did family caregivers without anxiety and depression.45 Huang et al conducted a study to investigate the proportion of caregivers of individuals with physical or mental disabilities experiencing suicidal ideation and found that nearly one-fifth (18.8%) of caregivers had experienced suicidal ideation.46 Above-mentioned two studies in both Korea and Taiwan found that caregivers had a higher suicide risk, and these findings were in line with our results that suicide risk is associated with depression in depressive patients’ caregivers.45,46 Of note, depressive caregivers had a 21% higher severity of suicide risk than non-depressive caregivers, and clinicians should pay particular attention to this special group’s mental condition to prevent possible tragedy.
Many of the variables discussed in this study can be encompassed within the construct of demoralization. This construct originated from the pioneering work of Clarke and Kissane (2002) and has been primarily explored in psychosomatic contexts involving both patients and healthcare professionals.47 The sub-components of this construct’s definition strikingly capture the experiences that caregivers may encounter. These sub-components include feelings of hopelessness or disheartenment, a loss of meaning in life, helplessness, a sense of failure, and dysphoria.47 Dismissing these experiences in individuals who do not meet the criteria for depression, as outlined in the DSM-5 criteria, can be highly perilous, as demoralization is associated with a significant risk of suicidal ideation and behavior.48 Further research on demoralization and its association with suicide risk in caregivers of individuals with depression is necessary to validate this concept.
In our study, family support was negatively associated with depression in depressive patients’ caregivers. Most previous studies have shown that low family support was related to depressive patients with cancer, sexual minority men, or people living with HIV/AIDS.49–52 For example, Su et al detected in 300 breast cancer patients an association between family support and major depressive disorder. The result demonstrated that low family support (odds ratio =0.87, 95% CI: 0.78–0.98) was an associated factor for depressive disorder in breast cancer patients. Nevertheless, very few studies have been performed on family support and caregiver depression.49 Only one study from Taiwan has focused on the association between family support and depression in caregivers of persons with ADHD. In that study, 382 caregivers of children with ADHD underwent one-year follow-up assessment, and caregivers’ perception of having low family support at baseline was found to predict depressive symptoms 1 year later.52 This study supports our result that lower family support is associated with depression in depressive patients’ caregivers. This result suggests that caregivers are a vulnerable group and need other social support or families’ care. To date, no other study has detected family support and its association with depression of depressive patients’ caregivers. More studies are needed to confirm our finding.
In addition to the four significant associated factors mentioned above, lower years of education, unmarried status, past psychiatric history, past suicide history, higher anxiety scores, higher conscientiousness scores, and higher stigma scores were associated with depression in caregivers of depressive patients. These factors were partially supported by prior studies on caregivers of patients with cancer or Parkinson disease.14–16,31 Even though the aforementioned factors showed non-significance after logistic regression analysis, clinicians should still be aware of these factors in order to have better psychoeducation and coping skills training for caregivers to prevent them from developing depressive disorder.
In this study, we observed gender differences among caregivers, with male caregivers being older, more likely to be married, experiencing lower levels of depression and anxiety. Previous research has indicated that female patients often experience higher levels of burden compared to male patients.15 Moreover, studies have consistently shown that female caregivers more frequently experience a decrease in psychosocial health and overall self-rated health.16 In addition to the aforementioned health-related issues, our study uncovered another noteworthy finding: female caregivers exhibited a higher prevalence of mood problems compared to their male counterparts. To validate our results, further large-scale prospective studies are warranted.
The strength of this report is that it is the first study on morbidity and associated factors of depressive disorder in caregivers of depressive patients using a standardized structured diagnostic interview. Nevertheless, this study has several limitations that should be mentioned: (1) our study design involved consecutive sampling, which may have led to sampling bias. However, a response rate of 88.2% of the caregivers helped negate the effect of this limitation. (2) We did not obtain reasons from the 16 caregivers who refused to participate in this study, but they likely had stigma about being studied, did not have time, or were too depressed to be interviewed. (3) This was a cross-sectional study, which did not allow for the exploration of those caregivers’ psychiatric disorders through the course of the disease. Therefore, further follow-up studies should be conducted to understand the precise nature of depression morbidity in caregivers of depressive patients, as well as any associated factors involved. (4) Our results cannot separate pre-morbid depressive symptoms or diagnoses from the concept of partner-depression-induced-caregiver-depression since we did not collect data to separate those two stages. Further studies are warranted to elucidate this concept. (5) We also did not clarify the relationship between physical comorbidity of depressive patients and caregivers’ depression, which may skew the pre-morbid psychopathology of caregivers. (6) Finally, our samples were taken from a general hospital, which may not be representative of the general population.
Conclusion
In conclusion, depression was the most prevalent psychiatric diagnosis in caregivers of patients with depressive disorder. Anxiolytics/hypnotics use, higher suicide risk, and lower family support were three significant associated factors of depression. The implications of this study are: 1. The prevalence of major depression in caregivers of depressive patients is higher than that of the general population in Taiwan. 2. The morbidity of caregivers among depressive patients is more prevalent than that of caregivers of patients with physical illness. 3. Early psychiatric diagnosis for caregivers of patients with depression and the proper management of these associated factors of depression are crucial to offering suitable support and treatment and may improve caregivers’ quality of life.
Data Sharing Statement
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported by a grant from the Ministry of Science and Technology, Taiwan (MOST 110-2314-B-182A-041-).
Disclosure
The authors hereby declare that they have no conflicts of interest to disclose in relation to this article.
References
1. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi:10.1016/S0140-6736(13)61611-6
2. Proudman D, Greenberg P, Nellesen D. The growing burden of Major Depressive Disorders (MDD): implications for researchers and policy makers. Pharmacoeconomics. 2021;39:619–625. doi:10.1007/s40273-021-01040-7
3. Collaborators GDa IIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi:10.1016/S0140-6736(18)32279-7
4. Melhem NM, Porta G, Oquendo MA, et al. Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry. 2019;76:603–613. doi:10.1001/jamapsychiatry.2018.4513
5. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:2861. doi:10.1038/s41598-018-21243-x
6. Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi:10.1186/1741-7015-9-90
7. Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief; 2018:1–8.
8. Rivera HR. Depression symptoms in cancer caregivers. Clin J Oncol Nurs. 2009;13:195–202. doi:10.1188/09.CJON.195-202
9. Liew TM, Tai BC, Yap P, Koh GC. Comparing the effects of grief and burden on caregiver depression in Dementia caregiving: a longitudinal path analysis over 2.5 years. J Am Med Dir Assoc. 2019;20:977–983.e974. doi:10.1016/j.jamda.2018.11.016
10. García-Torres F, Jabłoński MJ, Gómez Solís Á, et al. Caregiver burden domains and their relationship with anxiety and depression in the first six months of cancer diagnosis. Int J Environ Res Public Health. 2020;18:17. doi:10.3390/ijerph18010017
11. Marguerite S, Laurent B, Marine A, et al. Actor-partner interdependence analysis in depressed patient-caregiver dyads: influence of emotional intelligence and coping strategies on anxiety and depression. Psychiatry Res. 2017;258:396–401. doi:10.1016/j.psychres.2017.08.082
12. Wu HC, Chen FP. Sociocultural Factors Associated with Caregiver-Psychiatrist Relationship in Taiwan. Psychiatry Investig. 2016;13:288–296. doi:10.4306/pi.2016.13.3.288
13. Mauludina YS, Kustanti CY, Fields BE, Chang FH. A descriptive qualitative study of Foreign caregivers of older adult stroke survivors. Gerontologist. 2023;63:82–95. doi:10.1093/geront/gnac077
14. Chiao CY, Schepp KG. The impact of foreign caregiving on depression among older people in Taiwan: model testing. J Adv Nurs. 2012;68(5):1090–1099. doi:10.1111/j.1365-2648.2011.05814.x
15. Kao HFS, McHugh ML. The role of caregiver gender and caregiver burden in nursing home placements for elderly Taiwanese survivors of stroke. Res Nurs Health. 2004;27:121–134. doi:10.1002/nur.20007
16. Chiou CJ, Chen IP, Wang HH. The health status of family caregivers in Taiwan: an analysis of gender differences. Int J Geriatr Psychiatry. 2005;20:821–826. doi:10.1002/gps.1364
17. Covinsky KE, Newcomer R, Fox P, et al. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. J Gen Intern Med. 2003;18:1006–1014. doi:10.1111/j.1525-1497.2003.30103.x
18. Givens JL, Mezzacappa C, Heeren T, Yaffe K, Fredman L. Depressive symptoms among dementia caregivers: role of mediating factors. Am J Geriatr Psychiatry. 2014;22:481–488. doi:10.1016/j.jagp.2012.08.010
19. Lee Y, Lin PY, Chien CY, Fang FM. Prevalence and risk factors of depressive disorder in caregivers of patients with head and neck cancer. Psychooncology. 2015;24:155–161. doi:10.1002/pon.3619
20. Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. 2004;31:1105–1117. doi:10.1188/04.ONF.1105-1117
21. Haley WE, LaMonde LA, Han B, Burton AM, Schonwetter R. Predictors of depression and life satisfaction among spousal caregivers in hospice: application of a stress process model. J Palliat Med. 2003;6:215–224. doi:10.1089/109662103764978461
22. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
23. Mitchell AJ, Meader N, Symonds P. Diagnostic validity of the Hospital Anxiety and Depression Scale (Hads) in cancer and palliative settings: a meta-analysis. J Affect Disord. 2010;126:335–348. doi:10.1016/j.jad.2010.01.067
24. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi:10.1016/S0022-3999(01)00296-3
25. Juang KD, Wang SJ, Lin CH, Fuh JL. Use of the hospital anxiety and depression scale as a screening tool for patients with headache. Zhonghua Yi Xue Za Zhi. 1999;62:749–755.
26. Lee Y, Wu YS, Chien CY, et al. Use of the Hospital Anxiety and Depression Scale (Hads) and the Taiwanese Depression Questionnaire (TDQ) for screening depression in head and neck cancer patients in Taiwan. Neuropsychiatr Dis Trea. 2016;2016:2649–2657.
27. Lee Y, Lin P-Y, Yeh W-C, et al. Repeated suicide attempts among suicidal cases: outcome of one-year follow-up. Asia Pac Psychiatry. 2012;4:174–180. doi:10.1111/j.1758-5872.2012.00189.x
28. Yeh AW-C, Hung C-F, Lee Y, et al. Development and validation of the Assessment for Repeated Suicide. Asia Pac Psychiatry. 2012;4:20–29. doi:10.1111/j.1758-5872.2011.00165.x
29. Weiss MG, Doongaji DR, Siddhartha S, et al. The Explanatory Model Interview Catalogue (EMIC). Contribution to cross-cultural research methods from a study of leprosy and mental health. Br J Psychiatry. 1992;160:819–830. doi:10.1192/bjp.160.6.819
30. van Brakel WH, Cataldo J, Grover S, et al. Out of the silos: identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med. 2019;17:13. doi:10.1186/s12916-018-1245-x
31. Ackumey MM, Gyapong M, Pappoe M, Weiss MG. Help-seeking for pre-ulcer and ulcer conditions of Mycobacterium ulcerans disease (Buruli ulcer) in Ghana. Am J Trop Med Hyg. 2011;85:1106–1113. doi:10.4269/ajtmh.2011.11-0429
32. Chung EY, Lam G. Validation of two scales for measuring participation and perceived stigma in Chinese community-based rehabilitation programs. Health Qual Life Outcomes. 2018;16:105. doi:10.1186/s12955-018-0938-3
33. Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. 1978;6:1231–1239.
34. Good M-JD, Smilkstein G, Good BJ, Shaffer T, Arons T. The Family APGAR Index: a study of construct validity. J Fam Pract. 1979;8:577–582.
35. Chau TT, Hsiao TM, Huang CT, Liu HW. A preliminary study of family Apgar index in the Chinese [Article in Chinese]. Gaoxiong Yi Xue Ke Xue Za Zhi. 1991;7:27–31.
36. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33;quiz 34–57.
37. Sheehan DV, Lecrubier Y, Harnett Sheehan K, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. doi:10.1016/S0924-9338(97)83297-X
38. Chou FHC, Su TTP, Chou P, Ou-Yang WC, Lu MK, Chien IC. Survey of psychiatric disorders in a Taiwanese village population six months after a major earthquake. J Formos Med Assoc. 2005;104:308–317.
39. Chou FH. The Follow Up Study on Psychiatric Diseases Among 921 Earthquake Survivors [Doctoral Thesis]. Taiwan: National Yang-Ming University; 2003.
40. Innamorati M, Pompili M, Serafini G, et al. Psychometric properties of the suicidal history self-rating screening scale. Arch Suicide Res. 2011;15:87–92. doi:10.1080/13811118.2011.540471
41. Lee Y, Chiou YJ, Hung CF, et al. Prevalence and Associated Factors of Depressive Disorder in Caregivers of Individuals With Parkinson Disease. J Geriatr Psychiatry Neurol. 2021;34:418–425. doi:10.1177/0891988720933359
42. Liao SC, Chen WJ, Lee MB, et al. Low prevalence of major depressive disorder in Taiwanese adults: possible explanations and implications. Psychol Med. 2012;42:1227–1237. doi:10.1017/S0033291711002364
43. Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–480. doi:10.1093/sleep/31.4.473
44. Lee CY, Lee Y, Wang LJ, Chien CY, Fang FM, Lin PY. Depression, anxiety, quality of life, and predictors of depressive disorders in caregivers of patients with head and neck cancer: a six-month follow-up study. J Psychosom Res. 2017;100:29–34. doi:10.1016/j.jpsychores.2017.07.002
45. Park B, Kim SY, Shin JY, et al. Suicidal ideation and suicide attempts in anxious or depressed family caregivers of patients with cancer: a nationwide survey in Korea. PLoS One. 2013;8:e60230. doi:10.1371/journal.pone.0060230
46. Huang YC, Hsu ST, Hung CF, Wang LJ, Chong MY. Mental health of caregivers of individuals with disabilities: relation to Suicidal Ideation. Compr Psychiatry. 2018;81:22–27. doi:10.1016/j.comppsych.2017.11.003
47. Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust NZ J Psychiatry. 2002;36:733–742. doi:10.1046/j.1440-1614.2002.01086.x
48. Costanza A, Vasileios C, Ambrosetti J, et al. Demoralization in suicide: a systematic review. J Psychosom Res. 2022;157:110788. doi:10.1016/j.jpsychores.2022.110788
49. Su JA, Yeh DC, Chang CC, et al. Depression and family support in breast cancer patients. Neuropsychiatr Dis Treat. 2017;13:2389–2396. doi:10.2147/NDT.S135624
50. Boyd DT, Ramos SR, Quinn CR, Jones KV, Wilton L, Nelson LE. Family support and sociocultural factors on depression among black and latinx sexual minority men. Int J Environ Res Public Health. 2021;19(1):18. doi:10.3390/ijerph19010018
51. Shrestha S, Poudel KC, Poudel-Tandukar K, et al. Perceived family support and depression among people living with HIV/AIDS in the Kathmandu Valley, Nepal. J Int Assoc Provid AIDS Care. 2014;13:214–222. doi:10.1177/1545109712456741
52. Chou WJ, Hsiao RC, Chang CC, Yen CF. Predictors of depressive symptoms in caregivers of children with attention-deficit/hyperactivity disorder: a One-Year Follow-Up Study. Int J Environ Res Public Health. 2021;19:18.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
