Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
The Long-Term Maintenance Effect of Remote Pulmonary Rehabilitation via Social Media in COPD: A Randomized Controlled Trial
Authors Li Y , Qian H, Yu K , Huang Y
Received 29 January 2022
Accepted for publication 1 May 2022
Published 11 May 2022 Volume 2022:17 Pages 1131—1142
DOI https://doi.org/10.2147/COPD.S360125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Yi Li, Hongyu Qian, Kewei Yu, Ying Huang
Department of Respiratory and Critical Care Medicine, Tianjin Chest Hospital, Tianjin, People’s Republic of China
Correspondence: Yi Li, Department of Respiratory and Critical Care Medicine, Tianjin Chest Hospital, Tianjin, People’s Republic of China, Email [email protected]
Background: Although the benefits of conventional pulmonary rehabilitation (PR) maintenance are well documented, it is challenged by many difficulties. We investigated whether remote home-based PR maintenance strategy via social media (WeChat) is effective on clinical improvements and reducing the risk for acute exacerbation of chronic obstructive pulmonary disease (COPD).
Methods: The eligible stable COPD patients completing an initial 8-week PR were allocated into three groups randomly. Group A: PR maintenance via social media supervision at home. Group B: PR maintenance at hospital. Group C: Usual care. During a 12-month follow-up, the frequency of acute exacerbation of COPD (AECOPD), 6 minutes walking test (6MWT), COPD assessment test (CAT), and modified Medical Research Council scale (mMRC) were evaluated every 3 months.
Results: At the end of the follow-up, compared to the decline in the usual care group (n = 49), the clinical improvements of 6MWD, CAT, and mMRC were sustained in both the home-based group (n = 47) and the hospital-based maintenance group (n = 44) (p < 0.001), no difference was observed between these two groups (p > 0.05). In multivariate analysis, the home-based PR maintenance and hospital-based PR maintenance were independent predictors of lower risk for AECOPD (incidence rate ratio (IRR) 0.712, 95% CI 0.595– 0.841, p < 0.001 and IRR 0.799, 95% CI 0.683– 0.927, p = 0.002), respectively.
Conclusion: Remote PR maintenance via social media is effective in reducing the risk for AECOPD and keeping the clinical improvement from decline. Remote PR maintenance via social media might be used to deliver alternatives to conventional PR.
Keywords: chronic obstructive pulmonary disease, pulmonary rehabilitation, maintenance, exacerbations, home monitoring
Introduction
Chronic obstructive pulmonary disease (COPD) is a major public health problem and is the third leading cause of death in China.1 According to Global Strategy for the Diagnosis, Management, and Prevention of COPD (GOLD) 2022,2 pulmonary rehabilitation (PR) as one of the effective non-pharmacological therapies was recommended in COPD patients, to improve their symptoms, activities of daily living, muscle and emotional function as well as quality of life. Although the improvements of PR were well documented, these benefits could decrease gradually over time.3,4 Therefore, researches explored long-term maintenance strategies to extend PR benefits. Based on the results of recent studies,5,6 GOLD 2022 stated that a maintenance program should be provided to patients to increase and maintain activities of daily living.2
Despite the benefits, different PR maintenance programs were also challenged by many difficulties, such as distance to obstacle,7 lower frequency8 and unsupervised maintenance exercise.9 Recently, the American Thoracic Society (ATS)/European Respiratory Society (ERS) statement recommended that tele-rehabilitation was regarded as an alternative approach to increase the long-term degree of participation for PR maintenance,10 making it more efficient and feasible. Tele-rehabilitation involves the delivery of medical rehabilitation services to patients remotely via electronic information and social media.11 For example, one study of 10 patients with COPD investigated the effectiveness of telerehabilitation maintenance indicating that the strategy can decrease the frequency of acute exacerbation of COPD, improve health status and QoL.12 Recently, an intervention of PR maintenance strategy via tele-contact provided relevant clinical benefits on reduction in risk of exacerbation of COPD, hospitalization at the end of one-year follow-up.13 Moreover, Twitter and Facebook can provide convenient visual guidance and supervision to participants, results in improving the maintenance efficiency.14 To date, accumulating evidence indicates improvement from telerehabilitation. Although the results are promising, a system review showed that QoL, and exercise capacity could be possibly improved via supervised PR maintenance (telephone or web platform) but with low strength evidence due to high risk of bias.15 Likewise, other limitations such as high dropout rate, short PR maintenance duration, small sample size or poor adherence,16,17 made the value of telerehabilitation maintenance limited.
WeChat has rapidly developed into a comprehensive information platform integrating communication, entertainment, search, office collaboration, corporate customer service and medicine in China.18 The recent study indicated that WeChat app-based education and rehabilitation could reduce the emotional dysfunction such as anxiety, depression and improve QoL in non-small lung cancer patients undergoing surgery.19 It is reasonable to apply new technology in PR maintenance management in patients with COPD. Thus, we established a new system for PR maintenance under the WeChat platform. To our knowledge, our study is the first prospective clinical trial to explore a new WeChat PR maintenance strategy to maintain the clinical improvements of an initial PR program in Tianjin, North China.
Methods
Study Design and Participants
A one-year single-center random clinical trial was conducted by Tianjin Chest Hospital to investigate the effect of home-based maintenance strategy via WeChat and hospital-based maintenance compared with usual care (ChiCTR1900021320) from January 2019 to March 2021. Patients were enrolled by respiratory department in Tianjin Chest Hospital, which is a tertiary hospital offering specialized medical care in pulmonary and cardiovascular diseases. We included patients who were 1) having a diagnosis of stable COPD in the first 4 weeks according to guideline,2 2) able to complete the PR program and questionnaire survey successfully and independently, and 3) able to use WeChat proficiently. The exclusion criteria included the following: 1) having asthma; obstructive sleep apnea syndrome; underdiagnosis of cancer; diagnosed with Alzheimer’s disease or depression and anxious disorder, 2) having severe dysfunction of the heart, liver, or kidney, 3) unavailable for exercise, 4) suffering emotional trauma in the previous 6 months such as relative death and divorce, 5) life expectancy less than 1 year, and 6) history of PR exercise for a long time (≥3 times/week, ≥20 minutes/time, persisting for more than 12 months). All of the patients were requested to perform an 8-week primary PR program. Then, eligible participants were randomized after baseline post-PR measure on a 1:1:1 basis using a computer-generated randomized sequence to two interventional groups and one control group of the following. After the generation of this sequence, the envelopes were created, numbered in the appropriate order, and contained the result of the allocation. The order of the envelopes’ number was defined based on the order of participants’ enrollment. Randomization was independent of the control of the principal investigator, thereby maintaining a minimization randomization process. Based on intervention during follow-up, patients were allocated into Group A: PR maintenance via WeChat at home, Group B: PR maintenance at hospital, or Group C: Usual care throughout 12-month observation without maintenance. All patients provided written and verbal informed consent. This study was approved by the Ethics Committees of Tianjin Chest Hospital (No. 2019KY-004-01), and was conducted in accordance with the Declaration of Helsinki.
PR Intervention
The initial 8-week PR includes; (A) upper resistance training, (B) aerobic training, (C) balance and flexibility training, (D) respiratory training, and (E) health education and self-management. The details of PR physical sessions are well documented in our previous study.6 The session of health education and self-management help COPD patients to acquire the skills they need to carry out disease-specific medical regimens, guide changes in health behavior and provide emotional support to enable them to control their disease.20
Maintenance Strategy
After the initial 8-week PR, the patients of Group A performed the maintenance exercises at home via WeChat supervision. We established a PR maintenance group-chat platform team, which consisted of respiratory specialists, physiotherapists, pharmacists, nutritionists, and nurses. The respiratory specialists and head nurse served as the team leaders and were responsible for the operation and guidance of the project. The PR guideline video was uploaded once a week by physiotherapists. The home-based PR maintenance program was requested twice a week and completion of exercise had to be uploaded in time by participants. Patients could also upload their training pictures or speeches. Other patients and PR teammates can interact with them by commenting or giving thumbs up, thus promoting not only peer support between patients but also communication between doctors and patients. Moreover, the physiotherapists were also responsible for making tailored prescriptions and sending it to the patients via private message. Patients could get the electronic PR prescription and contact a nurse online if the training program needed to be adjusted. The pharmacists were in charge of pharmacological therapy including the correct use of any prescribed respiratory medicine. Recognition of exacerbations of COPD, information for the family and social support were also provided by nurses via the WeChat platform. The PR teammates will answer the questions raised by patients in the platform by different message forms, such as text, voice, picture and video from 8am to 8pm every day. The information of health education and skill of self-management were also announced in this WeChat group regularly.
As for patients of Group B, they continued to perform the same maintenance training sessions twice a week at the out-patients department in hospital when they accomplished the primary 8-week PR. The consultant for pharmacology and nutrition was also offered by our PR team.
After the initial PR, the patients in Group C were only offered the health consultant including cigarettes cessation, long-term oxygen therapy, correct use skill of respiratory medicine, symptoms management, and nutrition without any exercise.
Assessments
The assessments below were performed before and after the integrated PR program as well as every three months in the outpatient department with the same physiotherapist during follow-up, aiming to supervise and evaluate the change of health status in COPD patients.
Primary Outcomes Measure
The numbers of acute exacerbation of COPD, hospitalizations due to acute exacerbation of COPD and ED visits, were compared among the three groups over one year following completion of the initial PR program. Acute exacerbation of COPD is defined as an acute worsening of respiratory symptoms that result in additional therapy according to GOLD.2 Hospitalizations (severe exacerbations) and Emergency Department visits (ED visits) because of acute exacerbation of COPD were also assessed.
Secondary Outcomes Measure
1) Spirometry, such as forced expiratory volume in 1 s (FEV1), FEV1% pred, forced vital capacity (FVC), FEV1/FVC%. Spirometry was measured at the baseline and post inhaling bronchodilator respectively.2
2) Physical capacity assessment: Six-minutes walking test (6MWT) will be recommended. According to protocol of American Thoracic Society,21 patients walk as long as they can in a 30-meter straight corridor in six minutes without any interruption. The valid distances they completed were recorded when they finished the test.
3) Chronic Obstructive Pulmonary Disease Assessment Test (CAT),22 CAT was used to evaluate the Health-Related Quality of Life (HRQoL) for follow-up.
4) Modified Medical Research Council scale (mMRC)23 was applied to assess the severity of breathless. The mMRC is an effective and convenient evaluation of clinical methods for rating apnea, which can be performed under different conditions for COPD patients.
5) Beck Depression Inventory (BDI) and State-trait Anxiety Inventory (STAI).24 The content of BDI includes 21 items including evaluation of nervousness, dizziness, inability to relax. STAI is aimed at measuring severity of current anxiety and tendency to be anxious.
6) Instrumental Activities of Daily Living (IADL). Measuring IADL is one of the best ways to evaluate the level of health,25 assess the progress of the disease, and evaluate the efficacy of rehabilitation or other treatments in patients with COPD.
Once any accident events of tachycardia (higher than 85% of target HR), hypoxia (pulse oxygen saturation (SaO2) is lower than 10% of baseline), hypertension (blood pressure is higher than 200/100 mmHg), and syncope were observed during exercise, patients are forbidden to continue training and given therapy immediately.
Study Procedures
The outcomes of all subjects were evaluated at baseline before primary 8-week PR, and immediately after completion of the PR program in all three groups. Then, the patients of Group A performed the maintenance exercise described above at home with WeChat supervision during 12-month follow-up, while Group B did the maintenance training at the out-patient department in hospital for one year. For Group C, only health suggestions were provided without any form of rehabilitation exercise following completion of the initial PR. The regular reviews were applied every three months during the one-year follow-up by the same physiotherapists.
Sample Size
The sample size requirements for this study were intended to provide adequate power for the analysis of the primary outcome. In the current study, the calculation of sample size was based on ANOVA repeated measurements between the three groups. From the previous study with patients with similar characteristics,26 we estimated the power calculation by using the minimum detectable difference in the number of acute exacerbations of COPD. This previous study assessed the effect of PR program on frequency of acute exacerbation of COPD before and after PR. The mean number of acute exacerbations of COPD was reduced from 4.56 in the year preceding PR to 3.18 (a mean difference (1.37) and SD (3.26), an effect of size 0.4) in the year following PR. We calculated that a sample size of 114 patients would achieve a power of 0.90, with a type-I error (α) of 0.05 (two-sided). To compensate for a potential dropout rate of 20%, 136 patients (46 patients in each group) will be enrolled.
Statistical Analysis
The Shapiro–Wilk test revealed that all data were normally distributed. Descriptive data for the three groups are presented as mean and SD for continuous variables and frequency for categorical variables. One-way analysis of variance (ANOVA) was used to compare differences among the three groups at baseline for all variables. Pair-wise Tukey’s post-hoc analysis was used to compare all pairs of variables in each group of pre- and post-initial PR. We applied repeated-measure ANOVA and multivariate ANOVA to test the differences over time in 6WMD, CAT, mMRC, BDI, SAI, TAI and between-group differences. Time to first AECOPD for each group were analyzed by Kaplan–Meier survival curves and Log rank tests. We analyzed data via SPSS, version 22.0 software (SPSS Inc., Chicago, IL, USA). A probability P-value of <0.05 was considered statistically significant.
Results
150 eligible patients with COPD who met the inclusion criteria and accomplished the baseline assessments (Table 1) undertook the primary pulmonary rehabilitation program at the out-patient department in Tianjin Chest Hospital for 2 months. At the end of the PR, 148 participants were randomized and evaluated again with the exception of two subjects who were excluded due to transportation. During the one-year observation, 3 patients were excluded due to lack of motivation in Group A, while 5 quit the maintenance PR because of transportation problems, lower exercise self-efficacy and an adverse event in Group B (Figure 1).
 |
Table 1 Demographic and Clinical Characteristics of Patients at Baseline (N = 150) |
 |
Figure 1 Flow chart of the study population. |
Effect of PR
Compared to pre-PR, the patients in all groups had statistically significant improvements in the 6MWD, mMRC, CAT and emotional evaluation at the end of primary PR (post-hoc paired t-tests), particularly the difference for change in 6MWD in Group A and Group C that exceeded 26 m which is considered a minimal clinically important difference (MICD) in patients with COPD.27 The between-group differences in each outcome measures after initial PR showed no statistical significance analyzed by one-way ANOVA (Table 2).
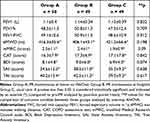 |
Table 2 The Differences of Clinical Improvements Between Pre- and Post-PR in All Three Groups |
The Frequencies of Acute Exacerbation, Hospitalization, and ED Visits
In comparison with the baseline, the frequencies of acute exacerbation of COPD, hospitalization, and ED visits all showed a significant decline at the end of one-year follow-up both in Group A (3.4 ± 1.5 vs 2.6 ± 1.2, p = 0.011; 1.4 ± 0.9 vs 0.9 ± 1.2, p = 0.027; 3.1 ± 1.7 vs 1.5 ± 1.8, p < 0.001) and Group B (3.2 ± 1.3 vs 2.5 ± 1.6, p = 0.004; 1.5 ± 1.2 vs 1.0 ± 1.4, p = 0.018; 3.3 ± 1.4 vs 2.6 ± 1.2, p < 0.001), analyzed by post hoc paired t-tests. Moreover, the frequencies of AECOPD after one-year PR maintenance in Group A and Group B were both lower than Group C (2.6 ± 1.2, 2.5 ± 1.6 vs 3.5 ± 1.3, p < 0.05, respectively). Similarly, the numbers of hospitalization for AECOPD in Group A and Group B were lower than Group C (0.9 ± 1.2, 1.0 ± 1.4 vs 1.4 ± 0.9, p < 0.05, respectively). Finally, the ED visits after one-year observation in Group A were lower than Group B and Group C (1.5 ± 1.8 vs 2.6 ± 1.2, 3.1 ± 1.9, p < 0.05, respectively).
The Kaplan–Meier curves evaluating the time to first acute exacerbation of COPD during our follow-up are shown in Figure 2. In the univariate regression analysis, significant predictors of AECOPD were smoking status, exacerbation numbers in the prior year and PR (either home-based maintenance via social media or hospital-based maintenance) (Table 3). In multivariate analysis, PR is an independent predictor of lower risk for acute exacerbation of COPD in the one-year follow-up for home-based maintenance via social media (incidence rate ratio (IRR) 0.712, 95% CI 0.595–0.841; p < 0.001) and hospital-based maintenance (incidence rate ratio (IRR) 0.799, 95% CI 0.683–0.927; p = 0.002), respectively (Table 3).
 |
Table 3 Predictors of Acute Exacerbations of Chronic Obstructive Pulmonary Disease |
One-Year Follow-Up Maintenance
During one-year follow-up, the 6MWD in Group A and Group B increased over time from month 3 to month 12, compared to month 0 (p < 0.001). In contrast, the result of 6MWD in Group C showed a decreased trend from month 6, and it declined below the level of month 0 at the end of observation (p < 0.001). The between-group differences (F(2, 136)= 5.834, p = 0.025), the time effect (F(4, 544)= 178.872, p < 0.001) and the time*group interact effect of 6MWD (F(8, 544)= 88.957, p < 0.01) showed significance when analyzed by repeat-measure ANOVA (Figure 3A).
Compared to month 0, the mMRC scores in Group A showed significant decrease in month 3, and then increased gradually from month 6 to month 12, but was still lower than the level of month 0 (p < 0.05). Similarly, the trend of mMRC scores in Group B showed a decline from month 3 to the end without any increase (p < 0.05). To the contrary, in Group C, the mMRC scores decreased initially and increased over time to the end (p < 0.001). The between-group differences (F(2, 136)= 23.433, p < 0.001), the time effect (F(4, 544)= 57.976, p < 0.001) and the time*group interact effect (F(8, 544)= 52.25, p < 0.001) showed significance when analyzed by repeat-measure ANOVA (Figure 3B).
The scores of CAT in Group A and Group B showed a similar trend which decreased from month 3 to month 12 (p < 0.001), while after the initial smooth decrease by month 3, the scores of CAT in Group C increased from month 6 to the end of observation. The between-group differences, the time effect and the interact effect of CAT showed significance analyzed by repeat-measure ANOVA (F(2, 136)= 12.489, p = 0.014; F(4, 544)= 150.404, p < 0.001; F(8, 544)= 20.764, p < 0.001, respectively) (Figure 3C).
During maintenance observation, BDI (Figure 3D), SAI (Figure 3E) and TAI (Figure 3F) did not show significant between-group differences over time (p > 0.05). Similarly, neither time effect (p > 0.05) nor interact effect (p > 0.05) of BDI, SAI, or TAI showed significant difference when analyzed by repeat-measure ANOVA.
Discussion
The main finding of the present study was that the PR maintenance strategy (both home-based WeChat-supervised maintenance and hospital-based maintenance) could preserve, even extend the effect of initial PR benefits on the performance of exercise tolerance, HRQL. After one-year follow-up, the frequency of AECOPD, hospitalization due to AECOPD and ED visits all showed significant decline in patients with COPD applying PR maintenance in Groups A and B, compared to the non-maintenance group. Moreover, home-based PR maintenance was as effective as the hospital-based PR maintenance and superior to non-maintenance in reducing the acute exacerbation of COPD during long-term follow-up. Finally, PR maintenance was an independent predictor of decreased risk for acute exacerbation of COPD.
In a previous study, the improvements pulmonary rehabilitation provided to COPD patients was preserved for a short term, most of the PR gains diminished over time without any maintenance.28 In the present study, we reached a similar conclusion that the effect of the initial 8-week PR provided to the patients in Group C faded gradually during the one-year follow-up. By contrast, the PR maintenance which was provided in Group A and Group B preserved, even extended, part of the benefits of initial PR at the end of follow-up. Therefore, PR maintenance strategy was recommended in GOLD 2022 recently.2 With respect to the reduction of risk for acute exacerbation of COPD in our study, the patients in PR maintenance groups were at a lower risk of deterioration than the non-PR maintenance group. This result was consistent with previous randomized controlled trials (RCT) which applied the similar long-term PR maintenance strategy.29,30 Indeed, program components including the suitable intensity of exercise, integrated skill for recognition of exacerbation, encouragement and support from family or physicians, even the nutrition and medicine information were provided to patients regularly during the maintenance follow-up. As a result, these patients taking part in and completing the structured maintenance program will have more chance to alleviate symptoms as well as decrease the risk for deterioration of COPD, hospitalization and ED visits, compared to the usual care strategy. Therefore, these findings implied that the PR maintenance strategy should be continued to be offered to patients who have a higher risk of exacerbation and more symptom burden in daily lives following an initial PR program, and as an extension of pulmonary rehabilitation. Moreover, maintenance could not only provide potential sustaining clinical improvements but also reduce the substantial healthcare cost to society.
In the last decade, studies have demonstrated the efficacy and safety of the technology-based interventions in promoting the physical activity, improving HRQL, monitoring physiological signs and reducing acute exacerbation in COPD.31–33 With the rapid development of internet technology, smart devices, and social media, information communication via network is convenient and accurate. WeChat is the most popular social network platform in China.34 In recent years, the “Internet Medical” model covers the shortage of unbalanced distribution of medical resources around the world, such as Twitter and Facebook, have been steadily applied in medical education.35,36 Likewise, WeChat has been gradually used in medical education and the follow-up of patients in China, and it has reported benefits in clinic. The recent study indicated that WeChat app-based education and rehabilitation could reduce emotional dysfunction such as anxiety, depression and improve HRQLin non-small lung cancer patients undergoing surgery.19 Another recent clinical trial demonstrated that WeChat PR strategy provided a greater improvement in HRQL, lung function, and showed better adherence.37 In the current study, we applied WeChat PR maintenance strategy in Group A. The patient-physician communications in this remote model were accomplished via smartphone applications which provided all PR maintenance components to patients and gave feedback or suggestions by clinicians according to uploaded patients’ vital signs during exercise. As a consequence, the novel remote PR maintenance model has a similar effect on clinical improvements and reduction of risk for AECOPD to the hospital-based PR maintenance group. This conclusion may be useful to inform the decision-making on resource allocation.38
Despite the clear evidence of benefit of hospital-based PR on physical activity and HRQL, the insufficient funding, imbalance resource allocation, and distance obstacle made value of traditional PR limited.39 Recently, many more studies have focused on implementing behavior-targeted interventions to improve physical activity via technology and the internet,40–42 and demonstrated the positive effect on reducing on risk for AECOPD. A systematic review from Cochrane database also illustrated that social media intervention may be effective at improving physical activity and well-being, which included 88 studies (871378 participants).14 Therefore, this novel remote maintenance model might be used to deliver alternatives to conventional PR across wide geographical areas, especially during the COVID-19 pandemic.
Although the PR is recommended2 and well documented in high-income countries’ COPD guidelines,3,43 the PR services are not widely available in low-income and middle-income countries (LIMICs) where the prevalence of COPD is higher and evidence of benefit of PR is very small.44 Whether the PR as implemented in high-income countries is the suitable model for LIMICs is also a critical question. The present study, to our knowledge, is the first clinical trial in regard to the PR maintenance via social media supervision in north China. The positive result of this research provided more evidence of PR and maintenance strategy benefits and verified the feasibility of this model in the local region. So, there was an important implication that it is necessary to explore the different forms and culturally appropriate PR program in LIMICs.
Limitations
There are several limitations to this work. First, this study is not a blinded design. The patients were given general information about the allocation and related intervention even different medical resources. Second, although the convenient and clear, the CAT and emotional function assessments could not evaluate the patients’ HRQL comprehensively, compared to St George’s Respiratory Questionnaire (SGRQ). Third, the technology applications were not familiar to elder COPD patients with likely recognition dysfunction. This led to uploaded vital sign being incorrect and made communication ineffective between patients and clinicians. Future studies need to explore more convenient and effective methods with comprehensive evaluation for PR maintenance delivery.
Conclusion
The remote PR maintenance via WeChat is effective at reducing the risk for AECOPD and keeping the improvements in 6MWD, mMRC, and CAT from decline. The remote PR maintenance via WeChat might be used to deliver alternatives to conventional PR.
Data Sharing Statement
Individual participant data that underlie the results reported in this article (tables and figures) are available after deidentification for 36 months after publication from the corresponding author Yi Li on reasonable request, and researchers should provide a methodologically sound proposal.
Acknowledgment
The authors thank Dr. Jerry Liu for improving the use of English in the manuscript.
Funding
This study was supported by the grants from China Soong Ching Ling Foundation (No. 2018MZFZY-009) and Tianjin Key Medical Discipline (Specialty) Construction Project.
Disclosure
All authors declare no competing interests.
References
1. Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for causes in China during 1990–2013: a systematic subnationalanalysis for the Global Burden of Disease Study. Lancet. 2016;387(10015):251–272. doi:10.1016/S0140-6736(15)00551-6
2. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease Report: 2022. Available from: https://goldcopd.org/wp-content/uploads/2021/12/GOLD-REPORT-2022-v1.1-22Nov2021_WMV.pdf.
3. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi:10.1164/rccm.201309-1634ST
4. Spruit MA, Singh SJ. Maintenance programs after pulmonary rehabilitation: how may we advance this field? Chest. 2013;144(4):1091–1093. doi:10.1378/chest.13-0775
5. Güell MR, Cejudo P, Ortega F, et al. Benefits of long-term pulmonary rehabilitation maintenance program in patients with severe chronic obstructive pulmonary disease. Three-year follow-up. Am J Respir Crit Care Med. 2017;195(5):622–629. doi:10.1164/rccm.201603-0602OC
6. Li Y, Feng J, Li Y, et al. A new pulmonary rehabilitation maintenance strategy through home-visiting and phone contact in COPD. Patient Prefer Adherence. 2018;12:97–104. doi:10.2147/PPA.S150679
7. Sabit R, Griffiths TL, Watkins AJ, et al. Predictors of poor attendance at an outpatient pulmonary rehabilitation programme. Respir Med. 2008;102:819–824. doi:10.1016/j.rmed.2008.01.019
8. Wilson AM, Browne P, Olive S, et al. The effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomised controlled trial. BMJ Open. 2015;5:e005921. doi:10.1136/bmjopen-2014-005921
9. Maltais F, Bourbeau J, Shapira S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2008;149:869–878. doi:10.7326/0003-4819-149-12-200812160-00006
10. Rochester CL, Vogiatzis I, Holland AE, et al. An official American Thoracic Society/European Respiratory Society policy statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. 2015;192(11):1373–1386. doi:10.1164/rccm.201510-1966ST
11. Brennan D, Tindall L, Theodoros D, et al. A blueprint for telerehabilitation guidelines. Int J Telerehabil. 2010;2(2):31–34. doi:10.5195/ijt.2010.6063
12. Zanaboni P, Hoaas H, Aaroen Lien L, et al. Long-term exercise maintenance in COPD via telerehabilitation: batwo-year pilot study. J Telemed Telecare. 2017;23(1):74–82. doi:10.1177/1357633X15625545
13. Vasilopoulou M, Papaioannou AI, Kaltsakas G, et al. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur Respir J. 2017;49(5):1602129. doi:10.1183/13993003.02129-2016
14. Petkovic J, Duench S, Trawin J, et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst Rev. 2021;5(5):CD012932. doi:10.1002/14651858.CD012932.pub2
15. Malaguti C, Dal Corso S, Janjua S, et al. Supervised maintenance programmes following pulmonary rehabilitation compared to usual care for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2021;8(8):CD013569. doi:10.1002/14651858.CD013569.pub2
16. Hoaas H, Andreassen HK, Lien LA, et al. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: a mixed methods study. BMC Med Inform Decis Mak. 2016;16:26. doi:10.1186/s12911-016-0264-9
17. Lundell S, Holmner A, Rehn B, et al. Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Respir Med. 2015;109(1):11–26. doi:10.1016/j.rmed.2014.10.008
18. Chen J, Ho E, Jiang Y, et al. Mobile social network-based smoking cessation intervention for Chinese male smokers: pilot randomized controlled trial. JMIR MhealthUhealth. 2020;8(10):e17522. doi:10.2196/17522
19. Sui Y, Wang T, Wang X. The impact of WeChat app-based education and rehabilitation program on anxiety, depression, quality of life, loss of follow-up and survival in non-small cell lung cancer patients who underwent surgical resection. Eur J Oncol Nurs. 2020;45:101707. doi:10.1016/j.ejon.2019.101707
20. Schrijver J, Lenferink A, Brusse-Keizer M, et al. Self-management interventions for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2022;1(1):CD002990. doi:10.1002/14651858.CD002990.pub4
21. Qaseem A, Wilt TJ, Weinberger SE, et al.; American College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. doi:10.7326/0003-4819-155-3-201108020-00008
22. Gupta N, Pinto LM, Morogan A, et al. The COPD assessment test: a systematic review. Eur Respir J. 2014;44(4):873–884. doi:10.1183/09031936.00025214
23. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–586. doi:10.1378/chest.93.3.580
24. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(011):S467- S472. doi:10.1002/acr.20561
25. Monjazebi F, Dalvandi A, Ebadi A, et al. Functional status assessment of COPD based on ability to perform daily living activities: a systematic review of paper and pencil instruments. Glob J Health Sci. 2015;8(3):210–223. doi:10.5539/gjhs.v8n3p210
26. van Ranst D, Stoop WA, Meijer JW, et al. Reduction of exacerbation frequency in patients with COPD after participation in a comprehensive pulmonary rehabilitation program. Int J Chron Obstruct Pulmon Dis. 2014;9:1059–1067. doi:10.2147/COPD.S69574
27. Holland AE, Spruit MA, Troosters T, et al. An official European respiratory society/American thoracic society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. doi:10.1183/09031936.00150314
28. Ko FW, Dai DL, Ngai J, et al. Effect of early pulmonary rehabilitation on health care utilization and health status in patients hospitalized with acute exacerbations of COPD. Respirology. 2011;16(4):617–624. doi:10.1111/j.1440-1843.2010.01921.x
29. Guell R, Casan P, Belda J, et al. Long-term effects of outpatient rehabilitation of COPD: a randomized trial. Chest. 2000;117(4):976–983. doi:10.1378/chest.117.4.976
30. Rubi M, Renom F, Ramis F, et al. Effectiveness of pulmonary rehabilitation in reducing health resources use in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(3):364–368. doi:10.1016/j.apmr.2009.09.025
31. Voncken-Brewster V, Tange H, de Vries H, et al. A randomized controlled trial evaluating the effectiveness of a web-based, computer-tailored self-management intervention for people with or at risk for COPD. Int J Chronic Obstr Pulm Dis. 2015;1061–1073. doi:10.2147/COPD.S81295
32. Demeyer H, Louvaris Z, Frei A, et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: a multicentre randomised controlled trial. Thorax. 2017;72(5):415–423. doi:10.1136/thoraxjnl-2016-209026
33. Moy ML, Collins RJ, Martinez CH, et al. An internet-mediated pedometer-based program improves health-related quality-of-life domains and daily step counts in COPD: a randomized controlled trial. Chest. 2015;148(1):128–137. doi:10.1378/chest.14-1466
34. TechWeb. WeChat Chinese and International versions combined monthly active users over 1.2 billion, mini-programme daily users over 400 million; 2020. Available from: https://tech.sina.cn/2020-05-13/detail-iircuyvi2911382.d.html.
35. Admon AJ, Kaul V, Cribbs SK, et al. Twelve tips for developing and implementing a medical education Twitter chat. Med Teach. 2020;42(5):500–506. doi:10.1080/0142159X.2019.1598553
36. Junhasavasdikul D, Srisangkaew S, Sukhato K, et al. Cartoons on Facebook: a novel medical education tool. Med Educ. 2017;51(5):539–540. doi:10.1111/medu.13312
37. Bi J, Yang W, Hao P, et al. WeChat as a platform for baduanjin intervention in patients with stable chronic obstructive pulmonary disease in China: retrospective randomized controlled trial. JMIR MhealthUhealth. 2021;9(2):e23548. doi:10.2196/23548
38. Dakin H, Wordsworth S. Cost-minimisation analysis versus cost effectiveness analysis, revisited. Health Econ. 2013;22(1):22–34. doi:10.1002/hec.1812
39. Vogiatzis I, Rochester CL, Spruit MA, et al.; American Thoracic Society/European Respiratory Society Task Force on Policy in Pulmonary Rehabilitation. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016;47(5):1336–1341. doi:10.1183/13993003.02151-2015
40. Mantoani LC, Rubio N, McKinstry B, et al. Interventions to modify physical activity in patients with COPD: a systematic review. Eur Respir J. 2016;48(1):69–81. doi:10.1183/13993003.01744-2015
41. Robinson SA, Shimada SL, Quigley KS, et al. A web-based physical activity intervention benefits persons with low self-efficacy in COPD: results from a randomized controlled trial. J Behav Med. 2019;42(6):1082–1090. doi:10.1007/s10865-019-00042-3
42. Wan ES, Kantorowski A, Polak M, et al. Long-term effects of web-based pedometer-mediated intervention on COPD exacerbations. Respir Med. 2020;162:105878. doi:10.1016/j.rmed.2020.105878
43. Yang IA, Brown JL, George J, et al. COPD-X Australian and New Zealand guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2017 update. Med J Aust. 2017;207(10):436–442. doi:10.5694/mja17.00686
44. Jones R, Kirenga BJ, Katagira W, et al. A pre-post intervention study of pulmonary rehabilitation for adults with post-tuberculosis lung disease in Uganda. Int J Chron Obstruct Pulmon Dis. 2017;12:3533–3539. doi:10.2147/COPD.S146659
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


