Back to Journals » International Journal of General Medicine » Volume 15
The Influence of Living in Rural Areas on the Evolution and Management of Pediatric Ovarian Cystic Lesions: A Retrospective Study on a Cohort from South Eastern Romania
Authors Stefanopol IA , Baroiu L , Chirila S , Miulescu M , Anghel L , Nechita L, Dinu CA, Stefanescu V , Bobeica C , Nechifor A , Tatu AL
Received 1 April 2022
Accepted for publication 10 May 2022
Published 27 May 2022 Volume 2022:15 Pages 5273—5284
DOI https://doi.org/10.2147/IJGM.S368202
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ioana Anca Stefanopol,1,2,* Liliana Baroiu,3,4 Sergiu Chirila,5 Magdalena Miulescu,6,* Lucreţia Anghel,3,7 Luiza Nechita,3,* Ciprian Adrian Dinu,8,* Victorita Stefanescu,3 Carmen Bobeica,1,* Alexandru Nechifor,3,* Alin Laurenţiu Tatu3,9– 11
1Department of Morphological and Functional Sciences, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galati, Romania; 2Department of Pediatric Surgery and Orthopedy, “Sf Ioan” Clinical Emergency Hospital for Children, Galati, Romania; 3Clinical Medical Department, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galati, Romania; 4Infectious Diseases Department, “Sf. Cuvioasa Parascheva” Clinical Hospital of Infectious Diseases, Galati, Romania; 5Medical Informatics and Biostatistics, Faculty of Medicine, Ovidius University, Constanta, Romania; 6Research Center in the Functional Cardiorespiratory and Neuromotor Exploration, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galați, Romania; 7Internal Medicine Department, “sf Andrew the Apostle” County Emergency Clinical Hospital, Galati, Romania; 8Dental Department, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galati, Romania; 9Research Center in the Field of Medical and Pharmaceutical Sciences, Reform-UDJ, Galati, Romania; 10Dermatology Department, “Sf. Cuvioasa Parascheva” Clinical Hospital of Infectious Diseases, Galati, Romania; 11Multidisciplinary Integrated Center of Dermatological Interface Research MIC DIR, Galati, Romania
*These authors contributed equally to this work
Correspondence: Liliana Baroiu, Clinical Medical Department, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, 47 Domnească Street, Galati, 800010, Romania, Tel +40723201241, Email [email protected] Sergiu Chirila, Medical Informatics and Biostatistics, Faculty of Medicine, Ovidius University, 1 University Alee, Campus B, Constanta, 900470, Romania, Tel +407213320668, Email [email protected]
Background: The incidence of ovarian cystic lesions (OCLs) in pediatric patients has been increasing in recent years. An early diagnosis is mandatory for a favourable prognosis but it depends on the primary medical care services and on the socioeconomic status of the patient. The present study aims at assessing the prevalence and the age-specific frequencies of pediatric OCLs, as well as identifying disparities between subjects in the urban and the rural areas, in order to explore the extent to which OCLs occurrence, diagnosis, evolution and treatment differ in the case of patients living in rural areas.
Methods: A 3-year retrospective study was conducted between 2017 and 2019. All the female patients aged between 0 and 18 with OCLs ≥ 10 mm (N = 488), diagnosed and treated at “Sf.Ioan” Clinical Emergency Hospital for Children in Galaţi were included in the study. The Chi2 test was used for comparing the distributions of frequencies, and the t-Student test was used for comparing the means of any two normally distributed variables. The statistical significance threshold (p) was set at 0.05.
Results: The prevalence of OCLs ≥ 10 mm was 14.85%, 47.13% of the subjects originating in rural area (p = 0.62). Different from the urban areas, the rural ones are characterised by a lower proportion of patients with BMI ≥ 25 (p = 0.002), larger OCLs mean size (p = 0.278), a more frequent complex aspect on ultrasonography (p = 0.01), and a smaller number of general physician referrals (p = 0.005). Moreover, a higher proportion of rural patients were intraoperatively diagnosed with OCLs (p = 0.044), had complicated OCLs (p = 0.012) and had their OCLs surgically treated OCLs (p < 0.01).
Conclusion: Taking into consideration the socio-economic situation of south eastern Romania, patients living in rural areas have proven exposed to a higher risk of presenting with larger, complex and complicated OCLs, which most often require surgical treatment.
Keywords: ovarian cyst, rural population, incidence, body mass index, management, torsion
Introduction
The ovarian masses incidence is estimated to be around 2.6 in 100,000 girls under the age of 18, with 10% of malignancy.1,2 Ovarian cancer represents 1% of children malignancies,3–5 and less than 5% of the ovarian malignant tumors occur in pediatric ages.6,7 The accessibility and relatively low cost of an abdominopelvic ultrasonography (USG), as well as recent technological advances, has led to an increased rate of OCLs detection and diagnosis in pediatric patients.8 Histologically, OCLs may be non-neoplastic or functional cysts (follicular cyst, corpus luteum cyst) and benign cystic neoplasms (mature cystic teratoma, cystadenoma, endometrioma).9 Although the etiopathogenesis is still unclear, numerous authors consider that there exists a relationship between the occurrence of functional cysts in pediatric patients and an improper functioning of the immature hypothalamic-pituitary-ovarian axis (HPOA).10–13 Recent studies have focused on the correlation between obesity and anovulatory cycles, with consequences on infertility and ovarian cysts occurrence, but further research is required.14–16 Occasionally, but not as often as in the case of polycystic ovary syndrome may coexist cutaneous pathologies such as acne, diffuse alopecia or hypertrichosis, and also, some cases of teratoma may associate with other genetically determined skin conditions.17–19
Considering the unspecific clinical features,20–22 an accurate diagnosis requires imaging tools. USG is the method of choice and it also allows monitoring the evolution of OCLs.23,24 90% of OCLs evolves to spontaneous resolution, thus their treatment should be conservative in order to ensure the patient’s normal sexual development and fertility.25–27 Surgical treatment remains indicated only for large or complicated OCLs or for malignant ovarian masses.28–31 Even in these cases efforts must be made to preserve the ovary.32–34 The most common complications of OCLs are ovarian torsion and cyst rupture, both occurring more frequently in lesions larger than 50 mm.35 Consequently, early identification of patients with OCLs is of paramount importance in preventing the progression and reducing the risk of complications.
The aim of this study was to assess the pediatric OCLs prevalence as well as the age-specific rates of occurrence, to identify disparities between urban and rural subjects, and to explore the influence of the living environment, in our case the rural one, on the occurrence, diagnosis, evolution and treatment of OCLs.
Materials and Methods
This is a retrospective observational analytical study including 488 female patients from neonates to the age of 18, with OCLs ≥ 10 mm, diagnosed and treated at “Sf. Ioan” Clinical Emergency Hospital for Children in Galaţi over a 3-year period, from January 2017 to December 2019. Written informed consent was obtained from the patients’ parents or legal representatives before publication, and procedures were in accordance with the Helsinki declaration. The present study received ethical approval from the Bioethics Commission of “Sf.Ioan” Clinical Emergency Hospital for Children, Galaţi.
OCLs were found on abdominopelvic USG or incidentally during abdominal surgery. The patients were from Galaţi county and from the neighbouring counties; they presented to our hospital either to the emergency care unit (ECU) or referred from the GPs to the outpatient clinics. The database includes information collected from our institutional records: patients’ medical charts, clinical and imaging records and operating registries, archived either electronically (“Atlas” soft) or on paper. Patients with ovarian malignant neoplasms (which are predominantly solid structures), polycystic ovary syndrome, paraovarian cysts, and torsion of an otherwise healthy ovary were excluded from the study.
The selection of the 488 patients included in the study group implied an initial data collection performed by analysing the electronic files from the radiology department and the medical charts from the pediatric surgery department. A total of 3284 consecutive female pediatric patients were selected in the initial stage who had been evaluated for abdominal or pelvic pain with both ovaries documented on abdominopelvic USG (excluding check-ups). A total of 2827 patients with ovarian cysts smaller than 10 mm or fulfilling one of the exclusion criteria were eliminated in the second stage of the study. Finally, a subgroup of 31 patients with intraoperatively discovered OCLs was added, thus obtaining the final study group of 488 patients. The study group was divided into two groups: 230 rural patients and 258 urban patients, which were comparatively analyzed (Figure 1).
 |
Figure 1 Flowchart of the patients’ inclusion. Abbreviations: USG, ultrasonography; OCLs, ovarian cystic lesions. |
The value of 10 mm was chosen as the cut-off limit for OCLs sizes. A cystic ovarian structure smaller than 10 mm represents a stage in the normal development of the ovarian follicles,36 and its visualisation in premenarcheal ages is considered to be physiological. According to the study conducted by Pienkowski et al, any lesion larger than 20 mm is considered to be an ovarian cyst in premenarcheal girls.12 Nevertheless, other studies state that OCLs < 20 mm in premenarcheal girls may be mature cystic teratoma or estrogen secreting follicular cysts (causing early puberty).8,13,21 OCLs were classified according to their size and aspect on USG. For the OCLs size, the greatest diameter among the 3 parameters (length, width, thickness) was selected. For bilateral OCLs the features of the largest cyst were taken into consideration. OCLs were further divided into small (10–29 mm), medium (30–49 mm), and large (≥50 mm). Anechoic, unilocular thin-walled OCLs were defined as having simple aspect. Complex OCLs were defined as multilocular, thick-walled, with a solid component, with/or without septa, with/or without internal echoes.
The patients were divided into 3 BMI groups: BMI < 18.5 (underweight), BMI = 18.5–24.9 (normal weight) and BMI ≥ 25 (overweight and obesity).
Statistical Analysis
This study was conducted according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement.
The data were systematized and centralized in an SPSS 24.0 (IBM Statistical Package for the Social Sciences, Chicago, Illinois) database and processed by using the appropriate statistical functions. A 95% confidence interval (95% CI) was used in data presentation.
Primary indicators (minimum, maximum, frequency), mean value indicators (mean, median), and dispersion indicators (standard deviation, standard error, confidence interval for the mean) were used for descriptive statistical analysis. The Skewness test (−2 < p < 2) was used to validate the normality of the data distribution for the analyzed continuous variables. Qualitative significance tests, such as the Chi2 test were used for comparing the distributions of frequencies. The relative risk (RR) was used to measure the association between the exposure and the outcome. The Kruskal–Wallis test, a nonparametric test, was used for intergroup comparison of 3 or more frequency distributions; the correlations between different phenomena were identified by using the Pearson correlation coefficient. The t-Student test was used for comparing the means of any two normally distributed variables. The multiple linear regression was used to analyze the correlation between the occurrence of large OCLs (as dependent variable) and a few independent variables, in order to find the best predictor factors. We used the risk ratio, also called relative risk (RR), to compare the risk of a health event (OCLs occurrence, complications, surgery, etc) for the two studied groups (rural, urban). We calculated the RR by dividing the risk (incidence proportion, attack rate) in group 1 by the risk (incidence proportion, attack rate) in group 2. If the RR is 1 (or close to 1), it suggests no difference or little difference in risk (incidence in each group is the same). RR > 1 suggests an increased risk of that outcome in the exposed group, while RR < 1 suggests a reduced risk in the exposed group.
The statistical significance threshold (p) was set at 0.05.
Results
During the 3 year study, 488 girls out of 3284 were identified with OCLs ≥ 10 mm, which means a 14.85% prevalence among pediatric female patients investigated for abdominal or pelvic pain. The age at menarche was documented for all the patients and the mean value was 11.8 years (extremes: 7 and 15 years). Age-specific frequencies for OCLs varies between 0% and 25.81%. For the patients aged under 12 (premenarcheal), the peak frequency was 13.9% at 11 years, while the maximum value (25.81%) was in the post-menarcheal girls, at the age of 15 (Table 1).
 |
Table 1 Age-Specific Frequencies of OCLs ≥ 10 mm |
The mean age of the 488 subjects in the study group at presentation was 14.11 ± 3.173 (mean ± standard deviation), the highest prevalence being in the 15 year-old patients with a rate of 19.26% (Figure 2).
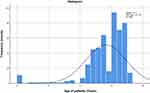 |
Figure 2 Age distribution histogram for the study group. |
OCLs distribution according to the patients’ area of origin is relatively homogeneous, with 258 (52.87%) girls from the urban area and 230 (47.13%) from rural one (p = 0.62, according to the Chi2 test). There were no statistically significant differences regarding the mean age of the patients at presentation, and the mean age at menarche (Table 2) The age at which the OCLs frequency reached the maximum values was 17 for the urban girls and 15 for the rural ones (p = 0.654) (Figure 3).
 |
Table 2 Comparative analysis of the mean values for some variables according to the patients'area of origin |
 |
Figure 3 The distribution of the patients’ ages according to the area of origin. |
BMI series of values were homogenous in both area of origin and the Skewness Test validated the normality of data, with variations between 11.80 and 40.04 kg/m2 in patients from rural areas, and between 10.29 and 37.22 kg/m2 in patients from urban areas. For the urban patients the mean values of BMI showed significantly higher values (22.30 versus 21.21 kg/m2; p = 0.003) (Table 2). Moreover, 24% of the urban girls had BMI ≥ 25 as compared to 13% of the rural patients (p = 0.002) (Table 3).
 |
Table 3 Comparative Analysis of the Main Variables According to the Patients’ Area of Origin |
The series of values for OCLs sizes were homogenous for the patients in both areas of origin. The Skewness Test validated the normality of data, varying between 10 mm and 154 mm in the rural patients, and between 10 mm nd 80 mm in the urban ones. In the rural areas, the OCLs mean size had statistically significant higher value (33.41 ± 17.25 mm versus 30.56 ± 14.24 mm; p = 0.046) (Table 2). The OCLs distribution by size categories showed that the percentage of large OCLs (≥50 mm) is 14.3% in the case of the patients originating in rural areas as compared to 10.5% in the case of those originating in urban ones (p = 0.278) (Table 3). The multivariate linear regression analysis pointed out that the rural environment, older age, and higher BMI are predictors of the larger sized OCLs (p = 0.001): Y = 29.059–2.879 area + 0.407 age + 0.068 BMI (Model 3) (Table 4).
 |
Table 4 Multivariate Analysis. Dependent Variable: OCLs. Predictors: Area, Age, BMI and Presence of Complications |
19.05% (N = 93) of the OCLs included in the study had a complex aspect on USG. The division by area of origin showed that 23.9% (N = 55) of the 230 rural girls had complex OCLs as compared to 14.7% (N = 38) of the 258 urban girls (p = 0.01) (Table 3). Patients originating in rural areas face a higher risk of complex lesions, both for small OCLs of 10–29 mm (RR = 1.43 [0.82–2.49], p = 0.291) and for medium OCLs of 30–49 mm (RR = 1.16 [0.87–1.60], p = 0.381), but the results cannot be extrapolated to the general population. The highest percentage of complex ultrasonographic aspect was observed in rural girls with large OCLs (72.7% of large OCLs were complex, p = 0.05) (Table 5).
 |
Table 5 Distribution of Patients According to OCLs Size and Aspect on USG |
The 488 patients participating in this study group requested medical examination either directly in the ECU (N = 328; 76.4%) or in the ambulatory care units based on a medical referral from the GPs (N = 115; 23.6%) (Table 3). The fact could be noticed that only 17.8% (N = 41) of the patients from the rural environment and 28.7% (N = 74) of the patients from the urban area were referred by GPs (p = 0.005).
There were two ways to diagnose OCLs (2 moduri de a diagnostica OCL): intraoperatively (N = 31; 6.4%), or during an abdominopelvic ultrasound examination (N = 457; 93.6%) (Table 3). The patients from the rural areas were diagnosed intraoperatively twice more often (8.7% versus 4.3%; p = 0.044).
In our study group 5.5% (N = 27) of the OCLs were complicated, with a statistically significant higher proportion of patients from the rural environment (8.3%) as compared to those from the urban one (3.1%) (p = 0.012). The complication was either rupture (N = 17) or torsion (N = 10). The fact was noticed that, regardless the complication type, these were more common for the rural patients: 70.5% (N = 12) of the ruptures and 70% (N = 7) of the torsions (p = 0.974) (Table 3).
Regarding the treatment, 40 OCLs (8.2% of the total) were treated surgically. Thirty of these (75%) being treated in rural patients (p = 0.001). There were two types of surgical interventions: elective (N = 17, 42.5%) and emergency (N = 23, 57.5%). 60% of the patients coming from rural areas had an emergency operation as compared to 50% of the urban area patients. Nevertheless, the difference was not statistically significant (p = 0.67).
Discussion
The incidence of OCLs in the entire spectrum of pediatric ages is not known with certainty. There are few studies covering the entire spectrum of pediatric ages,21,26,37,38 or performed on groups larger than 200 patients.4,7,9,20,22,39,40 In addition, OCLs studies are conducted by physicians with different specialties, which means that patients were selected according to the specifics of the department. Thus, epidemiological studies are difficult to carry out. Moreover, most studies were performed on inpatients. By comparison, the present study includes also outpatients, who were diagnosed and treated either in ambulatory clinics or in the ECU.
The present research, performed over a period of 3 years, found a 14.85% prevalence of OCL ≥ 10 mm with a frequency peak in the case of 15 year-old patients (19.26%). The mean age at presentation was 14.11 ± 3.17 years. Age-specific frequencies showed that the prevalence is higher in the perimenarcheal period, raising to the age of 11 (13.9%) and reaching its maximum value at the age of 15 (25.81%). These results are consistent with the findings of other studies. The study conducted by Emeksiz et al, similar to the present research regarding the distribution by patients age and OCL sizes, found a frequency of 13.1%, with a peak at the age of 15, as well.8
In Romania 43.6% of the entire population lives in rural areas, while in other European Union countries the standard is 25%. Depending on the symptoms and the patient’s age, the initial medical examination may be performed by general physicians (GPs), but also by pediatricians, endocrinologists, gynecologists or surgeons. GPs are the first point of contact for a person with a health concern regardless of age, gender, race or pathology. They may provide consultation and treatment, or referral as appropriate. According to Eurostat, the average number of primary care physicians is 60–120 per 100,000 inhabitants in European Union countries (42 in Greece and 253 in Portugal). In Romania, the average is 77.2, which means 1 general physician for 1300 residents.41 According to the Romanian National Institute of Statistics, there are over 6500 family medicine practices in urban areas and only 4400 in rural ones. Moreover, there are 11,500 specialized medical offices (USG, gynecology, pediatrics, etc.) in urban areas as compared to only 494 in rural ones (23 times less).42 In addition, the incidence of poverty in Romania is 34% higher in the rural areas than in urban ones, as compared to only 5% in Germany, and the degree of participation in the educational process is 4.5 times lower in rural areas.43 Corroborating these facts as regards our country, the rural population does not always have access to medical services for various reasons: a small number of GPs and medical care units, specialized clinics situated far away from the place of residence, travel costs and means of transport.44
Although the percentage of girls aged between 0 and 18 who live in urban settlements is slightly lower (49.9%) in Galaţi county, a higher proportion of OCLs was found in our urban group as compared to the rural one (52.87% vs 47.13%; p = 0.62). There were no significant differences between the two subgroups in terms of the patients’ age at presentation (p = 0.654), of their age of menarche (p = 0.922) and of the age at which the OCLs frequency reached the maximum values (p = 0.654). The fact that OCLs are more frequent in urban girls might be explained by the easier access of the urban population to a physician and to imaging diagnosis methods. An interesting hypothesis, based on the relationship between obesity and ovarian cysts occurrence, is the influence of environmental and dietary factors. In rural areas people have farms and gardens where they cultivate fruit and vegetables,44 so their diet is healthier (no fast or junkfood) and their lifestyle is more active, which may lead to a lower incidence of overweight and obesity. Our study found significantly higher mean values of BMI for the urban patients (p = 0.003). Similar BMI differences between rural and urban pediatric population were demonstrated in a study carried out in another county from south-eastern Romania.45 For urban settlements a higher percentage of patients with BMI ≥ 25 was identified, the obesity risk being 1.36 higher (RR = 1.36 [1.14–1.62], p = 0.002).
Out of the 488 patients included in the present study, only 115 were initially consulted by a GP and only 35.6% of them were from the rural area. Regarding the OCLs diagnosis, there was a slightly higher number of urban patients diagnosed by USG (247 versus 210), but a statistically significant higher number of rural patients diagnosed intraoperatively (20 versus 11). The statistical analysis has shown that girls living in rural areas have a higher risk to present at the hospital without a referral from GPs (RR = 1.42 [1.09–1.85], p = 0.005), and also to receive an accurate diagnosis during surgery (RR = 1.52 [0.94–2.47], p = 0.044).
The mean size of the OCLs in the case of rural patients was significantly higher (p = 0.046), but, analysing each of the three categories of OCLs in terms of their dimensions, the fact could be noticed that there were no significant differences (p = 0.278). However, the multiple linear regression identified the rural areas, the age and BMI as positive predictive factors for large OCLs.
The complexity of OCLs according to the patients’ area of origin showed that rural patients have a higher risk of presenting with complex lesions (RR = 1.34 [1.09–1.63], p = 0.01). The fact could also be noticed that the bigger the OCLs, the more numerous the cases of complex lesions, irrespective of the patients’ area of origin. Nevertheless, ignoring the dimensions of OCLs, more rural patients have complex OCLs as compared to urban ones, but this difference is statistically relevant for complex OCLs ≥ 50 mm (RR = 1.66 [0.94–2.91], p = 0.05).
Starting from the fact that the risk of complications and the need for surgical treatment increase for OCLs ≥ 50 mm, the present study highlighted that, although there are no significant differences in the distribution of large OCLs for the urban and rural patients, the incidence of complicated OCLs was significantly higher in the rural population (RR = 1.83 [1.02–3.29], p = 0.012). Moreover, 70.5% of the ruptures and 70% of the torsions occurred in rural patients; despite these quantitative differences there were no statistically significant differences (p = 0.974), the proportion of the complication type according to the patients’ area of origin having fairly similar percentages.
For the patients included in the study, the treatment of choice was conservative (91.8%). 75% of the 40 surgical interventions being performed in patients from the rural area (RR = 1.68 [1.37–2.07], p = 0.001). Despite the fact that 72.8% of the emergency operations were performed for rural residents there was not a statistically significant difference. In pediatric patients the anesthesiologists prefer the preoperative Dexamethasone administration for the vomiting prophylaxis,46 and the sevoflurane for induction.47 They must also be cautious when administrating neuromuscular blocking agents because they may cause allergic reactions.48 Special attention must be paid, as well, to the impact of the postanesthetic systemic inflammation on the liver function.49
It is obvious that there are important differences between urban and rural areas regarding the incidence, diagnosis, evolution and treatment of OCLs in pediatric patients, with a negative impact in the rural population. This is a consequence of multiple factors. First of all, the small number of GPs in the rural areas (the same physician providing medical assistance for several settlements), and the lack of specialized clinics or offices to assure a proper imaging examination or check-ups for patients with abdomino-pelvic pathology. Secondly, the unlikeliness of early diagnosis and of regular medical screening, considering the low level of health education and the living standards of numerous rural patients.
The present study has some limitations. Given its retrospective nature, there were not sufficient data about the environmental, socio-economic and dietary factors characterising the patients. Thus, the relationship between obesity and pediatric OCLs requires further investigations and constitutes the starting point for a future research. The study involved a single center, so the results cannot be generalized. In addition, the imaging examinations were not performed by the same radiologist. Despite all these limitations, the present study is, to our knowledge, the first devoted to this topic in the field of pediatric OCLs and brings to the fore the importance of primary medical assistance in early diagnosis.
Conclusions
This study was conducted on a relatively large cohort of girls from south-eastern Romania. The prevalence of OCLs ≥ 10 mm was 14.85%, with a relatively homogeneous distribution according to the patients’ area of origin, but with significantly higher mean values of BMI for the urban patients, strengthening the hypothesis of a relationship between obesity and OCLs. In accordance with the socio-economic reality of our region, patients living in rural areas have proven to face a higher risk of presenting with larger, complex and complicated OCLs, which require surgical treatment more frequently. In order to optimize the therapeutic results, we emphasize the fundamental role of the GP in increasing the level of food and health education of the population, in including ovarian pathology in the differential diagnosis of painful abdomen in pediatric patients, and in using the abdominopelvic USG as a mandatory method of first intention in OCLs screening.
Abbreviations
OCLs, ovarian cystic lesions; GPs, general physicians; HPOA, hypothalamic-pituitary-ovarian axis; USG, ultrasonography; RR, relative risk; CI, confidence interval; BMI, body mass index; ECU, emergency care unit.
Data Sharing Statement
The datasets are available from Dr Liliana Baroiu on reasonable request.
Ethics Approval and Informed Consent
The ethics approval was obtained from the Ethics Commission of “Sf. Ioan” Clinical Emergency Hospital for Children, Galaţi, Romania (approval no 4725/March 17, 2020).
Consent for Publication
Written informed consent was obtained from the patients’ parents or legal representatives prior to publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Acknowledgments
The authors wish to acknowledge that the present study was academically supported by “Dunărea de Jos” University of Galaţi, Romania through the Research Center “Multidisciplinary Integrated Center of Dermatological Interface Research” (MIC-DIR).
The linguistic review of the present article was made by Antoanela Marta Mardar, member of the Research Center “Interface Research of the Original and Translated Text. Cognitive and Communicative Dimensions of the Message”, Faculty of Letters, “Dunărea de Jos” University of Galați, Romania.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
The APC for the present study was supported by “Dunărea de Jos” University of Galaţi, Romania.
Disclosure
The authors declare that they have no financial competing interests.
References
1. Eskander RN, Bristow RE, Saenz NC, Saenz CC. A Retrospective Review of the Effect of Surgeon Specialty on the Management of 190 Benign and Malignant Pediatric and Adolescent Adnexal Masses. J Pediatr Adolesc Gynecol. 2011;24(5):282–285. doi:10.1016/j.jpag.2011.03.012
2. Berger-Chen S, Herzog TJ, Lewin SN, et al. Access to conservative surgical therapy for adolescents with benign ovarian masses. Obstet Gynecol. 2012;119(2 Pt 1):270–275. doi:10.1097/AOG.0b013e318242637a
3. Sonmez K, Turkyilmaz Z, Karabulut R, Can Basaklar A. Ovarian masses in infant-juvenile age. Arch Argent Pediatr. 2018;116(3):359–364. doi:10.5546/aap.2018.eng.359
4. Oltmann SC, Garcia N, Barber R, Huang R, Hicks B, Fischer A. Can we preoperatively risk stratify ovarian masses for malignancy? J Pediatr Surg. 2010;45(1):130–134. doi:10.1016/j.jpedsurg.2009.10.022
5. Gupta B, Guleria K, Suneja A, Vaid NB, Rajaram S, Wadhwa N. Adolescent ovarian masses: a retrospective analysis. J Obstet Gynaecol. 2016;36(4):515–517. doi:10.3109/01443615.2015.1103721
6. Zolton JR, Maseelall PB. Evaluation of ovarian cysts in adolescents. Open J Obstet Gynecol. 2013;3(07):12–16. doi:10.4236/ojog.2013.37A1004
7. Zhang M, Jiang W, Li G, Xu C. Ovarian masses in children and adolescents - An analysis of 521 clinical cases. J Pediatr Adolesc Gynecol. 2014;27(3):73–77. doi:10.1016/j.jpag.2013.07.007
8. Emeksiz HC, Derinöz O, Akkoyun EB, Güçlü Pınarlı F, Bideci A. Age-specific frequencies and characteristics of ovarian cysts in children and adolescents. J Clin Res Pediatr Endocrinol. 2017;9(1):58–62. doi:10.4274/jcrpe.3781
9. Liu H, Wang X, Lu D, Liu Z, Shi G. Ovarian masses in children and adolescents in China: analysis of 203 cases. J Ovarian Res. 2013;6(1):47. doi:10.1186/1757-2215-6-47
10. Brandt ML, Helmrath MA. Ovarian cysts in infants and children. Semin Pediatr Surg. 2005;14(2):78–85. doi:10.1053/j.sempedsurg.2005.01.002
11. Spinelli C, Di Giacomo M, Cei M, Mucci N. Functional ovarian lesions in children and adolescents: when to remove them. Gynecol Endocrinol. 2009;25(5):294–298. doi:10.1080/09513590802530932
12. Pienkowski C, Cartault A, Carfagna L, et al. Ovarian cysts in prepubertal girls. Endocr Dev. 2012;22:101–111.
13. Ki EY, Byun SW, Choi YJ, Lee KH, Park JP, Lee SJ. Clinicopathologic review of ovarian masses in Korean premenarchal girls. Int J Med Sci. 2013;10(8):1061–1067. doi:10.7150/ijms.6216
14. Silvestris E, de Pergola G, Rosania R, Loverro G. Obesity as disruptor of the female fertility. Reprod Biol Endocrinol. 2018;16(1):22. doi:10.1186/s12958-018-0336-z
15. Roberts JA, Carpenter RM, Blythe SN, Toporikova N. FSH/AMH ratio and adipocyte size are linked to ovarian dysfunction. Endocr Res. 2020;45(3):174–189. doi:10.1080/07435800.2020.1721015
16. Goldsammler M, Merhi Z, Buyuk E. Role of hormonal and inflammatory alterations in obesity-related reproductive dysfunction at the level of the hypothalamic-pituitary-ovarian axis. Reprod Biol Endocrinol. 2018;16(1):45. doi:10.1186/s12958-018-0366-6
17. Tatu AL, Ionescu MA. Multiple autoimmune syndrome type III- thyroiditis, vitiligo and alopecia areata. Acta Endo. 2017;13(1):124–125. doi:10.4183/aeb.2017.124
18. Clatici VC, Georgescu O, Draganita AMV, Tatu AL, Fica S. Milk and Insulin Growth Factor 1 (IGF1) – implication in acne and general health. Rom Biotech Lett. 2015;20(1):10013–10025.
19. Tatu AL. Umbilicated blue black lesion on the lateral thorax. J Cutan Med Surg. 2017;21(3):252. doi:10.1177/1203475417694859
20. Ryoo U, Lee D-Y, Bae D-S, Yoon B-K, Choi DS. Clinical characteristics of adnexal masses in Korean children and adolescents: retrospective analysis of 409 cases. J Minim Invasive Gynecol. 2010;17(2):209–213. doi:10.1016/j.jmig.2009.12.013
21. Aydin BK, Saka N, Bas F, et al. Evaluation, treatment and follow-up results of ovarian cysts in childhood and adolescence: a multicenter, retrospective study of 100 patients. J Pediatr Adolesc Gynecol. 2017;30(4):449–455. doi:10.1016/j.jpag.2017.01.011
22. Rathore R, Sharma S, Arora D. Spectrum of childhood and adolescent ovarian tumors in India: 25 years experience at a single institution. Open Access Maced J Med Sci. 2016;4(4):551–555. doi:10.3889/oamjms.2016.090
23. Gilligan LA, Trout AT, Schuster JG, et al. Normative values for ultrasound measurements of the female pelvic organs throughout childhood and adolescence. Pediatr Radiol. 2019;49(8):1042–1050. doi:10.1007/s00247-019-04419-z
24. Back SJ, Maya CL, Zewdneh D, Epelman M. Emergent ultrasound evaluation of the pediatric female pelvis. Pediatr Radiol. 2017;47(9):1134–1143. doi:10.1007/s00247-017-3843-8
25. Qazi SH, Jeelani SM, Dogar SA, Das JK, Saxena AK. Approaches to the management of pediatric ovarian masses in the 21st century: systematic review and meta-analysis. J Pediatr Surg. 2020;55(3):357–368. doi:10.1016/j.jpedsurg.2019.09.003
26. Abbas PI, Dietrich JE, Francis JA, Brandt ML, Cass DL, Lopez ME. Ovarian-sparing surgery in pediatric benign ovarian tumors. J Pediatr Adolesc Gynecol. 2016;29(5):506–510. doi:10.1016/j.jpag.2016.03.009
27. Bergeron LM, Bishop KC, Hoefgen HR, et al. Surgical management of benign adnexal masses in the pediatric/adolescent population: an 11-year review. J Pediatr Adolesc Gynecol. 2017;30(1):123–127. doi:10.1016/j.jpag.2016.09.002
28. Ritchie J, O’Mahony F, Garden A. Guideline for the management of ovarian cysts in children and adolescents. BritSPAG. 2018;11:1
29. Dural O, Yasa C, Bastu E, et al. Laparoscopic outcomes of adnexal surgery in older children and adolescents. J Pediatr Adolesc Gynecol. 2016;29(2):182–183.
30. Rieger MM, Santos XM, Sangi-Haghpeykar H, Bercaw JL, Dietrich JE. Laparoscopic outcomes for pelvic pathology in children and adolescents among patients presenting to the pediatric and adolescent gynecology service. J Pediatr Adolesc Gynecol. 2015;28(3):157–162. doi:10.1016/j.jpag.2014.06.008
31. Stefanopol IA, Baroiu L, Constantin GB, et al. Diagnostic and management of undescended ovary - a preoperative dilemma: a case-based systematic review. Int J Womens Health. 2022;14:15–27. doi:10.2147/IJWH.S345742
32. Braungart S, Craigie RJ, Losty PD. Controversies in the management of ovarian tumours in prepubertal children - a BAPS and UK CCLG surgeons cancer group national survey. J Pediatr Surg. 2018;53(11):2231–2234. doi:10.1016/j.jpedsurg.2017.11.068
33. Tessiatore P, Guanà R, Mussa A, et al. When to operate on ovarian cysts in children ? J Pediatr Endocrinol Metab. 2012;25(5–6):427–433. doi:10.1515/jpem-2012-0049
34. Trotman GE, Cheung H, Tefera EA, Darolia R, Gomez-Lobo V. Rate of oophorectomy for benign indications in a children’s hospital: influence of a gynecologist. J Pediatr Adolesc Gynecol. 2017;30(2):234–238. doi:10.1016/j.jpag.2016.10.008
35. Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Cannot exclude torsion-a 15-year review. J Pediatr Surg. 2009;44(6):1212–1216. doi:10.1016/j.jpedsurg.2009.02.028
36. Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US:Society of Radiologists in Ultrasound consensus conference statement. Ultrasound Q. 2010;26(3):121–131. doi:10.1097/RUQ.0b013e3181f09099
37. Łuczak J, Bagłaj M. Selecting treatment method for ovarian masses in children – 24 years of experience. J Ovarian Res. 2017;10(1):59. doi:10.1186/s13048-017-0353-0
38. Kirkham Y, Lacy J, Kives S, Allen L. Characteristics and management of adnexal masses in a Canadian pediatric and adolescent population. J Obstet Gynaecol Can. 2011;33(9):935–943. doi:10.1016/S1701-2163(16)35019-8
39. Cribb B, Vishwanath N, Upadhyay V. Paediatric ovarian lesions - The experience at Starship Children’s Hospital, New Zealand. New Z Med J. 2014;127(1395):41–51.
40. Michelotti B, Segura BJ, Sau I, Perez-Bertolez S, Prince JM, Kane TD. Surgical management of ovarian disease in infants, children, and adolescents: a 15-year review. J Laparoendosc Adv Surg Tech. 2010;20(3):261–264. doi:10.1089/lap.2009.0137
41. Family physicians, underrepresented in Romania, among all medical specialities (article written in Romanian). Available from: https://rohealthreview.ro/medicii-de-familie-subreprezentati-in-romania-in-totalul-specialistilor/.
42. NIS: the number of doctors has increased with 2700 in 2019 (article written in Romanian). Available from: https://www.viata-medicala.ro/stiri/ins-numarul-medicilor-a-crescut-cu-2700-in-anul-2019-18382.
43. Paradox - Living standards in predominantly urban regions from Romania, above the EU average. Explanation (article written in Romanian). Available from: https://cursdeguvernare.ro/paradox-nivelul-de-trai-din-regiunile-predominant-urbane-ale-romaniei-peste-media-ue-explicatia.html.
44. Moldoveanu R, Rădoi SA, Pisică S. Some socio-economic features of the rural environment–landmarks for rural development (article written in Romanian). Romanian Stat Rev Suppl. 2015;63(12):17–25.
45. Chirilă S, Hangan LT, Broască V, Severin B, Mocanu E. Difference of height, body mass index and self-assessment among high-school students in Constanta County- A comparison between rural and urban areas. ARS Medica Tomitana. 2015;20(3):144–149. doi:10.2478/arsm-2014-0026
46. Ciobotaru OR, Lupu MN, Rebegea L, et al. Dexamethasone- Chemical structure and mechanisms of action in prophylaxis of postoperative side effects. Rev Chim. 2019;70(3):843–847. doi:10.37358/RC.19.3.7017
47. Stefanopol IA, Miulescu M, Baroiu L, Anghele A-D, Danila DM, Tiron Z. An unusual case of Meckel diverticulitis misdiagnosed as an infected urachal cyst. Medicina. 2021;57(5):495. doi:10.3390/medicina57050495
48. Ciobotaru OR, Stoleriu G, Ciobotaru OC, et al. Postanesthetic skin erythema due to succinylcholine versus atracurium. Exp Ther Med. 2020;20(3):2368–2372.
49. Baroiu L, Dumitru C, Iancu A, et al. COVID-19 impact on the liver. World J Clin Cases. 2021;9(16):3814–3825. doi:10.12998/wjcc.v9.i16.3814
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
