Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
The influence of disease severity and lifestyle factors on the peak annual 25(OH)D value of COPD patients
Authors Kentson M, Leanderson P, Jacobson P, Persson HL
Received 5 November 2017
Accepted for publication 9 February 2018
Published 27 April 2018 Volume 2018:13 Pages 1389—1398
DOI https://doi.org/10.2147/COPD.S156121
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Magnus Kentson,1,2 Per Leanderson,3 Petra Jacobson,4,5 Hans Lennart Persson4,5
1Division of Medicine, Ryhov Hospital, Jönköping, Sweden; 2Department of Medical and Health Sciences (IMH), Linköping University, Linköping, Sweden; 3Department of Occupational and Environmental Medicine, Department of Clinical and Experimental Medicine (IKE), Linköping University, Linköping, Sweden; 4Department of Respiratory Medicine, 5Department of Medical and Health Sciences (IMH), Linköping University, Linköping, Sweden
Background: The prevalence of individuals deficient in vitamin D (defined as a serum level of the stable metabolite 25(OH)D <50 nmol/L) is increasing in countries with low annual ultraviolet (UV) radiation and among individuals unable to perform outdoor activities, for example, COPD patients.
Objective: To assess the role of vitamin D deficiency, independently of seasonal variation, the peak annual value of 25(OH)D was measured in subjects with advanced COPD ± long-term oxygen therapy (LTOT) and lung healthy control subjects. A method to grade the individual annual UV light exposure was designed and tested.
Subjects and methods: Sixty-six Caucasians with advanced COPD (28 with LTOT) and 47 control subjects were included, and the levels of 25(OH)D were determined in late summer/early fall when the annual peak was assumed. Questionnaires about COPD symptoms, general health, lifestyle, dietary habits and QoL were used to collect data. Lung function tests and blood sampling were performed.
Results: The peak annual 25(OH)D of COPD subjects was significantly lower than in the control subjects, but there was no significant difference between COPD patients with and without LTOT. Ongoing vitamin D supplementation was the single most important intervention to maintain 25(OH)D levels ≥50 nmol/L. Among vitamin D-deficient COPD subjects, 25(OH)D correlated positively with forced expiratory volume in 1 second as % predicted, Modified British Medical Research Council score, blood oxygenation, food portion size, Mediterranean Diet Score and Ultraviolet Score.
Conclusion: Vitamin D deficiency was common among healthy individuals and COPD subjects. Peak annual 25(OH)D levels of COPD subjects correlated with clinically important outcomes. The present study emphasizes the need to routinely monitor vitamin D status among patients with advanced COPD and to consider to medicate those with vitamin D deficiency with vitamin D supplementation.
Keywords: chronic obstructive pulmonary disease, inflammation, long-term oxygen therapy, quality of life, vitamin D, ultraviolet score
Introduction
COPD is an inflammatory airway disease characterized by a not fully reversible airflow limitation, which in advanced stages has a great impact on quality of life and survival.1,2 With regard to the clinical course and prognosis of COPD, lifestyle and nutritional factors are important. Indeed, malnutrition is particularly unfavorable for prognosis.3 Therefore, in recent years, the impact of dietary habits, nutritional status and nutritional interventions has been highlighted.4
Epidemiological studies have shown that a diet in balance with the individual need is associated with improved pulmonary outcomes.5,6 In recent years, the role of vitamin D status for the clinical course of COPD has gained increasing interest.7,8 Indeed, vitamin D deficiency (defined as a plasma level of the stable metabolite 25(OH)D <50 nmol/L) is increasingly recognized in patients with COPD and has been attributed to dietary, lifestyle and behavioral changes.9 Vitamin D deficiency is proposed to be a risk factor for COPD in terms of a positive correlation to COPD severity.7–9 However, it is by no means clear that vitamin D plays a major role in COPD.
Most individuals meet much of their vitamin D need through exposure to ultraviolet (UV) radiation of the sunlight and only to a minor extent via intake of vitamin D-rich foods, preferentially oily fish. At latitudes close to the poles, UV radiation is subject to great seasonal variations.7,8 Consequently, vitamin D is mainly formed during spring, summer and the early fall months and is then stored in the liver and fat for later usage during winter.10
Similar to a British population,11 one might assume that plasma 25(OH)D in a Scandinavian population will reach its peak annual value at the end of summer and the beginning of fall. It was recently shown in a Swedish population of COPD subjects that low intake of vitamin D and low plasma levels of 25(OH)D are common and the difference between COPD subjects and controls is most pronounced in wintertime.8 Moreover, in a Norwegian population, COPD was associated with an increased risk of vitamin D deficiency, and important disease characteristics were significantly related to 25(OH)D levels.7 Thus, the study by Persson et al demonstrated significant correlations between 25(OH)D and obesity, current smoking, depression and COPD severity, ie, Global initiative for chronic Obstructive Lung Disease (GOLD) stage III–IV.7
As the plasma level of 25(OH)D varies substantially due to seasonal influence, in the present study, we tested the idea to measure the annual peak values of 25(OH)D of COPD and control subjects. By sampling venous blood from all study subjects during a 7-week period at the late summer/early fall, we thought we would achieve a better standardization of the 25(OH)D analysis and, thereby, would make a more reliable evaluation of the factors that may influence the vitamin D status of COPD and control subjects. Because Persson et al have previously shown that COPD GOLD stage III–IV is associated with 25(OH)D levels, we sought to identify the clinical variables that determine COPD severity, which have a maximum influence on the level of 25(OH)D. Moreover, no previous study has analyzed the impact of long-term oxygen therapy (LTOT) on the vitamin D status of COPD subjects. We hypothesized that LTOT patients would be particularly prone to vitamin D deficiency because of the limitations in outdoor activities associated with such therapy. Since exposure to UV radiation is the most important source of vitamin D, we also thought to determine its influence on vitamin D status using an annual UV light exposure score designed by us.
Subjects and methods
Study population
Altogether, 170 individuals were invited to participate: 55 patients with COPD without LTOT, 67 COPD patients with LTOT and 48 lung healthy subjects. The final study sample included 113 subjects: 38 COPD subjects without LTOT, 28 COPD subjects with LTOT and 47 lung healthy subjects. All subjects were examined and included by the same senior consultant (HLP) and the same registered nurse (PJ) at the outpatient respiratory clinic at the University Hospital of Linköping, Sweden, during a 7-week period (August and September 2012). There is a considerable annual variation in exposure to sunlight and, therefore, a seasonal variation in 25(OH)D.11 To reduce noise and avoid having to do adjustment for this seasonal variation, we chose to perform all the sampling during a short period of time. Only COPD subjects with stable disease, forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) <0.7, FEV1 % predicted <80%, without a history of autoimmune diseases or active cancer in the past 5 years were included. All patients and control subjects provided written informed consent. The study was approved by the Regional Committee in Linköping (Östergötland, Sweden; Dnr: 2012:32-31, 2012:134-32).
Health and constitutional factors
Pulmonary function was measured with a spirometer from Jaeger using Hedenström as a reference. Smoking habits, comorbidities, use of medications and supplements were recorded. Exacerbations treated with oral steroids and/or oral antibiotics and/or requiring hospitalization during the previous year were registered. Dyspnea was graded by the Modified British Medical Research Council (mMRC), five-graded questionnaire (0–4).12 COPD symptoms were scored with the eight-item unidimensional COPD Assessment Test (CAT; 0–40).13 Health-related quality of life was assessed by the St George’s Respiratory Questionnaire (SGRQ), which consists of three domains (symptoms, impact and activity).14 Depending on the FEV1 % predicted, number of excacerbations during the previous year, mMRC and CAT scores (cut-off values ≥2 and ≥10, respectively), COPD subjects were categorized as A, B, C or D subjects.15 The Dyspnoea, Obstruction, Smoking, Exacerbation (DOSE) index (0–8) was calculated using the mMRC dyspnea scale, FEV1 % predicted, smoking status and the exacerbation rate during the previous year.15 Comorbidities were graded using the Charlson Comorbidity Index.16 Skin pigmentation score (SPS) was graded using the Fitzpatrick Skin Phototype Classification (scale 1–6).17 Body mass index (kg/m2) was calculated.
Dietary and lifestyle factors
For evaluation of the annual individual sunlight exposure, we constructed an UV Score (UVS). A four-part question was used to divide the past year into quarters (December–February, March–May, June–August and September–November). The average time spent outdoors in daylight during each quarter was estimated as “1–4 h/week”, “5–6 h/week”, “1–2 h/day”, “3–5 h/day” and “≥6 h/day”; the choices generated 1, 2, 3, 4 and 5 points. For each quarter, the individual point (index of time spent outdoors in daylight) was multiplied with the average UV radiation for that quarter. Finally, the result of “time spent outdoors in daylight × UV exposure” for each quarter was added, giving an annual UVS. The information about the UV radiation came from the Swedish Meteorological and Hydrological Institute that continuously measures the daily UV radiation (CIE [Commission Internationale de l’Eclairage]-weighted irradiation) at a location just 40 km northeast of the study center.18 The data that were used to calculate the quarterly radiation were collected from readings of the average daily UV radiation between 2008 and 2011.19 The radiation at each day during the quarter was used to calculate a quarterly mean that was 0.0265, 0.386, 0.685 and 0.149 Wh/m2 for the quarters December–February, March–May, June–August and September–November, respectively. Information on sources of extra-UV exposure (holidays in sunny countries or visits to tanning salons) during the past 4 months was also recorded.
Dietary habits were assessed by two ways: 1) by the average size of a typical lunch or dinner and 2) by the resemblance to a traditional Mediterranean diet, assessed as Mediterranean Diet Score (MDS). The average size of a food portion was assessed using four photos of plates as reference (showing small [=1], medium [=2], large [=3] or very large [=4] portions). An 11-item questionnaire (0–44) was used to assess the MDS.20 Omega-3 index of erythrocytes was also assessed as a high level relates to a diet rich in long chain omega-3 fatty acids that generally are considered as healthful. Moreover, the levels of omega-3 of erythrocytes and 25(OH)D in plasma are positively associated.21 The frequency of exercise was classified as: no exercise at all, rarely but sometimes walking or cycling, regular but easy exercise at least 1 time/week and regular exercise plenty of times/week.
Laboratory measurements
Venous peripheral blood samples were drawn for immediate analysis. After centrifugation, plasma was transferred to microtubes that were stored at −80°C. For analysis of 25-hydroxyvitamin D2 and D3, the plasma samples were worked up according to the method described by Turpeinen et al22 before derivatization with 4-phenyl-1,2,4-triazoline-3,5-dione and finally analyzed by high-performance liquid chromatography-electrospray tandem mass spectrometry. Quality of the assay was assured by participation in the Vitamin D External Quality Assessment Scheme.23 The fatty acid composition after hydrolysis of erythrocytes was analyzed with a slightly modified version of a method that was previously reported.24 Fifty microliters of erythrocytes was first transmethylated to fatty acid methyl esters in 2 mol/L KOH in methanol. After extraction with hexane and evaporation with nitrogen, the samples were diluted in carbon disulfide and finally analyzed with gas chromatography. Omega-3 index was expressed as the percentage of eicosapentaenoic acid + docosahexaenoic acid divided by the total fatty acids. Analyses of 25-hydroxyvitamin D and omega-3 index were performed at the Division of Occupational and Environmental Medicine at the Linköping University.
Statistical analysis
The results are reported as the mean ± SD for continuous variables. Chi-square test was used to compare nominal data, while Mann–Whitney U-test was used for ordinal data and Student t-test was used for normalized data on the least interval scale. Two-sided t-tests were used for continuous variables and Pearson’s chi-squared test for categorical variables. Correlations were analyzed by Pearson’s correlation coefficient.
Results
Differences between control subjects and COPD subjects
Sixty-six COPD subjects and 47 age- and gender-matched lung healthy subjects (hereafter referred to as “control group/subjects”) completed the study. The characteristics of the study population are presented in columns A and B of Table 1.
Compared to the control group (column A of Table 1), the COPD group (column B of Table 1) consisted of significantly more current and ex-smokers. COPD subjects displayed significantly higher Charlson Comorbidity Index scores and significantly lower FEV1 % predicted and blood oxygen saturation (SAT). Food portion size, MDS, omega-3 index, UVS and peak annual 25(OH)D were all significantly lower among COPD subjects. None of the COPD subjects had been on holidays in sunny countries during the past 4 months, while such excursions were rather frequent among healthy subjects (n=12). Among all subjects, only one COPD subject had visited a tanning salon during the past 4 months, and this subject presented with a peak annual 25(OH)D value ≥50 nmol/L. All subjects, except one control subject with SPS 3, were white skinned (SPS 1–2).
Most COPD subjects had very advanced disease: stage III–IV 70% and GOLD C–D 82%. Most COPD subjects (97%) regularly used inhaled steroids and 15% used oral steroids. Nearly 50% of the COPD subjects reported no or very limited exercise, while all control subjects performed some kind of exercise (data not presented). Thirty-four subjects (52%) in the COPD group showed peak annual 25(OH)D levels <50 nmol/L compared to only three subjects (6%) in the healthy control group.
Differences between COPD subjects with high and low peak annual 25(OH)D
The columns C and D of Table 1 show the results of COPD subjects with “high-level 25(OH)D” (defined as ≥50 nmol/L) and “low-level 25(OH)D” (defined as <50 nmol/L). Vitamin D supplementation was significantly more frequent among COPD subjects displaying peak annual 25(OH)D ≥50 nmol/L. Indeed, more than every second of these subjects was medicated with vitamin D. In contrast, only one (3%) of “low-level 25(OH)D” COPD subjects was supplemented with vitamin D. “Low-level 25(OH)D” COPD subjects demonstrated significantly higher CAT score and higher score on the symptom domain of SGRQ, while UVS was significantly lower.
Differences between COPD subjects with and without LTOT
While COPD subjects, in general, exhibited significantly lower peak annual 25(OH)D than the control subjects, there was no significant difference regarding the use of LTOT (Figure 1). Twenty-eight COPD subjects (42%) had ongoing LTOT. There were no significant differences between “high-level 25(OH)D” (≥50 nmol/L, n=13) and “low-level 25(OH)D” (<50 nmol/L, n=15) LTOT subjects with the following exceptions: “low-level 25(OH)D” LTOT subjects demonstrated significantly higher CAT score (p<0.01) and higher score on the SGRQ symptom domain (p<0.05), while the frequencies of vitamin D supplementation (p<0.05) and UVS (p<0.05) were significantly lower. Notably, 32% of COPD subjects without LTOT and 57% of COPD subjects with LTOT did not perform any exercise at all.
The relationship between COPD severity, lifestyle and peak annual 25(OH)D
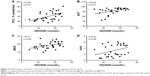
Figure 2A–C shows how the variables were linked to COPD severity and the lifestyle factors were related to vitamin D status in all COPD subjects, regardless of ongoing vitamin D supplementation. Thus, peak annual 25(OH)D in the COPD group (n=66) correlated significantly with CAT score (r=−0.26, p<0.05; Figure 2A), the symptom domain of SGRQ (r=−0.30, p<0.05), DOSE index (r=−0.28, p<0.05), high-sensitivity C-reactive protein (r=−0.26, p<0.05) and interleukin-6 (r=−0.30, p<0.05). The only lifestyle factors significantly associated with peak annual 25(OH)D were omega-3 index (r=0.24, p<0.05; Figure 2B), reflecting the intake of food rich in omega-3 fatty acids, and UVS (r=0.37, p<0.05; Figure 2C), reflecting exposure to UV light.
Ongoing supplementation with vitamin D was associated with a high peak annual 25(OH)D value (≥50 nmol/L). Thus, only 1 of 34 COPD subjects displaying peak annual value <50 nmol/L was medicated with vitamin D. “Low-level 25(OH)D” (<50 nmol/L) COPD subjects without ongoing vitamin D supplementation (n=33) demonstrated significant correlations between peak annual 25(OH)D and FEV1 % predicted (r=0.50, p<0.01; Figure 3A), mMRC (r=−0.36, p<0.05), SAT (r=0.48, p<0.01; Figure 3B) and DOSE index (r=−0.38, p<0.05). Lifestyle factors significantly associated with peak annual 25(OH)D were food portion size (r=0.38, p<0.05), MDS (r=0.41, p<0.05; Figure 3C) and UVS (r=0.35, p<0.05; Figure 3D).
Logistic regression analysis for peak annual value of 25(OH)D with a cut off level <50 nmol/L was also performed, but due to the small sample size, no significant results were found.
Discussion
The present study is the first to use the peak annual value of the stable vitamin D metabolite, 25(OH)D, to assess the influence of COPD severity and lifestyle on vitamin D status. By using the peak annual value, we were able to rule out the normal seasonal influence on the serum 25(OH)D value, and, thereby, we were in a better way able to define individuals truly lacking vitamin D at all seasons of the year, that is, individuals presenting with a peak annual value of 25(OH)D <50 nmol/L. In line with previous studies,7,8 this study supports the idea that COPD severity (reflected by FEV1 % predicted, mMRC, SAT and DOSE index) is associated with low levels of vitamin D. However, we could, not see if subjects with LTOT had significantly lower levels of vitamin D than COPD patients without LTOT (Figure 1).
This study also highlights CAT as a particularly useful marker to identify individuals with COPD at risk to develop vitamin D deficiency. Thus, “low-level 25(OH)D” COPD subjects and LTOT subjects demonstrated significantly higher CAT score. Moreover, CAT score correlated significantly with the 25(OH)D level. CAT scores ≥10 are used to define COPD patients with more pronounced symptoms of COPD, categorized as GOLD B and D. Notably, in this study, only one subject with CAT score <10 exhibited peak annual 25(OH)D level <50 nmol/L (Figure 2A), suggesting that this cut-off value of CAT could be used in the screening for vitamin D deficiency among outpatient COPD subjects.
Of all lifestyle factors evaluated in the present study, regular vitamin D supplementation was the single most important intervention to maintain serum 25(OH)D ≥50 nmol/L. Indeed, the majority of COPD subjects with adequate peak annual 25(OH)D ≥50 nmol/L (53%) had been medicated with vitamin D, while only 3% did the same among COPD subjects showing values <50 nmol/L. The same pattern was observed among COPD subjects on LTOT. Overall, 27% of all COPD subjects were supplemented with vitamin D and ~50% demonstrated 25(OH)D <50 nmol/L. During 2015/2016, 3 years after this study was conducted, we assessed serum 25(OH)D values among patients with advanced COPD who lived in the same region as the subjects participating in this study. We then found that, of all investigated subjects (N=71), the majority (76%) exhibited 25(OH)D levels <50 nmol/L and vitamin D supplementation was still rare (unpublished data).
Food rich in omega-3 is rich in vitamin D as well, and, omega-3 is positively associated with 25(OH)D.11,21 Among COPD subjects, we were able to repeat the same observation (Figure 2B). Compared to control subjects, the omega-3 index of COPD subjects was significantly less, indicating that their intake of food was not rich in vitamin D. This observation is well in line with previous findings by Måhlin et al.8 COPD patients are often malnourished, and we also found in this study that COPD subjects ate significantly smaller food portions than control subjects did. Moreover, the food of COPD subjects was also less similar to the traditional Mediterranean diet, which indicates that it was less healthy. A Mediterranean diet is generally considered healthy because it includes a low intake of red meat, saturated fat and refined grains, moderate intake of alcohol and a relatively high intake of fruits, vegetables, monounsaturated fat, fish, whole grains, legumes and nuts. This type of diet protects against all-cause mortality, coronary heart disease and diabetes.25
As already pointed out, exposure to UV light is a much greater source of vitamin D than the contribution provided by the diet. To capture the annual UV light exposure, we, therefore, tested a novel way to obtain an index (UVS). UVS is based on the subject’s self-made assumption of the average daily time they spent outdoors during different seasons and the mean UV irradiation for each specific season. A registered nurse also recorded the skin pigmentation of each subject. Skin pigmentation is of great importance for photosynthesis of the precursor of vitamin D in the skin. In this study, UVS was consistently of great importance in all statistical analyses made. Thus, UVS was significantly lower among COPD subjects compared to control subjects and significantly lower among COPD subjects with 25(OH)D <50 nmol/L compared to COPD subjects with higher levels. Moreover, as the only variable reflecting lifestyle, UVS was significantly associated with peak annual 25(OH)D among all included COPD subjects (Figure 2C) and among those COPD subjects presenting with 25(OH)D <50 nmol/L (Figure 3D). Since all included subjects were native Swedes, skin pigmentation did not differ much.
The results of this study are best understood in the light of two previous Scandinavian studies.7,8 Similar to these studies, this study shows that patients with COPD are more prone to show vitamin D deficiency and important disease characteristics are associated with the 25(OH)D level. Regarding the latter, in this study, those were the scores of CAT and the symptom domain of SGRQ, DOSE index and markers of systemic inflammation, ie, high-sensitivity C-reactive protein and interleukin-6. The study by Persson et al demonstrated significant correlations between 25(OH)D and obesity, current smoking, depression and COPD severity, ie, GOLD stage III–IV.7 The study by Måhlin et al highlighted diet with low content of vitamin D as a risk factor for vitamin D deficiency among Swedish COPD subjects and emphasized the importance of vitamin D supplementation.8 Unlike these studies, this study was a single-center study and 113 subjects were all included during a short 7-week period in order to assess peak annual 25(OH)D value. As we aimed to evaluate the influence of LTOT, the COPD subjects were generally more severely ill in this study. Unlike the previous studies mentioned,7,8 this study also accounts for the exposure to UV light of each study subject, which we believe is crucial for the understanding of vitamin D status of the study populations.
Being a single-center study, the study logistics ensured a uniform clinical assessment of all subjects included by the same senior consultant and by the same registered nurse, which we consider to be a great advantage. However, this study has limitations. The sample size was too small for statistical analysis using multiple linear regression models. Thus, the significant relationships reported in this study must be interpreted with some caution due to the lack of further statistical support. In line with the study by Måhlin et al,8 this study indicates that vitamin D levels are well maintained >50 nmol/L with vitamin D supplementation. This is a cross-sectional study. Thus, whether such supplementation has any impact on COPD outcomes as well is beyond the scope of this study. Previous randomized clinical studies analyzing the effects of vitamin D supplementation on different outcomes of COPD are contradictory.26–29 Martineau et al found in a prespecified subgroup analysis that vitamin D was protective against moderate or severe exacerbation in participants with baseline serum 25(OH)D concentration <50 nmol/L.26 In addition, Hornikx et al found an effect on respiratory muscle performance in a subgroup of patients with low levels of vitamin D.27 In contrast, Rafiq et al28 and Bjerk et al29 did not find any effect of vitamin D supplementation on physical performance.
Conclusion
Vitamin D deficiency was common among both healthy individuals and COPD subjects. Peak annual 25(OH)D levels of COPD subjects correlated with clinically important outcomes and lifestyle factors. In line with similar Scandinavian studies, this study emphasizes the need to routinely monitor vitamin D status among patients with advanced COPD and to consider to medicate those with vitamin D deficiency with vitamin D supplementation.
Acknowledgments
The authors thank all the subjects in this study for their committed participation in this research. The authors also thank M Romanovich for administration of the permission to use the St George’s Respiratory Questionnaire and Bo Rolander for statistical support. This work was supported by grants to HLP (from the County Council of Östergötland Region Östergötland, ALF), Sweden (grant numbers LIO-275901, LIO-355741, LIO-432861, LIO-534761, LIO-601911 and LIO-697521), the Medical Research Council of Southeast Sweden (FORSS; grant numbers FORSS-308331 and FORSS-559931), the Linköping University Hospital Foundation for Medical Research, Sweden (grant number LIO-475131), the Heart and Lung Foundation, Sweden (grant numbers 20140245 and 20140330) and the Swedish Society of Medicine (grant number SLS-368431); to PL from the County Council of Östergötland (ALF), Sweden (grant number LIO-201751) and the Medical Research Council of Southeast Sweden (FORSS; grant number FORSS-226801); and to MK from the County Council of Jönköping (Futurum), Sweden (grant numbers FUTURUM-342821, FUTURUM-489691, FUTURUM-608651, FUTURUM-712082 and FUTURUM-712181).
Part of the results were presented in a poster session at the European Respiratory Society (ERS) 2013 Annual Congress; September 711, Barcelona, Spain.
Author contributions
MK designed the study, performed the statistical analysis and wrote the manuscript. PL designed the study, performed analyses of 25(OH)D and omega-3 index, constructed the UVS, collected and analyzed data and wrote parts of the manuscript. PJ examined and included the study subjects, collected data and participated in manuscript writing. HLP designed the study, examined and included the study subjects, collected and analyzed data and wrote the manuscript. All authors have given their final approval of the version submitted. This study was performed at the Department of Pulmonary Medicine, Linköping University, Sweden. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
HLP has received honoraria for advisory boards/lectures from AstraZeneca, Boehringer Ingelheim, Novartis, Takeda Nycomed, Almirall, Intermune and Roche. MK has received honoraria for lectures from AstraZeneca, Boerhinger Ingelheim, Novartis, Roche, Lilly and Pfizer. None of these disclosures influenced the present study in any way. The other authors report no conflicts of interest in this work.
References
Jones PW. Health status and the spiral of decline. COPD. 2009;6(1):59–63. | ||
Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. Br Med Bull. 2009;92:7–32. | ||
Hallin R, Koivisto-Hursti UK, Lindberg E, Janson C. Nutritional status, dietary energy intake and the risk of exacerbations in patients with chronic obstructive pulmonary disease (COPD). Respir Med. 2006;100(3):561–567. | ||
Schols AM, Ferreira IM, Franssen FM, et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J. 2014;44(6):1504–1520. | ||
Fonseca Wald ELA, van den Borst B, Gosker HR, Schols AMWJ. Dietary fibre and fatty acids in chronic obstructive pulmonary disease risk and progression: a systematic review. Respirology. 2014;19(2):176–184. | ||
Varraso R, Willett WC, Camargo CA Jr. Prospective study of dietary fiber and risk of chronic obstructive pulmonary disease among US women and men. Am J Epidemiol. 2010;171(7):776–784. | ||
Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One. 2012;7(6):e38934. | ||
Måhlin C, von Sydow H, Osmancevic A, et al. Vitamin D status and dietary intake in a Swedish COPD population. Clin Respir J. 2014;8(1):24–32. | ||
Janssens W, Bouillon R, Claes B, et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax. 2010;65(3):215–220. | ||
Ross AC, Manson JE, Abrams SA, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–58. | ||
Hyppönen E, Power C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007;85(3):860–868. | ||
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. | ||
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. | ||
Engström CP, Persson LO, Larsson S, Sullivan M. Reliability and validity of a Swedish version of the St George’s Respiratory Questionnaire. Eur Respir J. 1998;11(1):61–66. | ||
Jones RC, Donaldson GC, Chavannes NH, et al. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE Index. Am J Respir Crit Care Med. 2009;180(12):1189–1195. | ||
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. | ||
Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124(6):869–871. | ||
Josefsson W. UV-radiation 1983–2003 measured at Norrköping, Sweden. Theor Appl Climatol. 2006;83(1–4):59–76. | ||
Sweden’s Meteorological and Hydrological Institute (SMHI). Långtidsmätningar av UV-strålning i Norrköping. Available from: https://www.smhi.se/klimatdata/meteorologi/uv-stralning/langtidsmatningar-av-uv-stralning-i-norrkoping-1.2088. Accessed April 9, 2018. Swedish. | ||
Goulet J, Lamarche B, Nadeau G, Lemieux S. Effect of a nutritional intervention promoting the Mediterranean food pattern on plasma lipids, lipoproteins and body weight in healthy French-Canadian women. Atherosclerosis. 2003;170(1):115–124. | ||
Park Y, Kim M. Serum 25-hydroxyvitamin D concentrations are associated with erythrocyte levels of n-3 PUFA but not risk of CVD. Br J Nutr. 2011;106(10):1529–1534. | ||
Turpeinen U, Hohenthal U, Stenman UH. Determination of 25-hydroxyvitamin D in serum by HPLC and immunoassay. Clin Chem. 2003;49(9):1521–1524. | ||
Burdette CQ, Camara JE, Nalin F, et al. Establishing an accuracy basis for the vitamin D external quality assessment scheme (DEQAS). J AOAC Int. 2017;100(5):1277–1287. | ||
Harris WS, Von Schacky C. The Omega-3 Index: a new risk factor for death from coronary heart disease? Prev Med. 2004;39(1):212–220. | ||
Gardener H, Wright CB, Gu Y, et al. Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: the Northern Manhattan Study. Am J Clin Nutr. 2011;94(6):1458–1464. | ||
Martineau AR, James WY, Hooper RL, et al. Vitamin D3 supplementation in patients with chronic obstructive pulmonary disease (ViDiCO): a multicentre, double-blind, randomised controlled trial. Lancet Respir Med. 2015;3(2):120–130. | ||
Hornikx M, Van Remoortel H, Lehouck A, et al. Vitamin D supplementation during rehabilitation in COPD: a secondary analysis of a randomized trial. Respir Res. 2012;13:84. | ||
Rafiq R, Aleva FE, Schrumpf JA, et al. Prevention of exacerbations in patients with COPD and vitamin D deficiency through vitamin D supplementation (PRECOVID): a study protocol. BMC Pulm Med. 2015;15:106. | ||
Bjerk SM, Edgington BD, Rector TS, Kunisaki KM. Supplemental vitamin D and physical performance in COPD: a pilot randomized trial. Int J Chron Obstruct Pulmon Dis. 2013;8:97–104. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.