Back to Journals » Journal of Pain Research » Volume 10
The influence of clinical equipoise and patient preferences on outcomes of conservative manual interventions for spinal pain: an experimental study
Authors Bishop MD, Bialosky JE, Penza CW, Beneciuk JM , Alappattu MJ
Received 22 December 2016
Accepted for publication 21 February 2017
Published 26 April 2017 Volume 2017:10 Pages 965—972
DOI https://doi.org/10.2147/JPR.S130931
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Mark D Bishop,1,2 Joel E Bialosky,1–3 Charles W Penza,1,2 Jason M Beneciuk,1,3 Meryl J Alappattu1,2
1Department of Physical Therapy, University of Florida, 2Center for Pain Research and Behavioral Health, 3Brooks-PHHP Research Collaboration, Gainesville, FL, USA
Background: Expected pain relief from treatment is associated with positive clinical outcomes in patients with musculoskeletal pain. Less studied is the influence on outcomes related to the preference of patients and providers for a specific treatment.
Objectives: We sought to determine how provider and patient preferences for a manual therapy intervention influenced outcomes in individuals with acutely induced low back pain (LBP).
Participants and methods: Pain-free participants were randomly assigned to one of two manual therapies (joint biased [JB] or constant touch [CT]) 48 hours after completing an exercise protocol to induce LBP. Expectations for pain relief and preferences for treatment were collected at baseline, prior to randomization. Pain relief was assessed using a 100 mm visual analog scale. All study procedures were conducted in a private testing laboratory at the University of Florida campus.
Results: Sixty participants were included in this study. After controlling for preintervention pain intensity, the multivariate model included only preintervention pain (B=0.12, p=0.07) and provider preference (B=3.05, p<0.0001) and explained 35.8% of the variance in postintervention pain. When determining whether a participant met his or her expected pain relief, receiving an intervention from a provider with a strong preference for that intervention increased the odds of meeting a participant’s expected pain relief 68.3 times (p=0.013) compared to receiving any intervention from a provider with no preference. Receiving JB intervention from any provider increased the odds of meeting expected relief 29.7 times (p=0.023). The effect of a participant receiving an intervention they preferred was retained in the model but did not meet the criteria for a significant contribution.
Conclusion: Our primary findings were that participant and provider preferences for treatment positively influence pain outcomes in individuals with acutely induced LBP, and joint-biased interventions resulted in a greater chance of meeting participants’ expected outcomes. This is contrary to our hypothesis that the interaction of receiving an intervention for which a participant had a preference would result in the best outcome.
Keywords: equipoise, expectations, manual therapy, acute pain
Introduction
Expected pain relief from treatment is associated with positive clinical outcomes in patients with musculoskeletal pain.1–3 In people with spinal pain disorders, for example, the expectation of gaining complete relief from treatment is associated with better short- and long-term outcomes, both for global ratings of change and for self-reports of pain and disability regardless of the intervention provided,1,2 and the specific expectation of benefit from an intervention was determined to be part of a derivative clinical prediction rule for patients with neck pain.3 Such expectations are unique to the individual, and demographic factors such as gender, education level, age, and race and psychological (fear and depression) factors influence patient expectations, as well as prior experiences of the patient.
Less widely studied is the influence on outcomes related to the preference of the patient for a specific treatment. Patient preferences for treatment are most commonly studied with respect to long-term adherence rates to intervention plans for chronic health conditions such as diabetes and heart disease. Preferences are also thought to bias enrollment and participation in clinical trials of interventions.4,5 However, studies of treatment outcomes when patient preferences are matched to a given intervention (i.e., patient prefers treatment A and is given treatment A vs. patient prefers treatment B and is given treatment A) are less common and thus a focus of this article.
Another consideration is the state of the clinical equipoise of a provider. Clinical equipoise is defined as genuine uncertainty regarding the efficacy of a particular treatment arm.6,7 In other words, true clinical equipoise indicates that providers do not have a preference for one intervention over another. In the case of clinical trials, providers should not have preferences for specific treatments to maintain the integrity of randomly administering treatment and reducing bias. However, with many interventions, providers may place importance on their expertise in that intervention, which will likely play some role in the outcome.7 The lack of equipoise, though a valid concern for random assignment in clinical trials, may positively or perhaps negatively influence patient outcomes. For example, Cook et al8 found that preference of the provider was significantly associated with improvements in patients’ disability and pain outcomes when that provider performed interventions that he or she preferred.
Consequently, we asked the following questions. First, how much change in pain intensity do people expect from a conservative manual therapy intervention for pain? Second, do participants and providers have preferences for a specific manual therapy intervention? Third, are these expectations and preferences related to the amount of actual pain relief that is experienced by participants after a manual therapy intervention? Finally, we sought to identify how participant and provider preferences interacted to influence the extent that a participant’s expectation for treatment outcome was met.
We used an established experimental model of low back pain (LBP) to answer these questions. This model creates clinically relevant levels of pain intensity and results in self-reports of disability and pain interference in most individuals.9 Similar to patients seeking care for LBP, pain intensity from the experimentally induced LBP is associated with measures of negative aspect (i.e., fear of pain), providing external validity as an experimental model of LBP. The advantage of using a preclinical model is that we are able to control the mechanism and site of injury across study participants and body regions, resulting in homogeneity of pain mechanism that cannot be obtained when recruiting patients with clinical pain conditions. Consequently, the variability in our outcomes may be explained by the variables of interest in this study, participant and provider preference, without needing to account for the mechanism of onset or source of pain.
Participants and methods
Participants
This study represents a planned subanalysis from a larger clinical trial (NCT-01406847). Participants were recruited from the university and surrounding community. Participants were included if they were pain free for 6 months prior to the experiment and understood spoken and written English. Participants were excluded if they met any of the following criteria: previous participation in a conditioning program specific to trunk extensors, any current back pain, any chronic medical conditions affecting pain perception, kidney dysfunction, muscle injury in the back or legs, major psychiatric disorder, history of previous injury including surgery to the lumbar spine, renal malfunction, cardiac condition, high blood pressure, osteoporosis, liver dysfunction, and performance of any intervention for symptoms induced by exercise and before the termination of their participation of the protocol. All participants completed the informed consent process, and the institutional review board of the University of Florida approved the study.
Induction of LBP
This model of acute endogenous LBP has been previously described in greater detail elsewhere.9 Briefly, participants performed repeated bouts of dynamic resisted trunk extension exercise individualized to each participant using a weight load equal to 90% of the peak torque measured during a baseline isometric test. After each bout, torque was reestimated. Using a criterion of 50% reduction in torque, participants either completed another bout if the torque was above 50% or ended if the reestimated torque was 50% or less than the baseline. Following the exercise, participants were instructed not to initiate any medication or apply any intervention to the lumbar spine to reduce painful symptoms.
Interventions
Participants were randomly assigned to one of two types of manual therapy interventions 48 hours following the exercise-induced LBP protocol. The randomization schedule was developed for the parent experiment by the protocol statistician and numbers marked in sealed envelopes. Just prior to the intervention, all participants, regardless of group assignment, were told, “This intervention is used by clinicians including osteopaths, chiropractors, and physical therapists for patients with back pain.” Each intervention met the criteria to be categorized as a “Mind and Body”-based therapy by the National Center of Complementary and Integrative Health (NCCIH).10
One of three licensed health care providers with specialized training and experience and who were not involved with the assessment of the participants performed interventions to each patient – two physical therapists (one male and one female) and one chiropractor (male). Each provider underwent training (with MDB) on the specific techniques performed in this study. The amount of “hands-on” and personal contact between provider and participant was equivalent between interventions. Verbal instructions regarding the techniques performed were scripted to ensure similar interaction and information exchange across the providers. Additionally, to minimize potential bias for one treatment over another, participants were given identical instructions regarding the use of these interventions in clinical practice: “This treatment is used by physical therapists, osteopaths, and chiropractors to treat people with LBP.”
Joint-biased (JB) interventions
Participants randomized to the JB group received manual interventions focused to the lumbar spine commonly used for the treatment of LBP by several health care professions and previously used in a recent clinical trial involving patients with acute or subacute pain.8 Timing was standardized so that each JB intervention was provided for 5 minutes.
Muscle and soft tissue-biased intervention
In this study, we used constant touch (CT) for the muscle and soft tissue intervention.11,12 Participants randomized to CT lay prone. The provider placed both hands in contact with the participants’ pelvis across the top of the posterior aspect of the sacrum and ilia. Light pressure was applied for 5 minutes so that the time was consistent with the JB interventions.
Measures
Pain intensity and expectation for pain relief following intervention
Participants used the 101-point numerical rating scale (NRS) to provide a measure of the current intensity of their lower back pain. The NRS is a valid and reliable measure anchored with 0 = “no pain” and 100 = “worst pain imaginable”.13 The therapist who performed the intervention collected participants’ ratings of their “current pain” immediately prior to the intervention. Next, participants were asked what they expected their pain to be after the intervention was performed. Finally, participants rated the actual pain intensity they experienced after the intervention.
Participant treatment preferences
Participants completed a questionnaire regarding preference for intervention (JB vs. CT) prior to the intervention. Information about the two types of potential interventions was verbally provided during the informed consent process and included in the informed consent document. The participants were also shown photographs of each of the interventions prior to randomization to their intervention group on the day of the intervention. The preference for treatment included an option for each intervention, as well as an option for “no strong preference”.
Provider equipoise
Prior to the start of the study, each health care provider completed a questionnaire regarding which intervention he or she preferred. The questionnaire included an option for no strong preference as well as each of the other interventions (JB vs. CT).
Adverse events
An adverse event was defined as any event in which a participant sought additional health care or if pain or interference with activities of daily living related to the manual therapy technique lasted longer than 96 hours. Any reports of pain, including their duration and severity, as well as the need for analgesics and additional medical care, were recorded and reported to the institutional review board and data safety monitoring board.
Statistical analyses
Only participants reporting greater “current” pain intensity than 10 on the NRS at the follow-up visit were included in the subsequent analysis of pain relief. This threshold was chosen so that there would be the potential for pain reduction from treatment. We used IBM SPSS Statistics 23 (IBM Corp., Armonk, NY, USA) for statistical analyses.
To represent matching between participant preferences and interventions that he or she received, a participant with a preference for JB who received JB was coded as a match. If the participant had “no strong preference”, this was also considered a match for the intervention received, indicating that the participant had equal preferences for each of the interventions. Similarly, a provider who preferred JB and provided JB was coded a match, as were providers with no strong preference for any intervention. We chose this approach to matching because true clinical equipoise would result in equal preferences for every intervention.
A regression model was built with actual postintervention pain as the dependent variable. Analysis of the distributions of the dependent and independent variables suggested that linear modeling would provide the simplest model. The preintervention rating of current pain was included in the model as were the preference/equipoise variables and intervention.
Next, general linear modeling (binary logistic) was used to evaluate the factors associated with the extent to which participants’ expectations for pain relief was met. To determine the magnitude of pain relief that participants expect from manual therapy, we subtracted the participant’s rating of expected pain from the current pain intensity collected preintervention. The extent to which participants’ expectations for pain relief were met was determined by comparing the “actual” change in pain to the “expected” change in pain resulting in a binary-dependent variable (met/not met) for subsequent modeling. The predictor variables entered were chosen in the same manner as for the first regression model.
Both models were built using backward elimination procedures. If a significant interaction term was identified, the main effects related to that interaction were retained in the model. Postregression diagnostics were performed for both models. Type 1 error was maintained at 5% throughout with corrections for multiple comparisons when appropriate.
Results
Sixty participants (66% female, mean age 24.2 years [SD=5.1]) completed the protocol for the parent study and reported pain of 10 or greater at the time of the intervention (Table 1). No adverse events occurred during this study.
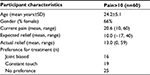  | Table 1 Summary of participants |
Pain intensity and relief
Prior to receiving the intervention, participants reported current pain intensity ranging from 10 to 60 (mean 20.6, SD=11.7) and expected to experience an average of 50% reduction in pain (SD=35%). Three people expected worse pain. The participants actually reported a 78% (SD=28%) reduction in pain on average, and no participants actually reported worse pain after intervention. The difference between the actual and expected pain relief was significant (p<0.001), where the actual reduction in pain was greater than the expected pain reduction (mean difference=28%, 95% CI=[34.95–16.54%]).
Preferences
The greatest number of participants had no preference for intervention (41%), followed by CT (31%) and JB (27%) (Table 1). There were no differences between genders in these preferences (χ2=3.65, p=0.302). One provider (female physical therapist) had no strong expectation for intervention provided and performed the intervention on 16 participants. The other two providers (male physical therapist and male chiropractor) indicated preference for JB techniques over CT and provided the intervention to the remaining 44 participants. The two providers with similar beliefs were combined in subsequent analyses. Providers observed equivalent numbers of male and female participants, and there was no difference in the proportions of interventions provided (χ2=3.15, p=0.368; Table 2).
Matching of patients’ intervention preference
Thirty-five participants received an intervention matched to their preference, and providers provided an intervention matched to provider preference 71% of the time (43 of 60 interventions). Twenty-one of the participants received an intervention that they preferred from a provider who also preferred that intervention. For the two providers who preferred JB interventions, they provided interventions that matched this preference 61% of the time.
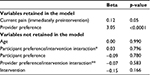
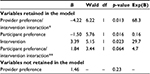
Association with postintervention pain
After controlling for preintervention pain intensity, the final parsimonious multivariate model included only current pain (preintervention) (B=0.12, p=0.07) and provider preference (B=3.05, p<0.0001) and explained 35.8% of the variance in postintervention pain. Participant preferences were not significant and neither were any of the interaction terms based on matching of intervention to preference (Table 2).
Effect of matching on expectations
Forty-four of the participants met or exceeded their expected pain relief after intervention. No differences existed in the frequency of meeting or exceeding expected pain relief (χ2=0.73, p=0.29) based on intervention alone, on the preference for an intervention (χ2=0.68, p=0.31), or on the gender of the participant (χ2=0.88, p=0.29).
An association did exist between the provider equipoise and whether a participant met expectations of relief (χ2=6.1, p=0.019) in which a larger proportion of participants receiving intervention (73%) from providers without equipoise (i.e., had a preference to provide JB interventions) met their expectations for pain relief regardless of the intervention provided. This finding was supported by the fact that there was no effect identified when a provider performed the actual technique that they preferred (χ2=0.50, p=0.34).
The parsimonious multivariate logistic model included three associations. Receiving the intervention from a provider with a strong preference for an intervention increased the odds of meeting a participant’s expected pain relief 68.3 times (p=0.013) compared to receiving any intervention from a provider with true equipoise. Receiving JB intervention from any provider increased the odds of meeting expected relief 29.7 times (p=0.023). Participant preference was retained in the model as well (odds ratio [OR]=0.16; p=0.016) (Table 3).
Discussion
We used an experimental model of acute LBP to examine the effects of participant and provider treatment preference for a manual therapy technique. Our results indicate that participants with experimentally induced LBP expected the body-based interventions to reduce their pain by an average of 50%, with no difference between the interventions. These positive expectations in our sample are consistent with prior work by Bishop et al who found that patients with back2 and neck1 pain believe that manual therapy interventions are an effective treatment for LBP. Following the intervention, participants reported an actual 78% reduction in the pain.
Treatment preference and experienced pain relief
The results of our study found that participants who received their intervention from a provider with a treatment preference experienced a greater reduction in pain compared to participants who received their intervention from a provider with equipoise. The results also indicate that participants were also significantly more likely to meet or exceed their expected pain relief if they received an intervention by a provider with a treatment preference, regardless of the actual intervention provided. These data extend previous work by Cook et al8 to demonstrate that a provider who provides a manual therapy intervention that he or she prefers (and may also have high treatment expectations for, although not directly assessed in this study) may positively influence pain relief. The positive influences from the providers may be in the form of nonspecific effects (e.g., communication with patients) or potentially may be linked to prior provider experiences, both of which have strong potential for driving patient expectations for a specific treatment.14,15 It is also a reasonable assumption that patient expectations and preference for a specific treatment are closely related, however involve complex interactions that require further investigation through adequately powered studies.16,17 These findings also reinforce the important role health care providers have when communicating clinical decision-making processes with patients in regard to expected outcomes and personal preferences as conflicts have potential to influence outcomes.14,15,18
Treatment preference and intervention effects on experienced pain relief
The comparative effects of the interventions on meeting or exceeding expectations were only significant after controlling for both participant and provider treatment preference. Participants who received JB interventions were more likely to meet or exceed their expected pain relief. Our results build upon an expanding body of work suggesting the effectiveness of manual therapy interventions on experimental pain,19 and short- and long-term clinical pain is dependent on the contextual environment in which they are performed.20,21 The results of the present study and the data from previous work support the recommendation that patient preferences for treatment be taken into account when developing a treatment plan.22 Shared decision-making is a process by which the health care provider solicits patient values and preferences and incorporates these into the clinical decision-making process. In this process, patients are better informed and become more engaged in helping to decide their treatment, which may lead to increased confidence in health care decisions.22 Shared decision-making provides an advantageous strategy toward developing a more effective approach to treating individuals with musculoskeletal pain conditions in part due to consideration of individual patient beliefs and preferences. This approach can be difficult when patient preferences and expectations do not match with their needs. Needs of patients that are not met by health care providers are associated with lower patient satisfaction, which can negatively influence the provider–patient relationship and may lead to lack of follow-up for needed health care.23 Ultimately, while it is necessary to evaluate patient preferences, providers have a responsibility to provide health care recommendations and treatment based on best clinical practices, including guidelines and sound evidence.
In our study, the majority of patients did not have a strong preference for any particular manual therapy intervention. This is consistent with prior work that has shown that a similar percentage of patients do not have a strong preference for different rehabilitative treatments. For example, George and Robinson24 found that 37% of participants did not show a strong preference between different styles of exercise (i.e., quota based vs. exposure). What we did not expect in our current study was that a larger percentage of subjects preferred CT over JB. The CT intervention was applied with comparable time to control for provider–participant interaction and contact delivered during JB interventions. Many factors have been shown to influence expectations; however, less is known regarding what factors influence what treatments patients prefer and why they prefer certain treatments to others. Although purely speculative, we suspect that the descriptive terminology used to describe the interventions may have influenced participants’ treatment preference, particularly if they have not had any prior experiences receiving the manual therapy interventions in this study. The instructions provided to participants in this study about each of the interventions were somewhat neutral. Previous research in shaping patient expectations for pain relief has used enhanced instructional sets where investigators use strong verbal suggestion of pain relief with a particular intervention; for example, “the agent you have just been given is known to significantly reduce pain in some patients”.25,26 Future work in this area should explore how providing a stronger suggestion of pain relief to patients may influence their preferences for particular interventions and also their treatment outcomes.
Limitations
There are limitations in this study to consider. There were only three providers in this study. Two of the providers had a preference for JB and one had no strong preference for any intervention. Because of this, our results may be attributed to provider characteristics that differed between the groups. For example, given that both male providers had a strong preference for JB, we are unable to comment on whether any gender interaction between provider and participant occurred. Previous work regarding pain reporting suggests interactions in pain reporting based on gender roles and expectations. Our findings would be stronger if 1) we had a greater sample of providers and 2) we were able to assess a wider range of preference; that is, if a provider had a stronger preference for CT for example. Alternatively, our findings may have been influenced by the categorical response options provided to both participants and providers regarding their preference for an intervention. Additionally, while we asked participants about their expectations for pain relief with the intervention they received, we did not ask them about previous experience(s) with any of the interventions. Previous experience with any of the interventions could potentially have influenced their expected pain relief with a given intervention.
Our study included participants with experimentally induced acute LBP, and therefore, these results may not be replicable in clinical populations, as the average pain intensity reported was low and only included pain of presumably muscular origin. While others have previously validated experimental preclinical models of acute LBP (REFS), we recognize that the pain experience of an individual with chronic pain who may report heightened emotional and/or cognitive distress associated with his or her pain may be different than those with acute musculoskeletal pain, particularly when participants were informed prior to enrolling in the study that their pain was expected to be short in duration. Additional studies investigating complex interactions between provider preference, patient preference, and expectations are needed in clinical populations to further advance our understanding of these nonspecific treatment effects. Further, our study looked at a single time point before and after a single intervention, and participants were informed prior to enrollment that their pain would likely last up to 1 week. Therefore, it is plausible that the amount of expected pain relief expected may have been influenced by the knowledge that their pain would resolve shortly. The dynamic evolution of preferences and expectations and their effects of pain relief need to be further evaluated over the course of treatment (i.e., several treatments provided over several weeks).
Acknowledgment
This work was supported by the National Institutes of Health NCMRR and NINDS K12 HD055929 (MJA, JMB), NCCIH R01 AT006334 (MDB, JEB), and NCCIH F32 AT007729 (CWG).
Disclosure
The authors report no conflicts of interest in this work.
References
Bishop MD, Mintken PE, Bialosky JE, Cleland JA. Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. J Orthop Sports Phys Ther. 2013;43(7):457–465. | ||
Bishop MD, Bialosky JE, Cleland JA. Patient expectations of benefit from common interventions for low back pain and effects on outcome: secondary analysis of a clinical trial of manual therapy interventions. J Man Manip Ther. 2011;19(1):20–25. | ||
Puentedura EJ, Cleland JA, Landers MR, Mintken PE, Louw A, Fernandez-de-Las-Penas C. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. J Orthop Sports Phys Ther. 2012;42(7):577–592. | ||
Brewin CR, Bradley C. Patient preferences and randomised clinical trials. BMJ. 1989;299(6694):313–315. | ||
Eiring O, Landmark BF, Aas E, Salkeld G, Nylenna M, Nytroen K. What matters to patients? A systematic review of preferences for medication-associated outcomes in mental disorders. BMJ. 2015;5(4):e007848. | ||
Miller FG, Brody H. A critique of clinical equipoise: therapeutic misconception in the ethics of clinical trials. Hastings Cent Rep. 2003;33(3):19–28. | ||
Cook C, Sheets C. Clinical equipoise and personal equipoise: two necessary ingredients for reducing bias in manual therapy trials. J Man Manip Ther. 2011;19(1):55–57. | ||
Cook C, Learman K, Showalter C, Kabbaz V, O’Halloran B. Early use of thrust manipulation versus non-thrust manipulation: a randomized clinical trial. Man Ther. 2013;18(3):191–198. | ||
Bishop MD, Horn ME, George SZ, Robinson ME. Self-reported pain and disability outcomes from an endogenous model of muscular back pain. BMC Musculoskelet Disord. 2011;12:35. | ||
NCCIH. Mind and Body Practices. Bethesda, MD: NCCIH; 2015. | ||
Monroe CM. The effects of therapeutic touch on pain. J Holist Nurs. 2009;27(2):85–92. | ||
Mancini F, Nash T, Iannetti GD, Haggard P. Pain relief by touch: a quantitative approach. Pain. 2014;155(3):635–642. | ||
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. | ||
Parsons S, Harding G, Breen A, et al. The influence of patients’ and primary care practitioners’ beliefs and expectations about chronic musculoskeletal pain on the process of care: a systematic review of qualitative studies. Clin J Pain. 2007;23(1):91–98. | ||
Carroll LJ, Lis A, Weiser S, Torti J. How well do you expect to recover, and what does recovery mean, anyway? Qualitative study of expectations after a musculoskeletal injury. Phys Ther. 2016;96(6):797–807. | ||
Main CJ, Foster N, Buchbinder R. How important are back pain beliefs and expectations for satisfactory recovery from back pain? Best Pract Res Clin Rheumatol. 2010;24(2):205–217. | ||
Franco MR, Ferreira ML, Ferreira PH, Maher CG, Pinto RZ, Cherkin DC. Methodological limitations prevent definitive conclusions on the effects of patients’ preferences in randomized clinical trials evaluating musculoskeletal conditions. J Clin Epidem. 2013;66(6):586–598. | ||
Klojgaard ME, Manniche C, Pedersen LB, Bech M, Sogaard R. Patient preferences for treatment of low back pain-a discrete choice experiment. Value Health. 2014;17(4):390–396. | ||
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. | ||
Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26(13):1418–1424. | ||
Myers SS, Phillips RS, Davis RB, et al. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 2008;23(2):148–153. | ||
Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ. 2012;345:e6572. | ||
Lateef F. Patient expectations and the paradigm shift of care in emergency medicine. J Emerg Trauma Shock. 2011;4(2):163–167. | ||
George SZ, Robinson ME. Preference, expectation, and satisfaction in a clinical trial of behavioral interventions for acute and sub-acute low back pain. J Pain. 2010;11(11):1074–1082. | ||
Vase L, Robinson ME, Verne GN, Price DD. The contributions of suggestion, desire, and expectation to placebo effects in irritable bowel syndrome patients. An empirical investigation. Pain. 2003;105(1–2):17–25. | ||
Pollo A, Amanzio M, Arslanian A, Casadio C, Maggi G, Benedetti F. Response expectancies in placebo analgesia and their clinical relevance. Pain. 2001;93(1):77–84. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.