Back to Journals » International Journal of General Medicine » Volume 16
The Incidence and Risk Factors of Acute Myocardial Infarction Among Patients with Gastrointestinal bleeding: A Retrospective Study
Authors Yang Y , Xue Y, Li W, Yang F, Guo X, Zhou Z
Received 6 June 2023
Accepted for publication 25 August 2023
Published 8 September 2023 Volume 2023:16 Pages 4091—4097
DOI https://doi.org/10.2147/IJGM.S422358
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yan Yang,1 Yaofeng Xue,1 Wenjing Li,1 Fang Yang,1 Xiaohe Guo,1 Zhongyin Zhou2
1Department of Gastroenterology, The First Affiliated Hospital of Xinxiang Medical University, Weihui, People’s Republic of China; 2Department of Gastroenterology, Renmin Hospital of Wuhan University, Hubei Key Laboratory of Digestive System Disease, Wuhan, People’s Republic of China
Correspondence: Zhongyin Zhou, Department of Gastroenterology, Renmin Hospital of Wuhan University, Hubei Key Laboratory of Digestive System Disease, No. 238, Jiefang Road, No. 99, Zhangzhidong Road, Wuchang District, Wuhan, 430060, People’s Republic of China, Tel +86-13871029766, Fax +86 027-88043958, Email [email protected]
Purpose: Patients with gastrointestinal bleeding (GIB) and acute myocardial infarction (AMI) have higher mortality than that with either GIB or AMI alone. The aims of this study were to determine the incidence and risk factors of AMI in patients with GIB.
Patients and Methods: From January 2015 to January 2018, we retrospectively studied 1287 patients with GIB in Renmin Hospital of Wuhan University. Various demographic, laboratory and outcome data were reviewed by charts.
Results: Thirty-seven patients had AMI and were placed in AMI group and the rest 1250 patients were in non-AMI group. Patients with AMI were more likely to be older than 70 years, have hypertension, coronary heart disease, chronic kidney disease, and have the recent history of taking aspirin before admission. The ROC curve of hemoglobin (HB) on admission showed area under curve was 0.762, the optimal cut-off value is 76.5g/L. Logistic regression analysis showed that age ≥ 70 years old, coronary heart disease and HB < 76.5g/L on admission were independent risk factors of AMI in patients with GIB. The mortality of patients during hospitalization in AMI group and in non-AMI group were 45.95% and 5.48%, respectively. Patients who displayed a history of liver disease and HB < 76.5g/L on admission had a higher death rate.
Conclusion: GIB increased the risk of subsequent AMI, especially in patients over 70 years old, with history of coronary heart disease and HB < 76.5g/L on admission. Patients with GIB and AMI who had history of liver disease and HB < 76.5g/L on admission had a higher mortality rate. Clinicians should identify the high-risk patients of AMI among the GIB population early and prevent AMI.
Keywords: cardiovascular, evaluation, gastrointestinal hemorrhages, prognosis
Introduction
Gastrointestinal bleeding (GIB) is common and associated with substantial morbidity, mortality, and health care costs. It is reported that the mortality rate is 2–10%.1,2 GIB can produce hypovolemia, hypotension, and diminished oxygen-carrying capacity, cause reflex tachycardia and increase myocardial oxygen consumption, and even lead to acute myocardial infarction (AMI). Moscucci and Cappell et al found the incidence of AMI in patients with GIB was 1–4%, while the incidence of AMI after severe GIB was nearly 12%.3,4 The mortality rate of patients with GIB combined with AMI will increase significantly.
Furthermore, physicians face a dilemma about the treatment. AMI guidelines recommend an initial high oral loading dose of dual antiplatelet therapy (DAPT), including aspirin (150–300mg), a P2Y12 inhibitor (60mg of prasugrel, 180mg of ticagrelor or 600mg of clopidogrel), and thrombolytic medications.5,6 However, these medications can aggravate GIB. Therefore, it is very important to accurately evaluate the condition of GIB and prevent AMI.
At present, there are many studies on the risk factors of AMI in patients with GIB. Prior studies showed that those patients with lower blood pressure and lower HB on admission, older age, a history of coronary heart disease and severe primary illnesses had a greater risk of AMI.7–10 GIB can lead to a decrease in hemoglobin. Low hemoglobin levels could increase the risk of adverse outcomes in patients with AMI. Longer symptom duration is associated with a lower admission hemoglobin level.11,12 However, there is still limited research on how low hemoglobin levels are more likely to precipitate AMI. In 2005, Bellotto et al found that HB ≤8.2g/dL was a significant risk factor for myocardial necrosis in patients with GIB. This study was a prospective study, but the number of cases was only 227.7 Therefore, the aim of the present study is to further explore the incidence, the relationship between hemoglobin and the risk of the subsequent AMI and risk factors of AMI in patients with GIB.
Materials and Methods
Patients
This was a retrospective analysis of hospitalized patients with GIB during the January 2015 to January 2018 period at Renmin Hospital of Wuhan University. The inclusion criterion was confirmed GIB patients. The study was approved by the ethics committee of Renmin Hospital of Wuhan University. The informed consent was obtained from all patients in this study. In addition, the research followed the guidelines outlined in the Declaration of Helsinki. GIB includes upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). The diagnostic criteria are: (1) with obvious symptoms: hematemesis, black stool, bloody stool, with or without peripheral circulation disorders such as dizziness, paleness and hypotension. (2) no obvious symptoms: positive in occult blood test or gastric occult blood test. Diagnostic criteria for AMI: acute myocardial injury [serum cardiactroponin (cTn) increases and/or falls back, and is higher than the upper normal limit normal (99th percentile of the upper limit of reference values) at least once], clinical evidence of concurrent acute myocardial ischemia, including: (1) symptoms of acute myocardial ischemia; (2) new ischemic ECG changes; (3) novel pathogenic Q wave; (4) new imaging evidence of viable myocardium loss or regional wall motion abnormality; (5) coronary artery thrombosis confirmed by coronary angiography or intracavity imaging or autopsy.13
Data Collection
Clinical data were collected for each patient. Data include demographic information (eg, age and sex), concomitant illnesses (eg, hypertension, coronary heart disease, diabetes, chronic kidney or liver disease, history of cerebral infarction, history of peptic ulcers, the recent history of taking aspirin, clopidogrel and warfarin before admission, HB on admission, the prognosis of all patients.
Statistical Analysis
Continuous data were presented as mean ± SD. The differences in baseline characteristics and comorbid variables between the two groups were assessed using t-test for continuous variables and χ2 tests for categorical variables. Logistic regression analysis was conducted to evaluate the risk factors of AMI in patients with GIB and in‑hospital mortality. In order to evaluate the specific declined degree of HB that can lead to AMI in patients with GIB, the ROC curve was drawn, and the area under the curve (AUC) was calculated. AUC = 1.0 was the most ideal diagnostic value, and AUC <0.5 indicated no diagnostic value. The optimal diagnostic cut-off value was obtained according to the principle of maximum Youden index. Data were analyzed using the SPSS 21.0 statistical software and P < 0.05 was considered statistically significant.
Result
Patient Characteristics
Based on both inclusion and exclusion criteria, 1287 patients with GIB were included in the current study. Among the 1287 patients, 37 patients were complicated with AMI, which was defined as the AMI group. The incidence of AMI in patients with GIB was 2.9%. The AMI group included 30 males and 7 females, aged 37 to 87 years, with an average of (70.8±11.4) years old. There were 1250 patients without AMI, defined as the non-AMI group, included 854 males and 396 females, aged 14 to 99 years, with an average of (60.2±16.8) years old. The general characteristics of patients are summarized in Table 1. The basic clinical data of two groups were analyzed and compared respectively. The results showed that there were statistically significant differences in age ≥70 years old, history of hypertension, coronary heart disease, chronic kidney disease and the recent history of taking aspirin before admission (P < 0.05). However, there were no significant difference in gender, history of peptic, cerebral infarction, chronic liver disease, diabetes, recent history of taking clopidogrel and warfarin before admission (P > 0.05).
 |
Table 1 Patient Demographic Characteristics |
Risk Factors of Acute Myocardial Infarction in Patients with Gastrointestinal Bleeding
The ROC curve was drawn according to the HB value on admission (Figure 1), the AUC was 0.762, the optimal diagnostic cutoff was 76.5 g/L, and the corresponding sensitivity and specificity were 64.6% and 75.7%, respectively.
 |
Figure 1 ROC curve of HB on admission. |
Logistic regression analysis was used to determine the independent risk factors for AMI in patients with GIB. The variables showing statistically significant differences between the AMI and non-AMI groups were selected for analysis (Table 2). The included variables were age ≥70 years old, a history of hypertension, coronary heart disease, chronic kidney disease, the recent history of taking aspirin before admission and HB <76.5g/L on admission. Interestingly, age ≥70 years old (OR, 4.372; 95% CI, 1.917–9.970, P = 0.000), coronary heart disease (OR, 2.927; 95% CI, 1.336–6.414, P = 0.007) and HB <76.5g/L on admission (OR, 4.909; 95% CI, 2.262–10.656, P = 0.000) were significantly associated with AMI in patients with GIB.
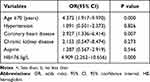 |
Table 2 Logistic Regression Analysis of Risk Factors for AMI |
Risk Factors of in‑hospital Mortality in Patients with Gastrointestinal Bleeding and Acute Myocardial Infarction
Of all patients, there were 84 patients died during hospitalization, and the mortality rate was 6.72%. In AMI group, 17 patients died during hospitalization, with a mortality rate of 45.95%, which was significantly higher than that in non-AMI group (VS 5.48%, P < 0.001).
To explore the risk factors of in‑hospital mortality, basic clinical data of the survival group and death group were analyzed and compared, respectively (Table 3). The results showed that patients with history of liver disease (P = 0.000) and HB <76.5g/L on admission (P = 0.000) had a higher death rate.
 |
Table 3 The Basic Clinical Data of the Survival Group and Death Group |
Discussion
This study strongly indicates that GIB can induce AMI, and GIB combined with AMI leads to higher in-hospital mortality. Age ≥70 years old, coronary heart disease and HB <76.5g/L on admission are significant risk factors of AMI in patients with GIB. Patients who had history of liver disease and HB <76.5g/L on admission had a higher death rate. These findings provide a basis for improving the clinical management of such patients.
GIB is more common in patients with AMI, which is mainly caused by the combination of aspirin, clopidogrel and anticoagulant drugs. Dual antiplatelet therapy can significantly reduce mortality, the incidence of adverse ischemic events, short-term and long-term complications after PCI and the incidence of other major adverse cardiovascular events, but it also undoubtedly increases the risk of GIB.14,15 It has been reported that the incidence of in-hospital GIB in patients with AMI was 1.19%, even up to 10.4% within 4 years in STEMI patients after primary PCI.16,17 Severe bleeding after acute coronary syndrome (ACS) can increase the mortality by 5 times, GIB was an independent predictor of mortality in patients with AMI.18,19
GIB is a common, costly, and potentially life-threatening disease, and can lead to AMI. The mechanism is as follows: Firstly, GIB can produce hypovolemia, hypotension, diminished oxygen-carrying capacity and low myocardial perfusion. Secondly, GIB can activate the sympathetic nervous system, which is able to increase heart rate and the demand for myocardial oxygen and worsen ischemia. Due to the imbalance of co-ordination of supply and demand, the myocardial injury is aggravated. In addition, the activation of sympathetic system leads to constriction of the coronary arteries and increases the risk of rupture of unstable plaques in the coronary arteries. Thirdly, after gastrointestinal bleeding, the systemic coagulation system is activated, promoting the formation of blood clots. Fourth, blood transfusion treatment is often required after massive GIB, which will also aggravate myocardial damage.
Generally speaking, GIB that leads to AMI is massive and urgent, and the mortality is high. The symptoms and signs of AMI are easy to be masked and neglected, and most of them have no typical symptoms such as chest pain. It has been reported that electrocardiogram expression is non-ST elevation myocardial infarction mostly.20 A previous study has shown that among patients in ICU due to GIB, the prevalence of AMI ranges from 30% to 49%, and the overall mortality is 5–10%. Other researches have suggested that the incidence of AMI in patients with UGIB is 1–14%.7–9 In this retrospective study, among 1287 patients with GIB, 37 patients developed AMI and 84 patients died, the incidence rate was 2.9%, and the total in‑hospital mortality rate was 6.5%, which was consistent with previous reports. In AMI group, 18 patients died, the mortality was as high as 48.6%. The basic clinical data of were analyzed and compared respectively to evaluate risk factors of in-hospital mortality. The result discovered that patients with history of liver disease (P = 0.000) and HB <76.5g/L on admission (P = 0.000) had a higher death rate. Possible reasons for analysis are as follows: patients over 70 years old are the majority and have many basic diseases. Therefore, the body’s ability to fight disease is very low. In addition, some patients give up treatment due to economic difficulties. For patients with liver disease, the most common cause of bleeding is esophageal and gastric varices bleeding (EGVB). EGVB is characterized by acute onset, severe bleeding, recurrent attacks, and difficulty in hemostasis. The prognosis is poor.
As shown above, age ≥70 years old, coronary heart disease and HB <76.5g/L on admission were independent risk factors for AMI in patients with GIB. Wu et al found that women and patients <65 years old had twice the risk of developing an AMI after UGIB than did CAD patients who do not have UGIB.21 Nevertheless, there were other studies reported that older age was a risk factor and simultaneous UGIB and AMI occurred most often in men.9,10 Iser et al retrospectively analyzed the clinical data of 156 patients with UGIB and found that patients with hemodynamic instability, history of coronary heart disease and age over 65 years old were more prone to acute myocardial injury.22 In 2015, Wu et al found UGIB was the most likely factor that contributed to AMI.21 As we all know, GIB can lead to decreased hemoglobin, but less research has been done on how low hemoglobin can induce acute myocardial infarction. Bellotto et al studied 227 patients with GIB and found that HB ≤8.2 g/dL was a significant risk factor for myocardial necrosis.7 In this retrospective study, we found that one of the independent risk factors for AMI in patients with GIB was HB <76.5g/L on admission.
GIB complicated with AMI seriously threatens the life of patients. Therefore, for patients with GIB, especially those over 70 years old, with history of coronary heart disease and HB <76.5g/L on admission, the patient’s condition should be accurately evaluated. Electrocardiogram and myocardial injury markers should be closely monitored to detect AMI as early as possible and in time. In addition, correct and effective treatment should be adopted to avoid adverse events. Hemostatic and vasoconstrictors should be applied cautiously. Furthermore, antiplatelet therapy should be modified reasonably. Blood volume needs to be supplemented to maintain HB >70g/L. For patients with AMI and GIB, the advantages and disadvantages should be weighed. Antiplatelet drugs, anticoagulants and drugs to improve coronary circulation need to be used reasonably to ensure myocardial perfusion.
However, there are some limitations in this study. First, this was a retrospective analysis and there were inherent shortcomings. Alcohol and cigarettes were not discussed in the study. Second, with serious conditions, these patients with AMI and GIB were usually treated with conservative therapy. Coronary angiography, coronary computed tomography angiography (CTA) and endoscopy were rarely performed. As a result, the heart conditions were mainly assessed by electrocardiogram, the levels of blood myocardial enzymes and BNP. Besides, the cause of GIB in some patients was unknown. Third, this study sample size was small and existed geographical limitations. The clinical data used for analysis were obtained from a single-center institution, and the representativeness of the sample was limited. The single-center study is prone to bias. Relatively few patients with AMI and GIB were included. Finally, variables such as vital signs and laboratory tests were mainly derived from the data of patients within 24 hours after admission, which may cause a certain degree of selection bias. There were few laboratory tests in this study, and the present findings should be interpreted with caution. We recommend further research to provide more evidence.
Conclusion
Our results suggest the need to pay careful attention to the cardiac status of patients with gastrointestinal bleeding, especially those over 70 years old, with history of coronary heart disease and HB <76.5g/L on admission. GIB complicated with AMI seriously threatens the life of patients. A history of liver disease and HB <76.5g/L on admission were associated with high mortality in patients with GIB and AMI. Consequently, physicians need to use earlier and more aggressive intervention to detect and prevent AMI in patients with GIB.
Acknowledgments
There was no industry involvement in the design, conduct, or analysis of the study. This work received grant support from: The Medical Science and Technology Research Program of Henan Province (grant no. LHGJ20200502), The Scientific and Technological Project of Hubei Province (grant no.2015BKB013).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Albeldawi M, Qadeer MA, Vargo JJ. Managing acute upper GI bleeding, preventing recurrences. Cleve Clin J Med. 2010;77(2):131–142. doi:10.3949/ccjm.77a.09035
2. Lanas A, García-Rodríguez LA, Polo-Tomás M, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104(7):1633–1641. doi:10.1038/ajg.2009.164
3. Moscucci M, Fox KAA, Cannon CP, et al. Predictors of major bleeding in acute coronary syndromes: the global registry of acute coronary events (GRACE). Eur Heart J. 2003;24(20):1815–1823. doi:10.1016/s0195-668x(03)00485-8
4. Cappell MS. Gastrointestinal bleeding associated with myocardial infarction. Gastroenterol Clin North Am. 2000;29(2):423–444. doi:10.1016/S0889-8553(05)70121-7
5. Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST⁃segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(10):766–783. doi:10.3760/cma.j.issn.0253-3758.2019.10.003
6. Sousa-Uva M, Neumann F-J, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2019;55(1):4–90. doi:10.1093/ejcts/ezy289
7. Bellotto F, Fagiuoli S, Pavei A, et al. Anemia and ischemia: myocardial injury in patients with gastrointestinal bleeding. Am J Med. 2005;118(5):548–551. doi:10.1016/j.amjmed.2005.01.026
8. Bhatti N, Amoateng-Adjepong Y, Qamar A, et al. Myocardial infarction in critically III patients presenting with gastrointestinal hemorrhage: retrospective analysis of risks and outcomes. Chest. 1998;114(4):1137–1142. doi:10.1378/chest.114.4.1137
9. Emenike E, Srivastava S, Amoateng-Adjepong Y, et al. Myocardial infarction complicating gastrointestinal hemorrhage. Mayo Clin Proc. 1999;74(3):235–241. doi:10.4065/74.3.235
10. Zeidman A, Fradin Z, Blecher A, et al. Anemia as a risk factor for ischemic heart disease. Isr Med Assoc J. 2003;6(1):16–18. doi:10.1016/S0953-6205(03)91274-X
11. Shacham Y, Leshem‐Rubinow E, Ben‐Assa E, et al. Lower admission hemoglobin levels are associated with longer symptom duration in acute ST‐elevation myocardial infarction. Clin Cardiol. 2014;37(2):73–77. doi:10.1002/clc.22215
12. Pei J, Wang X, Chen P, et al. Hb levels and sex differences in relation to short-term outcomes in patients with acute myocardial infarction. Front Cardiovasc Med. 2021;8:653351. doi:10.3389/fcvm.2021.653351
13. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):
14. Lv M, Zheng X, Wu T, et al. A new score for predicting acute gastrointestinal bleeding in patients administered oral antiplatelet drugs. Front Pharmacol. 2021;11:571605. doi:10.3389/fphar.2020.571605
15. Guo Y, Wei J. Clinical outcomes of various continued antiplatelet therapies in patients who were administered DAPT following the implantation of drug-eluting stents and developed gastrointestinal hemorrhage. Exp Ther Med. 2016;12(2):1125–1129. doi:10.3892/etm.2016.3378
16. Shi W, Fan X, Yang J, et al. In-hospital gastrointestinal bleeding in patients with acute myocardial infarction: incidence, outcomes and risk factors analysis from China acute myocardial infarction registry. BMJ Open. 2021;11(9):e044117. doi:10.1136/bmjopen-2020-044117
17. Xue WQ, Cai YX, Liu J, et al. Acute ST-elevation myocardial infarction after upper gastrointestinal bleeding: a clinical dilemma of antiplatelet therapy. Chin Med J. 2018;131(3):370–371. doi:10.4103/0366-6999.223863
18. Manoukian SV, Feit F, Mehran R, et al. Impact of major bleeding on 30-day mortality and clinical outcomes in patients with acute coronary syndromes: an analysis from the ACUITY Trial. J Am Coll Cardiol. 2007;49(12):1362–1368. doi:10.1016/j.jacc.2007.02.027
19. Eikelboom JW, Mehta SR, Anand SS, et al. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006;114(8):774–782. doi:10.1161/CIRCULATIONAHA.106.612812
20. Lee CT, Huang SP, Cheng TY, et al. Factors associated with myocardial infarction after emergency endoscopy for upper gastrointestinal bleeding in high-risk patients: a prospective observational study. Am J Emerg Med. 2007;25(1):49–52. doi:10.1016/j.ajem.2006.04.013
21. Wu CJ, Lin HJ, Weng SF, et al. Acute myocardial infarction risk in patients with coronary artery disease doubled after upper gastrointestinal tract bleeding: a nationwide nested case-control study. PLoS One. 2015;10(11):e0142000. doi:10.1371/journal.pone.0142000
22. Iser DM, Thompson AJV, Sia KK, et al. Prospective study of cardiac troponin I release in patients with upper gastrointestinal bleeding. J Gastroenterol Hepatol. 2008;23(6):938–942. doi:10.1111/j.1440-1746.2007.04940.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
