Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
The Impact of Using Donor Sperm After ICSI Failure in Severe Oligozoospermia on Male Mental Health and Erectile Function
Authors Yin Y, Wang K , Xu Y, Huang X , Zheng J, Fan Y, Bai J
Received 17 September 2023
Accepted for publication 4 December 2023
Published 4 January 2024 Volume 2024:17 Pages 21—28
DOI https://doi.org/10.2147/JMDH.S440778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ying Yin,1 Ke Wang,1,2 Yan Xu,2,3 Xin Huang,1 Jinxia Zheng,1 Yuping Fan,1 Jie Bai1
1Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, 200092, People’s Republic of China; 2School of Medicine, Tongji University, Shanghai, 200092, People’s Republic of China; 3School of International Medical Technology, Sanda University, Shanghai, 201206, People’s Republic of China
Correspondence: Ke Wang, Email [email protected]
Objective: To analyze the mental health and erectile function status of men using sperm donor during pregnancy after ICSI failure in severe oligoasthenospermia and to provide reference for clinical implementation of more targeted psychological intervention and nursing for this group.
Methods: A total of 410 sterile men who received assisted pregnancy treatment in our hospital from December 2020 to December 2022 and met the inclusion and exclusion criteria were collected as the study subjects. Among them, 68 patients with severe oligoasthenospermia who used donor assisted pregnancy after ICSI failure were used as the study group. Sixty-eight patients with severe oligoasthenospermia who continued to receive ICSI assisted pregnancy were matched by propensity score 1:1 as control group. General data questionnaire, self-rating Anxiety Scale (SAS), self-rating Depression Scale (SDS), Chinese version of perceived Stress Scale (CPSS) and International Erectile Function Index Rating Scale (IIEF-5) were used to conduct a cross-sectional investigation to compare the mental health and erectile function status of the two groups.
Results: There were statistical differences in age and occupational status between the two groups before PSM (P < 0.05), but there was no statistical significance in social demographic data between the two groups after matching (P > 0.05). The incidence of anxiety, depression, stress and erectile dysfunction (ED) in the study group was higher than that in the control group, and there were statistical differences between the two groups (P < 0.05).
Conclusion: The use of donor sperm to assist pregnancy has a great impact on the mental health and erectile function of infertile men. Medical personnel should pay attention to the mental health and erectile function of these men, and formulate targeted measures to help these patients actively cope with infertility, so as to improve the life and marriage quality of this group and improve their mental health status.
Keywords: sterile male, supply semen, erectile function, mental health, propensity score
Introduction
In recent years, the incidence of infertility has shown an increasing trend year by year. At present, infertility population accounts for about 10% to 15% of the population of childbearing age, and male infertility patients account for about 40%, among which 10% to 20% of infertility factors are severe oligospermia, teratospermia or azoospermia.1 Intracytop lasmic sperm injection (ICSI) technology provides a new way for severe oligoasthenospermia patients to become pregnant. However, some patients choose artificial insemination with donor sperm (AID) after repeated failure of ICSI. Due to the source of sperm, couples receiving AID for pregnancy will have more complex psychological problems, among which anxiety, depression and other psychological problems are more common.2,3 Erectile dysfunction (ED) is the most common chronic private disease in male sexual dysfunction. Studies showed that 85% to 90% of ED patients were caused by psychological problems.4 Mental health is an intact state of reasonable cognition, emotional stability and adaptation to changes in the process of growth and development. The main evaluation indicators include anxiety, depression and pressure.5
At present, there is little attention on the mental health and erectile function of patients who choose to donate sperm to assist pregnancy, and fewer studies on the mental health and erectile function of men who switch to donor sperm after ICSI failure, and such patients have a high incidence of negative emotions due to sudden changes in sperm sources, family pressure, social ethics and other reasons, and seriously affect the relationship between husband and wife and quality of life. Therefore, this study intends to conduct a questionnaire survey on infertile men on the day of the operation of assisted pregnancy after changing the source of sperm. The social demographic data of the men who changed to AID pregnancy after two or more ICSI failures and the men who continued to receive ICSI assisted pregnancy were eliminated by the propensity score matching method, and the mental health status and erectile function of the two groups of patients were compared, to explore the influence of sperm donation on infertile men and to provide reference for clinical treatment and more targeted psychological intervention and nursing.
Objects and Methods
Objects
A total of 410 infertile male patients who received assisted pregnancy treatment in the Department of Assisted Reproductive Medicine of the First Maternal and Infant Health Hospital Affiliated to Tongji University from December 2020 to December 2022 were selected as the study objects by convenience sampling method. Sixty-eight infertile male patients who received ICSI and changed to AID were part of the study group. Three hundred and forty-two infertile male patients with ICSI assisted pregnancy were selected as the control group. None of the subjects had sexual function problems with erectile function before being investigated.
Inclusion criteria: (1) Meet the diagnostic criteria for severe oligoasthenospermia in the Guidelines for Diagnosis and Treatment of Androgenic Diseases and Expert Consensus in China,6 sperm concentration ≤5×106/mL, or no class a forward motile sperm, and class b motile sperm ≤5%; (2) Male severe oligoasthenospermia as the main indication to be included in ICSI treatment; (3) The chromosome detection of both husband and wife is normal; (4) ICSI assisted egg retrieval ≥2 cycles (≥5 eggs per cycle), no pregnancy after transplantation; (5) Have basic communication skills, read without barriers, fully explain the purpose of this study and agree to participate in this study voluntarily. Exclusion criteria: (1) azoospermia patients; (2) Patients who use frozen sperm, undergo testicular puncture or open testicular extraction; (3) Patients with serious diseases, penile trauma and surgical history; (4) Patients with high blood pressure, diabetes, etc., which have a significant impact on sexual function; (5) The relationship with sexual partners is not compatible, there are other sexual function problems that affect erectile function: such as low sexual desire; (6) Long-term use of psychotropic drugs may affect erectile function of patients; (7) Poor compliance, unable to cooperate with the completion of the questionnaire. This study strictly adhered to the indications and complied with various laws, regulations and ethical principles related to sperm donation and assisted pregnancy, and was approved by the Ethics Committee of the First Maternal and Infant Health Hospital affiliated to Tongji University (Ethics number: KS2313).
Methods
Survey Tools
Socio-demographic data. Questionnaire designed by oneself, including age, height, weight, occupation status, household registration type, education level, family income, education level, infertility years, whether there are children.
Self-rating Depression Scale (SDS) and Self-rating Anxiety Scale (SAS).7,8 It was compiled by Zung and used to evaluate depression and anxiety symptoms respectively, both of which included 20 items. A 4-level score was used according to the frequency of symptoms in the last week, and each frequency was assigned 1–4 points. The higher the score, the more serious the symptoms were. According to the results of Chinese norm, the scale was divided into 53 points according to SDS standard, 53 ~ 62 points were classified as mild depression, 63 ~ 72 points were classified as moderate depression, and >72 points were classified as severe depression. The SAS standard score is 50 points, of which 50 ~ 59 is classified as mild anxiety, 60 ~ 69 is classified as moderate anxiety, and >70 and above is severe anxiety. The two scales have good reliability and validity.
The Chinese version of perceived stress scale (CPSS).9 The scale was developed by Cohen Equals in 1983 to assess an individual’s perceived level of stress. Chinese scholar Yang Tingzhong equal to 2003 revision. The Chinese version of the perceived Stress scale contains 14 items, covering two dimensions of tension and loss of control. Likert scale scores were used, with 1 representing “never” and 5 representing “always”. The total scale score between 11 and 26 represented a low perceived stress level, 27 to 41 represented a moderate level, and 42 or above represented a high level. Yang Tingzhong et al showed that Cronbach’s alpha of CPSS was 0.780 and had high structural validity.
International Index of Erectile Function-5 (IIEF-5).10 Five questions were used to evaluate erectile function, with a score of >21 as normal erectile function, 12 to 21 as mild, 8 to 11 as moderate, and less than 5 to 7 as severe.
Sex hormone levels. 3mL fasting venous blood was collected from two groups of subjects, and serum was separated and obtained, and the serum total testosterone level was determined by chemiluminescence method.
Investigation Methods
This study was a cross-sectional study. The data of patients who met the criteria were collected by male specialist nurses with the consent of the patients. The data of the study group was collected on the day of operation after switching to sperm donation to assist pregnancy, while the data of the control group was collected on the day of operation during the third cycle of ICSI assisted pregnancy. The purpose and steps of the study were explained with unified guidance, and the patients were instructed to respond according to their actual situation, fill in the questionnaire on the spot, and give enough time and an independent environment to check for no missing items before recycling. A total of 428 questionnaires were sent out, and 410 were effectively collected, with an effective rate of 95.79%.
Statistical Methods
SPSS26.0 software was used for data processing and analysis. Kolmogorov Smirnov test was used for the normal distribution. Those who met the normal distribution in quantitative data were represented by mean±standard deviation ( ) and the number of use cases of categorical variables n (%). Independent sample t-test was used for measurement data. The count data were compared by x2 test or Fisher test. In this study, a 1:1 propensity score matching (PSM) method was used to reduce the bias of observed variables and confounding factors on the treatment effect. The control range was 0.02. Matching items were subjects’ age and occupational status (other baseline measures did not differ statistically between the two groups). P < 0.05 was considered to be statistically significant.
) and the number of use cases of categorical variables n (%). Independent sample t-test was used for measurement data. The count data were compared by x2 test or Fisher test. In this study, a 1:1 propensity score matching (PSM) method was used to reduce the bias of observed variables and confounding factors on the treatment effect. The control range was 0.02. Matching items were subjects’ age and occupational status (other baseline measures did not differ statistically between the two groups). P < 0.05 was considered to be statistically significant.
Results
Comparison of Social Demographic Data Between the Two Groups Before and After Matching
During the study period, a total of 410 infertile men who met the criteria of allocation were collected, including 68 patients who changed to AID pregnancy assistance treatment and 342 patients who continued ICSI pregnancy assistance treatment. There were statistical differences in age and occupational status between the two groups (P < 0.05). PSM method was used to match patients by age and occupational status, and 136 patients were finally included in the analysis, 68 patients in the control group and 68 patients in the study group, and the baseline data of the two groups were not statistically significant (P > 0.05), as shown in Table 1.
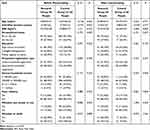 |
Table 1 Comparison of Social Demographic Data Between the Two Groups Before and After Matching [xˉ±S, n (%)] |
Comparison of the Incidence of Anxiety, Depression, Stress and erectile Dysfunction Between the Two Groups after Matching
The mental health status of the study group was significantly lower than that of the control group, the incidence of anxiety was 55.88%, the incidence of depression was 72.06% and the incidence of high stress was 42.65%. The incidence of erectile dysfunction in the study group was higher than that in the control group (82.35%). There was a statistical difference between the two groups (P < 0.05), as shown in Table 2.
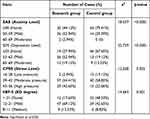 |
Table 2 Comparison of Incidence of Mental Health and Erectile Function Between the Two Groups After Matching [n (%)] |
Comparison of Serum Testosterone Level, Mental Health and Erectile Dysfunction Status Scores Between the Two Groups After Matching
There was no statistical significance in serum total testosterone level between the two groups (P > 0.05). The scores of mental health status in the study group were higher than those in the control group, and the scores of erectile function status were lower than those in the control group, with statistical differences between the two groups (P < 0.05), as shown in Table 3.
 |
Table 3 Comparison of Scores of Mental Health and Erectile Function Between the Two Groups After Matching [xˉ±S] |
Discussion
The Mental Health Status of Men Who Use Semen After ICSI Failure is Worrying
In this study, the scores of anxiety degree, depression degree and stress degree of men who used sperm donor after ICSI-assisted pregnancy failure were (50.63±4.33), (53.94±5.25) and (40.63±6.62), respectively. The incidence of anxiety, depression and stress accounted for 55.88%, 72.06 and 42.65% of this group, respectively, which was much higher than that of infertile men receiving other assisted pregnancy methods.11–14 Compared with azoospermia patients, the incidence of psychological disorders in the study group was still at a higher level.15,16 These men are faced with many challenges brought about by the change in the way of assisting pregnancy, such as the source of sperm and the lack of social role identification, as well as the lack of emotional vent channels and family support.17 In addition, often fluctuating semen routine objective test results may also have a negative impact on treatment.15 Therefore, it is necessary to provide appropriate psychological support and counseling for these patients.
There is a High Rate of Erectile Dysfunction in Men Who Use Sperm Donors After ICSI Failure
In this study, the score of erectile function of men using sperm donor after ICSI assisted pregnancy failure was (16.49±4.42), and the incidence of ED accounted for 82.35% of this group, which was much higher than the ED level of infertile men at home and abroad.18–20 85%~90% of ED patients are caused by psychological problems, known as psychogenic ED, and the incidence of ED is higher than that of other infertile men due to the high incidence of psychological problems in men who use sperm donors after ICSI failure. However, infertility caused by male factors will reduce the personal relationship and sexual life quality of infertile men,21,22 and may also lead to changes in the relationship, communication and understanding between couples, resulting in emotional expression disorders. Emotional expression mainly refers to the frequency of sex and love in the relationship between husband and wife, while infertility groups tend to have higher emotional expression disorders,23 resulting in a higher incidence of ED. Secondly, in the process of assisted pregnancy, the normal life of husband and wife is restricted by treatment, and sex is no longer an intimate behavior of husband and wife’s emotional transmission, but is regarded as a means of reproduction. Women need to fully cooperate with men to complete one or more sexual intercourse during ovulation, which will bring psychological pressure to men, lead to low sexual desire, and further produce resistance or rejection of sexual behavior, and increase the degree of ED; In addition, some patients only have sex during female ovulation,24,25 which leads to increased ED in men. In addition, some patients believe that their male role has failed, cannot accept physiological changes, close themselves and have psychological problems, and negative emotions are often more frequent during sexual life, resulting in the occurrence of ED.
Psychological Support for Donor Men After ICSI Failure
At present, clinical research focuses on the mental health status of azoospermia patients or the erectile function status of male infertility patients. There are few investigations and studies on patients who use sperm donor after ICSI failure in severe oligoasthenospermia. Due to sperm source problems and progeny blood problems, these patients have variable and complicated mental activities, and their mental health status is worrying. Although this group accounts for a relatively small proportion of the total population receiving assisted reproduction and assisted pregnancy treatment, this study focuses on clinical practice and has certain practical significance.
The problem of physical and mental disorders in androgenic diseases needs more attention and support from medical staff. In the treatment of such patients, we should pay attention to the construction of emotional bridge between husband and wife. Promote couples to receive psychological clinics and education together. Good family relationship has a positive impact on the psychological state of patients receiving assisted reproduction and assisted pregnancy.26 Companionship between husband and wife can provide more emotional identification and support, change patients’ sexual concept and awareness, and further improve the physical and mental health of such patients. At the same time, social support should be enhanced. Medical staff can adjust patients’ mentality and enhance their confidence through regular lectures on relevant knowledge, popular knowledge on diseases and sexual health, peer education and structured group psychotherapy.27 In addition, patients’ negative emotions should be alleviated. Medical staff should identify patients’ negative emotions in time and refer them to a psychotherapist for assistance in mindfulness-based stress reduction, relaxation training, music therapy, meditation resonance, singing pot healing and other measures. The Newman health system model28 can be adopted for patient management, and the traditional Chinese emotional guidance therapy29 can also be used to alleviate patients’ negative emotions.
Research Limitations
There are some limitations and limitations in this study. The sample size is relatively small, which may have sampling bias. The representativeness of a single center is insufficient, and the conclusion may have some limitations. The study design did not consider the influence of sociodemographic factors on the mental health and erectile function of infertile men and did not involve a pre - and post-control study of the mental health and erectile function of infertile men during the first cycle of assisted pregnancy and after changing the mode of assisted pregnancy. In the follow-up study, we will strive to cooperate with multiple centers in Shanghai, China, to collect more relevant medical records and conduct a more comprehensive investigation. In addition, on the basis of expanding the sample size, we will also include the influence of social demographic factors on the mental health and erectile function of these patients, and conduct a more comprehensive and in-depth study on infertile male patients.
Summary
The mental health status of men who used sperm donor after ICSI failure was worrying, the incidence of stress, anxiety and depression was high, and most patients had ED. It is suggested that medical staff should pay attention to the mental health and erectile function status of such people, identify the mental health problems of such patients as early as possible and take active nursing intervention measures, and refer psychotherapists and male doctors in time, in order to alleviate negative emotions, improve mental health status, reduce the incidence of ED, improve the quality of reproductive life and improve the relationship between husband and wife. On the basis of expanding the sample size, we will also include the influence of social demographic factors on the mental health and erectile function of these patients, and conduct a more comprehensive and in-depth study on infertile male patients.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Center of Shanghai first maternal and Infant Hospital (Ethics number: KS20182).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Funding
Shanghai Natural Science Foundation Project (23ZR1450200); Shanghai Municipal Health and Construction Commission Youth Project Fund (20204Y0132).
Disclosure
Ying Yin and Jinxia Zheng are co-first author. The authors declare no conflict of interest.
References
1. Barratt CLR, Bjorndahl L, De Jonge CJ, et al. The diagnosis of male infertility: an analysis of the evidence to support the development of global WHO guidance-challenges and future research opportunities. Hum Reprod Update. 2017;23(6):660–680. Chinese. doi:10.1093/humupd/dmx021
2. Chen C, Tian H, Zhang J, et al. Investigation on mental health status of patients with nonobstructive azoospermia of different etiology. South China Prevent Med. 2019;46(01):85–87+91. Chinese.
3. Liu L, Song G, Jiang RH, et al. Anxiety and depression status and influencing factors of 525 female patients with donor artificial insemination at file point. J Nurs. 2019;29(12):51–55.
4. Tianmin W, Zheng S, Che X, et al. Relationship between psychological and social support and stigma in patients with erectile dysfunction. J Sex Res. 2019;32(02):149–152.
5. Healthy China Action 2019–2030. Overall requirements, major actions and main indicators. Circ J. 2019;34(09):846–858.
6. Hallich O. Sperm donation and the right to privacy. N Biotechnol. 2017;23(2):107–120. doi:10.1080/20502877.2017.1355083
7. Xintian L. Medical Psychology. China Union Medical University Press; 2001:740–743.
8. Shaofei H, Wang H. Investigation on psychological state of elderly infertile women before assisted reproduction and pregnancy. J Fam Plann. 2019;29(08):1568–1573. Chinese.
9. Zhang Q, Anuo L, Jiang Y, et al. Potential categories of perceived stress and its relationship with professional identity among nurses with low seniority in Anhui province. Med Soc. 2012;35(10):107–112.
10. Rhoden EL, Telöken C, Sogari PR, Vargas Souto CA. Teloken C,sogari pr,et al.The use of the simplified international index of erectile function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res. 2002;14(4):245. doi:10.1038/sj.ijir.3900859
11. Singh V, Bhirud YR, Lele P, A survey of anxiety and depression in 752 cases of male infertility. Aerosp Med. 2015;26(11):1389–1390.
12. Ma Y, Lu Z, Qiang M. Effect of male anxiety and stress on methylation of sperm imprinting gene. J China Med Univ. 2018;32(08):589–593+595. Chinese.
13. Jianxiong M, Wang B, Dang J, et al. Relationship between erectile function and mental state in male infertility patients. Chinese J Androl. 2017;23(07):609–614.
14. Abolghasemi A, Rajabi S, Sheikhi M, Kiamarsi A, Sadrolmamaleki V. Comparison of resilience, positive/negative affect, and psychological vulnerability between Iranian infertile and fertile men. Iran J Psychiatry Behav Sci. 2013;7(1):9–15. Spring.
15. Ying L, Xing L. Research progress on psychological stress and coping measures of azoospermia patients. Rehabilitation Nurs. 2019;19(03):29–32. Chinese.
16. Wan W, Zhang Z, Yang H, et al. Investigation on mental health status of azoospermia patients and analysis of related factors. Nurs Res. 2016;30(15):1866–1869. Chinese.
17. Liang L, Wu M. Emotional expression and emotional expression conflict in marital relationship. Applied Psychology. 2009;15(04):334–338. Chinese.
18. Zare Z, Golmakani N, Amirian M. Comparison of sexual problems in fertile and infertile couples. J Caring Sci. 2017;3(3):269–279. doi:10.15171/jcs.2017.026
19. Yang B, Xu P, Shi Y, et al. Erectile dysfunction and associated risk factors in Chinese males of infertile couples. J Sex Med. 2018;15(5):671–677. doi:10.1016/j.jsxm.2018.02.019
20. Bendayan M, Sais E, Alter L, et al. For patients with non-obstructive azoospermia, the outcome of testicular sperm extraction correlates with self-esteem, sexual health and the quality of the couple’s relationship. Basic Clin Androl. 2022;32(1):3. doi:10.1186/s12610-022-00153-z
21. Chachamovich JR, Chachamovich E, Ezer H, Fleck MP, Knauth D, Passos EP. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynaecol. 2010;31(2):101–110. doi:10.3109/0167482X.2010.481337
22. Wischmann T, Thorn P. (Male) infertility: what does it mean to men? New evidence from quantitative and qualitative studies. Reprod Biomed Online. 2013;27(3):236–243. doi:10.1016/j.rbmo.2013.06.002
23. Shi L, Zhang M, Luo L, et al. Relationship between stigma and marital adjustment in female patients with donor artificial insemination. Chinese J Androl. 2019;27(12):1081–1086. Chinese.
24. Ouyang F, Huo R, Chen Q, Li B, Lin Z, Zhou J. Quality of life status and influencing factors of patients with in vitro fertilization-embryo transfer. Nurs Res Pract. 2022;19(17):2531–2537. Chinese.
25. Luo L, Shi L, Zhao Y. Fertility stress and quality of life in couples receiving donor sperm insemination. J Fam Plann Reprod Health Care. 2019;38(03):201–205. Chinese.
26. Zhang Q. Effect of family participation nursing mode on psychological state of patients with assisted reproductive technology. Ele J Pract Clin Nurs. 2019;4(50):133.
27. Chang S, Zhou Y, Zhang H, et al. Effect of structural group psychotherapy on patients with psychogenic erectile dysfunction. J Nurs Educ. 2021;4(4):376–379.
28. Yanying ZJ. Effect of nursing based on Neumann health system model in patients with chronic prostatitis and depression. Chin Med J. 2019;30(05):192–196.
29. Naling L, Fushun W. The effect of TCM psychotherapy on the depression of college students. J Clin Med Res. 2019;6(33):196–198. Chinese.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
