Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Impact of the Working Hours Among Malaysian Nurses on Their Ill-Being, Intention to Leave, and the Perceived Quality of Care: A Cross-Sectional Study During the COVID-19 Pandemic
Authors Jarrar M , Binti Ali N, Shahruddin R, Al-Mugheed K , Aldhmadi BK, Al-Bsheish M , AlSyouf A, AlBaker W, Alumran A
Received 23 October 2022
Accepted for publication 29 December 2022
Published 13 January 2023 Volume 2023:16 Pages 119—131
DOI https://doi.org/10.2147/JMDH.S394583
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mu’taman Jarrar,1,2,* Noorhaliza Binti Ali,3,* Rashidah Shahruddin,3 Khalid Al-Mugheed,4 Badr K Aldhmadi,5 Mohammad Al-Bsheish,6,7 Adi AlSyouf,8 Waleed AlBaker,9 Arwa Alumran10
1Vice Deanship for Development and Community Partnership, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2Medical Education Department, King Fahd Hospital of the University, Al-Khobar, Saudi Arabia; 3Cluster of Applied Sciences, Open University Malaysia, Selangor, Malaysia; 4Nursing College, Riyadh Elm University, Riyadh 13244, Saudi Arabia; 5Department of Health Management, College of Public Health and Health Informatics, University of Ha’il, Ha’il, Saudi Arabia; 6Health Management Department, Batterjee Medical College, Jeddah, Saudi Arabia; 7Al-Nadeem Governmental Hospital, Ministry of Health, Amman, Jordan; 8Department of Managing Health Services and Hospitals, Faculty of Business Rabigh, College of Business (COB), King Abdulaziz University, Jeddah, Saudi Arabia; 9Department of Internal Medicine, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 10Health Information and Management Department, College of Public Health, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
*These authors contributed equally to this work
Correspondence: Mu’taman Jarrar, Al-Khobar, Saudi Arabia, Tel +966 54 471 8523, Email [email protected]; [email protected] Mohammad Al-Bsheish, Jeddah, 21442, Saudi Arabia, Tel +966 59 103 6065, Email [email protected]
Purpose: This study explores the effect of working duration on nurses and their ill-being (ie, anxiety, depression, fatigue, and sleepiness), intention to leave, and the quality of nursing care.
Methods: A questionnaire survey was employed for a convenience sample of 400 nurses at Malacca General Hospital in Malaysia who voluntarily participated in this cross-sectional study. The Statistical Package for the Social Sciences (SPSS) was used to treat and analyze the data. Descriptive statistics were generated, and Post Hoc analyses and ANOVA tests were conducted.
Results: Findings indicated that working hours duration was significantly associated with nurses’ anxiety (F (4, 394) = 10.362, p < 0.001), depression (F (4, 395) = 23.041, p< 0.001), fatigue (F (4, 395) = 24.232, p< 0.001), sleepiness (F (4, 395) = 4.324, p < 0.002), quality of nursing care (F (4, 395) = 16.21, p < 0.001) and intention leave their job, (F (4, 395) = 50.29, p < 0.001). The results also revealed that working more than 14 hours was negatively associated with their perceived quality of nursing care and positively associated with their perceived ill-being and intention to leave.
Conclusion: Shift length is an important issue, and nursing managers must consider shift length as it can adversely correlate with the nurses’ perceptions of work and life.
Keywords: nurses, working hours, ill-being, intention to leave, quality of nursing care, COVID-19
Introduction
In March 2020, the World Health Organization (WHO) announced a global pandemic due to the impact of the international transmission of COVID-19, resulting in numerous deaths and creating economic disruptions and massive social problems.1,2 Meanwhile, front-line healthcare workers have faced extreme physical and psychological stress. In these circumstances, nurses work in high-demand environments for extended periods and are continually in danger of contracting diseases while away from their families and enduring societal stigma.3,4 Accordingly, the pandemic led to considerable challenges experienced by the nursing profession, including higher patient loads, patient volumes, and new COVID-19 protocols.
Evidence examining COVID-19 impacts on the nursing profession is rapidly emerging. Healthcare professionals reported physical and psychological ill-being during COVID-19.5,6 “Ill-being” refers to physical and psychological health levels.7 The increased level of ill-being refers to high anxiety, depression, fatigue, and sleepiness levels. The literature shows that nurses are significantly exposed to substantial physical and psychological stressors during the COVID-19 pandemic.8–10 For instance, Sagherian et al found that a sample of 587 nurses reported sleeplessness and mild to severe chronic fatigue during the COVID‐19 pandemic in the United States.11 Another study reported poor or worse well-being from nurses caring for COVID-19 patients compared to co‐workers.12 The high levels of anxiety and depression nurses experienced during the pandemic have also been found to be associated with low general health and high insomnia.13 Furthermore, many studies have shown the adverse effects of the pandemic on healthcare workers, such as depression and anxiety and found higher rates among nurses than other health workers during the pandemic.2,14
Nevertheless, few studies have explored the associations between working hours length and health workers’ ill-being during the pandemic15,16 or related the shift length duration with the perceived ill-being among nurses. Accordingly, this study posits that increasing duty hours during the pandemic was associated with health care sense of ill-being.
Nurses are one group of healthcare workers working on the front line in the fight against COVID-19. Of all healthcare workers, they serve the most time with patients and are available at all times during their shifts. Nurses’ working hour duration plays a primary role in the positive response against infection and quality of care.17–19 Nurses were further pushed to the breaking point during the pandemic because they were required to work longer hours due to a nursing shortage. The National Health Commission of the People’s Republic of China has recommended four hours per shift for intensive care unit nurses who deal with COVID-19 patients.20 Gisèle et al noted that the percentage of overtime among nurses from 2019 to 2020 in Canada had dramatically increased, particularly between April and May 2020, compared to the same period in 2019.21 The weekly overtime hours of nurses also showed an upward trend from 6.6 to 9.7 hours from April 2019 - April 2020 and from 5.8 to 10.3 hours from May 2019 to May 2020, respectively.
Several studies have demonstrated that overtime negatively affects the health and well-being of caregivers’ quality of care.22,23 Before the pandemic, Ball et al survey of nurses reported that shifts of more than 12 hours were associated with poor quality of care ratings, higher rates of care left undone, and the longer the shift, the higher the dissatisfaction level.24 Jarrar et al examined the associations between nursing duty hour length on nurses’ reported quality and safety in Malaysian hospitals.25 Unexpectedly, the 12-hour day or night shift was unrelated to care outcomes. These mixed results mean that further research is required. The longer working hours might be associated with the decreased quality of care compared with nurses working fewer hours. Accordingly, this study supposes increasing duty hours during the pandemic was associated with decreased reported quality of care.
Intention to leave the job is another factor nurses faced during COVID‐19. Before COVID‐19, stressful work overload, burden, and working environment encouraged nurses to leave their job.26,27 During the pandemic, frequent changes in nurses’ schedules and the extension of the world emergency to combat COVID‐19 were associated with increased intent to leave and resign from their jobs.22 A recent study demonstrated that nurses who provided treatment for COVID‐19 patients had higher intent to leave their jobs.28
Healthcare providers reported higher intention to leave their job after the high risk of exposure to COVID‐19 and workloads.29 Unsafe working environments were one factor encouraging employees to leave their jobs.30 Thus, with the continuing pandemic and shortage of resources and workforce, nurses might consider leaving their jobs more seriously. However, little research has examined the association of the shift length type with the perceived leave intention among nurses during the pandemic. Accordingly, this study supposes increasing duty hours during the pandemic was associated with increased intention to leave.
Nurses in Malaysian healthcare organizations have played a vital role in tackling the COVID-19 pandemic and protecting public health,31,32 especially considering that Malaysia’s health system has been suffering from a nurse shortage for a long time.33 Although the Malaysian Ministry of Health (2020) took the necessary precautions, 1771 cases of COVID-19 were recorded among healthcare professionals; 80% were nurses.34 Based on the above-supporting literature and the importance of the duration of working hours among nurses, this study explores the effect of working duration on nurses and their ill-being (ie, anxiety, depression, fatigue, and sleepiness), intention to leave, and the quality of nursing care in the Malaysian context.
Method
Design, Participants and Sampling
This study was cross-sectional and used convenience sampling because of the accessibility and proximity of respondents to the researcher.35 Convenience sampling is also called “accidental sampling”. Sampling units are selected because they are available. The inclusion criteria in this study were all nurses working in Malacca General Hospital, a secondary and specialized hospital. The exclusion criteria were nurses who were temporarily not working because of emergency leave, unpaid leave, leave for vacation, sick leave, confinement leave, and nurses doing post-basic and advanced diplomas for six months or one year.
A total of 1525 nurses work in Malacca General Hospital. The Yamane formula (1967) was used to get the appropriate sample by calculating the sample sizes of the known population.36 A total of 317 participants were the adequate sample size.
Hence,
n = required responses
e² = error limit / Margin of error
N = Population size
So, the nurse’s staff in Malacca General Hospital (N) = 1525
Instrument
The study’s questionnaire had four sections. Introduction included socio-demographic data with the respondents’ background data such as age, gender, marital status, race, educational status, job position, years of experience in the current workplace, total years of working experience in nursing, and the presence of any other chronic health problems. The duration of working hours of nurses was classified as working hours in the last shift. The working hours (independent variable) had five categories: 7 hours shift, 8 hours shift, 10 hours shift, 12 hours shift, and more than 14 hours shift.
Method contained Part A, the Hospital Anxiety and Depression Scale, adapted from Zigmond and Snaith,37 Part B, the Chalder Fatigue Scale, adapted from Cella and Chalder,38 and Part C, the Karolinska sleepiness Scale, adapted and modified from Chaiard and Swikruti.39 These scales are in the English language. Part A consists of 7 items of measuring anxiety (ie, “I feel tense or ‘wound up’”, “I can sit at ease and feel relaxed”) and 7 items of depression (ie, “I feel as if I am slowed down”, “I have lost interest in my appearance”). A 4-point Likert-type scale was used, with answers ranging from 1 = Most of the time, 2 = A lot of the time, 3 = From time to time, occasionally, and 4 = Not at all. Negatively worded items were reverse-coded. The higher scores refer to a higher level of anxiety and depression. Part B consists of 11 items for measuring fatigue (ie, “Do you have problems with tiredness?”, “Do you have less strength in your muscles?”). A 4-point Likert-type scale was used, with answers ranging from 1 = Less than usual, 2 = No more than usual, 3 = More than Usual, and 4 = Much more than usual. The higher score refers to a higher level of fatigue. Part C consists of 10 items measuring sleepiness (ie, “Do you feel sleepy in the early hour of your work?”, “Do you feel sleepy at the end of your working hour?”). A 4-point Likert-type scale was used, with answers ranging from 1 = Extremely alert, 2 = Very sleepy, 3 = Great effort fighting awake, and 4 = Fighting sleep. The higher score refers to a higher level of sleepiness.
Findings consisted of five items indicating the quality of nursing care in a respondent’s current ward adapted from the Agency for Healthcare Research and Quality (ie, “The quality of nursing care in my current work is good”, “If I needed hospital care I would come to this hospital”). A 4-point Likert-type scale with answers ranging from 1 = Strongly Disagree, 2 = Disagree, 3 = Agree to 4 = Strongly Agree. The higher score refers to a higher level of quality of care. Lastly, Discussion consisted of intention to quit items that evaluated the nurses’ intention to leave their job, adapted from Viklund,40 which consists of questions related to nurses’ intention and thinking to leave. This section consists of 13 items measuring nurses’ intention to quit their work (ie, “Do you have intentions to quit your job?”, “Have you applied for a new job during the last year?”). A 4-point Likert-type scale with answers ranging from 1 = Not at all, 2 = To a rather small extent, 3 = In quite a high degree, and 4 = In a very high degree. The higher score refers to a higher level of intention to quit.
A bilingual expert conducted back-to-back translations to translate the questionnaire from English to Malay. The questionnaire booklet included both English and Malay languages. To obtain the validity of the instrument items adopted, the researchers requested face validation from two experts. According to Oladimeji, A. B, 2021, face validity involves an expert looking at the items in the questionnaire and agreeing that the test is a valid measure of the concept which is being measured just on the face of it.41 The experts evaluated and approved that each of the measuring items matched the given conceptual domain of the concept.
Ethical Considerations and Data Collection
This study was conducted in accordance with the Declaration of Helsinki. The ethical committee of Open University Malaysia (OUM) University Approved this research (Approval Number: OUM-CAS/2.7/210/MN(001)). Permission to conduct the survey was obtained from the Head (Matron) of the Nursing Division Unit and the Director of Malacca General Hospital. Written consent was obtained from participants, and participants had the right to withdraw from the study at any time. A cover letter was attached to the questionnaire to inform participants of the study’s purpose and assure them that the data would be anonymous and that participation was voluntary. The socio-demographic data and answers from the participants were kept confidential to maintain the participants’ privacy and anonymity. To ensure privacy and anonymity, the name and personal information aside from their age, gender, race, marital status, job position, educational level, working experience, and health or mental problem were kept confidential.
Data were obtained between October and December 2020 via self-administered questionnaires. All respondents gave written approval to participate in this study, and the respondents were approached while free or at the end of their duty and voluntarily agreed to complete the survey. All respondents were given the participation information sheet, an informed consent form, and a questionnaire in a close envelope. Data were collected from nurses working in the critical care units in the Malacca General Hospital. Because some nurses might not agree to participate, the targeted sample was all registered nurses currently working in Malacca General Hospital who voluntarily agreed to complete the survey. A total of 400 complete responses were returned in a closed envelope.
Data Analysis Technique
The data were entered in SPSS (version 21), and the descriptive analysis of respondents’ demography data was performed. Cronbach’s alpha and factor analysis assessed the reliability and validity of scales used in the study, respectively. Then, Post Hoc analyses and ANOVA tests were conducted to measure the association between working hours and the level of anxiety, depression, fatigue, sleepiness, quality of nursing care, and intention to leave among the nurses.
Findings
Demographic Characteristics
Concerning age, 35.3% were more than 35 years old, and 33% were between 31 to 35 years old. Of the respondents, 93.8% were female, and 6.2% were male. Most respondents were married, 87.3% (n=349). The educational background of respondents was mostly at the diploma level, which was 89.3%.
The largest percentage of the nurses has working experience of about 6 to 10 years (34%). The chronic health problem data showed that 6.2% (n=25) of the respondents had chronic health problems. A total of 51.2% (n=205) of respondents worked 7 hours in the last shift, followed by 26.5% (n=106) 8 hours. Next, 14.2% (n=57) of respondents worked 10 hours in the last shift, followed by 6.8% (n=27) who worked more than 14 hours.
Validity and Reliability
Two experts evaluated whether each measurement item matched the conceptual domain, and both approved the items. Due to this study’s several instruments and tools, Exploratory Factor Analysis (EFA) evaluated the instrument’s validity. The results of EFA by using the value of Kaiser-Meyer-Olkin (KMO) revealed values close to 1 on all study scales (Anxiety and Depression Scale KMO = 0.868 and Sig = 0.000, Chalder Fatigue Scale KMO = 0.917 and Sig = 0.000, Karolinska sleepiness Scale KMO = 0.861 and Sig = 0.000, Quality of Nursing Care Scale KMO = 0.837 and Sig = 0.000, Intent to leave Scale KMO = 0.936 and Sig = 0.000), and the significance level for Bartlett’s values was below 0.05, indicating a substantial correlation in the data (See Table 1).
 |
Table 1 Demographic Data of the Respondents (N=400) |
Cronbach’s alpha assessed the reliability of scales in the questionnaire, and an alpha above 0.7 is considered an acceptable value to assure reliability. A pilot study using 40 respondents was conducted, and the reliability result for 54 items of the questionnaire was 0.840. The pilot study results also revealed an acceptable reliability level of study measurement scales (Anxiety Survey Questionnaire (7 items, Cronbach’s alpha = 0.720), Depression Survey Questionnaire (7 items, Cronbach’s alpha = 0.824), Chalder Fatigue Scale Questionnaire (11 items, Cronbach’s alpha = 0.896), Karolinska sleepiness Scale Questionnaire (10 items, Cronbach’s alpha = 0.799), Quality of Nursing Care Questionnaire (6 items, Cronbach’s alpha = 0.836), Intention to leave Questionnaire (13 items, Cronbach’s alpha = 0.919).
Working Hours and Nurse’s Ill-Being, Quality of Nursing Care and Intention to Leave
The impact of working hours on nurses’ ill-being was examined using a one-way ANOVA between-group analysis of variance. The ANOVA output was statistically significant, indicating that the duration of working hours greatly impacted a nurse’s ill-being, anxiety (variation between sample means) F = 10.36, p <0.001, Depression F = 23.04, p<0.001, Chalder F = 24.23, p< 0.001 and Karolinska Scale F = 4.32, p<0.002. Thus, a relationship exists between the duration of working hours and the nurses’ ill-being (See Table 2).
 |
Table 2 Working Hours and Nurse Ill-Being, Quality of Nursing Care and Intention to Leave |
Furthermore, a one-way between-group analysis of variance (ANOVA) investigated the impact of working hours on nursing care quality. The ANOVA was statistically significant, indicating that the working hours duration greatly impacted the scores that determine the quality of nursing care, F = 16.21, p <0.001. A one-way between-group analysis of variance (ANOVA) investigated the impact of working hours among nurses against their intention to leave. The ANOVA was statistically significant, indicating that the duration of working hours affects the intention among the nurses to leave their job, F = 50.29, p <0.001.
Post Hoc Analyses of Nurses’ Ill-Being
Post Hoc analyses with Tukey’s HSD, as shown in Table 3 (using α of 0.05), revealed that nurses who worked more than 14 hours in a shift (M = 14.26, SD = 4.65) had a significantly (p < 0.001) higher anxiety score than those who worked in 7, 8 and 10 hours shifts (See Figure 1).
 |
Table 3 Summary of the Post Hoc Analyses with Tukey’s HSD Results |
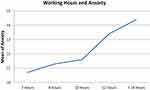 |
Figure 1 Working hours and anxiety. |
Post Hoc analysis with Tukey’s HSD (using α of 0.05) revealed that nurses who worked more than 14 hours (M = 18.63, SD = 3.94) had significantly (p < 0.001) higher depression scores than those that worked in lesser hours (See Figure 2).
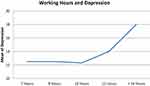 |
Figure 2 Working hours and depression. |
Post Hoc analysis with Tukey’s HSD (using α of 0.05) revealed that nurses who worked more than 14 hours (M = 30.85, SD = 4.13) had significantly (p < 0.001) higher Chalder fatigue scale scores than those that worked fewer hours (See Figure 3).
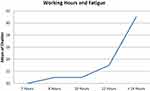 |
Figure 3 Working hours and fatigue. |
Post Hoc analysis with Tukey’s HSD (using α of 0.05) also revealed that nurses who worked more than 14 hours (M = 27.56, SD = 5.37) had significantly (p < 0.05) higher Karolinska sleepiness scale scores than those working 7 and 8 hours (See Figure 4).
 |
Figure 4 Working hours and sleepiness. |
Post Hoc Analyses of the Quality of Nursing Care
Post Hoc analysis with Tukey’s HSD (using an α of 0.05) revealed that nurses who worked more than 14 hours (M = 13.15, SD = 3.48) had significantly (p< 0.001) reduced scores on the quality of nursing care when compared with nurses that had 7, 8 and 10 hours of work shifts. Thus, this demonstrates a correlation between the duration of working hours and the quality of nursing care in the hospital (See Figure 5).
 |
Figure 5 Working hours and the quality of nursing care. |
Post Hoc Analysis of Nurses’ Intent to Leave
Post Hoc analyses with Tukey’s HSD (using α of 0.05) revealed that nurses who worked more than 14 hours (M = 41.89, SD = 11.98) had significantly (p < 0.001) higher intention to leave scores than those who worked fewer hours, showing a correlation between the duration of working hours and the nurses’ intent to leave (See Figure 6).
 |
Figure 6 Working hours and the intention to leave. |
Discussion
To our knowledge, this study is the first of its kind to explore the effect of working duration on nurses and their ill-being (ie, anxiety, depression, fatigue, and sleepiness), intention to leave, and the quality of nursing care in the Malaysian context. The study provides insights into the length of nurses’ duty hours during the pandemic. The association between a nurse’s shift length and perceived outcomes was explored. This study shows undesirable outcomes related to increasing the nurses’ duty hours.
The study reported a positive correlation between working hours and the nurses’ perception of ill-being (anxiety, depression, fatigue, and sleepiness). Nurses who worked fourteen hours reported higher anxiety, depression, fatigue and sleepiness than those working eight hours or less. This finding is consistent with an earlier qualitative study conducted among Chinese nurses who reported feeling fatigued.42 In another study, the prevalence of fatigue was 62.0%, and depression was 52.1% among nurses.23 Sagherian et al found that nurses who cared for COVID-19 patients for more than 40 hours per week had a significant risk for fatigue and psychosocial well-being.11 A qualitative study found that ICU nurses felt physical exhaustion caused by wearing PPE, which minimized their working capacity and ability to focus.43 The increase in anxiety, depression, fatigue, and sleepiness indicates a reduction in the effectiveness of the nursing workforce, which is a major impediment to overcoming the pandemic.44 However, if nurses were continuously supported, the delivery of nursing care to COVID-19 itself would not be a factor in increasing nurses’ ill-being. In addition, initial organizational precautions are necessary to provide mental health support to nursing staff to reduce their anxiety, depression, and fatigue from COVID-19 via counselling and continuous training.
At the start of 2021, the International Council of Nurses (ICN) expressed significant concerns experienced by nurses as a result of the COVID-19 pandemic. According to an ICN report, 90% of national nursing associations are concerned that burnout and stress workloads may contribute to rising numbers of nurses leaving the job.45 Aligned with this, our study revealed that nursing staff reported a high intention to leave their profession. Similarly, 22.3% of Canadian nurses reported a high desire to leave their current setting and the profession.13 This desire may be attributable to poor work environments, nurses assigned new roles and additional tasks and increased emotional demands. Also, the excessive strain is likely to reduce motivation and encourage nurses to leave the nursing profession and even their current workplace.46 A stressful and dissatisfying work environment strongly influences nurses’ desire to leave.47 Immediate interventions are required to improve the healthcare system’s strength and resiliency to deal effectively with the pandemic.
This study also found a negative association between the duration of nurse working hours and the quality of nursing care provided. This finding is aligned with Prichard,48 who mentioned that long duty hours affect the provision of quality nursing care. A study conducted in Sweden during the first wave of the COVID-19 pandemic showed that longer working hours were related to absence from work amongst nurses, and the quality of care was perceived as worse.49 These studies found that patient ratio adversely influenced nurses’ quality of care and patient safety.18,25
Possible explanations for the results of the current study are the new requirements when providing care, increasing bed capacity, changing protocols rapidly, caring for more critically-ill patients, and navigating unfamiliar settings.45 There is an urgent need to protect nurses’ occupational health and safety and support them in paying more attention during treatment to prevent or reduce the consequences of the current or future pandemics or uncertainties.
Implications of the Study
The data proved that the duration of working hours affects the nurses’ ill-being, intention to leave and the quality of nursing care. This condition adversely affects healthcare delivery, medical treatment and intervention, and health system management. Conclusively, nurses who work longer shifts experience more anxiety, depression, and fatigue. In addition, a longer shift also influences their tiredness, fatigue, sleepiness, and intention to leave work, especially during the COVID-19 pandemic. When nurses’ well-being is neglected, a work-life imbalance occurs. Thus, problems will arise if no initiative and remedial measures are taken to increase the number of staff nurses, especially during crises. The impact of duty working hours on nurses’ ill-being should not be ignored because if nurses are ill or have mental and physical problems, their ability to work will be adversely affected.
Long working hours were associated with the nurses’ ill-being, as indicated by high levels of anxiety, depression, fatigue, and sleepiness, which can affect the nurses as individuals.50 Prolonged working hours can cause fatigue, stress and depression. Billings (2020) highlighted that workers whom COVID-19 has directly affected might need to be given additional flexibility and support when it comes to shift scheduling.51
Additionally, the Ministry of Health must allocate more funds to build new healthcare facilities and hospitals to cater to the crowded patient space in current government hospitals. The Malaysian government to take action to secure more nurses in hospitals. This research provides evidence that prolonging shift hours for nurses is not sustainable because it will adversely affect nurses’ well-being, and their mental and physical health will deteriorate. This situation also might threaten the health system and patients’ safety.
Limitations of the Study
This study had several limitations. First, the study design was cross-sectional and could not establish causality between the study variables. Second, a non-random convenience sample technique was used, and future studies could use random sampling. Additionally, this study was limited to the Melaka General Hospital only; therefore, the results of this study cannot be generalized to all hospitals. Future investigations must explore longitudinal data from several hospitals in Malaysia and consider patients’ assessments and perceptions of the quality of care concerning the length of nurses’ duty hours. This study was conducted during the global health crisis (ie, COVID-19). Future studies should explore the impact of work duration when the health system returns to normal. These studies will assist in understanding this phenomenon more.
Conclusion
Because prolonging the duty hour to 14 hours per shift was associated with undesirable outcomes, preparedness for future crises needs to provide sufficient staffing support and adequate human resources to ensure an appropriate work and life balance among nurses, thus, providing the best services to the community. Cooperation between the Nursing Association and the Ministry of Health in Malaysia is vital to establish appropriate staffing policies and creating the best work environment in hospitals to improve nurses’ performances.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Al-Bsheish M, Jarrar MT, Scarbrough A. Public safety compliance model of safety behaviors in the age of the COVID-19 pandemic. J Health Care Org Pro Financ. 2021;58:1–6. doi:10.1177/00469580211031382
2. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2021;88:901–907. doi:10.1016/j.bbi.2020.11.023
3. Lorente L, Vera M, Peiro T. Nurses’ stressors and psychological distress during the COVID-19 pandemic: the mediating role of coping and resilience. J Adv Nurs. 2021;77(3):1335–1344. doi:10.1111/jan.14695
4. AL-Rawajfah O, Al-Mugeed K, Alaloul F, Al-Rajaibid HM, Al Omaria O. COVID-19 knowledge, attitude, and precautionary practices among health professional students in Oman. Nurse Educ Pract. 2021;52:103041. doi:10.1016/j.nepr.2021.103041
5. Duru H. The continuing effect of COVID-19 pandemic on physical well-being and mental health of ICU healthcare workers in Turkey: a single-centre cross-sectional later-phase study. J Intensive Care Med. 2021;37(9):1206–1214. doi:10.1177/088506662110704
6. Zhou Y, Wang W, Sun Y, et al. The prevalence and risk factors of psychological disturbances of front-line medical staff in China under the COVID-19 epidemic: workload should be concerned. J Affect Disord. 2020;277:510–514. doi:10.1016/j.jad.2020.08.059
7. Veenhoven R. Sociological theories of subjective well-being. In: Eid M, Larsen R, editors. The Science of Subjective Well-Being. Guilford Press; 2008:44–61.
8. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252–264. doi:10.1016/j.neubiorev.2021.03.024
9. Rodríguez-Rey R, Garrido-Hernansaiz H, Bueno-Guerra N. Working in the times of COVID-19. Psychological impact of the pandemic in frontline workers in Spain. Int J Environ Res Public Health. 2020;17(21):8149. doi:10.3390/ijerph17218149
10. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—A review. Asian J Psychiatr. 2020;51:102119. doi:10.1016/j.ajp.2020.102119
11. Sagherian K, Steege LM, Cobb SJ. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: a cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. 2020;10(21):1–8. doi:10.1111/jocn.15566
12. Alaradi A, Irum S, Ebrahim N, Mohamed FM, Hazeem FM, Ashfaq M. The mental health impact of COVID-19 pandemic on health care workers and coping strategies: a systematic literature review. Int J Online Biomed Eng. 2021;17(9):48–69. doi:10.3991/ijoe.v17i09.24791
13. Lavoie-Tremblay M, Gélinas C, Aubé T, et al. Influence of caring for COVID-19 patients on nurse’s turnover, work satisfaction and quality of care. J Nurs Manag. 2021;30(1):33–43. doi:10.1111/jonm.13462
14. Wang H, Liu Y, Hu K, et al. Healthcare workers’ stress when caring for COVID-19 patients: an altruistic perspective. Nurs Ethics. 2020;27(7):1490–1500. doi:10.1177/0969733020934146
15. Gong H, Zhang SX, Nawaser K, et al. The mental health of healthcare staff working during the COVID-19 crisis: their working hours as a boundary condition. J Multidiscip Healthc. 2021;14:1073–1081. doi:10.2147/JMDH.S297503
16. Lang Q, Liu X, He Y, Lv Q, Xu S. Association between working hours and anxiety/depression of medical staff during large-scale epidemic outbreak of COVID-19: a cross-sectional study. Psychiatry Investig. 2020;17(12):1167–1174. doi:10.30773/pi.2020.0229
17. Jarrar MT, Al‐Bsheish M, Dardas LA, Meri A, Sobri MM. Adverse events in Malaysia: associations with nurse’s ethnicity and experience, hospital size, accreditation, and teaching status. Int J Health Plan Manag. 2020;35(1):104–119. doi:10.1002/hpm.2822
18. Jarrar M, Minai MS, Al-Bsheish M, Meri A, Jaber M. Hospital nurse shift length, patient-centered care, and the perceived quality and patient safety. Int J Health Plan Manag. 2019;34(1):387–396. doi:10.1002/hpm.2656
19. Al-Mugheed K, Bayraktar N. Patient safety attitudes among critical care nurses: a case study in North Cyprus. Int J Health Plan Manag. 2020;35(4):910–921. doi:10.1002/hpm.2976
20. National Health Commission of the People’s Republic of China. Notice on the inclusion of pneumonia in the management of statutory infectious diseases. National Health Commission of the People’s Republic of China; 2020. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml.
21. Gisèle C, Jungwee P, Zechuan D. Overtime work among professional nurses during the COVID-19 pandemic. J Stat Can. 2020;1(1):1–8.
22. Djupedal IL, Pallesen S, Harris A, Waage S, Bjorvatn B, Vedaa Ø. Changes in the work schedule of nurses related to the COVID-19 pandemic and Its relationship with sleep and turnover intention. Int J Environ Res Public Health. 2022;19(14):8682. doi:10.3390/ijerph19148682
23. Lee H, Choi S. Factors affecting fatigue among nurses during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(18):11380. doi:10.3390/ijerph191811380
24. Ball J, Day T, Murrels T, et al. Cross-sectional examination of the association between shift length and hospital nurses job satisfaction and nurse reported quality measures. BMC Nurs. 2017;16:26. doi:10.1186/s12912-017-0221-7
25. Jarrar M, Rahman HA, Sebiany AM, AbuMadni MS, Hj S, Amalraj C. Nursing duty hours’ length and the perceived outcomes of care. Glob J Health Sci. 2018;10(4):1–6. doi:10.5539/gjhs.v10n4p1
26. Phillips C. Relationships between workload perception, burnout, and intent to leave among medical-surgical nurses. JBI Evidence Implem. 2020;18(2):265–273. doi:10.1097/XEB.0000000000000220
27. Shin S, Oh SJ, Kim J, Lee I, Bae SH. Impact of nurse staffing on intent to leave, job satisfaction, and occupational injuries in Korean hospitals: a cross‐sectional study. Nurs Health Sci. 2020;22(3):658–666. doi:10.1111/nhs.12709
28. Raso R, Fitzpatrick JJ, Masick K. Nurses’ intent to leave their position and the profession during the COVID‐19 pandemic. J Nurs Adm. 2021;51(10):
29. Al-Naeem MM, Hamdan‐Mansour M, Nashwan AJ, Abuatallah A, Al‐Hussam M. Healthcare providers’ intention to leave their jobs during COVID‐19 pandemic: a cross‐sectional study. Health Sci Rep. 2022;5:e859. doi:10.1002/hsr2.859
30. Swamy L, Mohr D, Blok A. Impact of workplace climate on burnout among critical care nurses in the veterans’ health administration. Am J Crit Care. 2020;29(5):
31. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi:10.1001/jama.2020.3972
32. Purba AK. How should the role of the nurse change in response to Covid-19? Nurs Times. 2020;116(6):25–28.
33. Jarrar M, Rahman HA, Shamsudin AS. The impact of patient to nurse ratio on quality of care and patient safety in the medical and surgical wards in Malaysian private hospitals: a cross-sectional study. Asian Soc Sci. 2015;11(9):326–332. doi:10.5539/ass.v11n9p326
34. Ministry of Health Malaysia. 1771 healthcare workers in Malaysia infected with COVID-19. CNA. Available from: https://www.channelnewsasia.com/asia/covid-19-malaysia-healthcare-workers-nurses-infected-487791.
35. Basavanthappa B. Nursing Research and Statistics. New Delhi: Jaypee Brothers Medical Publishers; 2014.
36. Chua YP. Kaedah penyelidikan (Edisi Kedua) Research methods.
37. Zigmond AZ, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
38. Cella M, Chalder T. Measuring fatigue in clinical and community settings. J Psychosom Res. 2010;69(1):17–22. doi:10.1016/j.jpsychores.2009.10.007
39. Swikruti CJ. The psychometric properties of the Karolinska sleep questionnaire. J Sleep Res. 2019;6:707–716. doi:10.1111/jsr.12059
40. Viklund M Nurses’ intention to quit: NITQ. Development of a measuring instrument [Master’s thesis, Mälardalens University]; 2017. Available from: https://www.diva-portal.org/smash/get/diva2:1113343/FULLTEXT02.pdf.
41. Oladimeji AB. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22(4):195. doi:10.4103/1117-1936.173959
42. Sun N, Wei L, Shi S, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48(6):592–598. doi:10.1016/j.ajic.2020.03.018
43. Moradi Y, Baghaei R, Hosseingholipour K, Mollazadeh F. Challenges experienced by ICU nurses throughout the provision of care for COVID-19 patients: a qualitative study. J Nurs Manag. 2021;29(5):1159–1168. doi:10.1111/jonm.13254
44. Kim YJ, Lee SY, Cho JH. A study on the job retention intention of nurses based on social support in the COVID-19 situation. Sustainability. 2020;12(18):7276. doi:10.3390/su12187276
45. International Council of Nurses (ICN). Policy brief: the global nursing shortage and nurse retention; 2021. Available from: https://www.icn.ch/sites/default/files/inlinefiles/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20Retention.pdf.
46. Hognestad HG, Olsen E, Mikkelsen A. The association between supervisor support and ethical dilemmas on nurses’ intention to leave: the mediating role of the meaning of work. J Nurs Manag. 2020;29(2):286–293. doi:10.1111/jonm.13153
47. Labrague LJ, Santos JA, Falguera CC, et al. Predictors of nurses’ turnover intention at one and five years’ time. Int Nurs Rev. 2020;67(2):191–198. doi:10.1111/inr.12581
48. Prichard K 7 Signs of fatigue and how it affects the workplace. OMAG. Available from: https://www.omag.org/news/2021/5/1/7-signs-of-fatigue-and-how-it-affects-The-workplace.
49. Nymark C, Vogelsang AC, Falk AC, Göransson KE. Patient safety, quality of care and missed nursing care at a cardiology department during the COVID-19 outbreak. Nurs Open. 2021;9(1):385–393. doi:10.1002/nop2.1076
50. Kutney-Lee A, Wu ES, Sloane DM, Aiken LH. Changes in hospital nurse work environments and nurse job outcomes: an analysis of panel data. Int J Nurs Stud. 2013;50(2):195–201. doi:10.1016/j.ijnurstu.2012.07.014
51. Billings J, Greene T, Kember T, et al. Supporting hospital staff during COVID-19: early interventions. Occup Med. 2020;70(5):327–329. doi:10.1093/occmed/kqaa098
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.