Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
The Impact of SARS-CoV-2 Infection on the Length of Stay in the Neuro-ICU:A Prospective Multicenter Cohort Study in Eight Neuro-ICU, China Between February and April 2023
Authors Tan L, Wang F, Huang Y, Fu C, Zhang H, Feng J, Xu Y, Ye X, Tang R, Chen Y, Mou L, Li R, Chen J, Xian J
Received 2 November 2023
Accepted for publication 21 March 2024
Published 30 March 2024 Volume 2024:20 Pages 765—775
DOI https://doi.org/10.2147/NDT.S447887
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Liang Tan,1,* Feilong Wang,1,* Yi Huang,2 Chuhua Fu,3 Haijun Zhang,4 Jianfei Feng,5 Yincai Xu,6 Xinzhen Ye,7 Rongrui Tang,8 Yinglian Chen,9 Liansheng Mou,10 Ronghao Li,11 Jingyu Chen,1 Jishu Xian1
1Department of Neurosurgery, Southwest Hospital, Army Medical University, Chongqing, People’s Republic of China; 2Department of Neurosurgery, The Ninth People’s Hospital of Chongqing, Chongqing, People’s Republic of China; 3Department of Neurosurgery, Xiangyang No.1 People’s Hospital, University of Medicine, Xiangyang, Hubei, People’s Republic of China; 4Department of Neurosurgery, Kaifeng Central Hospital, Kaifeng, Henan, People’s Republic of China; 5Department of Encephalopathy, Beibei Traditional Chinese Medical Hospital, Chongqing, People’s Republic of China; 6Department of Neurosurgery, Zheng Coal General Hospital, Zhengzhou, Henan Province, People’s Republic of China; 7Department of Neurosurgery, Songshan General Hospital, Chongqing, People’s Republic of China; 8Department of Neurosurgery, University-Town Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 9Zhuhai Brainlightning Research Institute, Zhuhai City, Guangdong, People’s Republic of China; 10Department of Neurosurgery, Liangping District People’s Hospital, Chongqing, People’s Republic of China; 11Department of Basic Medicine, Army Medical University, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jingyu Chen; Jishu Xian, Email [email protected]; [email protected]
Purpose: The SARS-CoV-2 infection cases are increasing rapidly in neuro-intensive care units (neuro-ICUs) at the beginning of 2023 in China. We aimed to characterize the prevalence, risk factors, and prognosis of critically ill patients treated in neuro-ICUs.
Materials and Methods: In the prospective, multicenter, observational registry study, critically ill patients with intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), and traumatic brain injury (TBI) admitted to eight Chinese neuro-ICUs between Feb 16, 2023, to Apr 30, 2023 were enrolled for the study. Mortality and ICU stay day were used as the primary outcomes.
Results: 131 patients were finally included and analyzed (mean age 60.36 years [SD 13.81], 64.12% male, 39.69% SARS-CoV-2 infected). The mortality is higher in the SARS-CoV-2 infection group without statistical signification (7.69% vs 5.06%, p> 0.05). The length of stay (LOS) in neuro-ICUs was significantly longer among the SARS-CoV-2 infection patients (7(1– 12) vs 4(1– 8), p< 0.01), with increased viral pneumonia occurrence (58.54% vs 7.32%, p< 0.01). SARS-CoV-2 infection, surgery, and low GCS scores were independent risk factors for prolonged LOS, and respiratory/renal failure were independent risk factors for death.
Conclusion: Based on the present neuro-ICU cohort, SARS-CoV-2 infection was a significant risk for the prolonged LOS of neuro-critically ill patients.
Trial Registration: Registered with Chictr.org.cn (ChiCTR2300068355) at 16 February 2023, Prospective registration. https://www.chictr.org.cn/showproj.html?proj=188252.
Keywords: SARS-CoV-2, intensive care unit, intracerebral hemorrhage, subarachnoid hemorrhage, traumatic brain injury
Introduction
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to a worldwide pandemic, resulting in a substantial number of patients needing critical care. SARS-CoV-2 primarily affects the respiratory system, resulting in cough, fever, and dyspnea.1 Recent studies have indicated that SARS-CoV-2 has the potential to impact various organ systems, including the central nervous system (CNS).2 Patients with pre-existing critical neurological conditions, such as intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), and traumatic brain injury (TBI), who subsequently acquire SARS-CoV-2 infection, may experience unfavorable outcomes when admitted to neuro-intensive care units (neuro-ICUs).
SARS-CoV-2 has the ability to invade endothelial cells and induce widespread endothelial inflammation in individuals diagnosed with COVID-19.3 Viral replication occurs in multiple respiratory and non-respiratory tissues during early infection, leading to systemic infection and persistence in the body for months.4 Patients admitted to neuro-ICUs are susceptible to SARS-CoV-2 infection and at risk of severe complications. Ischemic stroke can also manifest as a symptom of COVID-19 infection, presenting a substantial risk of 7.5 times greater than influenza virus infection.5 Nevertheless, the ability to conduct retrospective studies on the neurological manifestations of COVID-19 in both NICU and non-NICU settings is impeded by various methodological inconsistencies, discrepancies in the definition of neurological disorders, limitations in sample size, and potential reporting bias.
We present a prospective, multicenter, observational cohort study that aimed to examine the influence of SARS-CoV-2 on the prognosis of patients with ICH, SAH, or TBI in Chongqing, Hubei, and Henan provinces, China. Our main aim was to analyze and describe the condition of severely ill individuals admitted to neuro-ICUs and systematically evaluate the frequency of neurological symptoms resulting from SARS-CoV-2 infection during the COVID-19 outbreak in early 2023 in China. It is anticipated that the findings from our study will offer significant insights into the effects of SARS-CoV-2 infection on neuro-ICUs as well as aid in identifying prognostic indicators for unfavorable outcomes in COVID-19 patients receiving neurocritical care. Our research outcomes have the potential to provide valuable insights for clinical practitioners and to improve patient outcomes in this susceptible population.
Material and Methods
Study Design
We conducted a multicenter prospective cohort study from February 16, 2023, to April 30, 2023, at neuro-ICUs in eight centers in Chongqing, Hubei, and Henan provinces, China. The study design adhered to the STROBE statements for observational studies. The study was approved by the Ethics Committee of Southwest Hospital, which is affiliated with the Army Medical University (Approval No: (B) KY2023006) and registered with Chictr.org.cn (ChiCTR2300068355). The registration process was completed before the trial and enrollment of the first patient was initiated. COVID-19 was diagnosed using routine nucleic acid testing on admission. SARS-CoV-2 infection was confirmed through PCR nucleic acid testing in accordance with the Chinese COVID-19 Diagnosis and Treatment Protocol (Trial Version 10).6
Prior to hospitalization, each patient underwent a standardized medical history assessment encompassing the documentation of symptom onset. To mitigate the potential for nosocomial transmission of SARS-CoV-2, it is imperative to implement patient isolation measures and administer treatment while adhering to stringent personal protective equipment (PPE) protocols.
Study Participants
Inclusion criteria: ①Diagnosed of ICH, SAH, or TBI as the primary admission diagnosis in medical records; ②Age: 18–80;③ admitted to neuro-ICUs; ④ willing to participate in the study after informed consent; ⑤Admission GCS score >5. Exclusion criteria: ①Patients with novel coronavirus pneumonia as the primary disease; ② Patients with other serious central nervous system diseases; ③ Developed a late cerebral hernia at admission, with signs of bilaterally dilated pupils, central respiratory failure, and hemodynamic instability; ④ Patients who had been diagnosed with psychological diseases before, such as depression and anxiety; ⑤ Patients who had previously suffered from COVID-19; ⑥ Patients who refused to accept nucleic acid or antigen testing; ⑦ Patients without informed consent. Patients with delayed discharge were excluded, considering the administrative delay (principally bed block), to eliminate non-logistic factors. Ultimately, 160 patients who satisfied the inclusion criteria for this study were initially enrolled. The involvement of patients or the public was not incorporated into our research design, implementation, reporting, or dissemination strategies.
Study Design
Mortality and length of stay (LOS) in the neuro-ICUs were identified as the primary outcomes for evaluating the impact of SARS-CoV-2 infection. Viral pneumonia and respiratory failure were identified as secondary outcomes. The Glasgow Coma Scale (GCS) score improved from admission to discharge, and the modified Rankin Scale (mRS) score was also assessed upon discharge. Viral pneumonia was predominantly diagnosed through the utilization of chest CT scans and was referred to as a direct consequence of SARS-CoV-2 infection. Ground glass lesions or nodules were identified, irrespective of the outcome of SARS-CoV-2 PCR testing, to detect potential abnormalities.
Based on the data characteristics outlined in the referenced clinical studies and the risk factors specific to neuro-ICUs,7 several variables that could potentially influence LOS in neuro-ICUs were identified. The variables considered in this study encompass a range of factors such as mortality, initial GCS score at admission, septicemia or shock, renal failure, respiratory failure, D-dimer levels, treatment received at various medical centers, presence of other cardiovascular diseases, diabetes mellitus, hypertension, tumor presence, smoking status, age, sex, SARS-CoV-2 infection, vaccination status, and history of previous surgery.
Statistical Analysis
The baseline characteristics of the neuro-intensive cases infected with SARS-CoV-2 were determined using R 4.1.2. Chi-square and Wilcoxon tests were used to assess the relationship between the status of SARS-CoV-2 infection and multiple factors. The LOS between the two groups was compared using the Mann–Whitney nonparametric or Kruskal–Wallis test in GraphPad Prism 9.0.0. The assessment of the normal distribution was conducted using the Shapiro–Wilk method. A logistic regression model for ICU LOS or the difference in GCS scores (D-GCS) was constructed using R 4.1.2. The model selection process was based on a lower AIC value and theoretical knowledge. In logistic regression analysis models, the outcome is determined by prognosis, specifically the improved GCS score, which is an indicator for evaluating the prognostic effect. A value less than or equal to zero indicates a high risk of poor prognosis.
In contrast, a value greater than zero indicates a low risk of poor prognosis. Spearman correlation analysis was used to evaluate the relationship between the present risk factors and the duration of ICU stay or the incidence of death using R 4.1.2. Finally, a P-value <0.05 or <0.01 was considered statistically significant or extremely significant, respectively, and denoted by the “*” or “**” symbol, was considered statistically significant or extremely significant, respectively.
Results
Clinical Characteristics
A cohort of 160 patients diagnosed with ICH, SAH, or TBI was admitted to the neuro-ICUs of eight medical centers between February 16 and April 30, 2023. Of the patients included in the study, 29 were excluded (Figure 1). Among 131 eligible cases, SARS-CoV-2 infection occurred in 39.69% (n=52). As shown in Table 1, the initial GCS scores upon admission did not display any significant differences between the two groups, suggesting a comparable severity of the condition (Z=1.110, P=0.267).
 |
Table 1 Baseline Characteristics of Included Neuro-Intensive Cases Infected or Non-Infected with SARS-CoV-2 (N=131) |
 |
Figure 1 Study Flow Chart. |
The average age of the participants was 60.36 years, with a standard deviation of 13.81, and 84 (64.12%) were male. Of the participants, 52 tested positive for SARS-CoV-2 nucleic acid, accounting for 39.69%. The admitted diagnoses were categorized as follows: SAH, 39 (29.77%) participants; ICH, 76 (58.02%) participants; TBI, 16 (12.21%) participants. The median LOS in the intensive care unit was five days, with an interquartile range of two–ten days.
Among the participants, 41 (31.30%) were smokers, 88 (67.18%) had hypertension, 20 (15.27%) had diabetes, 31 (23.66%) had cardio-cerebrovascular disease, and two (1.53%) had tumors. A total of 74 (56.49%) underwent the surgical procedures. Among these individuals, 82 (62.60%) received antibiotic or antiviral treatments.
Eight (6.11%) participants died during the course of the study and 19 (14.50%) experienced respiratory failure. Five (3.82%) participants developed renal failure, and one (0.76%) experienced sepsis or shock. The mean Glasgow Coma Scale (GCS) score upon admission was 9.89, with a standard deviation of 3.85. The mean GCS score at discharge was 10.57, with a standard deviation of 4.54 (Table 2).
 |
Table 2 Baseline Characteristics of Included Neuro-Intensive Cases (N=131) |
SARS-CoV-2 Infection Acted as a Risk Factor for Viral Pneumonia and Prolonged ICU Length of Stay
Among the patients who tested positive for SARS-CoV-2, 24 (58.54%) had viral pneumonia. In contrast, only three subjects (7.32%) in the negative group showed signs of viral pneumonia. The difference in ICU stay days between the two groups was determined to be statistically significant using the Wilcox test (7(1–12) vs 4(1–8), p<0.001) (Table 1), the sub-group analysis of age ≥60 or <60 showed SARS-CoV-2 infection led to longer length of ICU stay among the patients in both age sub-groups (Figure S1A and S1B). The analysis also indicated that the mortality rate was higher in the positive group, although the difference was not statistically significant (7.69% vs 5.06%, p > 0.05, Table 1). Additionally, D-dimer levels after surgery were higher in patients with SARS-CoV-2 infection in neuro-ICUs, although the difference was not statistically significant vs 4.16(2.58–8.35), p=0.07, Table 1). Other demographic factors, including age, sex, and presence of respiratory failure, did not exhibit any significant differences between the two groups, suggesting their comparability. Therefore, COVID-19 infection poses a significant risk for the development of viral pneumonia in neuro-ICUs, resulting in an extended stay in neuro-ICUs.
Independent Risk Factors for Prolonged ICU Length of Stay: SARS-CoV-2 Infection, Surgery, and Low GCS Scores
Figure 2A provides additional evidence of an extended stay in neuro-ICUs in relation to SARS-COV-2 infection. A forest plot of risk factors showed that SARS-COV-2 infection significantly prolonged the ICU stay of patients with neurological conditions. Undergoing surgery was also associated with prolonged stay in neuro-ICUs. Conversely, patients with higher GCS scores upon admission had a relatively shorter duration of ICU stay, with an influence coefficient of −0.4787 (Figure 2B).
There was no statistically significant difference in ICU length of stay among patients with different neurological conditions, ICH, SAH, or TBI (Figure S2). Similarly, the ICU length of stay did not significantly differ between patients who received COVID-19 vaccination and those who did not (Figure S3).
Correlation Analysis Reinforces Prolonged ICU Length of Stay Was Associated with SARS-CoV-2 Infection
Spearman correlation analysis demonstrated a statistically significant association between the extended duration of stay in the ICU and various factors, including undergoing surgical procedures, testing positive for COVID-19, and presenting with low GCS scores upon admission (P<0.01) (Table 3). The study revealed a significant correlation between mortality in neuro-ICUs, respiratory failure, and renal failure (P<0.01) (Table 4).
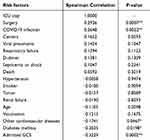 |
Table 3 Spearman Correlation Analysis and Significant Correlation Variables of the Length of ICU Stay. “*” Represented P<0.05 and “**” Represented P<0.01 |
 |
Table 4 Spearman Correlation Analysis and Significant Correlation Variables of the Mortality Rate. “**” Represented P<0.01 |
Discussion
This study focused on how SARS-CoV-2 infection influences the outcomes of patients with ICH, SAH, and TBI who were admitted to eight neuro-ICUs in different provinces of China after COVID-19 prevention and control measures were relaxed in China at the beginning of 2023. A prospective multicenter observational cohort study suggested that the SARS-CoV-2 infection rate was as high as 39.69% among critically ill patients admitted to neuro-ICUs at the initial easing of COVID-19 prevention and control measures. The severity of illness was similar between the two groups, as the admitted GCS scores showed no statistical differences. The mortality rate of COVID-19 cases was higher than that of non-infected patients in neuro-ICUs (7.69% vs 5.06%), without statistical differences. SARS-CoV-2 infection is a risk factor for viral pneumonia in the ICU, leading to prolonged LOS in the ICU.8 Additionally, the STRENGE analysis identified independent risk factors for prolonged LOS in the ICU, which included SARS-CoV-2 infection, surgery, and a lower GCS score upon admission.
COVID-19 has been found to worsen neurological symptoms in individuals with preexisting neurological disorders. In the available literature on COVID-19, the in-hospital neuro-ICU mortality rate exhibits significant variation, which can be attributed to differences in the analyzed cohort centers, periods, and clinical characteristics.9–11 A study conducted in 2021 found that in-hospital mortality among patients with SAH and COVID-19 was significantly higher than that among patients without COVID-19 (31.4% vs 12.2%), which was much higher than our results.12 However, the risk of SAH did not increase in COVID-19 patients. A prospective database of pediatric patients who suffered traumatic head injuries from 2018 to 2021 in Pittsburgh, USA, was post hoc analyzed to show that the prevalence of abusive head trauma did not increase during the Sars-Cov-2 lockdown (10.0%). The mortality rate related to abusive head trauma was 4.8 times higher during the lockdown period.13 Stroke patients with COVID-19 are particularly characterized by large vessel damage, and the main pathogenetic mechanism may be vasculitis induced by an immune response to damaged vascular endothelium, hypercoagulopathy, and cardioembolism. The direct injurious actions of SARS-CoV-2 on the brain vessels provoke wall rupture and hemorrhagic complications. Moreover, increases in blood pressure due to dysregulation of the renin-angiotensin system induced by viral invasion can contribute to the development of hemorrhages.
A Turkey study in 2020 revealed that 32.5% of patients diagnosed with ICH or SAH were also found to have COVID-19. The diagnosis was confirmed using nasopharyngeal SARS-CoV-2 PCR testing. The infection rate among these patients was as high as that observed in Chinese neuro-ICUs (39.69%) during the initial phase of easing epidemic prevention and control measures in 2023.14 Despite the relatively high vaccination rates, most countries have experienced a surge in COVID-19 cases after reducing lockdown measures, particularly in densely populated cities.15 Because of the flexible public healthcare provision in China, the lifting of the COVID-19 lockdown measures in early 2023 did not result in significant overcrowding of medical resources.16 This finding is consistent with our ICU mortality rate of 6.1% and an LOS of 5.2 days.
It has been reported that COVID-19 is an independent risk factor for ICU-acquired pneumonia among patients with common bacterial and viral pneumonia.8 Our study revealed that the prevalence of viral pneumonia among the participants was 20.61%. This finding aligns with a previous study that reported a 23% incidence of viral pneumonia among ICU patients.8 Moreover, the SARS-CoV-2 infected group has a higher percentage of viral pneumonia cases compared to the negative group (58.54% vs 7.32%). As reported, COVID-19 patients with viral pneumonia may have a higher risk of respiratory failure and ICU mortality rates than patients with bacterial pneumonia or other viral pneumonia.17 However, the respiratory failure and mortality rates did not differ significantly between the COVID-19 positive and negative groups in the present study. One possible reason is that preventive measures, such as high-flow oxygen therapy, timely mechanical ventilation, and prone position ventilation, can also alleviate respiratory symptoms.18–20 Consequently, respiratory failure and mortality can be significantly reduced. Another explanation is that the lowest oxygen saturation level was recorded and used to assess patients with COVID-19 in neuro-ICU settings.21 Decreased oxygen saturation is an independent risk factor for mortality in COVID-19 patients. Oxygen saturation below 90% upon admission is strongly associated with mortality in patients with COVID-19.22 In the present study, the minimum oxygen saturation level among all patients exceeded 93% (Table 2). Therefore, in resource-constrained settings, hospital administrators and healthcare professionals in China may prioritize routine pulse oximetry, concentrate on the early detection of hypoxemic respiratory failure, and promptly administer supplemental oxygen therapy to enhance hospital care during the COVID-19 pandemic.23
Accumulating research has shown that while SARS-CoV-2 primarily targets the respiratory system, it can also affect the vascular and central nervous systems throughout the body. This can occur directly through viral infection and indirectly through a cytokine storm, leading to endothelial dysfunction and multiorgan injury.24 Thus, COVID-19 has also been deemed an endothelial and microvascular disease that induces multisystem symptoms.25 The secretion of multiple endothelial activation/dysfunction markers is elevated in COVID-19 patients, such as D-dimer, which causes coagulation dysfunction and increases the risk of blood clotting or rebleeding, which is consistent with our results.26 It has been proposed that pericytes, which are extensively distributed in the intracranial vascular system and exhibit higher levels of ACE2 expression compared to endothelial cells, might be more vulnerable to SARS-CoV-2 infection.27 Angiotensin II was elevated in these patients and expressed higher levels of ACE2, which is essential for infectivity from SARS-COV-2. ACE2 receptors are also widely distributed in the cardiovascular system, then SARS-COV-2 can directly infect and destroy cardiovascular cells.28 Autopsy of COVID-19 patients showed that viral replication is present in multiple respiratory and non-respiratory tissues in the early infection stage, including the brain, suggesting that SARS-CoV-2 can cause continuous systemic infection, especially in the central nervous system.29 Blood-brain barrier dysfunction, microglial activation, and neuroinflammation have been observed in individuals with severe neuro-COVID. These patients exhibit significantly elevated levels of inflammatory markers in the cerebrospinal fluid.30,31 Therefore, COVID-19 can be indicated as a systemic epidermal cell disease that can cause systemic inflammatory response of the whole body, including cardiovascular/central nervous system dysfunction, which may explain the delayed hospitalization time of patients with severe neurological conditions.4,32,33
Additionally, patients treated with ACEIs or ARBs have increased sensitivity of ACE2 receptors to coronavirus S proteins. As a result, they may be at a higher risk of severe disease outcomes owing to SARS-CoV-2 infection.34 Given that hypertension is a prevalent underlying condition in neuro critically ill patients (67.18% in the current study cohort), it is plausible that the disturbance in the balance between ACE and ACE2, as well as the activation of the renin-angiotensin-aldosterone system (RAAS), could contribute to the unfavorable outcomes observed in patients with SARS-CoV-2 infection in neuro-ICUs.35 Therefore, SARS-CoV-2 infection has worsened the condition of critically ill patients through various direct and indirect pathways, resulting in an extended duration of ICU hospitalization.
This study had some limitations that can be further improved. First, the sample size was relatively small; therefore, the mortality rates in neuro-ICUs may not show statistical differences. Second, the absence of cerebrospinal fluid and brain imaging data hinders the ability to examine the precise impact of SARS-CoV-2 on the central nervous system. Currently, there is a dearth of research on the enduring effects of COVID-19 on critically ill individuals with neurological disorders. We will maintain ongoing communication with the patients post-discharge to ensure the completeness of the study.
Conclusions
In conclusion, this prospective, multicenter, observational registry study provides valuable insights into the outcomes of patients with ICH, SAH, or TBI admitted to neuro-ICUs during the early COVID-19 pandemic in China in 2023. Our findings suggest that SARS-CoV-2 infection is associated with prolonged stay in patients with neurological conditions in the neuro-ICU. The factors contributing to this prolongation included undergoing surgery and having a lower GCS score upon admission. Additionally, a significantly higher incidence of viral pneumonia has been observed in SARS-CoV-2-positive patients. Understanding these factors can assist healthcare providers in effectively managing patients with neurological conditions during an ongoing pandemic.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The Ethics Committee approved the protocol of this study at the First Affiliated Hospital of Army Medicine University (Approval No: (B) KY2023006). It complied with ethics principles from the Declaration of Helsinki and the International Conference on Harmonization Good Clinical. All eligible patients provided informed consent to be included in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Chongqing Middle and Young Medical High-end Talent Project, the Scientific Research Program of the Education Department of Hubei Province (Grant number D20222103), and the Chongqing Science-health joint medical research project (2022QNXM27). The funders were not involved in the study design, data collection/interpretation, and the decision to submit the publication results.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Synowiec A, Szczepański A, Barreto-Duran E, Lie LK, Pyrc K. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a systemic infection. Clin Microbiol Rev. 2021;34. doi:10.1128/CMR.00133-20
2. Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19). J Neurol. 2021;268(9):3059–3071. doi:10.1007/s00415-021-10406-y
3. Ma Z, Yang KY, Huang Y, Lui KO. Endothelial contribution to COVID-19: an update on mechanisms and therapeutic implications. J Mol Cell Cardiol. 2022;16469–16482. doi:10.1016/j.yjmcc.2021.11.010
4. Stein SR, Ramelli SC, Grazioli A, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. 2022;612(7941):758–763. doi:10.1038/s41586-022-05542-y
5. Merkler AE, Parikh NS, Mir S, et al. Risk of ischemic stroke in patients with covid-19 versus patients with influenza. medRxiv. 2020. doi:10.1101/2020.05.18.20105494
6. Nation health commission of people republic of China, Chinese Covid-19 diagnosis and treatment protocol; 2023. Available from: https://www.gov.cn/zhengce/zhengceku/2023-01/06/5735343/files/5844ce04246b431dbd322d8ba10afb48.pdf.
7. Crook H, Ramirez A, Hosseini A, et al. European working group on SARS-CoV-2: current understanding, unknowns, and recommendations on the neurological complications of COVID-19. Brain Connect. 2023;13(4):178–210. doi:10.1089/brain.2022.0058
8. Llitjos JF, Bredin S, Lascarrou JB, et al. Increased susceptibility to intensive care unit-acquired pneumonia in severe COVID-19 patients: a multicentre retrospective cohort study. Ann Intensive Care. 2021;11(1):20. doi:10.1186/s13613-021-00812-w
9. Raith EP, Luoma A, Earl M, et al. Repurposing a neurocritical care unit for the management of severely Ill Patients with COVID-19: a retrospective evaluation. J Neurosurg Anesthesiol. 2021;33(1):77–81. doi:10.1097/ANA.0000000000000727
10. Dimitriadis K, Meis J, Neugebauer H, et al. Neurologic manifestations of COVID-19 in critically ill patients: results of the prospective multicenter registry PANDEMIC. Crit Care. 2022;26(1):217. doi:10.1186/s13054-022-04080-3
11. Aboukaïs R, Devalckeneer A, Boussemart P, et al. Impact of COVID-19 pandemic on patients with intracranial aneurysm rupture. Clin Neurol Neurosurg. 2021:201106425. doi: 10.1016/j.clineuro.2020.106425.
12. Qureshi AI, Baskett WI, Huang W, et al. Subarachnoid hemorrhage and COVID-19: an analysis of 282,718 patients. World Neurosurg. 2021:151e615–615e620. doi:10.1016/j.wneu.2021.04.089.
13. Hect JL, Almast A, Simon D, Shoemaker S, McDowell MM. Prevalence, severity, and neurosurgical management of abusive head trauma during the COVID-19 pandemic. J Neurosurg Pediatr. 2023;1–7. doi:10.3171/2023.2.PEDS2317
14. Kafadar S, Yucetas SC, Gezgin I, Kaya H, Gulacti U, Bilek O. Influence of COVID-19 disease on subarachnoid hemorrhage and intracerebral hemorrhage. Bratisl Lek Listy. 2022;123(2):140–143. doi:10.4149/BLL_2022_024
15. Silva J, Lima AB, Alvim LB, et al. Epidemiological surveillance reveals the rise and establishment of the omicron SARS-CoV-2 variant in Brazil. Viruses. 2023;16(1):15. doi:10.3390/v15041017
16. Zhou Y, Zhang A, Liu X, et al. Protecting public’s wellbeing against COVID-19 infodemic: the role of trust in information sources and rapid dissemination and transparency of information over time. Front Public Health. 2023:111142230. doi:10.3389/fpubh.2023.1142230.
17. Haas L, Termorshuizen F, den Uil CA, de Keizer NF, de Lange DW. Increased mortality in. ICU patients ≥70 years old with COVID −19 compared to patients with other pneumonias. J Am Geriatr Soc. 2023;71(5):1440–1451. doi:10.1111/jgs.18220
18. Hu M, Zhou Q, Zheng R, et al. Application of high-flow nasal cannula in hypoxemic patients with COVID-19: a retrospective cohort study. BMC Pulm Med. 2020;20(1):324. doi:10.1186/s12890-020-01354-w
19. Kang H, Gu X, Tong Z. Effect of awake prone positioning in non-intubated COVID-19 patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. J Intensive Care Med. 2022;37(11):1493–1503. doi:10.1177/08850666221121593
20. Lee HJ, Kim J, Choi M, et al. Efficacy and safety of prone position in COVID-19 patients with respiratory failure: a systematic review and meta-analysis. Eur J Med Res. 2022;27(1):310. doi:10.1186/s40001-022-00953-z
21. Dillon K, Hook C, Coupland Z, Avery P, Taylor H, Lockyer A. Pre-hospital lowest recorded oxygen saturation independently predicts death in patients with COVID-19. Br Paramed J. 2020;5(3):59–65. doi:10.29045/14784726.2020.09.5.3.59
22. Mejía F, Medina C, Cornejo E, et al. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima. Peru PLOS ONE. 2020;15(12):e0244171. doi:10.1371/journal.pone.0244171
23. Ayinbuomwan SA, Mokogwu N, Akoria OA, Okwara BU, Omuemu CE, Obaseki DE. Arterial oxygen saturation and other clinical predictors of survival in patients with Covid-19: a review of cases in a tertiary care hospital in Nigeria. West Afr J Med. 2021;38:109–113.
24. Jin Y, Ji W, Yang H, Chen S, Zhang W, Duan G. Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches. Signal Transduct Target Ther. 2020;5(1):293. doi:10.1038/s41392-020-00454-7
25. Xu SW, Ilyas I, Weng JP. Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol Sin. 2023;44(4):695–709. doi:10.1038/s41401-022-00998-0
26. Chen AT, Wang CY, Zhu WL, Chen W. Coagulation disorders and thrombosis in COVID-19 patients and a possible mechanism involving endothelial cells: a review. Aging Dis. 2022;13(1):144–156. doi:10.14336/AD.2021.0704
27. Brann DH, Tsukahara T, Weinreb C, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci Adv. 2020:6. doi:10.1126/sciadv.abc5801.
28. Machado BH, Paton JFR. Relevance of carotid bodies in COVID-19: a hypothetical viewpoint. Auton Neurosci. 2021;233:102810. doi:10.1016/j.autneu.2021.102810
29. Porzionato A, Emmi A, Contran M, et al. Case report: the carotid body in COVID-19: histopathological and virological analyses of an autopsy case series. Front Immunol. 2021;26(12):736529. doi:10.3389/fimmu.2021.736529
30. Etter MM, Martins TA, Kulsvehagen L, et al. Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: a prospective cross-sectional study. Nat Commun. 2022;13(1):6777. doi:10.1038/s41467-022-34068-0
31. Reinhold D, Farztdinov V, Yan Y, et al. The brain reacting to COVID-19: analysis of the cerebrospinal fluid proteome, RNA and inflammation. J Neuroinflammation. 2023;20(1):30. doi:10.1186/s12974-023-02711-2
32. Thakur KT, Miller EH, Glendinning MD, et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain. 2021;144(9):2696–2708. doi:10.1093/brain/awab148
33. Emmi A, Rizzo S, Barzon L, et al. Detection of SARS-CoV-2 viral proteins and genomic sequences in human brainstem nuclei. NPJ Parkinsons Dis. 2023;9(1):25. doi:10.1038/s41531-023-00467-3
34. Beyerstedt S, Casaro EB, Rangel ÉB. COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis. 2021;40(5):905–919. doi:10.1007/s10096-020-04138-6
35. Camargo RL, Bombassaro B, Monfort-Pires M, et al. Plasma angiotensin ii is increased in critical coronavirus disease 2019. Front Cardiovasc Med. 2022:9847809. doi:10.3389/fcvm.2022.847809.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

