Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
The Impact of Patient Preference on Attendance and Completion Rates at Centre-Based and mHealth Pulmonary Rehabilitation: A Non-Inferiority Pragmatic Clinical Trial
Authors Candy S , Reeve J, Dobson R, Whittaker R, Garrett J, Warren J, Calder A, Tane T, Robertson T, Rashid U, Taylor D
Received 3 March 2023
Accepted for publication 3 July 2023
Published 12 July 2023 Volume 2023:18 Pages 1419—1429
DOI https://doi.org/10.2147/COPD.S408423
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Sarah Candy,1,2 Julie Reeve,2 Rosie Dobson,3,4 Robyn Whittaker,3,4 Jeffrey Garrett,1 Jim Warren,5 Amanda Calder,3 Taria Tane,3 Trina Robertson,4 Usman Rashid,2 Denise Taylor2
1Te Whatu Ora Counties Manukau Health, Auckland, New Zealand; 2Health & Rehabilitation Research Institute, Auckland University of Technology, Auckland, New Zealand; 3National Institute for Health Innovation, University of Auckland, Auckland, New Zealand; 4Te Whatu Ora Waitematā, Auckland, New Zealand; 5School of Computer Science, University of Auckland, Auckland, New Zealand
Correspondence: Sarah Candy, Department of Respiratory Medicine, Te Whatu Ora Counties Manukau, Private Bag 93311, Otahuhu, Auckland, 1640, New Zealand, Tel +64274363116, Email [email protected]
Purpose: Pulmonary rehabilitation (PR) is vital in the management of chronic respiratory disorders (CRDs) although uptake, attendance and completion are poor. Differing models of delivering PR are emerging in an attempt to increase the uptake and completion of this intervention. This study aimed to evaluate participant rate of attendance and completion of PR when given a preference regarding model of delivery (centre-based and mPR). Secondary aims were to evaluate the factors affecting patient preference for model of delivery and determine whether mPR is non-inferior to centre-based PR in health outcomes.
Methods: A multi-centre non-inferiority preference based clinical trial in Auckland, New Zealand. Participants with a CRD referred for PR were offered the choice of centre-based or mHealth PR (mPR). The primary outcome was completion rate of chosen intervention.
Results: A total of 105 participants were recruited to the study with 67 (64%) preferring centre-based and 38 (36%) mPR. The odds of completing the PR programme were higher in the centre-based group compared to mPR (odds ratio 1.90 95% CI [0.83– 4.35]). Participants opting for mPR were significantly younger (p = 0.002) and significantly more likely to be working (p = 0.0001). Results showed that mPR was not inferior to centre-based regarding changes in symptom scores (CAT) or time spent in sedentary behaviour (SBQ). When services were forced to transition to telehealth services during COVID-19 restrictions, the attendance and completion rates were higher with telephone calls and video conferencing compared to mPR – suggesting that synchronous interpersonal interactions with clinicians may facilitate the best attendance and completion rates.
Conclusion: When offered the choice of PR delivery method, the majority of participants preferred centre-based PR and this facilitated the best completion rates. mPR was the preferred choice for younger, working participants suggesting that mPR may offer a viable alternative to centre-based PR for some participants, especially younger, employed participants.
Keywords: chronic respiratory disorder, mHealth, preference, pulmonary rehabilitation, telehealth, telerehabilitation
Plain Language Summary
When offered the choice of centre-based or mPR, 2/3 of participants opted for centre-based PR. Those who preferred mPR were younger, working participants which may have the potential to increase the reach of PR for these groups. Data analysis showed the likelihood of completing PR was nearly twice as high if participants were enrolled in centre-based compared to mPR.
Introduction
Chronic respiratory disorders (CRDs) contribute 7% of the global burden of disease and are the third leading cause of death worldwide.1 People with CRD experience considerable symptom burden including shortness of breath, fatigue, and reduced health-related quality of life (HRQoL). Pulmonary rehabilitation (PR) is an evidence-based, key intervention in the management of people with CRD, and includes a structured programme of exercise and self-management education.2 It is usually delivered in group sessions twice weekly over eight-weeks.3 Systematic reviews of PR have demonstrated reductions in breathlessness, reduced hospital admissions for acute exacerbations and improved HRQoL.4,5 Clinical guidelines strongly recommend referral to PR for all patients with COPD with increasing evidence supporting PR for other CRDs.6,7 Despite this, up to 50% of people referred do not attend and 10–32% fail to complete PR.8 Known barriers to attendance and completion include travel distance, transport, illness, and lack of perceived benefit.8
Mobile health (mHealth), the delivery of healthcare interventions through mobile devices (phones, tablets and computers), is increasingly considered an option to support the management of chronic health conditions.9,10 A mHealth PR programme (mPR) was developed in 2019 for use in Aotearoa New Zealand (NZ) context by our team of public health and mHealth experts, physiotherapists, respiratory physicians, psychologists, respiratory nurse specialists, cultural experts, and ongoing input from end users.11,12 The feasibility of this programme has been demonstrated for people living with CRD in NZ.12
Patients have preferences for how they receive rehabilitation programmes;13,14 however, an important limitation in PR clinical trials to date is that they do not account for patient preferences for mode of delivery13–16. Several home-based trials of PR have reported low uptake due to participant’s preference for centre-based PR.13–16 The primary aim of this study was to evaluate attendance and completion rates when PR was delivered via two different delivery models (centre-based and mPR). Secondary aims were to evaluate patient preferences for model of delivery and to determine if mPR could achieve improvements in clinical outcomes that were not inferior to centre-based PR when patients chose mPR as their preferred mode of delivery.
Methods
Study Design
A parallel non-randomised preference-based non-inferiority clinical trial was conducted at three tertiary hospitals in Auckland, NZ from June to November 2021. The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12621000365864p) and received ethical approval from the Health and Disability Ethics Committee (21/NTB/54) and met the principles of the Declaration of Helsinki. The CONSORT checklist for pragmatic trials can be found in Supplemental File 1.
Participants
Patients who attended PR clinics at the participating hospitals were invited to take part in the study. Eligibility criteria were age ≥18 years, physician diagnosed CRD and able to read and understand English. Participants should not have completed PR within the last year. The mPR group required access to a standard mobile phone capable, at minimum, of sending and receiving SMS.
Procedures
At the initial PR appointment, the study was explained, and choices of delivery described. If participants gave written consent, they were offered the choice of intervention delivery model. Baseline assessment was then completed by a clinician blinded to patient preference. Post intervention assessments were completed by the attending PR team who were not blinded to group allocation.
Interventions
All participants in both groups attended a standard centre-based PR assessment based on best practice guidelines,3 which included a measure of exercise capacity (six-minute walk test), HRQoL (EQ5D), symptom score (CAT tool) and dyspnoea score (mMRC). All participants received an eight-week PR programme, consisting of exercise, education, and behaviour change interventions. The exercise programme was prescribed based on assessment findings and included aerobic, resistance and balance exercises. Participants were informed they were to exercise five times per week regardless of group allocation.
Centre-Based PR
This followed best practice guidelines which was standard care at all study sites.3 Participants received face-to-face group exercises twice a week supervised by a senior PR physiotherapist, and self-management education delivered by a member of the team. Participants were given a home-based exercise programme to complete on a further three days per week. Further intervention details are described in the TIDieR checklist - Supplemental Information 2.
Mobile Pulmonary Rehabilitation (mPR)
mPR was based on standard PR programmes and met best practice guidelines,3 including a patient-tailored intervention based on assessment findings. The multicomponent intervention was delivered to participants through text messages (SMS) with an optional web-based app and wearable sensor (Fitbit or Withings). Participants were also provided with a paper manual which included detailed instructions on how to safely complete each of the prescribed exercises. The exercise component of the programme was scheduled for five days per week for the 8-week intervention and was progressed with weekly increases in duration of aerobic exercises and numbers of repetitions of resistance exercises (see Supplemental File 2).
Impact of COVID-19 Restrictions
During the study, national lockdown restrictions were imposed due to the COVID-19 pandemic and centre-based services and face-to-face research and recruitment were required to cease. All participants allocated to the mPR arm of the study continued as per protocol and the following protocol change was implemented for those in the centre-based PR arm. All participants in the centre-based group during the onset of restrictions were offered alternative home-based options which comprised: either weekly telephone calls or twice weekly video-conference classes. All interventions were scheduled, clinician delivered and synchronous, to reproduce being as close to centre-based PR as possible. All participants in centre-based group attended a minimum of one in-person session prior to COVID-19 restrictions. These interventions continued until participants had completed their 8-week PR programme. See CONSORT checklist for COVID affected trials -Supplemental File 3.17
Outcomes
Consistent with similar studies,18 attendance was recorded as a percentage of the number of sessions offered and completion was defined as attendance ≥70%.
- For the centre-based PR group this was initially two sessions per week. However, modifications due to COVID-19 meant some participants received scheduled weekly telephone calls or twice weekly videoconferencing from their PR clinician.
- For the mPR group, a proxy measure of attendance was used based on participants replying to two SMS per week. The first asked how many times participants had completed their programme and the second if participants were ready to progress their exercise programme. This measure of attendance was chosen as it was deemed achievable for all participants regardless of device used and involved minimal participant burden.
Secondary outcomes were patient preference (centre-based or mPR), engagement with mPR (measured using system recorded data, eg app page views, SMS sent/received) and clinical outcomes: HRQoL (EQ5D-VAS),19 symptom score (COPD assessment tool (CAT)),20 dyspnoea (Modified Medical Research Scale (mMRC))21 and time in sedentary activities (sedentary behaviour questionnaire (SBQ)).
Statistical Analysis
A two-sample proportion test for non-inferiority was used to determine the required sample size to detect a difference between the attendance and completion at centre-based and mPR. We used a completion rate of 60% for the centre-based group based on previous research findings.22 Calculations were based on a non-inferiority margin of 30% between the groups. Using a statistical power of 80% the two-sample proportion test determined 50 participants would be required in the smallest group.
The non-inferiority null hypothesis in terms of Odds ratio was: Odds of completion in centre-based PR/Odds of completion in mPR ≥3.5 (equivalent to Cohen's d=0.5).23
Data were analysed using IBM SPSS Statistics (Version 26) and R environment for statistical computing24. All participants were included in an intention to treat analysis regardless of number of sessions attended. As the proportion of missing values was <5% no imputations were used for missing data. Between-group comparisons were analysed with independent sample t-tests and chi-square tests. In the primary model used to evaluate odds ratios, logistic regression was used with the dependent variable of “group”. The secondary model to detect predictor variables used multivariate logistic regression with the dependent variables “group” and “completion rate” of PR. An analysis of co-variance was used to determine between-group differences after controlling for baseline values. For both primary and secondary outcomes, one-sided non-inferiority null hypothesis tests were conducted with a non-inferiority margin equivalent to Cohen's d=0.5. These non-inferiority tests evaluated whether the differences between centre-based and mPR were smaller than a medium effect size corresponding to a clinically meaningful difference25. These tests evaluated whether the differences between the two interventions were smaller than clinically meaningful differences. Statistical significance level was set at 0.05 and 0.025 for the two-sided and one-sided hypothesis tests, respectively.
Results
A total of 129 participants were screened for eligibility and 105 recruited. Following recruitment, participants were asked their preference for delivery of PR; 67/105 (64%) selected centre-based and 38/105 (36%) mPR. Follow-up assessment was completed for 95/105 (90%) of participants; 63/67 (94%) from the centre-based PR group, and 32/38 (84%) from the mPR group. Flow of participants through the study can be seen in Figure 1. The demographic and clinical characteristics of participants at baseline can be seen in Table 1. Those who chose mPR were younger (p = 0.002) and more likely to be working (p = 0.0001). Due to the COVID-19 lockdown, the planned face-to-face follow-up assessment could only be completed for three (4%) centre-based and two (6%) mPR participants. Remaining participants completed the follow-up assessment over the telephone which further prevented the assessment of exercise capacity.
 |
Table 1 Baseline Characteristics of Participants by Preferred Intervention |
 |
Figure 1 Study flow diagram. |
Primary Outcome
The overall proportion of participants who attended ≥70% of the available sessions was 67%; 50/67 (75%) in the centre-based group, and 20/38 (53%) in the mPR group. Logistic regression showed the likelihood of completing PR was nearly twice as high if participants were enrolled in centre-based compared to mPR (odds ratio 1.90 95% CI [0.83–4.35]). We were unable to reject the non-inferiority null hypothesis (H0: Odds ratio ≥ 3.5, z-value = −1.446, p-value = 0.074), and thus we cannot confirm whether mPR achieves a completion rate which is not inferior to centre-based PR. A secondary model using multi-variate logistic regression assessed the impact of a set of predictor variables on the odds of participants completing PR (Table 2) and did not identify any significant predictors of completion. No multicollinearity existed between variables.
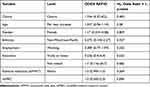 |
Table 2 Multivariate Logistic Regression |
The overall completion rate for the centre-based group was 75%. In the centre-based group, 13/67 (19%) participants reached the end of the intervention period prior to COVID-19 restrictions (pre-COVID-19 group). When restrictions were implemented 54/67 (81%) centre-based participants were impacted, of whom two participants declined telerehabilitation. The remaining 52/67 (78%) were subsequently given the choice of receiving their telerehabilitation via clinician-based, scheduled synchronous telephone calls or videoconferencing classes, with 41/52 (79%) opting for telephone and 11/52 (21%) videoconferencing. Attendance rates for both groups are shown in Figure 2.
 |
Figure 2 Box and whisker plot of attendance rates at PR. |
According to our a priori definition, the completion rate for the mPR group was 53%. In the mPR group, 3/38 (8%) opted to receive SMS only, 8/38 (21%) mPR-app and SMS, and the remaining 25/38 (66%) mPR-app, sensor, and SMS and 2/38 (5%) did not receive the intervention, see study flow diagram. The delivery of the mPR intervention was not affected by the COVID 19 lockdown.
Engagement in mPR
The mPR app dashboard was viewed by participants a total of 8593 times during the study period and videos were opened 1038 times. A total of 3932 SMS was sent to participants (mean per participant = 109.22, range 14–169). Of those who started mPR 33/38 (87%) engaged to some degree (responded to SMS or accessed the app). Of those registered to use the app, 25/33 (76%) were still accessing it in week 8, with 63% responding to SMS questions at week 8, but did not fulfil our a priori completion definition (ie they were responding to one rather than two SMS).
Secondary Outcomes
Centre-based participants demonstrated significant improvements in dyspnoea (mMRC), symptoms (CAT) and health-related quality of life (EQ5D-VAS), with no change in time spent in sedentary behaviours (SBQ) (Table 3). mPR participants showed improvement in symptoms (CAT) and reduced sedentary time (SBQ) but did not show improvement in dyspnoea (mMRC) or health-related quality of life (EQ5D-VAS). Statistical analysis showed mPR was not inferior in terms of changes in symptom score (CAT) or time spent in sedentary behaviour (SBQ), but we were unable to exclude non-inferiority for dyspnoea (mMRC) or HRQoL (EQ5D-VAS).
 |
Table 3 Outcome Measures Taken at Baseline and Follow-Up Assessments, Mean (Standard Deviation) |
One adverse event was reported; a participant in the mPR group fell whilst walking, injuring her shoulder and was unable to complete the intervention but participated in the follow-up assessment. No other adverse events were reported.
Discussion
This trial provides information regarding attendance and completion rates of PR when participants are given choice in delivery model. The likelihood of completing PR was nearly twice as high if participants were enrolled in centre-based PR compared to mPR, even when centre-based model were forced to transition to a telephone/VC model. Despite being almost twice as likely to complete in the centre-based group, this was not statistically significant and thus we cannot confirm whether mPR can achieve the same completion rate as centre-based PR. The centre-based completion rate is similar to a National UK audit rate26 and higher than a previous NZ audit at our centre where completion rates were 61%.22 We believe the forced transition of the centre-based group to telerehabilitation (due to COVID-19 restrictions), may be a contributor to this higher completion rate of the centre-based group in our study. This study has shown whilst 64% preferred centre-based PR, when forced to transition to telerehabilitation models (telephone and videoconferencing), an improvement in attendance and completion rates occurred in this group. This anomalous finding could be due to participants having already developed a therapeutic relationship with clinicians and peers, thus facilitating the desire to continue. Additionally, the telerehabilitation models were clinician led, scheduled, and synchronously delivered. This suggests that once a therapeutic relationship is established, participants may be more able to successfully transfer to remotely delivered PR and maintain this engagement at a distance. Previous home-based PR trials using telephone calls and videoconferencing have shown higher completion rates than centre-based PR14,27 and it has been suggested it is easier to “attend” a telephone call than travel to a centre,14 and this may have been one of the reasons for completion rates in our centre-based group increasing.
Our mPR programme was designed to be an asynchronous, “stand-alone” intervention with no scheduled clinician interactions, and whilst participants were advised they could contact a clinician through the mPR “contact us” page, only four participants did so. It is possible that adding regular contact points would establish a therapeutic relationship with the clinician and have the potential to enhance outcomes, as found in a trial of home-based PR with health coaching, where high patient adherence and satisfaction was attributed to the interactions with the physiotherapist.28 Interestingly, The American Thoracic Society suggests that regular contact between health care professionals and the patients was desirable rather than essential.29
Whilst the completion rate of mPR in this study was lower than that of centre-based (53% v 75%), several factors may have influenced this. The study was underpowered to determine non-inferiority due to recruitment stopping when national COVID-19 restrictions forced the closure of face-to-face services. The required sample size of 50 in the smallest group was not achieved with only 38 participants is the mPR group. We used a proxy measure of attendance to determine completion rates in the mPR group requiring participants to respond to two messages per week for 8-weeks. This may have underestimated the true completion rate of mPR, as our analysis showed that participants were more likely to answer general questions regarding progression of their exercise programme than the more specific question regarding frequency count of completed exercises. It is inherently difficult to measure engagement with digital health interventions30,31 and we are reliant on either subjective reports or system measures, such as participant logins, which indicate usage but do not provide information on fidelity to the intervention. In this study, we needed a measure of attendance which could accommodate the different levels of engagement participants had with the intervention, as some participants received mPR via SMS alone and others using mPR-app. Whilst we appreciate the limitations with this outcome measure, we are yet to determine accurate measures of attendance and fidelity with remotely delivered interventions and this needs ongoing consideration.
Previous studies investigating web-based programmes have shown a gradual decline in usage over time13,32, however this was not seen in our study. Based on responses to the two questions aimed at ascertaining attendance there were fewer responses in the first week suggesting technical or digital challenges may have been a factor at that point in time. Several authors have stressed the importance of training participants in the use of technology33,34 and the inclusion of technical support to facilitate this should be considered in any future work.
Our results show that whilst the majority of participants preferred centre-based PR, one-third of participants preferred mPR, and that for patients who are younger, employed and living in rural locations, mPR offered a useful alternative. Whilst there is limited data available on the uptake and completion of telerehabilitation in real-world settings, an implementation study reported 36% of participants opted for home-based PR with telephone support after declining centre-based PR,35 and our study supports this finding. It is likely as our population ages and digital confidence grows, the portion of participants opting for telerehabilitation options may also increase.
The improvements in clinical outcomes observed in both groups were lower than expected with significant improvements seen only for symptom scores in both groups. Whilst the centre-based group showed improvements in HRQoL, the mPR group did not. A meta-analysis of centre-based PR trials has shown improvements in HRQoL,36 with a recent Cochrane review showing equivalence in HRQoL outcomes between telerehabilitation and centre-based PR.37 However, our trial along with other pragmatic trials has failed to show improvements in HRQoL.14,16 Our study occurred during a pandemic when people living with a CRD felt particularly vulnerable which may have impacted on their feelings of anxiety, perceived health status and respiratory status. In people living with CRD in the UK undergoing COVID-19 restrictions, reductions in physical activity levels and HRQoL were observed,38 and it is likely that similar impacts may have occurred for participants in this study.
A major limitation of this study was our inability to measure changes in exercise capacity due to the restrictions in face-to-face contact which were imposed by the COVID-19 pandemic. Additionally, the inability to recruit to the target sample size due to COVID restrictions impacted the statistical power and thus our ability to clearly demonstrate non-inferiority between centre-based and mPR. Importantly, an advantage of the pragmatic trial design of this study was the broad inclusion criteria reflecting clinical practice and resulting in a low rate of participants declining participation in PR.
Conclusions
This trial has shown that whilst centre-based PR remained the preferred method of delivery for the majority of patients, mPR was preferred by 36% of participants and appealed to younger participants who are working and may have found attendance at centre-based programmes challenging. Attendance and completion rates were highest in the group who started centre-based and transitioned to telerehabilitation via telephone and videoconferencing during the COVID-19 pandemic, suggesting the opportunity to develop a therapeutic relationship with clinicians prior to remotely delivered PR may be important.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Human/Animal Ethics Approval Declaration
This trial was approved by the New Zealand Health and Disability Ethics Committee (HDEC) (21/NTB/54). The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12621000365864p). All patients provided written informed consent.
Acknowledgments
The authors wish to acknowledge all the participants who participated in this study. We also would like to acknowledge the PR and support staff at Te Whatu Ora Counties Manukau and Waitemata, and the staff at NIHI. This work was funded by the MedTech CoRE (Medical Technologies Centre of Research Excellence), a collaboration of Universities and Callaghan Innovation in New Zealand (cmdt.org.nz), and the Royal Arch Masons, NZ.
Funding
This work was funded by the MedTech CoRE (Medical Technologies Centre of Research Excellence), a collaboration of Universities and Callaghan Innovation in New Zealand (cmdt.org.nz), and from the Royal Arch Masons, NZ.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Maio S, Baldacci S, Carrozzi L, et al. Respiratory symptoms/diseases prevalence is still increasing: a 25-yr population study. Respir Med. 2016;110:58–65. doi:10.1016/j.rmed.2015.11.006
2. Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Article. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi:10.1164/rccm.201309-1634ST
3. Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand pulmonary rehabilitation guidelines. Respirology. 2017;22(4):800–819. doi:10.1111/resp.13025
4. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015. doi:10.1002/14651858.CD003793.pub3
5. Puhan MA, Gimeno‐Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;2016(12):CD005305. doi:10.1002/14651858
6. Dowman L, Hill CJ, May A, Holland AE. Pulmonary rehabilitation for interstitial lung disease. Review. Cochrane Database Syst Rev. 2021;2021(1):Cd006322. doi:10.1002/14651858.CD006322.pub4
7. Pasteur MC, Bilton D, Hill AT. British Thoracic Society guideline for non-CF bronchiectasis. Thorax. 2010;65(Suppl 1):i1–i58. doi:10.1136/thx.2010.136119
8. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. doi:10.1177/1479972310393756
9. Pfaeffli Dale L, Dobson R, Whittaker R, Maddison R. The effectiveness of mobile-health behaviour change interventions for cardiovascular disease self-management: a systematic review. Eur J Prev Cardiol. 2016;23(8):801–817. doi:10.1177/2047487315613462
10. Dobson R, Whittaker R, Jiang Y, et al. Effectiveness of text message based, diabetes self management support programme (SMS4BG): two arm, parallel randomised controlled trial. BMJ. 2018;361:k1959. doi:10.1136/bmj.k1959
11. Dobson R, Herbst P, Candy S, et al. Understanding end-user perspectives of mobile pulmonary rehabilitation (mPR): cross-sectional survey and interviews. Review. JMIR Form Res. 2019;3(4):e15466. doi:10.2196/15466
12. Whittaker R, Dobson R, Candy S, et al. Mobile pulmonary rehabilitation: feasibility of delivery by a mobile phone-based program. Article. Front Comput Sci. 2021:3546960. doi:10.3389/fcomp.2021.546960
13. Chaplin E, Hewitt S, Apps L, et al. Interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. BMJ open. 2017;7(3):e013682. doi:10.1136/bmjopen-2016-013682
14. Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: a randomised, controlled equivalence trial. Thorax. 2017;72(1):57–65. doi:10.1136/thoraxjnl-2016-208514
15. Cox NS, McDonald CF, Alison JA, et al. Telerehabilitation versus traditional centre-based pulmonary rehabilitation for people with chronic respiratory disease: protocol for a randomised controlled trial. Article. BMC Pulm Med. 2018;18(1):71. doi:10.1186/s12890-018-0646-0
16. Hansen H, Bieler T, Beyer N, et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Article. Thorax. 2020;75(5):413–421. doi:10.1136/thoraxjnl-2019-214246
17. Orkin AM, Gill PJ, Ghersi D, et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA. 2021;326(3):257–265. doi:10.1001/jama.2021.9941
18. Williams MT, Lewis LK, McKeough Z, et al. Reporting of exercise attendance rates for people with chronic obstructive pulmonary disease: a systematic review. Respirology. 2014;19(1):30–37. doi:10.1111/resp.12201
19. Rabin R, Charro F. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi:10.3109/07853890109002087
20. Tsiligianni IG, van der Molen T, Moraitaki D, et al. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm Med. 2012;12(1):1–9. doi:10.1186/1471-2466-12-20
21. Launois C, Barbe C, Bertin E, et al. The modified Medical Research Council scale for the assessment of dyspnea in daily living in obesity: a pilot study. BMC Pulm Med. 2012;12(1):1–7. doi:10.1186/1471-2466-12-61
22. Candy S, Jepsen N, Coomarasamy C, et al. Patient characteristics and predictors of completion of a pulmonary rehabilitation programme in Auckland, New Zealand. N Z Med J. 2020;133(1522):30–41.
23. Wang Y-X, Zhang Y-J. Nonnegative matrix factorization: a comprehensive review. IEEE Trans Knowl Data Eng. 2012;25(6):1336–1353. doi:10.1109/TKDE.2012.51
24. Team RC. R: A language and environment for statistical computing; 2013. Available from: https://cir.nii.ac.jp/all?q=http://www.R-project.org.
25. Sedaghat AR. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. 2019;161(4):551–560. doi:10.1177/0194599819852604
26. Steiner M, Holzhauer-Barrie J, Lowe D, et al. National COPD audit programme: pulmonary rehabilitation: time to breathe better; 2015.
27. Tsai LLY, McNamara RJ, Moddel C, Alison JA, McKenzie DK, McKeough ZJ. Home‐based telerehabilitation via real‐time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR Study. Respirology. 2017;22(4):699–707. doi:10.1111/resp.12966
28. Benzo RP, Kramer KM, Hoult JP, Anderson PM, Begue IM, Seifert SJ. Development and feasibility of a home pulmonary rehabilitation program with health coaching. Respir Care. 2018;63(2):131–140. doi:10.4187/respcare.05690
29. Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. An official American thoracic Society workshop report. Ann Am Thorac Soc. 2021;18(5):e12–e29. doi:10.1513/AnnalsATS.202102-146ST
30. Danaher BG, Boles SM, Akers L, Gordon JS, Severson HH. Defining participant exposure measures in Web-based health behavior change programs. J Med Internet Res. 2006;8(3):e542. doi:10.2196/jmir.8.3.e15
31. Yeager CM, Benight CC. If we build it, will they come? Issues of engagement with digital health interventions for trauma recovery. Mhealth. 2018;4:37. doi:10.21037/mhealth.2018.08.04
32. Bourne S, DeVos R, North M, et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. BMJ open. 2017;7(7):e014580. doi:10.1136/bmjopen-2016-014580
33. Alwashmi MF, Fitzpatrick B, Davis E, Farrell J, Gamble J-M, Hawboldt J. Features of a mobile health intervention to manage chronic obstructive pulmonary disease: a qualitative study. Ther Adv Respir Dis. 2020;14:1–25. doi:10.1177/1753466620951044
34. Vorrink S, Huisman C, Kort H, Troosters T, Lammers J-W. Perceptions of patients with chronic obstructive pulmonary disease and their physiotherapists regarding the use of an eHealth intervention. JMIR Human Fact. 2017;4(3):e7196. doi:10.1109/TKDE.2012.51
35. Bondarenko J, Babic C, Burge AT, Holland AE. Home-based pulmonary rehabilitation: an implementation study using the RE-AIM framework. ERJ Open Res. 2021;7(2):00469–2020. doi:10.1183/23120541.00469-2020
36. Lacasse Y, Martin S, Lasserson T, Goldstein R, Cook DJ, Goldstein RS. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet. 2007;348(9035):1115–1119. doi:10.1016/S0140-6736(96)04201-8
37. Cox NS, Dal Corso S, Hansen H, et al. Telerehabilitation for chronic respiratory disease. Review. Cochrane Database Syst Rev. 2021;1(1):CD013040. doi:10.1002/14651858.CD013040.pub2
38. Hume E, Armstrong M, Manifield J, et al. Impact of COVID-19 shielding on physical activity and quality of life in patients with COPD. Breathe. 2020;16(3):200231. doi:10.1183/20734735.0213-2020
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
