Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
The Impact of Nursing Interventions on the Treatment Outcomes of Renal Cell Carcinoma with Postoperative Interleukin-2 and Recombinant Human Interferon
Authors Guo L, Zhao LQ, Chen JY, Li M
Received 31 October 2023
Accepted for publication 30 January 2024
Published 17 February 2024 Volume 2024:17 Pages 735—741
DOI https://doi.org/10.2147/JMDH.S447537
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Li Guo,1 Li-Qin Zhao,2 Jin-Yu Chen,2 Ming Li2
1Third Department of General Surgery (Breast Armor Surgery), Ezhou Central Hospital, Ezhou City, 436000, People’s Republic of China; 2Department of Oncology, Ezhou Central Hospital, Ezhou City, 436000, People’s Republic of China
Correspondence: Ming Li, Department of Oncology, Ezhou Central Hospital, No. 9 Wenxing Road, Echeng District, Ezhou City, Hubei Province, 436000, People’s Republic of China, Tel + 86-15969693217, Email [email protected]
Objective: This study investigates the impact of nursing interventions on treatment outcomes and adverse reaction rates in renal cell carcinoma (RCC) patients treated postoperatively with Interleukin-2 and recombinant human Interferon.
Methods: In a retrospective analysis of 90 RCC patients, 43 received standard care (control group), while 47 received additional nursing interventions (intervention group), including psychological care, vital signs monitoring, dietary care, adverse reaction management, and post-discharge care. Patients with concurrent major diseases or other malignancies were excluded. Key assessments included clinical symptom improvement, treatment efficacy, and postoperative adverse reactions.
Results: Among the 90 participants, no significant demographic differences were found between the two groups. The intervention group showed significant improvements in fever resolution, leukocyte normalization, and shorter hospital stays. The overall treatment effectiveness was similar in both groups (90.7% in the intervention group vs 91.5% in the control group). However, the intervention group experienced significantly fewer postoperative adverse reactions, including fever, gastrointestinal symptoms, bone marrow suppression, and neurological abnormalities (6.3% vs 23.2%).
Conclusion: The study suggests that nursing interventions can improve treatment outcomes by reducing postoperative adverse reactions in RCC patients receiving postoperative Interleukin-2 and recombinant human Interferon. The overall effectiveness of treatment and care was comparable between the groups. Further extensive studies are needed to confirm these findings and fully understand the impact of nursing interventions on RCC patient outcomes.
Keywords: renal cell carcinoma, interleukin-2, recombinant human interferon, nursing interventions, treatment outcomes, adverse reactions
Introduction
Renal cell carcinoma (RCC) is the most common type of kidney cancer in adults, accounting for approximately 90% of all renal neoplasms.1 Over the past few decades, advancements in surgical techniques and adjuvant therapies have substantially improved the prognosis of RCC patients. Among these, postoperative treatment with Interleukin-2 (IL-2) and recombinant human Interferon has emerged as a potentially effective therapeutic approach.2,3
Adverse events documented with the use of high-dose IL-2 include hypotension, pre-renal azotemia, oliguria, and pulmonary edema. Pulmonary edema has been postulated to be caused by IL-2 activated NK cells and direct effect on vascular endothelium leading to capillary leak syndrome. Neurologic changes are one of the most common toxicities associated with high-dose IL-2 therapy. Hypotension, as a result of capillary leak syndrome, was one of the most commonly reported side effects from IL-2 treatment among the studies. Lower doses, prolonged infusions, and subcutaneous administration have been evaluated as strategies for improving IL-2 tolerability, but these regimens have produced response rates lower than those produced with high-dose regimens.4–7
Nursing interventions have been widely recognized as a critical component of comprehensive cancer care.8 By encompassing psychological care, vital sign monitoring, dietary guidance, adverse reaction management, and post-discharge care, nursing interventions can potentially enhance treatment adherence, improve symptom management, and alleviate adverse reactions.9,10 These holistic interventions can play a significant role in improving patients’ quality of life and overall treatment outcomes.11
However, existing literature lacks specific investigations into the impact of nursing interventions on the outcomes of RCC patients undergoing postoperative IL-2 and recombinant human Interferon therapy. Given this gap in the literature, the present study aims to assess the effectiveness of nursing interventions on treatment outcomes and adverse reaction rates in this particular patient population.
Methods
Study Design and Population
A retrospective cohort study design was implemented, with data being sourced from medical records of RCC patients who underwent postoperative treatment with Interleukin-2 (IL-2) and recombinant human Interferon at a tertiary care hospital between January 2020 and December 2022. Patients with co-existing cardiopulmonary, hepatic, renal, hematological, psychiatric, immune system diseases, or other malignant tumors were excluded from the study.
In this study, both the intervention and control groups consisted of patients with renal cell carcinoma. For the intervention group: 80% of patients had clear cell carcinomas, 20% had papillary RCC, 75% had tumors confined to the kidney, and 25% had local lymph node metastasis with no distant metastasis. For the control group: 83% had clear cell carcinomas, 17% had papillary RCC, 73% had tumors confined to the kidney, and 27% had local lymph node metastasis with no distant metastasis. Most patients in both groups presented with clinical symptoms of hematuria, abdominal masses, and abdominal pain. Statistical analysis revealed no significant differences in baseline characteristics of the study population between the intervention and control groups. This finding suggests that although there may be differences in lesion location and presentation status between the groups, these differences are not significant enough to affect the reliability of the statistical results.
Grouping and Interventions
Patients were grouped into a control group that received standard postoperative care, and an intervention group that received additional nursing interventions alongside standard care. The standard care included routine follow-up, wound care, medication management, and necessary medical interventions as per hospital protocol.12 The additional nursing interventions comprised psychological care, monitoring of vital signs, dietary care, management of adverse reactions, and post-discharge care.
The patients in this study underwent nephrectomy as the primary surgical treatment for RCC. Postoperative treatment with IL-2 and recombinant human Interferon began within two weeks after surgery. The dosage of IL-2 was administered at 600,000 IU/kg intravenously every 8 hours for a maximum of 14 doses, followed by a nine-day rest period. This cycle was repeated every 12 weeks. Recombinant human Interferon was given at a dose of 5 million units subcutaneously three times a week for 48 weeks. Treatment duration varied based on patient response and tolerance, with a maximum duration of one year.
Psychological Care: This included regular counseling sessions, stress management techniques, and support group meetings to help patients cope with their diagnosis and treatment. Dietary Care: Patients received tailored nutritional plans from the outset of treatment. Dietary adjustments were made based on individual needs and gastrointestinal symptoms, focusing on high-protein, low-fat diets, and adequate hydration. Management of Adverse Reactions: This involved proactive monitoring for symptoms of toxicity and prompt administration of symptomatic treatments. For instance, Anemia: Monitor hemoglobin levels and watch for fatigue or weakness. Administer iron supplements or erythropoietin as prescribed. Acute Kidney Injury: Regularly check kidney function and ensure proper hydration. Avoid nephrotoxic substances and adjust medications as needed. Hypotension: Monitor blood pressure closely. Support fluid intake and adjust the patient’s position slowly to prevent dizziness. Post-Discharge Care: Following discharge, patients received regular follow-up calls for the first month and biweekly thereafter. This included monitoring for any late-onset adverse effects, ensuring medication adherence, and providing guidance on lifestyle adjustments to support recovery. The type and frequency of vital sign assessment were consistent at every time point in both the intervention and control groups.
Outcome Measures
Primary outcomes included fever resolution time, leukocyte normalization time, length of postoperative hospital stay, and incidence of postoperative adverse reactions, such as fever, gastrointestinal symptoms, bone marrow suppression, and neurological abnormalities. The overall effectiveness of treatment and care was also assessed, including parameters like complete remission, partial remission, improvement, stability, and deterioration.
Complete resolution: The condition has completely resolved, and the patient is back to their normal state of health.
Partial resolution: Some improvement has been observed, but the condition has not completely resolved.
Improvement: The patient’s condition is getting better, but it has not yet fully resolved.
Stable: There is no significant change in the patient’s condition, either good or bad.
Deterioration: The patient’s condition is getting worse.
Statistical Analysis
Descriptive statistics were used to present demographic and clinical characteristics of the study population. Student’s t-test was used to compare continuous variables, and the chi-square test was used for categorical variables. All statistical tests were two-tailed, and a p-value of less than 0.05 was considered statistically significant. All analyses were performed using SPSS software.
Results
Patient Characteristics
This retrospective study included a total of 90 patients diagnosed with renal cell carcinoma (RCC) who underwent postoperative treatment with IL-2 and recombinant human interferon. 43 patients receiving standard care were divided into a control group, and 47 patients receiving additional nursing interventions were divided into an intervention group. There were no statistically significant differences between the two groups in terms of demographic characteristics, including gender, age, lesion location, and disease course, confirming the comparability of the two groups (Table 1).
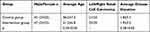 |
Table 1 The Demographic and Characteristics of Two Study Groups |
Outcome Measures
Primary outcome measures demonstrated that the nursing intervention group had significantly shorter fever resolution time, leukocyte normalization time, and postoperative hospital stay duration compared to the control group (p<0.05) (Table 2). Although the overall effectiveness of treatment and care (including complete remission, partial remission, improvement, stability, and deterioration) showed no statistically significant difference between the two groups (p>0.05), with rates of 90.7% and 95.8% in the intervention and control groups, respectively, the intervention group experienced notably fewer postoperative adverse reactions (Table 3).
 |
Table 2 Comparison of Clinical Symptom Improvement Between Two Groups ( |
 |
Table 3 Comparison of Treatment and Nursing Outcomes Between Two Groups (N%) |
Adverse Reactions
The incidence of postoperative adverse reactions, including fever, gastrointestinal symptoms, bone marrow suppression, and neurological abnormalities, was significantly lower in the intervention group compared to the control group (6.3% vs 23.2%, respectively, p<0.05) (Table 4).
 |
Table 4 Adverse Reactions After Surgery Between Two Groups |
Discussion
This study was aimed at assessing the impact of nursing interventions on the treatment outcomes and adverse reaction rates of RCC patients who underwent postoperative treatment with IL-2 and recombinant human Interferon. It employed a retrospective design to analyze the medical records of these patients and grouped them into two: a control group that received standard care and an intervention group that received additional nursing interventions, including psychological care, monitoring of vital signs, dietary care, management of adverse reactions, and post-discharge care. The study’s primary findings revealed that the nursing interventions led to significant improvements in the fever resolution time, leukocyte normalization time, and length of postoperative hospital stay.
Comparison with Previous Research
The findings from our study resonate with the conclusions of previous research which underscore the crucial role of nursing interventions in optimizing postoperative care outcomes.13 One study14 found that patients who received additional nursing care reported better management of symptoms and lower rates of postoperative complications compared to those receiving standard care alone. The objective of the study was to investigate the influence of comprehensive high-quality nursing care on postoperative complications, the degree of pain, and nursing satisfaction in these patients during the perioperative period. The results showed that the experimental group, which received comprehensive high-quality nursing, had significantly better outcomes in terms of reduced postoperative complications, lower pain scores, and higher nursing satisfaction compared to the control group. These findings are relevant to our study as they highlight the importance of nursing care quality in patient recovery. This highlights the importance of patient-focused nursing interventions in postoperative settings. However, our study stands apart by specifically focusing on RCC patients undergoing IL-2 and recombinant human Interferon therapy, which is a less explored patient demographic in the extant literature.
Interpretation of the Results
Our findings revealed significant improvements in fever resolution time, leukocyte normalization time, and postoperative hospital stay length in the intervention group. This suggests that targeted nursing interventions may expedite the postoperative recovery process.15 It noted that frequent monitoring of vital signs, including temperature, is key to early identification and management of febrile episodes, potentially explaining the observed reduction in fever resolution time. It is the intervention following the detection of early abnormalities that is crucial in reducing the adverse effects, not just the monitoring itself. The primary value of monitoring vital signs and white blood cell counts lies in its ability to provide early warning signs of potential complications. Once these signs are identified, timely and appropriate interventions can be implemented to mitigate or prevent the progression of adverse effects. The significance of leukocyte normalization time in assessing patients’ postoperative recovery and immune function status is paramount. This metric is vital for a comprehensive understanding of the patients’ biological response to both the surgical procedure and the nursing interventions implemented. Comprehensive post-discharge care could have resulted in reduced hospital stay duration.
Interestingly, the study also revealed a lower incidence of postoperative adverse reactions, including fever, gastrointestinal symptoms, bone marrow suppression, and neurological abnormalities, in the group receiving nursing interventions. This is consistent with the premise that nursing interventions, particularly those related to symptom management and adverse reaction monitoring, can minimize the severity and frequency of such complications.16
However, it should be noted that the overall effectiveness of treatment and care was similar between the two groups. This finding suggests that while nursing interventions may improve some specific postoperative outcomes, they may not necessarily influence the overall treatment trajectory in RCC patients undergoing IL-2 and recombinant human Interferon therapy.
Implications for Practice
The potential benefits of nursing interventions, as demonstrated in our study, underline the importance of integrating these practices into the routine care plan for RCC patients undergoing postoperative IL-2 and recombinant human Interferon therapy. Moreover, nursing interventions focused on psychological care, monitoring vital signs, dietary care, managing adverse reactions, and post-discharge care could be particularly beneficial.17 This multi-dimensional care model aligns well with the patient-centered care approach, which is becoming increasingly recognized for its role in improving patient satisfaction, engagement, and health outcomes.18 Therefore, healthcare professionals should consider developing and implementing comprehensive nursing intervention protocols in order to enhance the quality of care for RCC patients.
Post-discharge care for RCC patients in our study includes several key components designed to support the patient’s recovery and manage their health effectively outside the hospital setting. This care is tailored to each patient’s specific needs and typically includes the following elements:
Follow-up Appointments: Regularly scheduled follow-up appointments with healthcare providers to monitor the patient’s recovery and manage any ongoing health issues related to RCC or its treatment.
Medication Management: Assistance with medication adherence, including understanding the medication regimen, managing side effects, and ensuring continuity of care.
Symptom Monitoring: Education and tools for patients and caregivers to monitor for signs of complications or recurrence, such as changes in pain levels, urinary symptoms, or general health status.
Nutritional Guidance: Diet and nutrition advice specific to RCC patients to support overall health and recovery.
Physical Rehabilitation: Depending on the patient’s condition, physical therapy or exercises may be prescribed to enhance recovery and improve strength and functionality.
Psychosocial Support: Access to counseling services or support groups to help patients and their families cope with the emotional and psychological impacts of RCC and its treatment.
Health Education: Information on lifestyle changes and health behaviors that can support recovery and improve quality of life.
Limitations of the Study
This study is not without its limitations. First, due to the retrospective design, our ability to infer causality between nursing interventions and improved patient outcomes is limited.19,20 Future studies should consider employing randomized controlled trial designs to better ascertain causality. Second, the study was conducted in a single institution, which may limit the generalizability of the results. Moreover, certain unmeasured factors or confounders, such as differences in individual nursing practices or variations in patient health behaviors, could have potentially influenced the outcomes. Lastly, as the study only included patients without concurrent cardiopulmonary, hepatic, renal, hematological, psychiatric, immune system diseases, or other malignant tumors, the findings may not apply to patients with these conditions.
Future Research
Despite the limitations, our study lays the groundwork for future research in this area. Longitudinal, multicenter studies are needed to validate our findings in different settings and among a more diverse patient population. Future studies should also consider using more objective measures of patient outcomes, such as biochemical markers or imaging results, and evaluating other dimensions of nursing interventions, such as the frequency, intensity, or duration of interventions. Furthermore, given the complex nature of nursing care, qualitative research methods might also provide valuable insights into the underlying mechanisms through which nursing interventions affect patient outcomes.
Conclusion
In conclusion, this retrospective study has illuminated the potential benefits of nursing interventions for patients with renal cell carcinoma receiving postoperative treatment with Interleukin-2 and recombinant human Interferon. Our findings suggest that nursing interventions may enhance treatment outcomes and reduce postoperative adverse reactions, although the overall effectiveness of treatment and care was similar between the intervention and control groups. These findings underscore the importance of integrating comprehensive nursing care into the treatment regimen for these patients.
However, it is important to note that these findings are preliminary, and our study had several limitations, including its retrospective design, single-center setting, and potential confounding factors. Further research, particularly prospective, multicenter studies, is needed to confirm our findings and further elucidate the impact of nursing interventions on treatment outcomes in this patient population.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of the Ezhou Central Hospital, written informed consent was obtained from all subjects.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Funding
There is no funding to report.
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Ouyang D, Sun H, Chen N, Yan Y, Ma H, Xia J. Survival improvement in patients with renal cell carcinoma and disparities between different sexes, races, and socioeconomic status: 1977–2016. J Oncol. 2022;2022:1587365. doi:10.1155/2022/1587365
2. Negrier S, Escudier B, Lasset C, et al. Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. Groupe Français d’Immunothérapie. N Engl J Med. 1998;338(18):1272–1278. doi:10.1056/NEJM199804303381805
3. Figlin RA, Belldegrun A, Moldawer N, Zeffren J, deKernion J. Concomitant administration of recombinant human interleukin-2 and recombinant interferon alfa-2A: an active outpatient regimen in metastatic renal cell carcinoma. J Clin Oncol. 1992;10(3):414–421. doi:10.1200/JCO.1992.10.3.414
4. Baziar N, Jafarian K, Shadman Z, Qorbani M, Khoshniat Nikoo M, Abd Mishani M. Effect of therapeutic dose of vitamin d on serum adiponectin and glycemia in vitamin d-insufficient or deficient type 2 diabetic patients. Iran Red Crescent Med J. 2014;16(9):e21458. doi:10.5812/ircmj.21458
5. Pachella LA, Madsen LT, Dains JE. The toxicity and benefit of various dosing strategies for interleukin-2 in metastatic melanoma and renal cell carcinoma. J Adv Pract Oncol. 2015;6(3):212–221.
6. Schwartz RN, Stover L, Dutcher JP. Managing toxicities of high-dose interleukin-2. Oncology. 2002;16(11 Suppl 13):11–20.
7. Dutcher JP. Current status of interleukin-2 therapy for metastatic renal cell carcinoma and metastatic melanoma. Oncology. 2002;16(11 Suppl 13):4–10.
8. Cadet T, Davis C, Elks J, Wilson P. A holistic model of care to support those living with and beyond cancer. Healthcare. 2016;4(4):88. doi:10.3390/healthcare4040088
9. Li H, Li J, Wang X, et al. Systematic review and meta-analysis of the efficacy and safety of psychological intervention nursing on the quality of life of breast cancer patients. Gland Surg. 2022;11(5):882–891. doi:10.21037/gs-22-206
10. Singano V, van Oosterhout JJ, Gondwe A, et al. Leveraging routine viral load testing to integrate diabetes screening among patients on antiretroviral therapy in Malawi. Int Health. 2021;13(2):135–142. doi:10.1093/inthealth/ihaa030
11. McCorkle R, Ercolano E, Lazenby M, et al. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61(1):50–62. doi:10.3322/caac.20093
12. Luta X, Colomer-Lahiguera S, Martins Cardoso RJ, et al. Nurse-led consultation and symptom burden in patients with head and neck cancer: a comparative analysis of routine clinical data. Cancers. 2022;14(5):1227. doi:10.3390/cancers14051227
13. Aya HD, Cecconi M, Rhodes A. Perioperative haemodynamic optimisation. Turk J Anaesthesiol Reanim. 2014;42(2):56–65. doi:10.5152/TJAR.2014.2220141
14. Wei L, Hong Q, Lin X, et al. Effect of comprehensive high-quality nursing care on postoperative complications, degree of pain, and nursing satisfaction in gallstone patients during perioperative period. Am J Transl Res. 2021;13(4):2678–2685.
15. Liu A, Li M, Gao W, Wen X, Zhu H, Chen Y. Evaluating the impact of personalized rehabilitation nursing intervention on postoperative recovery of respiratory function among thoracic surgery patients: a protocol for systematic review and meta-analysis. Medicine. 2022;101(9):e28776. doi:10.1097/MD.0000000000028776
16. Hu J, Wang LL, Li Y. Effects of high-quality nursing intervention on negative emotions, postoperative complications and gastrointestinal function in patients with gastric cancer surgery. Am J Transl Res. 2022;14(3):1652–1662.
17. Riegel B, Westland H, Iovino P, et al. Characteristics of self-care interventions for patients with a chronic condition: a scoping review. Int J Nurs Stud. 2021;116:103713. doi:10.1016/j.ijnurstu.2020.103713
18. Kuipers SJ, Cramm JM, Nieboer AP. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv Res. 2019;19(1):13. doi:10.1186/s12913-018-3818-y
19. Liang F, Zhao Y, Yan X, et al. Choice of ANaesthesia for EndoVAScular treatment of acute ischaemic stroke at posterior circulation (CANVAS II): protocol for an exploratory randomised controlled study. BMJ Open. 2020;10(7):e036358. doi:10.1136/bmjopen-2019-036358
20. van den Berg GH, Huisman-de Waal GGJ, Vermeulen H, de van der Schueren MAE. Effects of nursing nutrition interventions on outcomes in malnourished hospital inpatients and nursing home residents: a systematic review. Int J Nurs Stud. 2021;117:103888.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

