Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
The Health-Related Quality of Life, Work Productivity, Healthcare Resource Utilization, and Economic Burden Associated with Levels of Suicidal Ideation Among Patients Self-Reporting Moderately Severe or Severe Major Depressive Disorder in a National Survey
Authors Benson C, Singer D, Carpinella CM, Shawi M, Alphs L
Received 27 June 2020
Accepted for publication 22 December 2020
Published 18 January 2021 Volume 2021:17 Pages 111—123
DOI https://doi.org/10.2147/NDT.S229530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Carmela Benson,1 David Singer,2 Colleen M Carpinella,3 May Shawi,4 Larry Alphs4
1Real-World Value & Evidence, Janssen Scientific Affairs, LLC, Titusville, NJ, USA; 2Jefferson College of Population Health, Thomas Jefferson University, Philadelphia, PA, USA; 3Real-World Evidence Health Division, Kantar Health, San Mateo, CA, USA; 4Neuroscience Medical Affairs, Janssen Scientific Affairs, LLC, Titusville, NJ, USA
Correspondence: Carmela Benson Director, Real-World Value & Evidence, Janssen Scientific Affairs, LLC, 1125 Trenton-Harbourton Road, Titusville, NJ 08560, USA
Email [email protected]
Background: Suicidal ideation (SI) is a cardinal aspect of major depressive disorder (MDD); however, patient-reported outcomes data from large-scale surveys are limited concerning SI in the context of MDD. This study aims to understand the association between varying levels of SI and health-related quality of life (HRQoL), work productivity, healthcare resource utilization (HRU), and associated costs in patients with moderately severe/severe MDD.
Methods: This was a retrospective, cross-sectional analysis of 2013 national survey data. Patients who self-reported moderately severe or severe MDD and completed the Short Form Survey Version 2 (SF-36v2), Work Productivity Loss and Activity Impairment questionnaire (WPAI), and questions related to HRU were analyzed. Direct and indirect costs were calculated. Patients were categorized and analyzed by the level of SI (no SI, low, moderate, and high) based on their response to Item 9 of the Patient Health Questionnaire-9.
Results: Among 75,000 respondents, 15.3% self-reported receiving a physician diagnosis of moderately severe or severe MDD and 2.8% of the total sample endorsed some level of SI. Patients with high SI showed a higher burden than patients with no SI, reporting lower mean SF-36v2 mental component summary scores (p< 0.001), higher work productivity loss (p=0.039), and higher numbers of per patient per month hospitalizations (p=0.002) and emergency room visits (p=0.011). High SI was associated with greater per patient per month direct costs ($1220 vs $796; p=0.002) and indirect costs ($1449 vs $1058; p=0.001) compared with no SI. When patients with low or moderate SI were compared with patients with no SI, the results were mixed.
Conclusion: Higher levels of SI were associated with lower HRQoL, greater HRU, and more work impairment resulting in higher direct and indirect costs compared with patients with MDD but no SI. These results highlight the need to implement effective treatment models and interventions in the employed population.
Keywords: major depression, suicidal ideation, economic burden, health-related quality of life
Introduction
Major depressive disorder (MDD) is a common, serious mood disorder with symptoms lasting for ≥2 weeks that can vary from mild to severe and affect feelings, thoughts, and daily activities.1,2 Depression is the leading cause of disability worldwide3,4 and is associated with significant health-related quality of life (HRQoL) impairment and economic burden.5–8 In 2018, an estimated 17.7 million adults in the United States (US) had at least 1 major depressive episode in the past year, representing approximately 7.2% of the adult population;9 the lifetime prevalence rate of major depressive episodes in the US has been estimated to be as high as 20.6%.10 The incremental economic burden of MDD in the US is considerable; in 2010, it was approximately $210.5 billion.7 This burden varies by the severity of depression symptoms; in a study of adults with treatment-resistant MDD, all-cause total healthcare costs, adjusted for baseline characteristics, were significantly greater for patients with moderate and severe depression symptoms relative to those with mild symptoms ($3455 and $5150 per patient per year, respectively).8
Suicidal ideation (SI) is a cardinal aspect of MDD.11 The link between MDD and suicide has been well established,12 with an estimated 31% of US adults with MDD experiencing past-year SI in 2017 (an increase from 26% in 2009).13 Suicide-related costs among patients with MDD are substantial; such costs were estimated to be $9.7 billion in the US in 2010, which was approximately 5% of the total incremental economic burden of adults with MDD.7
In the overall US population, suicide rates have been increasing,14 and MDD is among the most prevalent conditions associated with SI and suicidal behavior.15 While the humanistic and economic burden of MDD and SI have been investigated individually,5–8,16,17 less is known about the association between SI and the burden experienced by patients with MDD. The serious nature of SI suggests that its presence could lead to reduced HRQoL and increased economic burden. However, levels of SI vary across a spectrum and detecting its presence can be difficult. Moreover, the effect of SI could be subtle, such as decreasing work productivity or increasing utilization of acute care services. Given these potential challenges, the current study employed a broad, US-based survey that collected data from the Patient Health Questionnaire-9 (PHQ-9) to provide important insights into this patient population. The PHQ-9, a patient self-reported instrument, is aligned with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition symptom criteria for MDD and has been validated as a useful tool for the screening of depressive disorders and as a reliable and valid measure of depression symptom severity.18,19 Additionally, it has been shown to have a high sensitivity to identify patients who are at increased risk for suicide attempt or death over a range of risk levels.20–23
In the current study, we evaluated HRQoL, work productivity, healthcare resource utilization (HRU), and economic burden for patients with a diagnosis of moderately severe or severe MDD by increasing levels of SI in an effort to better understand how SI may be associated with these parameters.
Materials and Methods
Data Source
This was a retrospective, cross-sectional study that used the US National Health and Wellness Survey (NHWS), a self-report survey of the US adult population. The NHWS is a large, yearly, general health survey of US adults (18+ years). The survey instrument and study procedures used in the survey were reviewed and approved by the Essex Institutional Review Board (Lebanon, NJ). All participants provided informed consent. For the current study, data from the 2013 US NHWS (N=75,000) were used.
Sample
Adult patients who self-reported a physician diagnosis of depression and a score of ≥15 on the PHQ-924 were categorized as having moderately severe or severe MDD and were included in the analysis. PHQ-9 scores of 5, 10, 15, and 20 were previously identified as valid and responsible thresholds for the lower limits of mild, moderate, moderately severe, and severe depression, respectively, and scores of ≥15 were shown to be highly specific in predicting the presence of major depression.18 Patients who screened positive on the mood disorder questionnaire (MDQ) were excluded. The MDQ is a screening tool used to evaluate potential bipolar disorder.25 Both the PHQ-9 and MDQ criteria were used to ensure that the study population specifically had MDD. Furthermore, as HRU and cost burden increase with increasing MDD severity,8 the population with more severe MDD is of particular interest to clinicians and researchers.
Measures
Levels of Suicidal Ideation
Levels of SI were assessed using Item 9 of the PHQ-9.24 Increasing scores on this item have been shown to be associated with a higher risk of suicide in short- and long-term follow-up.20,22,23 Patients responded to the question: “Over the past 2 weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” Patients who scored 0 (not at all) were categorized as ‘no SI: depressed but without SI’; patients who scored 1 (several days), 2 (more than half the days), or 3 (nearly every day) were categorized as ‘low SI’, ‘moderate SI’, and ‘high SI’, respectively. Based on previous research,22 we expected to find a stepwise increase in the associated burden as PHQ-9 Item 9 scores increase.
Patient Demographic and Clinical Characteristics
Demographic characteristics collected from each respondent, including age, gender, race/ethnicity, marital status, education, employment status, household income, type of health insurance, and census region based on zip code, were used to characterize the patients. Further, the following clinical characteristics were also characterized: body mass index (BMI), cigarette smoking, alcohol consumption, exercise, self-reported physical and mental comorbidities associated with depression, and Charlson comorbidity index.26
Depression-Specific Measures
Respondents meeting the criteria for the MDD module of the survey completed additional depression-specific variables, including a family history of depression, length of diagnosis, whether the individual participated in talk therapy (yes/no), current medication(s) class(es), who prescribed the medication(s), and number of months on current medication. These variables were included to explore associations with patients’ level of SI.
Health-Related Quality of Life
Patients’ HRQoL was measured by the Short Form Survey Version 2 (SF-36v2).27 The SF-36v2 is a 36-item general validated measure of HRQoL across multiple populations.28 The measure was scored as two summary scores (physical [PCS] and mental [MCS] component summary scores) and as eight specific separate domain scores (see Appendix Table 1 and Appendix Table 2 for domain scores). These metrics were normed such that the population mean for PCS and MCS is 50. The minimal important difference (MID), or the smallest difference that a clinician would regard as important, is 3 points for PCS and MCS and 5 points for the eight health domain scales.29 The Short Form-6 Dimension (SF-6D) health utilities index was calculated using SF-36v2 items. Scores on the SF-6D range from 0 (death) to 1 (perfect health), and the general population mean score has been found to be 0.79–0.81 among a representative sample of UK respondents30 and 0.76–0.80 among US respondents.31 A MID of 0.041 points has been reported for the SF-6D.32
Work Productivity Loss and Activity Impairment
Work productivity loss and activity impairment in the past week was assessed by the 6-item Work Productivity Loss and Activity Impairment questionnaire (WPAI).33 The WPAI is a validated general measure widely used across several populations.34 This measure assesses presenteeism (time not productive while at work), absenteeism (time absent from work), and activity impairment (% of impairment in daily activities due to health). The overall work impairment was scored based on the aggregated absenteeism and presenteeism scores. Scores on the WPAI represent the percentage of time impaired in the past 7 days. Only respondents who were employed full- or part-time responded to the presenteeism and absenteeism questions.
Healthcare Resource Utilization
NHWS data include the number of traditional healthcare provider (HCP) visits (eg, general practitioner, internist, psychiatrist), number of hospitalizations, and number of ER visits respondents report having in the last 6 months. Using these data, mean utilization rates for patients with each level of SI were calculated for the 6-month recall period and then divided by 6 to estimate the mean per patient per month (PPPM) utilization.
Direct and Indirect Costs
The cost for an average HCP visit, hospitalization, and ER visit were obtained from the 2013 Medical Expenditure Panel Survey (MEPS) data.35 The 2013 mean values (US dollars) for each HRU type were: ER visit ($939), hospitalization ($13,097), and HCP visit ($200). To calculate mean PPPM direct costs for each HRU type, for each level of SI, the mean PPPM utilization rates were multiplied by the mean cost for the corresponding type of HRU.
Indirect costs were calculated based on responses to the WPAI for each employed respondent and by using 2013 median weekly income figures obtained from the Bureau of Labor Statistics.36 For each respondent, an hourly rate was estimated by dividing the median weekly income by the number of hours in the typical work week. Next, the number of hours missed in the last week because of one’s health (absenteeism) and the number of hours not productive in the last week because of health impairment while at work (presenteeism) were multiplied by the hourly rates to arrive at total lost wages for the week. These figures were then multiplied by the average number of work weeks in a year to obtain annual estimates. Finally, costs were divided by 12 to arrive at a PPPM estimate of indirect costs.
Analysis
The overall sample was analyzed by the level of SI. Patient demographic and clinical characteristics were assessed using descriptive statistics, using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Differences between the levels of SI groups were examined across all patient demographics, clinical characteristics, and outcomes. For categorical variables, chi-square tests were used to determine significant differences while analysis of variance was used for continuous variables. The focal comparison was between patients with high SI and those with no SI.
Results
Patient Demographics
Among 75,000 respondents to the 2013 US NHWS, 11,456 (15.3%) met the initial study inclusion criteria of a self-reported physician’s diagnosis of depression. From this group of patients, the analysis sample included the 2196 patients who scored ≥15 on the PHQ-9 and screened negative on the MDQ (Figure 1). Among all patients with moderately severe or severe MDD, 68.0% reported any SI. Those reporting any level of SI were younger (p-values ≤0.05 for each SI severity group compared with the no SI group), and the proportion of males increased with increasing levels of SI (p’s ≤0.01 for each SI severity group compared with the no SI group; Table 1). Across SI groups, commercial insurance coverage was reported by 41% to 47% of patients; the high SI group had the largest proportion of uninsured patients (28%) compared with the other SI groups (Table 1).
 |
Table 1 Demographic Characteristics by Level of Suicidal Ideation |
Clinical Characteristics
Clinical characteristics, including BMI, smoking status, and number and types of comorbidities, were generally similar across groups (Table 2). A higher proportion of patients with moderate SI (30%) and high SI (29%) reported social anxiety as a mental health comorbidity compared with patients with no SI (22%; p’s ≤0.014; Table 2). The most commonly used medications across patient groups were selective serotonin reuptake inhibitors and/or serotonin-norepinephrine reuptake inhibitors (Appendix Figure 1a and 1b). Use of bupropion, antipsychotics, and other medications was generally similar across SI groups; a higher proportion of patients with high SI (14%) and patients with moderate SI (12%) compared with those with no SI (6%) reported taking antipsychotics (p’s ≤0.005; Table 2).
 |
Table 2 Comorbidities and Depression-Specific Variables by Level of Suicidal Ideation Among Patients with Moderately Severe or Severe MDD |
Health-Related Quality of Life
Patients with high SI reported significantly lower mean SF-36v2 MCS scores compared with those with no SI (25.90 [SD=10.76] vs 29.01 [SD=9.25]; p <0.001; Table 3). Patients with high SI did not differ on their mean SF-36v2 PCS scores compared with those with no SI (p=0.796). Patients with high SI also reported significantly lower mean SF-6D health utility index scores compared with those with no SI (0.52 [SD=0.11] vs 0.54 [SD=0.09]; p <0.001; Table 3).
 |
Table 3 Health Outcomes and Direct and Indirect Costs by Level of Suicidal Ideation Among Patients with Moderately Severe or Severe MDD |
Work Productivity and Activity Impairment and Indirect Costs
Among employed patients, work productivity was not statistically significant across all levels of SI (p=0.104); however, patients with high SI showed significantly higher work productivity loss (absenteeism and presenteeism combined; 45% vs 39%; p=0.039; Table 3) compared with those with no SI. For example, this would equate to 18 hours of work productivity impairment per person compared with 15.6 impaired hours for an average 40-hour work week. Patients with high SI had higher activity impairment (60% vs 57%; p=0.087; Table 3) compared with those with no SI; however, this difference did not reach statistical significance. Patients with high SI incurred greater PPPM indirect costs ($1449 vs $1058; p=0.001; Table 3) compared with patients with no SI.
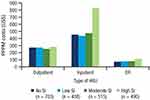
Healthcare Resource Utilization and Direct Costs
Patients with high SI reported significantly higher monthly rates of hospitalizations and ER visits compared with those with no SI (p’s <0.002; Table 3 and Figure 2), although there was no difference in HCP visits between these groups (p=0.679). Patients with high SI incurred greater PPPM direct costs ($1220 vs $796; p=0.002; Table 3) compared with those with no SI. Considering the total PPPM direct and indirect costs, monthly total costs for patients with high SI ($2475) were significantly higher than for those with no SI ($1714; p=0.010).
Discussion
To gain insights into the humanistic and economic burden of varying levels of SI in the context of MDD, we analyzed patients with moderately severe or severe MDD experiencing SI using the NHWS. Patients endorsing Item 9 of the PHQ-9, who comprised 2.0% of all NHWS respondents, were younger, more often male, and more often uninsured.
Health utilities observed in patients with high SI were significantly lower than in patients without SI. These utilities represent levels of overall HRQoL as low or lower than those observed in certain cancers and chronic pain.37,38 Patients with high SI had higher work productivity loss resulting in higher indirect costs compared with patients with no SI, which is unsurprising in the context of such low HRQoL. The results of this study showed most of the indirect cost was due to impairment at work (ie, presenteeism), suggesting that patients often show up to work despite the severity of their condition and demonstrate low productivity. The association between presenteeism and SI among patients with MDD is consistent with observations in a European population.39 Moreover, results from a previous study evaluating the relationship between depression symptoms and presenteeism have shown that cognitive symptoms accompanying depression, such as impaired concentration, anhedonia, and self-criticism, had a significant impact on presenteeism but were less important in predicting absenteeism.40 Using a multivariate model to compare patterns and severity of self-reported productivity impairment across several different medical conditions, depression was associated with the highest odds of problems with mental/interpersonal functioning tasks and with overall output.41 A linear relationship has been demonstrated in the literature, with more severe depression symptoms correlated with increased presenteeism.40,42 Poor work adjustment may be an important risk factor for suicidal behavior in people with mood disorders.43 One study showed that while overall social adjustment was not associated with suicide attempt history, individuals with poor work adjustment were significantly more likely to report a history of a suicide attempt.44
Among the patients with moderately severe or severe MDD in the current study, those with high SI had significantly higher rates of hospitalization and ER visits than those with no SI. While not all patients experience hospitalization or seek care, the cost of hospitalization accounted for the largest portion of direct costs in this study. These results support previous studies showing the high impact of hospitalization on the economic burden associated with MDD and SI.7,45 In 2010, almost $100 billion of the estimated $210.5 billion economic burden of MDD in the US was attributable to direct medical costs, and $20.5 billion was due to inpatient medical services.7 Data from the Agency for Healthcare Research and Quality reported that, in 2013, over 70% of emergency department (ED) visits related to SI resulted in admission or transfer to another hospital or facility compared with only 19% of all other ED visits.46 Among these SI-related ED visits that resulted in admissions, the aggregate cost of ED and inpatient care increased by 20% annually from 2006 to 2013.46
Such high HRQoL and economic burden highlight the need for effective screening and management of patients with MDD and SI. Considering the risk to these patients, it is important to note that several validated screening instruments to detect depression have been utilized in the primary care setting;47 however, challenges remain in identifying those at risk of suicidality.48,49 The PHQ-9 is a practical way to screen for and assess depression symptom severity in the real world given its inclusion in National Quality Forum (NQF)–endorsed quality measures, inclusion in Healthcare Effectiveness Data and Information Set (HEDIS) and Merit-based Incentive Payment System (MIPS) measures, and ease and frequency of use.24
Multiple health systems have published guidelines referencing or endorsing the use of the PHQ-9 in the screening and management of depression. One example is Kaiser Permanente which published a guideline specifically including recommendations around screening and treatment based on the PHQ-9.50 The Department of Defense and Department of Veterans Affairs published joint guidelines recommending the use of the PHQ-9 for initial measurement of depression severity as well as treatment monitoring.51 These examples support the use of the PHQ-9 in depression screening, making this tool even more relevant to clinicians. With routine use, there is an opportunity to more effectively identify patients with MDD, and to better identify patients with SI, providing a chance for treatment and management of these at-risk individuals.
Limitations
Despite the insight that this study provides into the burden associated with SI in patients with moderately severe or severe MDD, several limitations should be considered. First, the data source used for this analysis was based on a cross-sectional study design that does not permit causal conclusions to be drawn. The data were collected from self-reports of patients responding to a survey conducted online, and thus responses may be subject to recall bias, could not be objectively confirmed through review of medical records (including diagnosis of MDD), and may overrepresent certain types of individuals who are more comfortable with online engagement. Of note, the instruments used in the data source did possess relatively short recall periods and thus should have limited the degree to which recall bias influenced study results. However, because the work productivity measure reports only the prior week’s functioning, we are unable to establish conclusions regarding long-term impact or association. Moreover, different outcome measures had varying recall periods (ie, 4 weeks for SF-36v2, 7 days for WPAI, 6 months for HRU, and 2 weeks for the PHQ-9). Nevertheless, the results reported here trended as expected and were consistent with similar studies.6,7,16,39,45,46
The second limitation of this study was the absence of a clinical measure to categorize patients based on their level of SI. This analysis relied on using Item 9 on the PHQ-9 to form the basis for assessing patients’ suicidal level in the analysis, as it has been associated with the risk of suicide.20,22,23 However, limitations may exist in the wording of this question. The PHQ-9 asks about the presence of either thoughts of being dead, without specifically asking about suicide (“you would be better off dead”), or thoughts of self-injury (“hurting yourself in some way”). Moreover, the range of responses, including “several days” and “more than half of the days”, may be confusing for respondents, particularly if they did not consider the appropriate recall period of 2 weeks.
Additional limitations include the non-random assignment of patients based on their level of SI, which could lead to imbalances in risk factors between subpopulations and thus bias results. Since patients included in the analysis self-reported their physician diagnosed depression, the data do not provide codes to allow examination of specific depression subtypes. All combined, these limitations may limit the comparability and generalizability of the results.
Conclusions
Higher levels of SI among patients with moderately severe or severe MDD were associated with significantly lower HRQoL, greater HRU, and greater work impairment resulting in higher direct and indirect costs compared with patients reporting no SI. These findings emphasize the importance of examining direct, indirect, and total costs for patients with MDD experiencing SI. Considering the increased HRQoL and economic burden among patients with moderately severe or severe MDD and high SI observed in this study, from the payer and employer perspectives, it is important to ensure these patients are identified and receive appropriate intervention to avoid further worsening of their SI levels and increased economic burden.
Abbreviations
BMI, body mass index; ED, emergency department; ER, emergency room; HCP, healthcare provider; HEDIS, Healthcare Effectiveness Data and Information Set; HRQoL, health-related quality of life; HRU, healthcare resource utilization; MCS, mental component summary; MDD, major depressive disorder; MDQ, mood disorder questionnaire; MEPS, Medical Expenditure Panel Survey; MID, minimal important difference; MIPS, Merit-based Incentive Payment System; NHWS, National Health and Wellness Survey; NQF, National Quality Forum; PCS, physical component summary; PHQ-9, Patient Health Questionnaire–9; PPPM, per patient per month; SD, standard deviation; SF-6D, Short Form-6 Dimension; SF-36v2, Short Form Survey Version 2; SI, suicidal ideation; UK, United Kingdom; US, United States; WPAI, Work Productivity Loss and Activity Impairment questionnaire.
Data Sharing Statement
The data that support the findings of this study are available from Kantar Health but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from Carmela Benson ([email protected]) upon reasonable request and with permission of Kantar Health.
Acknowledgments
The authors acknowledge Errol J. Philip, PhD for his assistance with literature review and writing. Editorial support was provided by Courtney St. Amour, PhD, of MedErgy, and funded by Janssen Scientific Affairs, LLC. David Singer is currently affiliated with Boehringer Ingelheim Pharmaceuticals, Inc.; Colleen M. Carpinella is currently affiliated with Thermo Fisher Scientific; May Shawi is currently affiliated with Janssen Research & Development, LLC; and Larry Alphs is currently a consultant at Larry Alphs, MD, PhD Consulting.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Janssen Scientific Affairs, LLC.
Disclosure
Carmela Benson is a full-time employee of Janssen Scientific Affairs, LLC. May Shawi and Larry Alphs were full-time employees of Janssen Scientific Affairs, LLC at the time of the study. David Singer was a post-doctoral fellow with Thomas Jefferson University and reports a grant from Janssen Scientific Affairs, LLC at the time of the study. Colleen M. Carpinella was an employee of Kantar Health, which conducted this study with funding from Janssen Scientific Affairs, LLC, at the time of the study. The authors report no other conflicts of interest in this work.
References
1. National Institute of Mental Health. Depression; 2020. Available from: https://www.nimh.nih.gov/health/topics/depression/index.shtml.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association; 2013.
3. G.B.D. Disease Injury Incidence Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/S0140-6736(18)32279-7
4. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva, Switzerland: WHO Document Production Services; 2017.
5. Mitchell PM, Al-Janabi H, Richardson J, Iezzi A, Coast J. The relative impacts of disease on health status and capability wellbeing: a multi-country study. PLoS One. 2015;10(12):e0143590. doi:10.1371/journal.pone.0143590
6. Gauthier G, Guerin A, Zhdanava M, et al. Treatment patterns, healthcare resource utilization, and costs following first-line antidepressant treatment in major depressive disorder: a retrospective US claims database analysis. BMC Psychiatry. 2017;17(1):222. doi:10.1186/s12888-017-1385-0
7. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–162. doi:10.4088/JCP.14m09298
8. Pilon D, Sheehan JJ, Szukis H, et al. Is clinician impression of depression symptom severity associated with incremental economic burden in privately insured US patients with treatment resistant depression? J Affect Disord. 2019;255:50–59. doi:10.1016/j.jad.2019.04.100
9. Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration;2019.
10. Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. doi:10.1001/jamapsychiatry.2017.4602
11. American Psychiatric Association. Practice Guidelines for Treatment of Patients with Major Depressive Disorder.
12. Sokero P. Suicidal Ideation and Attempts Among Psychiatric Patients with Major Depressive Disorder. Helsinki: National Public Health Institute; 2006.
13. Kuvadia H, Wang K, Daly E, et al. National trends in the prevalence of major depressive disorder with suicidal ideation among adults using the National Survey on Drug Use and Health.
14. Hedegaard H, Curtin SC, Warner M. 2020. Increase in Suicide Mortality in the United States, 1999–2018. Hyattsville, MD: National Center for Health Statistics, NCHS Data Brief, no 362.
15. Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293(20):2487–2495. doi:10.1001/jama.293.20.2487
16. Shepard DS, Gurewich D, Lwin AK, Reed GA
17. Ballard ED, Horowitz LM, Jobes DA, Wagner BM, Pao M, Teach SJ. Association of positive responses to suicide screening questions with hospital admission and repeated emergency department visits in children and adolescents. Pediatr Emerg Care. 2013;29(10):1070–1074. doi:10.1097/PEC.0b013e3182a5cba6
18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
19. Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81(1):61–66. doi:10.1016/S0165-0327(03)00198-8
20. Simon GE, Coleman KJ, Rossom RC, et al. Risk of suicide attempt and suicide death following completion of the Patient Health Questionnaire depression module in community practice. J Clin Psychiatry. 2016;77(2):221–227. doi:10.4088/JCP.15m09776
21. Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi:10.1176/appi.ps.201200587
22. Rossom RC, Coleman KJ, Ahmedani BK, et al. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord. 2017;215:77–84. doi:10.1016/j.jad.2017.03.037
23. Louzon SA, Bossarte R, McCarthy JF, Katz IR. Does suicidal ideation as measured by the PHQ-9 predict suicide among VA patients? Psychiatr Serv. 2016;67(5):517–522. doi:10.1176/appi.ps.201500149
24. Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. doi:10.3928/0048-5713-20020901-06
25. Hirschfeld RM. The mood disorder questionnaire: a simple, patient-rated screening instrument for bipolar disorder. Prim Care Companion J Clin Psychiatry. 2002;4(1):9–11. doi:10.4088/PCC.v04n0104
26. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
27. Maruish ME, ed. User’s Manual for the SF-36v2 Health Survey.
28. Busija L, Pausenberger E, Haines TP, Haymes S, Buchbinder R, Osborne RH. Adult measures of general health and health-related quality of life: medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF-6D), Health Utilities Index Mark 3 (HUI3), Quality of Well-Being Scale (QWB), and Assessment of Quality of Life (AQoL). Arthritis Care Res. 2011;63(suppl11):S383–S412.
29. Ware JE, Kosinski M, Dewey JE, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Lincoln, RI: QualityMetric Inc; 2000.
30. van den Berg B. SF-6D population norms. Health Econ. 2012;21(12):1508–1512. doi:10.1002/hec.1823
31. Fryback DG, Dunham NC, Palta M, et al. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Med Care. 2007;45(12):1162–1170. doi:10.1097/MLR.0b013e31814848f1
32. Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523–1532. doi:10.1007/s11136-004-7713-0
33. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. doi:10.2165/00019053-199304050-00006
34. Tang K, Beaton DE, Boonen A, Gignac MA, Bombardier C. Measures of work disability and productivity: rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA), Workplace Activity Limitations Scale (WALS), Work Instability Scale for Rheumatoid Arthritis (RA-WIS), Work Limitations Questionnaire (WLQ), and Work Productivity and Activity Impairment Questionnaire (WPAI). Arthritis Care Res. 2011;63(suppl 11):S337–S349.
35. Medical Expenditure Panel Survey. Health care costs/expenditures; 2013. Available from: https://www.meps.ahrq.gov/mepsweb/data_stats/MEPS_topics.jsp?topicid=5Z-1.
36. US Census Bureau of Labor Statistics. Earnings; 2014. Available from: https://www.bls.gov/cps/earnings.htm.
37. Jeong K, Cairns J. Systematic review of health state utility values for economic evaluation of colorectal cancer. Health Econ Rev. 2016;6(1):36. doi:10.1186/s13561-016-0115-5
38. Torrance N, Lawson KD, Afolabi E, et al. Estimating the burden of disease in chronic pain with and without neuropathic characteristics: does the choice between the EQ-5D and SF-6D matter? Pain. 2014;155(10):1996–2004. doi:10.1016/j.pain.2014.07.001
39. Jaffe DH, Rive B, Denee TR. The burden of suicidal ideation across Europe: a cross-sectional survey in five countries. Neuropsychiatr Dis Treat. 2019;15:2257–2271. doi:10.2147/NDT.S204265
40. Johnston DA, Harvey SB, Glozier N, Calvo RA, Christensen H, Deady M. The relationship between depression symptoms, absenteeism and presenteeism. J Affect Disord. 2019;256:536–540. doi:10.1016/j.jad.2019.06.041
41. Burton WN, Pransky G, Conti DJ, Chen CY, Edington DW. The association of medical conditions and presenteeism. J Occupational Environmental Med. 2004;46(6 Suppl):S38–45. doi:10.1097/01.jom.0000126687.49652.44
42. Beck A, Crain AL, Solberg LI, et al. Severity of depression and magnitude of productivity loss. Ann Fam Med. 2011;9(4):305–311. doi:10.1370/afm.1260
43. Schneider B, Grebner K, Schnabel A, Hampel H, Georgi K, Seidler A. Impact of employment status and work-related factors on risk of completed suicide. A case-control psychological autopsy study. Psychiatry Res. 2011;190(2–3):265–270. doi:10.1016/j.psychres.2011.07.037
44. Lizardi D, Grunebaum MF, Burke A, et al. The effect of social adjustment and attachment style on suicidal behaviour. Acta Psychiatr Scand. 2011;124(4):295–300. doi:10.1111/j.1600-0447.2011.01724.x
45. Citrome L, Jain R, Tung A, Landsman-Blumberg PB, Kramer K, Ali S. Prevalence, treatment patterns, and stay characteristics associated with hospitalizations for major depressive disorder. J Affect Disord. 2019;249:378–384. doi:10.1016/j.jad.2019.01.044
46. Owens PL, Fingar KR, Heslin KC, Mutter R, Booth CL. Emergency department visits related to suicidal ideation, 2006–2013. HCUP Statistical Brief #220. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
47. Bienenfeld D Screening tests for depression; 2016. Available from: https://emedicine.medscape.com/article/1859039-overview.
48. O’Connor E, Gaynes B, Burda BU, Williams C, Whitlock EP. Screening for suicide risk in primary care: a systematic evidence review for the US Preventative Services Task Force. Evidence synthesis no. 103. AHRQ publication no. 13-05188-EF-1. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013.
49. Weber AN, Michail M, Thompson A, Fiedorowicz JG. Psychiatric emergencies: assessing and managing suicidal ideation. Med Clin North Am. 2017;101(3):553–571. doi:10.1016/j.mcna.2016.12.006
50. Kaiser Permanente. Adult & Adolescent Depression Screening, Diagnosis, and Treatment Guideline; 2017. Available from: https://wa.kaiserpermanente.org/static/pdf/public/guidelines/depression.pdf.
51. The Management of Major Depressive Disorder Working Group. VA/Dod Clinical Practice Guideline for the Management of Major Depressive Disorder. Washington, DC: VA/DoD; 2016.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.