Back to Journals » Infection and Drug Resistance » Volume 16
The Global Health Threat of Monkeypox Virus: Understanding Its Biology, Transmission, and Potential Therapeutic Interventions
Authors He Y , Tang Y, Wang C, Zhou Z , Li W, Tian M
Received 8 September 2023
Accepted for publication 13 December 2023
Published 21 December 2023 Volume 2023:16 Pages 7759—7766
DOI https://doi.org/10.2147/IDR.S438725
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yan He,1,* Ying Tang,2,* Caiyun Wang,3 Zilie Zhou,3 Wei Li,4 Man Tian3
1Department of Infection Management, Nanjing Drum Tower Hospital, Nanjing, Jiangsu, People’s Republic of China; 2Department of Ultrasound Diagnostic, Children’s Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 3Department of Respiratory, Children’s Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 4Department of Clinical Research, Children’s Hospital of Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wei Li; Man Tian, Email [email protected]; [email protected]
Abstract: Monkeypox virus (MPXV), a member of the Orthopoxvirus genus, shares its genus with Variola virus (VARV), the causative agent of smallpox, and Vaccinia virus (VACV), used for smallpox vaccination. While smallpox has been eradicated, MPXV and related poxviruses continue to pose a global health threat. Monkeypox (Mpox), similar in clinical presentation to smallpox but milder, is endemic in Central and West Africa. Sporadic outbreaks emphasize the potential for wider dissemination. Understanding their biology, transmission, immune evasion, and clinical features informs disease control strategies. The intersection of medical innovation and biotechnology with poxviruses underscores their importance in both disease and scientific advancement. Further research is essential to enhance prevention, management, and therapeutic interventions for these viruses.
Keywords: monkeypox, poxviruses, biology, epidemiology, vaccines and antivirals, biotechnology
Introduction
Monkeypox virus (MPXV) is a zoonotic virus belonging to the genus Orthopoxvirus, which includes variola, vaccinia and camelpox viruses. Monkeypox (Mpox) was first discovered in 1958 in a primate research facility in Denmark, with the first human case reported in 1970 in Democratic Republic of the Congo (DRC).1,2 In 1980, it was recognized by the World Health Organization (WHO) as the foremost Orthopoxvirus affecting humans since the eradication of smallpox.3 Outbreaks of Mpox have almost only occurred in several Sub-Saharan African countries in the past.4,5 Recently, however, outbreaks of Mpox have occurred in countries outside of Africa emphasize its potential for wider dissemination.6 The first report of Mpox, which led to the discovery of global outbreak, was made to WHO on May 13, 2022.7 From January 1, 2022 to October 31, 2023, 116 countries around the world has reported a total of 91,788 laboratory-confirmed cases and 660 probable cases, including a total of 167 deaths.8 This brief review aims to provide an in-depth understanding of MPXV and related poxviruses, exploring their biology, host interactions, immune responses, transmission dynamics, evolution, epidemiology, ecology, clinical features, pathogenicity, vaccine and antiviral development, and their role in biotechnological advancements.
Biology and Host Interactions
MPXV is a member of the Orthopoxvirus genus, characterized by its large, enveloped structure with a double-stranded DNA genome. Unlike most DNA viruses that replicate in the nucleus of the host cell, MPXV, akin to other poxviruses, carries out its replication cycle exclusively in the cytoplasm. This unique feature allows the virus to evade the host’s nuclear defense mechanisms and control the cellular machinery for its replication.9
The interactions between MPXV and its host are intricate and multifaceted, encompassing various aspects of immune evasion, host range determination, and pathogenesis. MPXV has evolved a plethora of strategies to evade the host’s immune response, including inhibiting apoptosis, blocking interferon activity, and manipulating cytokine responses.10,11 These mechanisms enable the virus to establish infection, propagate within the host, and contribute to the severity of the disease.
Serological studies indicate that Monkeypox virus has been found to infect various animal species under natural conditions, including squirrels, non-human primates, rabbits, and rats. However, the reservoirs for human infections remain unidentified, highlighting the need for further research in this area.12 The virus’s ability to infect a range of hosts can be attributed to its broad cellular tropism, facilitated by specific virus-host cell surface interactions.13
The pathogenesis of MPXV is a complex process that involves viral entry, replication, spread within the host, and immune response modulation. Understanding these intricate virus-host interactions is crucial for developing effective therapeutic strategies and preventive measures against this emerging infectious disease.
Dynamics of Pathogenicity and Life Cycle
PXV possesses both mature virions (MV) and enveloped virions (EV). The enveloped virion enters the host cell through fusion, while the mature virion employs micropinocytosis or fusion for entry. The MV is characterized by an outer lipoprotein envelope encapsulating the viral core and a lateral body containing proteins. This structure remains relatively stable in the external environment and plays a primary role in mediating transmission between hosts. On the other hand, the EV is formed by the lipid membrane wrapping around the MV periphery, a process derived from the Golgi apparatus or endosomes. Following viral DNA replication and protein assembly in the cytoplasm, MV is released through cell lysis, while EV exits the cell via exocytosis.14,15
The incubation period for Monkeypox, defined as the duration from exposure to symptom onset, typically ranges from 3 to 17 days.16 During this phase, infected individuals may feel well with no apparent symptoms. The disease initiates with a prodromal phase lasting 0–5 days, marked by fever, headache, muscle and backaches, chills, and fatigue. Subsequently, a rash emerges, initially on the face and later spreading to other body parts. The rash progresses through macules, papules, vesicles, and finally pustules. Although this evolution mirrors that of smallpox, the lesions in monkeypox are typically fewer in number.17 Additional symptoms may include lymphadenopathy (swollen lymph nodes), sore throat, cough, and shortness of breath. In some instances, severe complications like secondary bacterial infection, sepsis, bronchopneumonia, encephalitis, and corneal infection leading to blindness can occur.
Immune Responses
The immune response to MPXV is a complex interplay involving both innate and adaptive immunity.11,18 Innate Immunity: This is the body’s first line of defense against MPXV. Upon infection, the host’s innate immune system recognizes the virus through pattern recognition receptors (PRRs) that identify pathogen-associated molecular patterns (PAMPs) on the virus. This recognition triggers a cascade of signaling pathways leading to the production of type I interferons and pro-inflammatory cytokines, which inhibit viral replication and initiate an inflammatory response.19 Adaptive Immunity: This is the second line of defense and is specific to the pathogen. It involves both B-cell and T-cell responses. B-cells produce antibodies that can neutralize the virus, preventing its entry into cells.20 T-cells, on the other hand, can kill infected cells and produce cytokines that further aid in controlling the infection.
However, MPXV has evolved several strategies to evade these immune responses. For instance, it produces proteins that inhibit interferon signaling, prevent apoptosis of infected cells, and manipulate cytokine responses. The virus can also inhibit the function of natural killer cells, a critical component of innate immunity.21 Moreover, MPXV can interfere with the host’s adaptive immune response by suppressing T-cell activation and proliferation, and by inhibiting B-cell antibody production. These immune evasion strategies make MPXV a challenging pathogen to combat and highlight the need for effective vaccines and therapeutics to enhance the host’s immune response against this virus.12 Understanding these evasion mechanisms is crucial for developing such interventions.11
Transmission and Evolution
Mpox is transmitted through various routes, including person-to-person, animal-to-human, and indirect contact.22 Person-to-person transmission occurs through direct contact with infectious skin or lesions, such as through face-to-face interaction, skin-to-skin contact, kissing, and respiratory droplets from prolonged close contact.23 The virus can enter the body through broken skin, mucosal surfaces, or the respiratory tract. Transmission is possible within households and among sexual partners, with a higher risk for those with multiple sexual partners.24 According to WHO, the ongoing outbreak is largely occurring in networks of men who have sex with men, among cases with known data on sexual behaviour, 85.0% (28,504/33,522) identified as men who have sex with men.8
Animal-to-human transmission can occur through bites or scratches from infected animals, as well as during activities like hunting, skinning, trapping, cooking, playing with carcasses, or consuming animals.25 The extent of viral circulation in animal populations is not fully understood, prompting ongoing studies.
Additionally, according to the WHO, Mpox can be contracted through contaminated objects such as clothing or linens, sharps injuries in healthcare settings, or in community settings like tattoo parlors. Understanding and preventing transmission through these various pathways are crucial for effective control and prevention measures.
The evolutionary course of MPXV plays a pivotal role in unraveling its complex epidemiology,26 particularly concerning the potential for zoonotic spillover events. Genetic adaptations within MPXV influence its interactions with human cells, impacting transmission efficiency and clinical severity. This adaptation to the human host, coupled with zoonotic origins, accentuates the risk of spillover from animal reservoirs.27 Human activities, such as the handling of bushmeat, contribute to the increased risk of zoonotic pathogen spillover.28 The current Monkeypox outbreak intensifies concerns, highlighting the potential for spillover events with pandemic implications.29,30 Notably, the latest variant exhibits a milder clinical profile, suggesting an evolution in the virus’s clinical characteristics that may impact overall transmissibility.31
Anticipating and managing potential outbreaks requires a vigilant approach to monitoring MPXV evolution. Genomic surveillance provides critical insights, guiding the development of interventions and informing public health strategies to curb the spread of the virus. The focus on spillover events emphasizes the need for comprehensive measures to prevent and control zoonotic transmission, mitigating the risks posed by MPXV, as well as public health interventions aimed at reducing human-animal interactions that can lead to transmission.32
Epidemiology
The first human case of Mpox was reported in 1970 in DRC. Since then, Mpox cases have been reported in other parts of Central and West Africa, including Cameroon, Central African Republic, Gabon, Liberia, Nigeria, Republic of the Congo, and Sierra Leone.33 In 2003, there was an outbreak of Mpox in the United States. The outbreak was caused by contact with infected prairie dogs that had been imported from Ghana. There were 47 confirmed cases of Mpox in the United States during this outbreak.34
In 2017, there was an outbreak of Mpox in the United Kingdom. The outbreak was caused by contact with an infected person who had traveled to Nigeria. There were 8 confirmed cases of Mpox in the United Kingdom during this outbreak.35
In 2022, there has been an outbreak of Mpox in several countries outside of Africa. The outbreak is thought to have been caused by contact with infected animals or people who had traveled to Africa. From January 1, 2022, cases of mpox have been reported to the World Health Organization (WHO) from 116 member states spanning all six WHO regions. As of October 31, 2023, the WHO has been notified of a total of 91,788 laboratory-confirmed cases and 660 probable cases, among which 167 have resulted in death.8 Of the 84,072 cases where sex, age and region were available, 96.66% are male, 68.91% cases reported aged 18–39, The majority of cases are reported from the Region of the Americas(55,178/84,072, 65.63%), Table 1.9
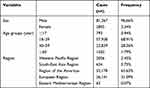 |
Table 1 The Distribution of Mpox Cases |
Clinical Manifestations and Their Diagnostic Findings
Mpox typically presents with clinical symptoms similar to those of smallpox, but generally, the disease course is less severe.36 The incubation period, ie, the time from exposure to the onset of symptoms, usually ranges from 7 to 14 days. The illness begins with a prodromal phase that lasts for 2–4 days, characterized by fever, headache, muscle aches, backache, chills, and fatigue. This is often followed by the development of a rash, initially appearing on the face and then spreading to other parts of the body. The rash progresses through stages from macules to papules to vesicles and then to pustules. This evolution is similar to that seen in smallpox, but the lesions are typically fewer in number.17 Other symptoms can include lymphadenopathy (swollen lymph nodes), sore throat, cough, and shortness of breath. In some cases, severe complications such as secondary bacterial infection, sepsis, bronchopneumonia, encephalitis, and corneal infection leading to blindness can occur.
While Mpox is usually self-limiting in healthy individuals, severe and fatal cases can occur, particularly in individuals with weakened immune systems, such as those with HIV/AIDS or those receiving immunosuppressive treatments. The MPXV exhibits distinct characteristics across its identified clades. Clade I is associated with a significant Case Fatality Rate (CFR) of up to 10% in humans. In contrast, Clade IIa demonstrates a substantially lower CFR, standing at less than 1%.37 The ongoing 2022–23 global Mpox outbreak is primarily linked to Clade IIb. Although the specific CFR for Clade IIb is not provided, the outbreak has resulted in 167 deaths among 92,448 cases, as of October 31, 2023.
Given the similarity in clinical presentation between Mpox and other diseases like smallpox, chickenpox, and even measles, accurate diagnosis often requires laboratory testing. Understanding these clinical features is crucial for early detection, appropriate treatment, and containment of outbreaks.
Vaccines and Antivirals
At present, there is no specific antiviral treatment or vaccine approved solely for the management or prevention of Mpox. However, a vaccine known as the “Smallpox Vaccine” has been used in specific circumstances to prevent Monkeypox infections. This cross-protection can significantly reduce the severity of Mpox symptoms or even prevent the disease in vaccinated individuals.36,38 Despite this, the use of the smallpox vaccine is limited due to safety concerns, particularly in certain populations such as individuals with compromised immune systems, pregnant women, and people with certain skin conditions.39
Two approved vaccines are notable for their relevance to Monkeypox Virus.40,41 ACAM2000 is a purified clone isolated from the Dryvax vaccine and is one of the approved vaccines to prevent smallpox in the USA. JYNNEOS is a modified vaccinia Ankara (MVA) vaccine. It is approved by the US Food and Drug Administration (FDA) and the European Medicine Agency (EMA) for use in preventing both smallpox and monkeypox. Additionally, a third-generation vaccine called LC16 m8 is noteworthy. It is an attenuated vaccinia virus derived from the Lister (Elstree) strain, licensed for active smallpox immunization in Japan since 1975.42
Scientists are actively developing vaccines for Monkeypox, relying on the unique properties of poxviruses, particularly the Vaccinia virus (VACV).43 Additionally, synthetic approaches, including synthetic peptides and mRNA vaccines, are being explored as alternative strategies, offering stability, specificity, and versatility in vaccine development.44 DNA vaccines, such as TNX-801, and mRNA vaccines by companies like Moderna, are in development, demonstrating the diverse approaches being explored to combat Monkeypox.45
Supportive care, including fluid management and treatment of secondary infections, remains the mainstay of therapy for patients with Mpox.46 In terms of antiviral therapy, several drugs are currently under investigation for their potential efficacy against MPXV. These include cidofovir and its oral prodrug brincidofovir, both of which have shown activity against poxviruses in vitro and in animal models.47,48 Another promising candidate is tecovirimat, an antiviral drug that was approved by the FDA for the treatment of smallpox in 2018.49 These drugs could potentially be repurposed for the treatment of Mpox, However, these drugs have drawbacks, including toxic side effects, limited availability, and the potential for resistance formation. To address these challenges, there is a need for additional, readily available drugs.
The development of a safe and effective vaccine or antiviral treatment specifically for Mpox is a crucial area of ongoing research. Such advancements would greatly enhance our ability to control outbreaks and reduce morbidity and mortality associated with this disease.
Limitations and Challenges of MPXV and Related Poxviruses
Mpox virus and related poxviruses pose several challenges and limitations in terms of understanding, prevention, and control of the diseases they cause. Here are some of the key challenges and limitations.
Limited Therapeutic Options: There are limited therapeutic options available for the treatment of Mpox and other related poxviruses. This limits the ability to manage and control outbreaks effectively.
Lack of Specific Vaccines: There is currently no specific vaccine for Mpox or other related poxviruses. The smallpox vaccine has been used with some success, but it is not specifically designed for these viruses.
Diagnostic Challenges: Diagnosing Mpox can be challenging due to its similarity to other diseases such as smallpox and chickenpox. This can lead to misdiagnosis and delays in treatment.
Zoonotic Transmission: Mpox is a zoonotic disease, meaning it can be transmitted from animals to humans. This complicates control measures and increases the risk of sporadic outbreaks.
Limited Understanding of Viral Pathogenesis: The exact mechanisms by which these viruses cause disease are not fully understood, which hinders the development of effective treatment strategies.
Emergence of Virulent Strains: The potential for the emergence of more virulent or drug-resistant strains of these viruses poses a significant challenge.
Bioterrorism Threat: Poxviruses, including Mpox, have potential as agents of bioterrorism. This presents a unique set of challenges in terms of detection, prevention, and response.
Geographical Distribution: The distribution of Mpox and related poxviruses is not fully understood, making it difficult to predict and prevent outbreaks.
Resource Constraints: Research into these viruses often lacks sufficient funding and resources, which can slow progress in understanding and controlling these diseases.
Public Awareness: There is often a lack of public awareness about these diseases, which can lead to delays in seeking treatment and contribute to disease spread. These challenges highlight the need for ongoing research and resources dedicated to understanding these viruses, improving diagnostic capabilities, developing specific vaccines and treatments, and enhancing public awareness and education about these diseases.
Conclusion
In conclusion, the persistent challenges posed by poxviruses, exemplified by the MPXV, highlight the ongoing importance of public health efforts, particularly in endemic regions. While the monumental success of smallpox eradication stands as a beacon, the occurrence of sporadic outbreaks and the heightened risk for severe disease in immunocompromised individuals underscore the imperative for sustained research and surveillance initiatives.
Advancements in understanding MPXV’s transmission dynamics, clinical manifestations, and evolutionary patterns have been substantial. Nevertheless, critical gaps persist in comprehending its epidemiology and ecology, necessitating further research to unravel the intricate interactions among the virus, animal reservoirs, and human hosts.
While the smallpox vaccine offers a degree of cross-protection against Mpox, the development of targeted antiviral treatments or a dedicated Mpox vaccine holds immense potential to bolster our capacity to manage outbreaks and curtail the associated morbidity and mortality.
Beyond their implications for public health, poxviruses emerge as invaluable tools in biotechnology, spanning applications from vaccine development to oncolytic virotherapy. The realization of these benefits, however, demands a judicious equilibrium and stringent oversight to mitigate associated risks.
In summary, the journey of ongoing research and surveillance into poxviruses, including MPXV, stands as a linchpin not only for upholding public health but also for propelling advancements in medical science and biotechnology. The pursuit of knowledge and vigilance in the face of evolving challenges remain paramount for a resilient and proactive global health landscape.
Abbreviations
MPXV, Monkeypox virus; Mpox, Monkeypox; VACV, Vaccinia virus; VARV, Variola virus; PRRs, Pattern Recognition Receptors; PAMPs, Pathogen-Associated Molecular Patterns.
Funding
This work was supported by China Postdoctoral Science Foundation (2022M721682), the Young Scientists Fund of the National Natural Science Foundation of China (82103896) and Nanjing Medical Science and Technology Development Foundation (ZKX20039).
Disclosure
None of the authors has any conflict of interest to disclose.
References
1. Sklenovská N, Van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front Public Health. 2018;6:241. doi:10.3389/fpubh.2018.00241
2. Parker S, Buller RM. A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012. Future Virol. 2013;8(2):129–157. doi:10.2217/fvl.12.130
3. Walter K, Malani PN. What is monkeypox? JAMA. 2022;328(2):222. doi:10.1001/jama.2022.10259
4. Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16(2):e0010141. doi:10.1371/journal.pntd.0010141
5. Ejaz H, Junaid K, Younas S, et al. Emergence and dissemination of monkeypox, an intimidating global public health problem. J Infect Public Health. 2022;15(10):1156–1165. doi:10.1016/j.jiph.2022.09.008
6. Reed KD, Melski JW, Graham MB, et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med. 2004;350(4):342–350. doi:10.1056/NEJMoa032299
7. Laurenson-Schafer H, Sklenovská N, Hoxha A, et al. Description of the first global outbreak of mpox: an analysis of global surveillance data. Lancet Glob Health. 2023;11(7):e1012–e1023. doi:10.1016/S2214-109X(23)00198-5
8. World Health Organization. 2022–23 Mpox (Monkeypox) Outbreak: global Trends. Available from: https://worldhealthorg.shinyapps.io/mpx_global/.
9. Harapan H, Ophinni Y, Megawati D, et al. Monkeypox: a comprehensive review. Viruses. 2022;14(10):2155. doi:10.3390/v14102155
10. Shchelkunov SN. Orthopoxvirus genes that mediate disease virulence and host tropism. Adv Virol. 2012;2012:524743. doi:10.1155/2012/524743
11. Qudus MS, Cui X, Tian M, et al. The prospective outcome of the monkeypox outbreak in 2022 and characterization of monkeypox disease immunobiology. Front Cell Infect Microbiol. 2023;13:1196699. doi:10.3389/fcimb.2023.1196699
12. Lucena-Neto FD, Falcão LFM, Vieira-Junior AS, et al. Monkeypox virus immune evasion and eye manifestation: beyond eyelid implications. Viruses. 2023;15(12):2301. doi:10.3390/v15122301
13. Alakunle E, Moens U, Nchinda G, Okeke MI. Monkeypox virus in Nigeria: infection biology, epidemiology, and evolution. Viruses. 2020;12(11):1257. doi:10.3390/v12111257
14. Kumar N, Acharya A, Gendelman HE, Byrareddy SN. The 2022 outbreak and the pathobiology of the monkeypox virus. J Autoimmu. 2022;131:102855. doi:10.1016/j.jaut.2022.102855
15. Schmidt FI, Bleck CK, Mercer J. Poxvirus host cell entry. Curr Opin Virol. 2012;2(1):20–27. doi:10.1016/j.coviro.2011.11.007
16. Center for Disease Control and Prevention. Poxvirus. Available from: https://www.cdc.gov/poxvirus/mpox/clinicians/clinical-recognition.html.
17. Petersen E, Kantele A, Koopmans M, et al. Human monkeypox: epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin North Am. 2019;33(4):1027–1043. doi:10.1016/j.idc.2019.03.001
18. Saghazadeh A, Rezaei N. Poxviruses and the immune system: implications for monkeypox virus. Int Immunopharmacol. 2022;113(Pt A):109364. doi:10.1016/j.intimp.2022.109364
19. Zandi M, Shafaati M, Hosseini F. Mechanisms of immune evasion of monkeypox virus. Front Microbiol. 2023;14:1106247. doi:10.3389/fmicb.2023.1106247
20. Lum F-M, Torres-Ruesta A, Tay MZ, et al. Monkeypox: disease epidemiology, host immunity and clinical interventions. Nat Rev Immunol. 2022;22(10):597–613. doi:10.1038/s41577-022-00775-4
21. Suraweera CD, Hinds MG, Kvansakul M. Poxviral strategies to overcome host cell apoptosis. Pathogens. 2020;10(1):6. doi:10.3390/pathogens10010006
22. Elsayed S, Bondy L, Hanage WP. Monkeypox virus infections in humans. Clin Microbiol Rev. 2022;35(4):e0009222. doi:10.1128/cmr.00092-22
23. Luo Q, Han J. Preparedness for a monkeypox outbreak. Infectious Medicine. 2022;1(2):124–134. doi:10.1016/j.imj.2022.07.001
24. Sah R, Abdelaal A, Reda A, et al. Monkeypox and its possible sexual transmission: where are we now with its evidence? Pathogens. 2022;11(8):924. doi:10.3390/pathogens11080924
25. Tajudeen YA, Oladipo HJ, Muili AO, Ikebuaso JG. Monkeypox: a review of a zoonotic disease of global public health concern. Health Promot Perspect. 2023;13(1):1–9. doi:10.34172/hpp.2023.01
26. Li H, Zhang H, Ding K, et al. The evolving epidemiology of monkeypox virus. Cytokine Growth Factor Rev. 2022;68:1–12. doi:10.1016/j.cytogfr.2022.10.002
27. Ellwanger JH, Chies JAB. Zoonotic spillover: understanding basic aspects for better prevention. Genet Mol Biol. 2021;44(Suppl 1):e20200355. doi:10.1590/1678-4685-GMB-2020-0355
28. Jagadesh S, Zhao C, Mulchandani R, Van Boeckel TP. Mapping global bushmeat activities to improve zoonotic spillover surveillance by using geospatial modeling. Emerg Infect Dis. 2023;29(4):742–750. doi:10.3201/eid2904.221022
29. Patiño LH, Guerra S, Muñoz M, et al. Phylogenetic landscape of Monkeypox Virus (MPV) during the early outbreak in New York City, 2022. Emerg Microbes Infect. 2023;12(1):e2192830. doi:10.1080/22221751.2023.2192830
30. Bryer J, Freeman EE, Rosenbach M. Monkeypox emerges on a global scale: a historical review and dermatologic primer. J Am Acad Dermatol. 2022;87(5):1069–1074. doi:10.1016/j.jaad.2022.07.007
31. Pan D, Nazareth J, Sze S, et al. Transmission of monkeypox/mpox virus: a narrative review of environmental, viral, host, and population factors in relation to the 2022 international outbreak. J Med Virol. 2023;95(2):e28534. doi:10.1002/jmv.28534
32. Saied AA, Metwally AA, Choudhary OP, Choudhary OP. Monkeypox: an extra burden on global health. Int J Surg. 2022;104:106745. doi:10.1016/j.ijsu.2022.106745
33. Saied AA, Dhawan M, Metwally AA, Fahrni ML, Choudhary P, Choudhary OP. Disease history, pathogenesis, diagnostics, and therapeutics for human monkeypox disease: a comprehensive review. Vaccines. 2022;10(12):2091. doi:10.3390/vaccines10122091
34. Centers for Disease Control and Prevention (CDC. Update: multistate outbreak of monkeypox--Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(27):642–646.
35. Vaughan A, Aarons E, Astbury J, et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Euro Surveill. 2018;23(38). doi:10.2807/1560-7917.ES.2018.23.38.1800509
36. Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22(8):1153–1162. doi:10.1016/S1473-3099(22)00228-6
37. Christodoulidou MM, Mabbott NA. Efficacy of smallpox vaccines against Mpox infections in humans. Immunother Adv. 2023;3(1). doi:10.1093/immadv/ltad020
38. Cheema AY, Ogedegbe OJ, Munir M, Alugba G, Ojo TK. Monkeypox: a review of clinical features, diagnosis, and treatment. Cureus. 2022;14:7. doi:10.1590/1678-4685-GMB-2020-0355
39. Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y. Prevention and treatment of monkeypox. Drugs. 2022;82(9):957–963. doi:10.1007/s40265-022-01742-y
40. Abdelaal A, Reda A, Lashin BI, et al. Preventing the next pandemic: is live vaccine efficacious against monkeypox, or is there a need for killed virus and mRNA vaccines? Vaccines. 2022;10(9):1419. doi:10.3390/vaccines10091419
41. Watarkar S, Upadhyay P, Ghosh S, et al. Vaccines for monkeypox disease and challenges in its production and distribution: a lesson from COVID-19 pandemic. Int J Surg. 2023;109(3):536–538. doi:10.1097/JS9.0000000000000016
42. Kenner J, Cameron F, Empig C, Jobes DV, Gurwith M. LC16m8: an attenuated smallpox vaccine. Vaccine. 2006;24(47–48):7009–7022. doi:10.1016/j.vaccine.2006.03.087
43. Sánchez-Sampedro L, Perdiguero B, Mejías-Pérez E, García-Arriaza J, Di Pilato M, Esteban M. The evolution of poxvirus vaccines. Viruses. 2015;7(4):1726–1803. doi:10.3390/v7041726
44. Lozano JM, Muller S. Monkeypox: potential vaccine development strategies. Trends Pharmacol Sci. 2023;44(1):15–19. doi:10.1016/j.tips.2022.10.005
45. Harrison C. Monkeypox response relies on three vaccine suppliers. Nat Biotechnol. 2022;40(9):1306–1307. doi:10.1038/s41587-022-01463-3
46. Shafaati M, Zandi M. Human monkeypox (hMPXV) re-emergence: host immunity status and current vaccines landscape. J Med Virol. 2023;95(1):e28251. doi:10.1002/jmv.28251
47. Baker RO, Bray M, Huggins JW. Potential antiviral therapeutics for smallpox, monkeypox and other orthopoxvirus infections. Antiviral Res. 2003;57(1–2):13–23. doi:10.1016/S0166-3542(02)00196-1
48. Chittick G, Morrison M, Brundage T, Nichols WG. Short-term clinical safety profile of brincidofovir: a favorable benefit-risk proposition in the treatment of smallpox. Antiviral Res. 2017;143:269–277. doi:10.1016/j.antiviral.2017.01.009
49. Hoy SM. Tecovirimat: first Global Approval. Drugs. 2018;78(13):1377–1382. doi:10.1007/s40265-018-0967-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
