Back to Journals » Clinical Interventions in Aging » Volume 16
The Electronic Frailty Index is Associated with Increased Infection and All-Cause Mortality Among Older Patients with Primary Lung Cancer: A Cohort Study
Authors Shen Y, Wang Y, Shi Q, Hou L, Chen X, Dong B , Hao Q
Received 20 August 2021
Accepted for publication 4 October 2021
Published 11 October 2021 Volume 2021:16 Pages 1825—1833
DOI https://doi.org/10.2147/CIA.S335172
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Yanjiao Shen,1,* Yuting Wang,2,* Qingyang Shi,1 Lisha Hou,3 Xiaoyan Chen,4 Birong Dong,3 Qiukui Hao3,5
1Department of Guideline and Rapid Recommendation, Cochrane China Centre, MAGIC China Centre, Chinese Evidence-Based Medicine Centre, West China Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China; 2Department of Health Research Methods, Evidence and Impact, McMaster University, Hamilton, Canada; 3The Center of Gerontology and Geriatrics/National Clinical Research Center of Geriatrics, West China Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China; 4Zigong Mental Health Center, Zigong, Sichuan, People’s Republic of China; 5School of Rehabilitation Science, McMaster University, Hamilton, Ontario, Canada
*These authors contributed equally to this work
Correspondence: Qiukui Hao
The Center of Gerontology and Geriatrics/National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University, #37 Guoxue Lane, Chengdu, 610041, People’s Republic of China
Tel/Fax +86-28-85422321
Email [email protected]
Introduction: To assess whether the electronic frailty index (eFI) is independently associated with all-cause mortality and chemotherapy adverse reactions among older Chinese patients with lung cancer.
Methods: This is a retrospective, single-institution, chart review, and not a prospective cohort study. All patients ≥ 60 years with primary lung cancer in the West China Hospital from 2010 to 2017 were included in this cohort. The eFI was established using 35 frailty-related variables in the electronic medical record (EMR) system and was cut by a value of 0.2 to classify the patients into frail (eFI ≥ 0.2) and robust/non-frail groups (eFI< 0.2). The long-term outcome was all-cause mortality identified by government databases and telephone interviews. Short-term outcomes were any infection, bone suppression, chemotherapy discontinuation, impaired liver function, any gastrointestinal reactions and length of hospitalization. An inverse probability weighting method was used to eliminate the potential confounders. An adjusted Kaplan–Meier estimator and a weighted Cox model were used to calculate the survival and hazard ratio. A weighted logistic model was used to calculate the odds of short-term outcomes.
Results: A total of 997 patients were included in this study with a median follow-up of 34 months. Compared with non-frail patients, frail patients had an increased risk of mortality and shortened overall survival (hazard ratio [HR] of mortality, 1.29; 95% confidence interval [CI], 1.05 to 1.60; adjusted restricted mean survival time [aRMST] difference, − 5.68 months; 95% CI, − 10.15 to − 1.21 months). For short-term outcomes, frail patients had increased odds of infection compared to non-frail patients (odds ratio, 1.83; 95% CI, 1.09 to 3.06). No other outcome showed a significant result.
Conclusion: This study of older Chinese patients with primary lung cancer suggests that eFI-based frail patients had worse prognoses with increased risk of all-cause mortality and shortened survival times.
Keywords: electronic frailty index, all-cause mortality, lung cancer
Introduction
Lung cancer is one of the most common causes of cancer-related deaths1–3 and is frequently treated with chemotherapy. Currently, most of the pre-chemotherapy assessments are based on clinicians’ empirical judgments. Both tumor-related factors such as clinical staging and host-related factors such as sarcopenia or overall health status are known to influence lung cancer prognosis.3–5 A study of older patients with non-small cell lung cancer suggested that comprehensive geriatric assessment (CGA) could help improve the therapeutic management of older lung cancer patients.6
Frailty is a state of being most commonly observed that increases in prevalence with age in which the physiological reserves and stress responses of an individual’s body are severely diminished such that the affected individual is more vulnerable to harm.7 Frail individuals are at a higher risk of negative events such as falls, delirium, disability, admission to a long-term care facility, and death.7–11 Approximately 11% of adults over the age of 65 and 25–50% of adults over 85 are considered to be frail in high-income countries.12 The frailty index (FI) is the ratio of health defects present in the older patients to all measured variables based on the deficits accumulation theory,13–17 including symptoms, clinical findings, or laboratory test results.16 FI scores are generally defined by enumerating the number of deficits in a given individual and dividing by the total possible number to yield a score from 0–1, with higher scores corresponding to a greater degree of frailty.15,16 FI scores based upon laboratory test results (FI-LAB) and electronic FI (eFI) scores have both been shown to be predictive of a number of long-term negative outcomes including hospitalization, admission to a long-term care facility, and death.11,18–20 We strive for everyone to receive optimal quality of care, we strive to identify frailty to improve prognostication and individualization of treatment strategy.7,21–23
Previous studies found that the eFI was associated with increased risk of adverse outcomes in community-dwelling older people19 and in patients with disease such as hip fractures24 or heart failure.25 Our team conducted a cohort study and found that the frailty index based on routine laboratory data can predict the risk of mortality and other adverse clinical events in patients with lung cancer.20 The role of the frailty index-based on electronic medical record in predicting mortality and chemotherapy-related adverse events in the older Chinese population is not well understood. We used a previous established cohort with a longer follow up to evaluate the relationship between eFI-based frailty determination and all-cause mortality and other adverse events in older Chinese patients with lung cancer.
Methods
Data Source and Study Population
The study was conducted using data from the electronic medical record (EMR) system in the West China Hospital from 2010 to 2017. The analysis is based on the same dataset of a paper published in this journal by the same research group.20 The data were extracted independently and cross-checked by two investigators. We included the patients if they 1) were diagnosed with primary lung cancer, 2) underwent chemotherapy, and 3) were aged ≥60 years at the diagnosis of lung cancer. We excluded the patients if 1) the diagnosis date of lung cancer was unclear or missing, 2) the discharge diagnoses of adverse events of interest were unclear or missing, 3) the eFI-related variables were incomplete. The verbal informed consent was approved by the Ethics Review Committee of West China Hospital (No.2018-94), and that this study was conducted in accordance with the Declaration of Helsinki.
Electronic Frailty Index
The eFI values were calculated based upon an internationally established cumulative deficit model that can be used to measure baseline frailty status in a given patient,16 we selected 35 health-related variables with 10 domains from the EMR, including cardiovascular diseases (3 variables), respiratory diseases (3 variables), digestive diseases (3 variables), endocrine diseases (3 variables), urinary diseases (2 variables), nervous diseases (1 variables), immune diseases (1 variable), osteoarthritis (1 variable), symptoms (11 variables), general information (6 variables) and signs (1 variable) (see details in Appendix Table 1).
Each variable was defined with the binary indicators 0 and 1 for normal and abnormal or no and yes, respectively. The final eFI was defined as the sum of indicator 1 divided by the total number of eFI variables. For example, the number of indicator 1 variables was 10 and the number of total eFI was 35, the final eFI was calculated as 10/35 or 0.29. The range of the eFI was 0 to 1, with higher eFI values indicating higher degrees of frailty. We followed previous studies in the classification of frail and non-frail/robust patients using a cutoff of 0.2.3,26
Time Zero and Follow-Up
Patient mortality information was initially obtained from a local government mortality database on 1 April 2018. From March 1, 2019 to March 7, 2019, three trained research assistants then conducted telephone-based follow-up (interviews) to assess patients’ survival status and got the time of death for all survivors identified in above-mentioned mortality database. Time zero of this cohort study was set as the date of lung cancer diagnosis. Patients were followed from time zero to the administrative end of follow-up (March 1, 2019) or death, whichever came first. All death-free patients that were not followed until the administrative end were labeled as censoring.
Outcomes
The primary outcome of interest was time to death (also referred to as survival time). We used hazard of death and restricted mean survival time to measure this outcome. The identification of death was assessed by three well-trained researchers via telephone interviews. The secondary outcomes were all short-term outcomes, including infection (both bacterial and fungal infection), bone suppression (leucopenia (<3.5*109/L), neutropenia (<1.8*109/L), thrombocytopenia (<100*109/L), decreased hemoglobin (≤110g/L), chemotherapy discontinuation, impaired liver function (abnormal transaminase, alanine aminotransferase [ALT ≥ 50 IU/L], aspartate aminotransferase [AST ≥ 40 IU/L]), gastrointestinal reactions, and length of hospitalization.
Covariates
We identified a series of covariates that were potentially associated with both the frailty index and death or other outcomes. We sequentially adjusted the covariates by three models: 1) model 1 adjusted for age and sex. 2) model 2 further adjusted for smoking, alcohol intake, and BMI, and 3) model 3 further adjusted for invasive examination, histology, clinical stage, metastasis, regimen of chemotherapy, and radiotherapy.
Statistical Analyses
We described the study population using mean and standard deviation for normally distributed continuous variables or median and interquartile for non-normally distributed continuous variables, and number and percentage for binary variables. The t-test, chi-square test, and Mann–Whitney U-tests were used, where appropriate, for analyzing between-group differences. We classified patients with eFI < 0.2 as non-frail patients and as the reference group.3,26 The effect of eFI was defined as the effect of frail patients compared with that of non-frail patients.
We used the inverse probability weighting (IPW) method for the confounders.27,28 Multinomial logistic regressions were used to generate the probability of propensity of the groups, and then distribution comparisons were used to check the balance of covariates between the groups. The entropy balance method was used to handle the IPW of continuous eFI. For all-cause mortality, we used the IPW Cox model and the IPW restricted mean survival time (RMST) difference to measure the effect. We used the adjusted Kaplan–Meier estimator and drew the survival curve. For short-term outcomes, we used logistic regression to model the odds and quantile regression to model the length of hospitalization, along with the IPW adjustment. In addition, we modeled the effect of per unit and per 1 SD eFI instead of the categorized eFI groups to test the robustness. All analyses were done using R 4.0.5. We used a threshold two-sided P value of 0.05 to define statistical significance.
Results
Baseline Characteristics
We identified a total of 1263 lung cancer patients ≥60 years who had undergone chemotherapy between 2010 and 2017. Among them, 165 cases were excluded because of incomplete medical records and 101 cases because the date of diagnosis of lung cancer was unknown or missing. We finally included 997 eligible patients with 196 (19.66%) patients that were classified as frail (eFI ≥0.2). The study population had the following characteristics: the mean age and BMI were 66.07 years (SD, 4.9) and 22.61 kg/m2 (SD, 3.0), respectively; 71.20% of patients were male; 58.80% and 38.60% of patients had no history of drinking or smoking, respectively. For between-group comparisons (frailty vs non-frailty), smoking, histology, metastasis, clinical stage, and radiotherapy suggested important differences with more than 0.25 standardized mean difference (SMD) (Table 1).
 |
Table 1 Characteristics of Study Population |
Frailty and All-Cause Mortality
A total of 681 patients died during the follow-up, with a median survival time of 30 months (IQR, 16.80 to 45.33). After adjusting for several confounders, we found that frail patients had a higher risk of all-cause mortality compared with non-frail patients (hazard ratio [HR], 1.29; 95% confidence interval [CI], 1.05 to 1.60). Similar results were found for the adjusted overall survival (aOS), namely, that frail patients survived 5.68 months less than non-frail patients (95% CI, 1.21 to 10.15 months) (Table 2 and Figure 1). We provided a adjusted OS nomogram based on eFI score in Appendix Figure 1. The effects of per 0.1 and per 1 SD of eFI were consistent with that of dichotomous frailty (per 0.1: HR, 1.18; 95% CI, 1.06 to 1.32; per 1 SD: HR, 1.13; 95% CI, 1.04 to 1.22) (Appendix Table 2).
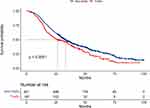 |
Figure 1 Kaplan–Meier curves displaying survival probability of all-cause mortality according to frail and non-frail patients. |
Frailty and Short-Term Outcomes
During hospitalization, a number of separate short-term outcomes were observed. These were infections (84 patients), bone suppression (174 patients), discontinuation of chemotherapy (22 patients), impaired liver function (67 patients), and gastrointestinal reactions (56 patients). After adjusting for all potential confounders, only “infection” was shown to have higher odds in frail patients (odds ratio [OR], 1.83; 95% CI, 1.09 to 3.06) (Table 2). The odds of bone suppression and chemotherapy discontinuation were significantly higher in frail patients after adjustment for age, sex, smoking, alcohol intake, and BMI (bone suppression: OR, 1.64; 95% CI, 1.09 to 2.46; chemotherapy discontinuation: OR, 2.69; 95% CI, 1.10 to 6.61) but were non-significant after adjustment all confounders (Table 2). The median length of hospitalization was 13 days (IQR, 9 to 19 days). There was no significant difference between frail and non-frail patients in the adjusted median length of hospitalization. Similar results were found in the effect of per 0.1 and per 1 SD of eFI (Appendix Table 2).
 |
Table 2 Effects of Frailty vs Non-Frailty on All Outcomes |
Discussion
In this cohort study consisting of 997 older patients with primary lung cancer, we investigated the relationship between eFI-based frailty and all-cause mortality in a median of 2.5 years follow-up, as well as chemotherapy-related short-term outcomes during hospitalization. To the best of our knowledge, we are the first to assess eFI-based frailty in the older Chinese population with lung cancer.
The results demonstrated that the eFI-defined frail patients had worse overall survival and a higher risk of mortality. The similar effects of per 0.1 and per 1 SD of eFI indicated the robustness of these results. This finding is consistent with a previous study in the same population.20 That study used 44 laboratory variables to construct the frailty index (FI-LAB) and found that the FI-LAB-defined frail patients had a greater risk of mortality. Our study built on that study and further used statistical methods to estimate the adjusted overall survival to complement the relative effect which generally suffers from poor interpretability and to facilitate shared decision-making. Our findings also provide an improved understanding of the prognostic value of eFI-based frailty in this specific clinical scenario.
Besides the mortality, we investigated short-term outcomes and found that eFI-based frailty was associated with an increased risk of infection. Chemotherapy often affect patients’ immune system function, so patients with lung cancer after chemotherapy are more likely to develop lung infections,29,30 and similarly, frail patients are at increased risk of infection.20 Our study suggests that frailty further increases the risk of infection even after adjusting the confounding factors such as chemotherapy regimens in patients with lung cancer, but we are unable to answer the question of its causality because of the present study is a retrospective cohort study we can not adjusted all confound factors. Our study found no statistically significant association between eFI and other outcome indicators including bone suppression, chemotherapy discontinuation, impaired liver function, gastrointestinal reactions, longer length of hospitalization. This may be related to a lack of statistical power due to small sample size in this study. The associations between eFI and these outcomes need to be confirmed by prospective cohort studies idealy with multicentre and large sample size.
While eFI measures are commonly utilized, such EMR-based FI are not routinely available in international settings.31,32 There is increasing interest in developing such frailty measures, but the mechanisms whereby EMR data are recorded vary among international institutions. The eFI developed in this study exhibited properties consistent with other FIs, such as the FI-CSHA, which is defined based upon 38 CSHA clinical evaluation items utilized in Comprehensive Geriatric Assessments.32–36 Many efforts to date have been made to improve awareness of frailty and associated patient well-being.37,38 A number of studies have detected associations between frailty, risk of death, and increased requirement for services.10,39–41 However, there are few validations for the Chinese population. Our study has filled this gap in a specific clinical setting, demonstrating the association between eFI-based frailty and the prognosis of lung cancer.
There are several limitations of this study. Firstly, there is an insufficiency of short-term outcome events, such as bone suppression and chemotherapy discontinuation, that lead to an underpowering of statistical inference and may result in false-negative errors. Secondly, in some patients, the difference between frail and non-frail may be the result of socioeconomic differences. However, this impact would be expected to underestimate the effect, producing a conservative result that would not alter the direction of the effect. Thirdly, although the eFI is well-established, it is still subject to measurement error which might affect the results.
Conclusion
In conclusion, the eFI-defined frail patients in the older Chinese population had worse lung cancer prognoses, including shortened overall survival and higher risk of mortality. Our findings indicate that the eFI-based frailty measure plays an important role in predicting lung cancer prognosis, and suggest further directions to uncover the relationship in other cancers.
Data Sharing Statement
The datasets generated during this current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The verbal informed consent was approved by the Ethics Review Committee of West China Hospital (No.2018-94), and that this study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
Qiukui Hao (QH) conceived the study and secured funding for this study. Yanjiao Shen (YS), Yuting Wang (YW), and Xiaoyan Chen (XC) conducted the electronic frailty index assessment and processed data. Yanjiao Shen (YS), Yuting Wang (YW) and Birong Dong (BD) presented the results and drafted the initial manuscript under the supervision of Qiukui Hao (QH). Yanjiao Shen (YS), Qingyang Shi (QS), and Lisha Hou (LH) performed the data analysis and verified the analysis outcomes and revised the manuscript. Qiukui Hao (QH), Qingyang Shi (QS), Lisha Hou (LH) and Birong Dong (BD) helped with results interpretation. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Project of Health and family planning commission of Sichuan Province (CGY2017-101) and the Project of Science and Technology Bureau of Sichuan Province (2020YFS0167). The sponsors did not participate in the design, methods, data collection, analysis, or preparation of this manuscript.
Disclosure
The authors declare that they have no competing interests.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
2. Chen G, Feng J, Zhou C, et al. Quality of life (QoL) analyses from OPTIMAL (CTONG-0802), a Phase III, randomised, open-label study of first-line erlotinib versus chemotherapy in patients with advanced EGFR mutation-positive non-small-cell lung cancer (NSCLC). Ann Oncol. 2013;24(6):1615–1622. doi:10.1093/annonc/mdt012
3. Franco I, Chen YH, Chipidza F, et al. Use of frailty to predict survival in elderly patients with early stage non-small-cell lung cancer treated with stereotactic body radiation therapy. J Geriatr Oncol. 2018;9(2):130–137. doi:10.1016/j.jgo.2017.09.002
4. Anderson LJ, Albrecht ED, Garcia JM. Update on management of cancer-related cachexia. Curr Oncol Rep. 2017;19(1):3. doi:10.1007/s11912-017-0562-0
5. Collins J, Noble S, Chester J, Coles B, Byrne A. The assessment and impact of sarcopenia in lung cancer: a systematic literature review. BMJ Open. 2014;4(1):e003697. doi:10.1136/bmjopen-2013-003697
6. Antonio M, Saldaña J, Linares J, et al. Geriatric assessment may help decision-making in elderly patients with inoperable, locally advanced non-small-cell lung cancer. Br J Cancer. 2018;118(5):639–647. doi:10.1038/bjc.2017.455
7. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi:10.1016/S0140-6736(12)62167-9
8. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727. doi:10.1093/gerona/62.7.722
9. Hajek A, Bock JO, Saum KU, et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47(2):233–241. doi:10.1093/ageing/afx157
10. Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45(3):353–360. doi:10.1093/ageing/afw039
11. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi:10.1093/gerona/56.3.M146
12. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–1492. doi:10.1111/j.1532-5415.2012.04054.x
13. Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553. doi:10.1136/bmj.d6553
14. Chowdhury R, Peel NM, Krosch M, Hubbard RE. Frailty and chronic kidney disease: a systematic review. Arch Gerontol Geriatr. 2017;68:135–142. doi:10.1016/j.archger.2016.10.007
15. Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–336. doi:10.1100/tsw.2001.58
16. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8(1):24. doi:10.1186/1471-2318-8-24
17. Kulminski AM, Ukraintseva SV, Kulminskaya IV, Arbeev KG, Land K, Yashin AI. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56(5):898–903. doi:10.1111/j.1532-5415.2008.01656.x
18. Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47(2):193–200. doi:10.1093/ageing/afx162
19. Blodgett JM, Theou O, Howlett SE, Wu FC, Rockwood K. A frailty index based on laboratory deficits in community-dwelling men predicted their risk of adverse health outcomes. Age Ageing. 2016;45(4):463–468. doi:10.1093/ageing/afw054
20. Wang Y, Zhang R, Shen Y, Su L, Dong B, Hao Q. Prediction of chemotherapy adverse reactions and mortality in older patients with primary lung cancer through frailty index based on routine laboratory data. Clin Interv Aging. 2019;14:1187–1197. doi:10.2147/CIA.S201873
21. Polidoro A, Dornbusch T, Vestri A, Di Bona S, Alessandri C. Frailty and disability in the elderly: a diagnostic dilemma. Arch Gerontol Geriatr. 2011;52(2):e75–e78. doi:10.1016/j.archger.2010.06.001
22. Rodriguez-Mañas L, Fried LP. Frailty in the clinical scenario. Lancet. 2015;385(9968):e7–e9. doi:10.1016/S0140-6736(14)61595-6
23. Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10. doi:10.1016/j.ejim.2016.03.007
24. Shen Y, Hao Q, Wang Y, et al. The association between preoperative modified frailty index and postoperative complications in Chinese elderly patients with hip fractures. BMC Geriatr. 2021;21(1):370. doi:10.1186/s12877-021-02330-7
25. Ju C, Zhou J, Lee S, et al. Derivation of an electronic frailty index for predicting short-term mortality in heart failure: a machine learning approach. ESC Heart Fail. 2021;8(4):2837–2845. doi:10.1002/ehf2.13358
26. Cohen HJ, Smith D, Sun CL, et al. Frailty as determined by a comprehensive geriatric assessment-derived deficit-accumulation index in older patients with cancer who receive chemotherapy. Cancer. 2016;122(24):3865–3872. doi:10.1002/cncr.30269
27. Royston P, Parmar MK. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med Res Methodol. 2013;13(1):152. doi:10.1186/1471-2288-13-152
28. Dehbi HM, Royston P, Hackshaw A. Life expectancy difference and life expectancy ratio: two measures of treatment effects in randomised trials with non-proportional hazards. BMJ. 2017;357:j2250. doi:10.1136/bmj.j2250
29. Udo EE, Al-Sweih N, John P, Chugh TD. Antibiotic resistance of enterococci isolated at a teaching hospital in Kuwait. Diagn Microbiol Infect Dis. 2002;43(3):233–238. doi:10.1016/S0732-8893(02)00397-8
30. Liu H, Liu B, Zheng F, Chen X, Ye L, He Y. Distribution of pathogenic bacteria in lower respiratory tract infection in lung cancer patients after chemotherapy and analysis of integron resistance genes in respiratory tract isolates of uninfected patients. J Thorac Dis. 2020;12(8):4216–4223. doi:10.21037/jtd-20-928
31. Brundle C, Heaven A, Brown L, et al. Convergent validity of the electronic frailty index. Age Ageing. 2019;48(1):152–156. doi:10.1093/ageing/afy162
32. Kernick D, Chew-Graham CA, O’Flynn N. Clinical assessment and management of multimorbidity: NICE guideline. Br J Gen Pract. 2017;67(658):235–236. doi:10.3399/bjgp17X690857
33. Howlett SE, Rockwood MR, Mitnitski A, Rockwood K. Standard laboratory tests to identify older adults at increased risk of death. BMC Med. 2014;12(1):171. doi:10.1186/s12916-014-0171-9
34. Krishnan M, Beck S, Havelock W, Eeles E, Hubbard RE, Johansen A. Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing. 2014;43(1):122–126. doi:10.1093/ageing/aft084
35. Rockwood K, Rockwood MR, Mitnitski A. Physiological redundancy in older adults in relation to the change with age in the slope of a frailty index. J Am Geriatr Soc. 2010;58(2):318–323. doi:10.1111/j.1532-5415.2009.02667.x
36. Rockwood MR, Howlett SE, Rockwood K. Orthostatic hypotension (OH) and mortality in relation to age, blood pressure and frailty. Arch Gerontol Geriatr. 2012;54(3):e255–260. doi:10.1016/j.archger.2011.12.009
37. Stow D, Matthews FE, Barclay S, et al. Evaluating frailty scores to predict mortality in older adults using data from population based electronic health records: case control study. Age Ageing. 2018;47(4):564–569. doi:10.1093/ageing/afy022
38. Moorhouse P, Mallery LH. Palliative and therapeutic harmonization: a model for appropriate decision-making in frail older adults. J Am Geriatr Soc. 2012;60(12):2326–2332. doi:10.1111/j.1532-5415.2012.04210.x
39. Rockwood K, Mitnitski A, Song X, Steen B, Skoog I. Long-term risks of death and institutionalization of elderly people in relation to deficit accumulation at age 70. J Am Geriatr Soc. 2006;54(6):975–979. doi:10.1111/j.1532-5415.2006.00738.x
40. Kahlon S, Pederson J, Majumdar SR, et al. Association between frailty and 30-day outcomes after discharge from hospital. CMAJ. 2015;187(11):799–804. doi:10.1503/cmaj.150100
41. Singh M, Stewart R, White H. Importance of frailty in patients with cardiovascular disease. Eur Heart J. 2014;35(26):1726–1731. doi:10.1093/eurheartj/ehu197
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
