Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Effects of Respiratory Training Combined with Limb Exercise on Pulmonary Function and Quality of Life in Patients with Bronchiectasis
Authors Ni R, Cai L, Xing Y, Fan X
Received 6 September 2022
Accepted for publication 12 December 2022
Published 22 February 2023 Volume 2023:16 Pages 475—482
DOI https://doi.org/10.2147/JMDH.S388944
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Rongping Ni,1,* Lizhang Cai,2,* Yingru Xing,3 Xiaoyun Fan1
1Department of Geriatric Respiratory and Critical Care, The First Affiliated Hospital of Anhui Medical University, Hefei, Anhui People’s Republic of China; 2Department of Respiratory, Shanghai Nanxiang Hospital, Shanghai, People’s Republic of China; 3Department of Clinical Laboratory, Huainan Oriental Hospital Group of Anhui University of Science and Technology, Huainan, Anhui People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyun Fan, Department of Geriatric Respiratory and Critical Care, The First Affiliated Hospital of Anhui Medical University, Jixi Road 218, Hefei, Anhui, 230022, People’s Republic of China, Tel +86 13956988552, Email [email protected]
Objective: To investigate the effects of respiratory rehabilitation training combined with limb rehabilitation on sputum clearance and quality of life in patients with bronchiectasis.
Methods: A retrospective analysis of 86 patients with bronchiectasis was divided into an intervention group and an observation group, with 43 cases in each group. All patients were above 18 years of age with no history of relevant drug allergies. Patients in the observation group were treated with conventional drugs, and those in the intervention group were given respiratory rehabilitation training and limb rehabilitation on this basis. After three months of treatment, the indexes of sputum discharge, sputum traits, lung function, and the 6-minute walk distance (6MWD) were compared and quality of life and survival skills were assessed using the Barthel index and a quality-of-life comprehensive assessment questionnaire (GQOLI-74).
Results: The percentage of patients with mild Barthel index in the intervention group was higher than that in the observation group, and the difference between the groups was statistically significant (P < 0.05). After treatment, the scores of life quality and the lung function in the intervention group were higher than those in the observation group (both P < 0.05). After three months of treatment, the sputum volume and sputum viscosity scores of the two groups were higher than those before treatment (P < 0.05).
Conclusion: Respiratory rehabilitation training with limb exercise rehabilitation can effectively improve the sputum clearance rate, lung function, and quality of life of patients with bronchiectasis and is thus worthy of clinical promotion and application.
Keywords: bronchiectasis, respiratory rehabilitation training, limb exercise rehabilitation, lung function, quality of life
Introduction
The destruction of muscle and elastic fibres in the bronchial wall can lead to abnormal and persistent bronchial dilatation, which, in turn, may give rise to the occurrence of tracheal dilatation. Tracheal dilatation occurs primarily as a result of acute and chronic airway infections and bronchial obstruction and can also occur in patients with genetic, immunological, or anatomical defects.1–3 Bronchiectasis and diseases such as chronic obstructive pulmonary disease promote one another, and bronchiectasis can simultaneously cause recurrent airway infections and increased sputum, thus aggravating airway obstruction.4–7 Based on incomplete statistics, the incidence of bronchiectasis in China is approximately 53–566/100,000 – a trend that is increasing annually.8 Effective sputum removal and anti-infective treatment, and maintenance of airway patency, have been routinely relied upon as important approaches for treating bronchiectasis.1
The effective clearance of airway secretions is an important part of the long-term treatment of patients with bronchiectasis. Although patients’ adverse symptoms can be temporarily relieved after treatment with anti-infective, bronchodilator, and expectorant drugs,9–11 their long-term motor function does not improve. In recent years, the treatment of chronic airway diseases such as bronchiectasis is no longer limited to simply the improvement of bronchial lesions and airflow limitations but has shifted to improving patients’ motor function and quality of life through a variety of rehabilitation exercises.12–14 Respiratory rehabilitation training is one of the most important rehabilitation exercises in bronchiectasis treatment. This treatment can improve patients’ lung function by helping them to change their existing breathing patterns, which primarily involves lip constriction breathing and breathing deeply from within the chest. A study by Liu et al15 found that the use of effective respiratory muscle training for patients with chronic obstructive pulmonary disease (COPD) could improve their lung function and increase their blood oxygen saturation and endurance. Limb exercise training can also significantly improve the muscle strength and endurance of all muscle groups, improve the exercise capacity and respiratory muscle strength of patients, prevent premature airway trapping, and relieve respiratory distress.
However, the clinical efficacy of respiratory training with limb exercise rehabilitation in the treatment of bronchiectasis is not yet clear. This study investigates the effect of respiratory rehabilitation training with limb exercise rehabilitation on sputum clearance and quality of life in patients with bronchiectasis.
Materials and Methods
Study Subjects
The research group retrospectively investigated the electronic medical records of 86 patients with bronchiectasis and accompanying infections who were admitted to our hospital from March 2017 to June 2020, then randomly divided them into an observation group and an intervention group, with 43 cases in each group. The observation group was treated with conventional drugs, and the intervention group was given respiratory rehabilitation and limb exercise rehabilitation based on the observation group. The study was conducted following the Declaration of Helsinki of the World Medical Association and was approved by the hospital’s ethics committee. All patients signed an informed consent form for inclusion in the study.
Inclusion and Exclusion Criteria
The inclusion criteria of the current study were as follows: (1) patients had to meet the diagnostic criteria of the Expert Consensus on the Diagnosis and Treatment of Adult Bronchiectasis;6 (2) they had to be able to complete follow-up and had to have good treatment compliance; (3) they had to have no history of relevant drug allergies; (4) they needed to be above 18 years of age; (5) they had to have signed the informed consent form.
Exclusion criteria: (1) combined asthma, tuberculosis, and lung tumour conditions; (2) major organ conditions such as heart, liver, and kidney diseases; (3) mental disorders, neurological diseases, etc., that may render patients unable to cooperate with exercise training; (4) incomplete patient information.
Randomization and Blinding
Eligible patients were randomly assigned in a 1:1 ratio to each group using permuted, block-randomization to balance the number of patients allocated to each group. The permuted block randomization sequence was generated, using Package “randomize R” in R software version 3.6.1 and placed in individual sealed and opaque envelopes by the statistician. The investigator enrolled the patients and only then open envelopes to assign patients to the different groups. This method of allocation concealment could result in minimum selection and confounding biases.16
Sample Size Calculations
In this study, we conducted sample size calculations based on detecting minimum clinically relevant differences (MCRDs) from expert opinion and previous research findings. Sample size calculations were based on detecting MRCDs with 80% power and a significance level of 5% and on the premise of using a two-sample paired means test. All sample size calculations were conducted in STATA V.17 From the calculations, this study required the smallest sample size of 32 participants. Allowing for drop outs, we aimed to recruit 43 participants for each group.
Six-Minute-Walk Distance (6MWD) Test
6MWT was performed in a flat, straight, surface rigid corridor inside the chamber. Before each 6MWT, patients were required to have a resting oxygen saturation of at least 83% as measured by pulse oximetry after 10 minutes of rest breathing room air or after breathing at the baseline O2 flow rate. The patient was instructed to walk as far as possible and not jogging or running; If they needed to decelerate or stop to rest, they were allowed to do so and were encouraged to resume walking as soon as possible. Testing was stopped if the patient experienced chest pain, intolerable dyspnea, leg cramps, sweating, or saturation below 83%.18
Treatment Methods
Both groups were given anti-infection and expectorant treatment to improve the symptoms of acute infection. The following drugs were routinely administered. A terbutaline sulfate solution for nebulisation (AstraZeneca, imported drug registration No. H20030642, 2 mL: 5 mg/tube) – one dose dissolved in 10 mL of 0.9% saline for nebulised inhalation three times daily. An ambroxol hydrochloride oral solution (Jiangsu Hengrui Pharmaceutical Co., Ltd., pharmaceutical product registration no. HC20040026; 100 mL, 0.3 g) – 10 mg, twice daily. Glucocorticoid drugs were added when necessary.
Based on these medications, the intervention group was given respiratory rehabilitation training and extremity exercise rehabilitation treatment. Respiratory training included deep breathing with chest expansion and lip contraction while walking or climbing stairs (among other things), which was performed under standardised demonstration conditions. The walking speed was controlled at 60–80 steps per minute for 15 minutes each time, and slow breathing with the mouth and lips was carried out once for every two steps when climbing stairs. This was conducted on the premise that each exercise should be tolerated by the individual, and attention should be paid to monitoring vital signs. Limb exercise training included endurance and strength training. The formerly employed cycle ergometer training (CPX/MAX/D, McGuffey, USA) for 20 minutes each time; the latter tested the single repetition maximum (one repetition maximum: 1RM) before training, and the training intensity was controlled at 70%–85% of 1RM. Eight repetitions for each muscle group action were completed in four sets. The training was conducted three times a week, with each session lasting 40 minutes. Both groups were treated for three months.
Primary Observation Indexes
Researchers were blinded to patient grouping and evaluated patients before and after implementation of the intervention protocol. The main observation indexes included the patients’ sputum volume, sputum properties, lung function-related indexes, and Barthel19 and GQOLI-7420 scores.
Patients rinsed twice with water and twice with hydrogen peroxide 10 min before induction of expectoration, according to the method of Pinto Plata et al.21 After clearing nasal mucus, the patient was deeply coughed for sputum removal. Sputum volume for collection was required to be no less than 1 mL and to contain no saliva. A pipette was used to determine sputum volume. A dynamic rheological assessment of each collected sputum was performed using a rheometer (ar1500ex, Ta instruments, New Castle, Delaware). Interfacial tension was measured at the air–mucus interface by a strain gauge connected to the ring (Tensiomat Model 21, Fisher Scientific, Pittsburgh, Pennsylvania) to assess sputum viscosity.22
In this study, the Barthel index was used to evaluate the patients’ daily living abilities after treatment. The index includes 10 items with a total score out of 100. A score ≥60 was considered “mild”, 59–41 was considered “moderate”, and ≤40 was considered “severe”. The post-intervention quality of life survey was conducted using the GQOLI-74 scale, which included four dimensions: physical life status, physical function, social function, and psychological function. All dimensions included five items, except for the first dimension, which included four. Five levels of scoring were applied to individual items, and these scores positively correlated with the effects. A pulmonary function tester was used to test the lung function indexes, eg the force expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC. The amount of deep pulmonary sputum effectively coughed up by patients within 24 hours was recorded, and the sputum viscosity was assessed with reference to the relevant literature.7
Statistical Analysis
The SPSS Statistics (v.20.0) software package was used for data processing in this study. The measurement data were expressed as mean ± standard deviation ( ). Count data were expressed as percentages (%). Normality tests were performed using the W-test. The W-test was used to compare the normal distribution data between the two groups; the non-parametric test was used for comparison between the groups regarding data that did not obey normal distribution patterning. A chi-square test was used for counting data; P < 0.05 was considered a statistically significant difference.
). Count data were expressed as percentages (%). Normality tests were performed using the W-test. The W-test was used to compare the normal distribution data between the two groups; the non-parametric test was used for comparison between the groups regarding data that did not obey normal distribution patterning. A chi-square test was used for counting data; P < 0.05 was considered a statistically significant difference.
Results
General Information
Between March 2017 and June 2020, 86 patients with bronchiectasis were identified and enrolled in the study, and they were randomly divided into observation and intervention groups (n = 23 for each group). There was 23 male and 20 female in Intervention group compared with 22 male and 21 female in Observation group. The Age of intervention group and observation group was 65.51±5.54 vs 65.70±5.55 years, the disease duration was 5.65±0.45 vs 5.75±0.39 years, and the Barthel Index was 35.41±3.20 vs 35.43±3.21. There was no statistically significant difference between the two groups in terms of gender, age, disease duration, and Barthel Index scores on admission (P > 0.05) (Table 1).
 |
Table 1 Comparison of General Data Between the Two Groups |
Comparison of Barthel Scores Between the Two Groups
The results of this study indicated a mild Barthel score for 90.70% (39/43) of patients in the intervention group; in the observation group, this value was 72.09% (31/43). Accordingly, the percentage of patients with a Barthel score below mild was significantly higher in the intervention group than in the observation group, with statistically significant differences (P < 0.05).
Comparison of the Quality-of-Life Scores in the Two Groups Before and After Treatment
The results showed that before treatment, there were no differences between the two groups in physical life status score, physical function score, social function score, and psychological function score (P > 0.05). The post-treatment physical life status score, physical function score, social function score, and psychological function score of the patients in the intervention group were significantly higher than those in the observation group, and the differences were statistically significant (P < 0.001). Intervention group and observation group, the post-treatment physical life status score, physical function score, social function score, and psychological function score of the patients were significantly higher than before treatment (P < 0.001) (Table 2).
 |
Table 2 Comparison of Quality of Life Scores Between the Two Groups (Points) |
Comparison of Pulmonary Function Indexes Between the Two Groups Before and After Treatment
The results showed that before treatment, there were no differences between the two groups in FEV1, FVC, and FEV1/FVC (P > 0.05). After treatment, FEV1, FVC, and FEV1/FVC in the intervention group were significantly higher than those in the observation group, and all differences were statistically significant (P < 0.001). Intervention group and observation group the post-treatment FEV1, FVC, and FEV1/FVC were significantly higher than before treatment (P < 0.001) (Table 3).
 |
Table 3 Comparison of Pulmonary Function Indexes Between the Two Groups |
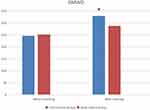
Figure 1 presented changes in 6MWD at baseline and after treatment for the intervention and observation groups. The results showed no significant differences in 6MWD experimental outcomes between the intervention and observation groups before treatment. While after receiving the respiratory rehabilitation training and extremity exercise rehabilitation treatment, patients in the intervention group showed a significant increase in the distance traveled, in contrast to the observation group (P < 0.05).
Comparison of Sputum Excretion Between the Two Groups Before and After Treatment
The results of this study showed that there was no statistical difference between the two groups in terms of sputum volume (mL/d) and sputum viscosity (score). After treatment, the sputum volume and sputum viscosity scores of patients in the intervention group after three months of treatment were higher than in the observation group, and the differences were statistically significant (P < 0.001). Intervention group and observation group the post-treatment sputum volume and sputum viscosity scores of patients were significantly higher than before treatment (P < 0.001) (Table 4).
 |
Table 4 Comparison of Sputum Excretion Between the Two Groups Before and After Treatment |
Discussion
In this study, respiratory rehabilitation training combined with exercise training was used for patients with bronchiectasis. The results indicated that the lung-function score of the intervention group was significantly higher than that of the observation group, suggesting enhanced improvement. Furthermore, FEV1, FVC, FEV1/FVC, and 6WMD were all increased to different degrees. The current study results suggest that patients in the intervention group significantly improved their self-care ability and quality of life after respiratory and limb exercise training. In this study, the duration of treatment was increased to three months, and Barthel scores were more significantly increased, indicating that the patients’ self-living ability had been significantly improved.
Respiratory Rehabilitation Training and Limb Exercise Training Can Improve the Limb Training Efficiency and Promote the Recovery of Respiratory Function
Results from evidence-based medical research published in recent years have shown that pulmonary rehabilitation (PR) can significantly improve exercise capacity and health-related quality of life in patients with bronchiectasis, adding to the growing evidence to support the routine provision of PR to patients with bronchiectasis and exertional dyspnoea.23,24 Previous study also suggested that respiratory muscle stretching associated with aerobic training could reduce respiratory muscle activity during exercise and improves lung volumes and capacities in patients with moderate-to-severe COPD.25 Similarly, we also observed that respiratory rehabilitation training and limb rehabilitation significantly improved the scores of patients’ quality of life indicators.
The Mechanism of Lung Function Improvement
Respiratory muscle training promotes the growth of diaphragm type I muscle fibres by imposing a reasonable respiratory load. In this way, the patient’s respiratory muscle endurance and fatigue resistance is improved, and ultimately, the strength of the patient’s main inspiratory muscle and auxiliary inspiratory muscle is also enhanced, while the sympathetic tone is strengthened and vagal tone reduced through respiratory feedback training, thus promoting the autonomic function regulation of breathing and ultimately improving the patient’s lung function-related indexes. Many patients with bronchiectasis have sputum accumulation, which affects respiratory function. Effective respiratory and exercise training can enhance the clearance efficiency of respiratory muscles and liquefy and loosen airway secretions, thus making them easier to cough up. This study found that the sputum clearance rate and 24-hour clearance in the intervention group were significantly higher than those in the observation group. However, these indications are reliant on effective anti-infection treatment.26
Limitations
Our data have several common limitations relevant to most prospective analyses. First, because of the study’s retrospective nature, treatment options were not randomised. Second, the specific protocols of respiratory training and limb exercise training, particularly the frequency and time, remain open for discussion. However, regardless of the training programme, subjective feelings of fatigue, activity ability, and the clinical manifestations of patients should be considered important reference indexes.
Conclusions
Respiratory rehabilitation training with limb exercise rehabilitation can effectively increase the sputum clearance rate, improve lung function, and enhance the survival quality in patients with bronchiectasis, and it exhibits broad clinical application prospects.
Research and Publication Ethics
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Huainan Eastern Hospital Group and Nanxiang Hospital of the Jiading District, Shanghai. All patients signed an informed consent form for inclusion in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. Xiaoyun Fan designed the study. Rongping Ni was responsible for collecting all the epidemiological and clinical data, writing the paper. Yingru Xing made the illustrations and Weiwei Ren helped analyze the data. All authors took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers U1803126).
Disclosure
All of the authors had no any personal, financial, commercial or academic conflicts of interest separately for this work.
References
1. Polverino E, Goeminne PC, McDonnell MJ, et al. European respiratory society guidelines for the management of adult bronchiectasis. Eur Respir J. 2017;50:1700629. doi:10.1183/13993003.00629-2017
2. Chan CH, Ho AK, Chan RC, Cheung H, Cheng AF. Mycobacteria as a cause of infective exacerbation in bronchiectasis. Postgrad Med J. 1992;68:896–899. doi:10.1136/pgmj.68.805.896
3. Ekanayake A, Madegedara D, Chandrasekharan V, Magana-Arachchi D. Respiratory bacterial microbiota and individual bacterial variability in lung cancer and bronchiectasis patients. Indian J Microbiol. 2020;60:196–205. doi:10.1007/s12088-019-00850-w
4. Tiew PY, Lim AYH, Keir HR, et al. High frequency of allergic bronchopulmonary aspergillosis in bronchiectasis-COPD overlap. Chest. 2021;S0012–3692(21):3620. doi:10.1016/j.chest.2021.07.2165
5. Tiew PY, Jaggi TK, Chan LLY, Chotirmall SH. The airway microbiome in COPD, bronchiectasis and bronchiectasis-COPD overlap. Clin Respir J. 2021;15:123–133. doi:10.1111/crj.13294
6. Nowiński A, Korzybski D, Bednarek M, Goljan-Geremek A, Puścińska E, Śliwiński P. Does bronchiectasis affect COPD comorbidities? Adv Respir Med. 2019;87:214–220. doi:10.5603/ARM.2019.0059
7. Jin M, Yu WL, Li SL, Lu LJ, Liu XF, Sun YC. Factors associated with bronchiectasis in patients with moderate-severe chronic obstructive pulmonary disease. Medicine. 2016;95:e4219. doi:10.1097/MD.0000000000004219
8. Quint JK, Millett ERC, Joshi M, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study. Eur Respir J. 2016;47:186–193. doi:10.1183/13993003.01033-2015
9. Sidhu MK, Mandal P, Hill AT. Developing drug therapies in bronchiectasis. Expert Opin Investig Drugs. 2015;24:169–181. doi:10.1517/13543784.2015.971153
10. Tsang KW, Bilton D. Clinical challenges in managing bronchiectasis. Respirology. 2009;14:637–650. doi:10.1111/j.1440-1843.2009.01569.x
11. Gillham MI, Sundaram S, Laughton CR, Haworth CS, Bilton D, Foweraker JE. Variable antibiotic susceptibility in populations of Pseudomonas aeruginosa infecting patients with bronchiectasis. J Antimicrob Chemother. 2009;63:728–732. doi:10.1093/jac/dkp007
12. Liaw MY, Wang YH, Tsai YC, et al. Inspiratory muscle training in bronchiectasis patients: a prospective randomized controlled study. Clin Rehabil. 2011;25:524–536. doi:10.1177/0269215510391682
13. Goldstein RS. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax. 2005;60:889–890. doi:10.1136/thx.2005.043810
14. O’Neill K, O’Donnell AE, Bradley JM. Airway clearance, mucoactive therapies and pulmonary rehabilitation in bronchiectasis. Respirology. 2019;24:227–237. doi:10.1111/resp.13459
15. Liu ZX, Peng L. Impact of lung function and exercise endurance in chronic obstructive pulmonary disease patients treated with respiratory rehabilitation training. Modern Med J. 2014;42:615–618. doi:10.3969/j.issn.1671-7562.2014.06.006
16. Irvani SSN, Golmohammadi M, Pourhoseingholi MA, Shokouhi S, Darazam IA. Effectiveness of Interferon Beta 1a, compared to Interferon Beta 1b and the usual therapeutic regimen to treat adults with moderate to severe COVID-19: structured summary of a study protocol for a randomized controlled trial. Trials. 2020;21(1):473. doi:10.1186/s13063-020-04382-3
17. Stanford G, Davies JC, Usmani O, et al. Investigating outcome measures for assessing airway clearance techniques in adults with cystic fibrosis: protocol of a single-centre randomised controlled crossover trial. BMJ Open Respir Res. 2020;7(1):e000694. doi:10.1136/bmjresp-2020-000694
18. du Bois RM, Albera C, Bradford WZ, et al. 6-Minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2014;43(5):1421–1429. doi:10.1183/09031936.00131813
19. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65.
20. Liu J, Lin CS, Gan WQ, et al. Effect of healthcare insurance policy on the quality of life of chronic hepatitis C patients receiving interferon α-2a plus ribavirin therapy. Exp Ther Med. 2012;3:1062–1066. doi:10.3892/etm.2012.519
21. Lv Y, Guo S, Li XG, Chi JY, Qu YQ, Zhong HL. Sputum and serum microRNA-144 levels in patients with tuberculosis before and after treatment. Int J Infect Dis. 2016;43:68–73. doi:10.1016/j.ijid.2015.12.014
22. Daviskas E, Anderson DS, Jaques A, Charlton B. Inhaled mannitol improves the hydration and surface properties of sputum in patients with cystic fibrosis. Chest. 2010;137(4):861–868. doi:10.1378/chest.09-2017
23. Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest. 2007;131:4S–42S. doi:10.1378/chest.06-2418
24. Patel S, Cole AD, Nolan CM, et al. Pulmonary rehabilitation in bronchiectasis: a propensity-matched study. Eur Respir J. 2019;53:1801264. doi:10.1183/13993003.01264-2018
25. Wada TJ, Borges-Santos E, Porras CD, et al. Effects of aerobic training combined with respiratory muscle stretching on the functional exercise capacity and thoracoabdominal kinematics in patients with COPD: a randomized and controlled trial. Int J Chron Obstruct Pulmon Dis. 2016;11:2691–2700. doi:10.2147/COPD.S114548
26. Elkins M, Dentice R. Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: a systematic review. J Physiother. 2015;61:125–134. doi:10.1016/j.jphys.2015.05.016
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.