Back to Journals » International Journal of General Medicine » Volume 17
The Effects of Budesonide Inhalation Treatment on the Expression Levels of Serum IL-6, TGF-β1, and IgE and Pulmonary Function in Patients with Cough Variant Asthma and an Evaluation of Treatment Efficacy
Authors Niu Y, Cao M, Li S, Mo J, Zhu Z, Wang H
Received 20 December 2023
Accepted for publication 26 March 2024
Published 29 March 2024 Volume 2024:17 Pages 1253—1261
DOI https://doi.org/10.2147/IJGM.S455872
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Woon-Man Kung
Yueying Niu,1 Mengqing Cao,1 Shumin Li,1 Juanfen Mo,2 Ziyi Zhu,1 Haiqin Wang1
1Department of Respiratory Medicine, The Second Hospital of Jiaxing, Jiaxing, Zhejiang, People’s Republic of China; 2The Key Laboratory, The Second Hospital of Jiaxing, Jiaxing, Zhejiang, People’s Republic of China
Correspondence: Haiqin Wang; Ziyi Zhu, Department of Respiratory Medicine, The Second Hospital of Jiaxing, 1518 Huanchen North Road, Jiaxing, Zhejiang, 314000, People’s Republic of China, Email [email protected]; [email protected]
Objective: To retrospectively study the effects of budesonide inhalation combined with conventional symptomatic treatment on serum inflammatory factor expression levels and pulmonary function in patients with cough variant asthma (CVA) and to evaluate treatment efficacy.
Methods: This retrospective cohort study included 200 patients diagnosed with CVA at the Second Hospital of Jiaxing between January 2022 and June 2023 and given conventional symptomatic treatment plus budesonide inhalation were included in this study. Patients were divided into a no remission group, a partial remission group and a complete remission group based on treatment effect. The expression levels of serum inflammatory factors, cough symptom scores, and small airway function indicators in the three groups of patients at different time points were compared.
Results: In the three groups of CVA patients, after receiving budesonide inhalation combined with conventional symptomatic treatment, the expression levels of serum IL-5, IL-6, IL-8, TNF-α, TGF-β 1, and IgE and number of eosinophils significantly decreased (P < 0.05). There were statistically significant differences in the IL-6 and TGF-β 1 levels among the three groups of CVA patients at T1, T2 and T3. There were statistically significant differences in IgE levels, number of eosinophils, cough symptom scores, and small airway function indicators between T2 and T3 (P< 0.05). The receiver operating characteristic (ROC) curve prediction analysis revealed significant differences in the expression of IL-6 and TGF-β 1 at T1, T2, and T3.
Conclusion: Budesonide inhalation combined with conventional symptomatic treatment can significantly reduce the levels of serum inflammatory factors in patients with CVA to reduce inflammation and the allergic response, thereby reducing the cough symptom score, improving pulmonary function, and improving therapeutic efficacy. In addition, IL-6 and TGF-β 1 can be used as early predictors of budesonide inhalation efficacy.
Keywords: budesonide, cough variant asthma, cytokines, IL-6, TGF-β 1
Introduction
Cough variant asthma (CVA) is a type of asthma whose main clinical manifestation is chronic cough accompanied by airway hyperresponsiveness, with no obvious symptoms or signs of wheezing and shortness of breath,1 and it is more obvious at night or in the early morning. In recent years, due to environmental changes, the overuse of antibiotics and other factors, the incidence of CVA has increased annually.2,3 The pathogenesis of CVA has still not been fully elucidated. Scholars in China and abroad have proposed that CVA has certain similarities to typical bronchial asthma; that is, chronic inflammatory changes in the airway are predominantly caused by eosinophilic infiltration, with the participation of a variety of inflammatory cells and mediators, and airway hyperresponsiveness.4,5 Moreover, eosinophils can produce leukotriene mediators, thus causing inflammation.6 Moreover, simple and effective monitoring and evaluation measures for the treatment response and prognosis of patients with CVA are lacking. If CVA cannot be effectively controlled in a timely manner, it may develop into typical asthma.
At present, the “Guidelines for the Diagnosis and Treatment of Cough” in China recommend glucocorticoids combined with conventional treatment for CVA, and the clinical benefits have been significant. Due to the differences between individual patients and variations in conditions, the treatment response of patients still needs to be evaluated in a timely manner during clinical treatment to rationally adjust regimens.7 Routine treatments for CVA include bronchodilators, glucocorticoids, antiallergic drugs, and leukotriene receptor antagonists.8,9 Budesonide is a glucocorticoid, and its unique molecular structure leads to long-acting, highly effective, and local anti-inflammatory effects.10 It has a clear first-pass effect and can reduce inflammatory damage, control airway sensitivity, improve pulmonary function, and reduce the symptoms of asthma; therefore, it is often used in nebulized inhalation.11 The commonly used clinical methods for evaluating the efficacy of CVA include pulmonary function tests, symptom scores, and quality of life assessments. Among them, the pulmonary function test is one of the most commonly used evaluation methods and can evaluate a patient’s pulmonary function status by measuring the peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1).12 When evaluating the efficacy of CVA treatment, a variety of factors should be comprehensively considered, including patient age, patient sex, disease course, disease severity, and comorbidities. Moreover, appropriate evaluation methods and indicators need to be selected based on the specific conditions of each patient to more accurately evaluate the treatment effect. However, there are few studies on the effects of interleukin-5 (IL-5), interleukin-6 (IL-6), interleukin-8 (IL-8), tumour necrosis factor α (TNF-α), transforming growth factor-β1 (TGF-β1), and other expression levels on the progression and efficacy of CVA patients receiving budesonide inhalation therapy. Therefore, it exists large research space on the relationship between the changes of inflammatory cytokines, TGF-β1, IgE and other expression levels in peripheral blood of CVA patients receiving budesonide inhalation therapy at different treatment time points and the changes of cough symptom scores and small airway function indexes.
IL-5, IL-6, IL-8, TNF-α, TGF-β1 and IgE, which are associated with the treatment response and prognosis of patients with CVA, were analysed in this study. The abovementioned inflammatory factors were measured in the peripheral blood of CVA patients receiving budesonide inhalation treatment. The expression levels of cytokines and inflammatory mediators were compared at different treatment time points, and the differences in expression levels were compared to investigate the duration of action of inhaled budesonide in the treatment of CVA. Moreover, a prediction model of CVA molecular markers combined with pulmonary function was constructed based on changes in the cough symptom score and small airway function indicators of patients to improve the ability to predict CVA occurrence, CVA development, the clinical efficacy of CVA treatment and the prognosis of CVA patients.
Subjects and Methods
Subjects
This study complied with the relevant principles of the Declaration of Helsinki; the rights and interests of the subjects were fully protected, the rights of the research subjects to make independent decisions were protected, and the personal information of the research subjects was kept confidential. A total of 200 CVA patients admitted to the Department of Respiratory Medicine of the Second Hospital of Jiaxing between January 2022 and June 2023 were included. The causes of chronic cough were diagnosed via a validated management algorithm according to the Chinese national guidelines on the diagnosis and management of cough.13 To observe the therapeutic effect of 200 CVA patients, they were divided into a no remission group (16 patients), a partial remission group (72 patients), and a complete remission group (112 patients).
Inclusion criteria: cough duration of more than 8 weeks, and bronchial provocation test positive; antibiotics and antitussives were ineffective, and bronchospasmodic or corticosteroids were effective. Complete clinical data; voluntary participation in this study.
The exclusion criteria were as follows: (1) liver and kidney functional impairment; (2) drug allergies; (3) chronic cough similar to CVA; (4) recent use of bronchodilators; and (5) failure to take medication during the treatment course.
The treatment efficacy criteria were as follows: complete remission: disappearance of cough symptoms within 3 months of treatment; partial remission: significant reduction in cough symptoms, with varying degrees of prolongation of the coughing interval or a reduction in the number of coughs; and no remission: no relief of cough symptoms.
Methods
Medication
All patients had received budesonide inhalation combined with conventional treatment (eg, treatment for cough, phlegm, or infection). The dose of inhaled budesonide (AstraZeneca Pharmaceutical Co., Ltd., SFDA approval number H20140517) was 400 μg/application, 2 times/d. After the improvement of cough symptoms, it was reduced to 200 μg/time, 2 times/d. The discontinuation criteria were as follows: resolution of symptoms.
Test methods
All CVA patients underwent pulmonary function tests and whole blood and serum collection before treatment (T0) and after 2 weeks (T1), 4 weeks (T2), and 8 weeks (T3) of treatment. A whole-blood test was performed. Five millilitres of peripheral venous blood was collected. The blood was allowed to naturally coagulate at room temperature for 10–20 min. The blood was subsequently centrifuged for 20 min (2500 r/min; centrifugation radius: 15 cm). The supernatant was collected and placed in another clean EP tube. A portion of the serum was used to measure the IgE concentration via an enzyme-linked immunofluorescence assay (ELISA), and another portion was cryopreserved at −20 °C until ELISAs.
ELISA Measurement of Serum Inflammatory Indicators
IL-5, IL-6, IL-8, TNF-α, and TGF-β1 levels were measured using ELISA kits (Proteintech, China). For the ELISAs, standards were diluted, and samples were added to wells and incubated; the wells were washed, after which enzymes were added. After washing, colour development reagents were added. The absorbance (OD) value of each well was measured sequentially at a wavelength of 450 nm. The measurement was performed within 15 min after the addition of stop solution. The corresponding concentration from a standard curve was multiplied by the dilution factor to calculate the concentrations of IL-5, IL-6, IL-8, TNF-α, and TGF-β1 in the samples.
Cough Symptom Score
The cough symptom scores, including the daytime symptom score and nocturnal symptom score, were recorded for the two groups before and after treatment.14,15 The daytime symptom score was 0 for patients who were asymptomatic during the day, 1 for patients with occasional coughing during the day, 2 for patients with intermittent single coughing during the day, and 3 for patients with intermittent coughing during the day. The nocturnal symptom score was 0 points if the patient did not have any symptoms at night, 1 point if the patient woke up once due to coughing at night, 2 points if the patient woke up twice due to coughing at night, and 3 points in the patient woke up more than 3 times due to coughing at night.
Pulmonary Function Test
The conventional pulmonary ventilation function of patients was evaluated using the MasterScreen pulmonary function detection system (Jaeger, Germany). Pulmonary function indicators were recorded, including the percentage of forced expiratory volume at the end of the first second (FEV1% pred), forced vital capacity (FVC), and peak expiratory flow (PEF).
Statistical Analysis
GraphPad Prism 7.0 software was used for the statistical analysis. All quantitative data are expressed as ±s. Comparisons among multiple groups were performed using one-way analysis of variance (ANOVA), and count data were compared using the χ2 test. Receiver operating characteristic (ROC) curves were plotted, and the area under the curve (AUC) was calculated. P < 0.05 was considered statistically significant.
Results
Comparison of the Basic Information of the CVA Patients in the Three Groups
A retrospective study of 200 CVA patients who received budesonide combined with conventional treatment was performed; 114 males and 86 females were included. The oldest patient was 87 years of age, and the youngest was 29 years of age. CVA patients treated with budesonide were divided into a no remission group, a partial remission group and a complete remission group based on remission rate. Among them, there were 112 patients in the complete remission group, with a clinical complete remission rate of 56%; 72 patients in the partial remission group, with a clinical partial remission rate of 36%; and 16 patients in the no remission group, with a clinical no remission rate of 8%. Age, sex, smoking history, history of allergic rhinitis, and duration of disease were not significantly different among the three groups (Table 1).
 |
Table 1 Comparison of Baseline Data with Three CVA Groups |
3.2 Effect of budesonide treatment on the expression of inflammatory cytokines in the serum of CVA patients at different time points
To understand the changes in inflammatory cytokines in the serum of CVA patients treated with budesonide for different durations, ELISAs were used to measure the levels of IL-5, IL-6, IL-8, TNF-α and TGF-β1 in the serum of CVA patients at the four time points (T0, T1, T2, and T3). The results showed that all serum inflammatory factor levels gradually decreased with CVA treatment. Among them, compared with those in the no remission group and the partial remission group, the expression levels of IL-6 and TGF-β1 in the remission group were significantly lower at the T1, T2, and T3 time points (P <0.05). There was a statistically significant difference in the serum IL-8 concentration among the CVA patients in the three groups at T3 (P <0.05), with the lowest level occurring in the remission group. Although the expression levels of serum IL-5 and TNF-α also decreased with CVA treatment, there were no significant differences among the three groups of CVA patients at different time points (P>0.05). Therefore, we propose that although these inflammatory cytokines are involved in the development of airway inflammation in CVA patients, IL-6 and TGF-β1 levels are directly correlated with the efficacy of budesonide treatment (Table 2).
 |
Table 2 Serum Cytokine Indicators with Three CVA Groups |
3.3 Effect of budesonide treatment on the serum IgE concentration and number of eosinophils in the blood of patients with CVA
The effects of budesonide treatment on the levels of IgE in the serum and eosinophils in the blood of CVA patients were assessed at different time points. The results showed that both the serum IgE concentration and the absolute number of eosinophils gradually decreased with CVA treatment. Between time points T2 and T3, there were statistically significant differences in the serum IgE concentration and absolute number of eosinophils among the three groups of CVA patients (P < 0.05), and the expression level in the remission group was significantly lower than that in the no remission group and the partial remission group. There were no significant differences in the serum IgE levels or the absolute number of eosinophils in the three groups of CVA patients at the T1 and T2 time points (P >0.05) (Table 3).
 |
Table 3 IgE and Eosinophil Indicators with Three CVA Groups |
Effect of Budesonide Treatment on the Pulmonary Function of Patients with CVA
To further understand the effect of budesonide on the pulmonary function of CVA patients at different time points, we evaluated the cough symptom score and the FEV1, FVC and PEF values. The results showed that the cough symptom score and all the indicators of pulmonary function improved after budesonide treatment. Among them, the cough symptom score as well as the values for FEV1, FVC, and PEF, which are indicators of pulmonary function, were significantly different among the three groups of CVA patients at T2 and T3 (P < 0.05) (Table 4).
 |
Table 4 Cough Symptom Score and Small Airway Function Index with Three CVA Groups |
Evaluation Value of Different Indicators for CVA Patients Receiving Budesonide Treatment
ROC curves were generated to analyse whether different indicators at different time points were significantly related to remission in patients treated with budesonide. The results showed that at the T1 period, the AUC for IL-6 was 0.65 (95% CI was 0.48–0.80, the sensitivity was 35.67%, and the specificity was 95.33%); at the T2 period, the AUC for IL-6 was 0.69 (95% CI was 0.53–0.80, the sensitivity was 38.50%, and the specificity was 91.25%); and at the T3 period, the AUC for IL-6 was 0.72 (95% CI was 0.50.5–0.85, the sensitivity was 89.67%, and the specificity was 45.33%), P <0.05. At the T1 period, the AUC for TGF-β1 was 0.69 (95% CI was 0.40–0.69, the sensitivity was 40.50%, and the specificity was 75.50%); at the T2 period, the AUC for TGF-β1 was 0.71 (95% CI was 0.42–0.75, the sensitivity was 85.67%, and the specificity was 54.33%); and at the T3 period, the AUC value for TGF-β1 was 0.74 (95% CI was 0.539–0.825, the sensitivity was 96.33%, the specificity was 51.50%), P <0.05. At the T3 period, the AUC for the cough symptom score was 0.67 (95% CI=0.48–0.76, sensitivity=96.50%, specificity=37.50%), P<0.05. There was no significant difference in the remaining variables (P >0.05) (Table 5).
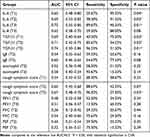 |
Table 5 The ROC Curve Analysis of Complete Relief Group |
Discussion
CVA is a special type of asthma and a common respiratory disease. Timely and effective treatment and treatment efficacy evaluations are important for treating this disease. In this study, we retrospectively analysed the remission of CVA patients after budesonide treatment. After treatment, clinical symptoms, serum inflammatory cytokines, and pulmonary function recovery improved significantly. Studies have shown that budesonide is effective at controlling the symptoms of CVA, has few systemic adverse reactions, and has strong local anti-inflammatory effects; moreover, it has been widely used in clinical practice to treat bronchial asthma.16 After budesonide is inhaled into the lungs, it specifically binds to glucocorticoid receptors expressed in the cytoplasm of target cells to affect the transcription of various inflammatory factors, thereby exerting its anti-inflammatory effect.17
In retrospective studies, after budesonide treatment, the relevant inflammatory indicators significantly normalized, with improvements in the remission group being more significant than those in the control group at different time points. These findings indicate that inflammatory cytokines are involved in the CVA progression and are consistent with the findings of published reports in China and abroad.18,19 IL-6 is a proinflammatory cytokine secreted by TH2 cells that can induce the differentiation of B lymphocytes and the proliferation of T helper cells and is involved in chronic airway inflammation and airway remodelling.20 TGF-β1 is secreted mainly by eosinophils and plays dual roles in the pathogenesis of CVA; an increase in TGF-β1 can cause a weakened inflammatory response and enhanced airway reconstruction.21 However, if the airway is subjected to repeated antigen stimulation, chronic inflammation can occur, possibly leading to a persistent and excessive increase in TGF-β1 levels, which can cause tissue fibrosis, airway reconstruction and chronic airway obstruction.22 Therefore, serum IL-6 and TGF-β1 can be used as valuable blood indicators for evaluating the efficacy of CVA treatment. However, these indicators are related to Th2 cell immunity, which has certain limitations for the disease research of CVA patients, but also for some lymphocyte immunity research as a reference.
CVA patients often have different degrees of pulmonary function damage and reversible airway obstructive changes, and most have no wheezing symptoms, with chest tightness and cough being the only clinical manifestations. Due to the increased vagal tone at night, cough symptoms mostly manifest at night.23 Persistent airway hyperresponsiveness and small airway obstruction are common features of CVA and bronchial asthma in terms of pulmonary function. Therefore, pulmonary function tests have important clinical significance for the diagnosis and treatment of this disease. Our results confirmed that budesonide inhalation therapy can effectively improve the pulmonary function of patients with CVA. However, pulmonary function indicators generally decreased after 4–8 weeks, and serum IL-6 and TGF-β1 significantly decreased at 2–4 weeks. The ROC curve results indicated that serum IL-6 and TGF-β1 concentrations at 2 weeks could better predict the effect of budesonide treatment. Therefore, we concluded that serum IL-6 and TGF-β1 have obvious significance in predicting the efficacy of budesonide inhalation in the 2 weeks treatment of CVA in clinical application. However, the sample quantity is not large enough, and the expression of inflammatory markers at different time points may have certain defects. More specimens are needed to support these views in the future.
In conclusion, budesonide inhalation combined with conventional symptomatic treatment can significantly reduce the levels of serum IL-5, IL-6, IL-8, TNF-α, TGF-β1, and IgE and number of eosinophils in patients with CVA to reduce inflammation and the allergic response, thereby reducing the cough symptom score, improving pulmonary function, and improving therapeutic efficacy. At different time points, IL-6 and TGF-β1 were good early predictors of the efficacy of budesonide treatment.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki (revised in 2013) and was approved by the Ethics Committee of The Second Hospital of Jiaxing (Ethics number JXEY-2022JX060). Samples were obtained from all patients with written informed consent.
Funding
This work was supported by Health Bureau of Zhejiang Province (grant no. 2024KY443), and Science and Technology Bureau of Jiaxing (grant no 2022AD30028).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Uryasjev MO, Ponomareva IV, Bhar M, et al. [The cough variant asthma]. Ter Arkh. 2020;92(3):98–101. doi:10.26442/00403660.2020.03.000404
2. Zhan W, Wu F, Zhang Y, et al. Identification of cough-variant asthma phenotypes based on clinical and pathophysiologic data. J Allergy Clin Immunol. 2023;152(3):622–632. doi:10.1016/j.jaci.2023.04.017
3. Diab N, Patel M, O’Byrne P, et al. Narrative Review of the Mechanisms and Treatment of Cough in Asthma, Cough Variant Asthma, and Non-Asthmatic Eosinophilic Bronchitis. Vol. 200. LUNG; 2022:707–716
4. Wang MZ, He QN, Yuan HX, et al. [Roles of IL-4, IL-5 and IgE in childhood cough variant asthma]. Zhongguo Dang Dai Er Ke Za Zhi. 2006;8(5):382–384.
5. Yi F, Jiang Z, Li H, et al. Small airway dysfunction in cough variant asthma: prevalence, clinical, and pathophysiological features. Front Physiol. 2021;12:761622. doi:10.3389/fphys.2021.761622
6. Lai K, Zhan W, Wu F, et al. Clinical and inflammatory characteristics of the Chinese APAC cough variant asthma cohort. Front Med. 2021;8:807385. doi:10.3389/fmed.2021.807385
7. Vogelberg C, Cuevas SF, Watling CP, et al. Therapeutic principles and unmet needs in the treatment of cough in pediatric patients: review and expert survey. BMC Pediatr. 2023;23(1):34. doi:10.1186/s12887-022-03814-0
8. Holzinger F, Beck S. [Diagnostics and treatment of cough]. Dtsch Med Wochenschr. 2014;139(40):2025. doi:10.1055/s-0034-1374716
9. Fujimura M. [Pathophysiology, diagnosis and treatment of cough variant asthma]. Rinsho Byori. 2014;62(5):464–470.
10. Hodgson D, Mortimer K, Harrison T. Budesonide/formoterol in the treatment of asthma. Expert Rev Respir Med. 2010;4(5):557–566. doi:10.1586/ers.10.60
11. Peces-Barba RG, Villar AF. [Budesonide/formoterol in the treatment of COPD]. Arch Bronconeumol. 2010;46(Suppl 4):22–27.
12. Gao J, Wu HG, Wu F. Small airways dysfunction and bronchial hyper-responsiveness in cough variant asthma. Int J Gen Med. 2020;13:1427–1434. doi:10.2147/IJGM.S286144
13. Asthma Workgroup CS, Respiratory, Diseases (CSRD). Chinese medical, association. the Chinese national guidelines on diagnosis and management of cough,(December 2010). Chin Med J. 2011;124(20):3207–3219.
14. Shi X, Peng XF, Kong LF. An analysis of factors for quality-of-life in patients with chronic cough. Chinese J Int Med. 2011:50(08):672.
15. Kobayashi F, Saraya T, Akizawa T, et al. Impact of cough severity on the diagnostic yield of endobronchial ultrasonography transbronchial biopsy with guide sheath: a retrospective observational Study. J Clin Med. 2024;13(2):347. doi:10.3390/jcm13020347
16. Wu Q, Wang L, Wu M, Lin H. Effect of montelukast combined with budesonide on inflammatory response and pulmonary function in children with cough variant asthma: a meta-analysis. J Coll Physicians Surg Pak. 2023;33:1040–1049.
17. Yi F, Zhan C, Liu B, et al. Effects of treatment with montelukast alone, budesonide/formoterol alone and a combination of both in cough variant asthma. Respir Res. 2022;23(1):279. doi:10.1186/s12931-022-02114-6
18. Ibrahim AS, Amer YS, Adnan AT, et al. Patient response to the management during the acute presentation of cough variant asthma: retrospective cohort study. Saudi J Biol Sci. 2023;30(12):103875. doi:10.1016/j.sjbs.2023.103875
19. Bao W, Chen Q, Lin Y, et al. Efficacy of procaterol combined with inhaled budesonide for treatment of cough-variant asthma. Respirology. 2013;18(Suppl 3):53–61. doi:10.1111/resp.12169
20. Qiang L, Li X, Li Q, et al. ABHD2 deficiency aggravates ovalbumin-induced airway remodeling through the PI3K/Akt pathway in an animal model of chronic asthma. Pol J Vet Sci. 2023;26(4):635–646. doi:10.24425/pjvs.2023.148283
21. Lodyga M, Hinz B. TGF-beta1 - A truly transforming growth factor in fibrosis and immunity. Semin Cell Dev Biol. 2020;101:123–139. doi:10.1016/j.semcdb.2019.12.010
22. Boutanquoi PM, Burgy O, Beltramo G, et al. TRIM33 prevents pulmonary fibrosis by impairing TGF-beta1 signalling. Eur Respir J. 2020:55;1.
23. Niimi A, Matsumoto H, Minakuchi M, et al. Airway remodelling in cough-variant asthma. Lancet. 2000;356(9229):564–565. doi:10.1016/S0140-6736(00)02584-8
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
