Back to Journals » International Journal of Women's Health » Volume 12
The Effect of Perceived Stress During Pregnancy on Preterm Birth
Authors Tanpradit K, Kaewkiattikun K
Received 18 November 2019
Accepted for publication 30 March 2020
Published 15 April 2020 Volume 2020:12 Pages 287—293
DOI https://doi.org/10.2147/IJWH.S239138
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Kittikhun Tanpradit, Kasemsis Kaewkiattikun
Department of Obstetrics & Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand
Correspondence: Kasemsis Kaewkiattikun
Department of Obstetrics & Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Bangkok 10300, Thailand
Tel +668 95366601
Email [email protected]
Background: Preterm birth is one of the most common problems in pregnancy globally, often leading to neonatal death. The rate of preterm birth is increasing every year. The etiology of preterm birth is multifactorial; preventable maternal psychosocial stress is one of the causes of preterm birth. There has not yet been a report of maternal psychosocial stress and preterm birth in Thailand. This study aimed to explore the relationship between maternal perceived stress and preterm birth.
Objective: To study the effects of maternal perceived stress on preterm birth.
Patients and Methods: An unmatched case–control study was conducted in postpartum women, between January 17, 2019, and September 30, 2019, at the Department of Obstetrics and Gynecology, Faculty of Medicine, Vajira Hospital. A total of 200 participants were enrolled and divided into case and control groups in a 1:1 ratio. The case group consisted of postpartum women with preterm birth and the control group consisted of consecutive postpartum women with term birth. Perceived stress was measured by using the Thai Perceived Stress Scale-10 (T-PSS-10).
Results: Maternal perceived stress during pregnancy was significantly greater in preterm birth compared with term birth in both means score (19.43± 4.48 vs 14.08± 4.06, p< 0.001) and moderate to high stress level (92 vs 51, p< 0.001). Perceived stress score and stress level were significant predictive factors for preterm birth (AOR 1.31, 95% CI 1.20– 1.44, P < 0.001 and AOR 8.66, 95% CI 3.64– 20.63, P < 0.001, respectively).
Conclusion: Maternal perceived stress during pregnancy was statistically greater in preterm birth. Perceived stress score and stress level were significant predictive factors for preterm birth.
Keywords: perceived stress, pregnancy, preterm birth, T-PSS-10, Thailand
Introduction
The World Health Organization (WHO) defines preterm birth as any birth before 37 completed weeks of gestation, or fewer than 259 days since the first day of the women’s last menstrual period.1 Preterm birth results in a significant perinatal health problems and long-term impacts on families. Preterm birth rate appears to be increasing.2 Globally, the preterm birth rate was estimated at 9.8% (8.3–10.9) in 2000, and 10.6% (9.0–12.0) in 2014.3 The highest preterm birth rates in 2014 were in Southeastern Asia, South Asia and sub-Saharan Africa.2,3 Preterm birth rates in Thailand in 2010 were 12.0%, the 55th in the world.2
It is now clear that the etiology of preterm birth is multifactorial. Risk factors include uterus overdistension, maternal genital tract infection, diabetes mellitus, hypertension, and psychological stress. Psychosocial stress is increasingly being reported as a significant risk factor for preterm birth because of neuroendocrine, immune-inflammatory, vascular, and behavioral changes during pregnancy.4 Moreover, lifestyle changes are also an important cause of increasing psychosocial stress including urbanization, health behavior, physical activities, employment, working condition, tobacco use, alcohol use, and illicit drug use.
Perceived stress is the feelings or thoughts that an individual has about how much a stress event or situation generates at a given point in time or over a given time period.5 Measurement of psychosocial stress has been proposed by several experts. The most widely used psychological instrument for measuring the perception of stress is the Perceived Stress Scale (PSS) which was originally developed by Cohen S. et al in 1983.6 The PSS is a self-assessment tool to appraise the degree to which an individual has been confronted with unpredictable, uncontrollable, and overloaded events in the past month. The PSS has been translated into various versions and languages, including Thai. The PSS version in Thai is PSS-10 which is a brief, easy-to-use version with equivalent psychometric properties to the PSS-14. The Thai version of the PSS-10 (T-PSS-10) has been proved to have good reliability and validity for estimating the level of stress perception within a Thai cultural context.7
The prevalence of perceived stress during pregnancy ranges from 11.6% to 34%.8,9 There is strong evidence that antenatal psychosocial stress during pregnancy increases the likelihood of preterm birth.10 Results from a systematic review discovered that the association of psychological stress with preterm birth varied according to the dimensions and timing of stress exposure. Most studies demonstrated positive results with risk ratios between 1.2 and 2.1.11 Recently, a systematic review and meta-analysis revealed that antenatal stress was significantly associated with preterm birth.12 Additionally, there is evidence that higher levels of psychological stress during pregnancy put expectant mothers at significantly increased risk of preterm birth.13
Although many studies have reported the effect of maternal perceived stress on preterm birth, this has not yet been studied in Thailand and in South-East Asia region. Moreover, there have been few reports of possible risk factors among pregnant women. This study sought to explore maternal stress levels, perceived stress scores, associated and predictive factors in pregnant women with preterm birth. Furthermore, results of this study will provide further information for the prevention and management of antenatal perceived stress to reduce preterm birth.
Patients and Methods
An unmatched case–control study was conducted in postpartum women, between January 17, 2019, and September 30, 2019, at the Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital. Approval for the study was obtained from the Institutional Review Board (IRB) of the Faculty of Medicine Vajira Hospital, Navamindradhiraj University.
The studied population consisted of postpartum women who gave birth at the Department of Obstetrics & Gynecology, Faculty of Medicine Vajira Hospital. The population was divided into case and control groups. The case group was postpartum women with preterm birth (gestational age of 24–36+6 weeks) and the control group was consecutive postpartum women with term birth (37–42 weeks). Inclusion criteria of both groups were Thai nationals who could communicate in Thai, age >19 years old, and singleton pregnancy. Exclusion criteria of both groups were potential risk for preterm birth, including polyhydramnios, fetal macrosomia, incompetent cervix, history of preterm birth, history of cervical surgery, preterm premature rupture of membrane, uterine abnormalities, and maternal infection (intrauterine, urogenital and periodontal disease); conditions that affected maternal physiologic stress such as gestational diabetes mellitus; maternal indication for termination of pregnancy (severe preeclampsia, placental abruption, placenta previa with active vaginal bleeding); and history of psychiatric illness.
The sample size for unmatched case–control was calculated using data from a previous study in Sweden.14 They found that maternal stress during pregnancy was 42.3% in preterm birth and 20% in term birth (p < 0.000). The confidence level of 95% and power of 90% was applied to determine the difference between groups. Adding 10% for incomplete data, a total of 198 participants (99 in each group) were enrolled in this study by computerized simple random sampling technique and divided into case and control groups at a ratio of 1:1.
All participants were informed about study processes by a well-trained research assistant, including the aim of the study, the methods of interview, benefits of the study, harm that may be caused to the participant physiologically and psychologically, and their right to leave the study at any time they desired or feel uncomfortable about anything in the study. Data from the study always remained confidential.
After completing informed and written consent, participants who fulfilled the inclusion and exclusion criteria were interviewed by a well-trained research assistant using a structured questionnaire which included demographic data (age, body mass index: BMI, marital status, educational status, occupation, incomes, smoking, and alcohol drinking), obstetric data (parity, abortion, pregnancy intention), serious life events during the past month of pregnancy (death of close relatives, divorced/separated, fired/forced to change job, physical/psychological trauma from family members, suicidal ideation/attempts), perceived stress score, and maternal stress level during the past month of pregnancy.
Maternal perceived stress was measured by T-PSS-10. The T-PSS-10 is composed of a 10-item questionnaire with 5-point Likert scale ranging from 0 (never) to 4 (very often), representing how often they had perceived stress within the past month. The sum of all 10 items was calculated for the final T-PSS-10 score. Individual scores can range from 0 to 40 with higher scores indicating greater perceived stress. In this study, the authors categorized the final T-PSS-10 score into 3 groups to identify maternal stress level. Scores of 0–13 were considered as low stress, 14–26 as moderate stress, and 27–40 as high stress.
The primary outcomes of this study were identifying maternal stress level and perceived stress score during pregnancy in pregnant women and comparing preterm birth to term birth. The secondary outcomes were investigating associated factors and predictive factors of preterm birth. The data were analyzed by a statistician using SPSS version 22 (IBM Corp., Armonk, NY, USA).15 Student’s t-test and Chi-squared test were used for data analysis. Univariate and multivariate analyses were further entered into logistic regression analysis to determine independent predictors of preterm birth and presented as odds ratio and 95% CI. P-value of less than 0.05 was considered statistically significant.
Results
This case–control study was conducted between January 17, 2019, and September 30, 2019. A total of 200 postpartum women were enrolled in this study, including 100 cases and 100 controls. Baseline demographic characteristics of all participants are shown in Table 1. The majority of the 200 participants had a mean age of 27.01±6.39 years old, normal BMI (85.5%), were married (79.0%), had a high school education (50.0%), were employed (53.5%), had income of 10,001–20,000 baht, were non-smokers (93.5%), and drank no alcohol during pregnancy (93.5%). The obstetric characteristics showed that the majority were multiparity (59.5%), had no previous abortion (82.0%), and had unintended pregnancy (55.5%). Most participants had no serious life events during the last month of pregnancy including no death of close relatives (91.0%), not divorced/separated (85.0%), nor fired/forced to change job (90.5%), nor suffered physical/psychological trauma from family members (80.0%), and suicidal ideation/nor had suicide attempts (95.5%). A comparison of preterm birth with term birth found that marital status, alcohol drinking, pregnancy intention, divorce/separation, and physical/psychological trauma from family members was significantly different between groups (p<0.005).
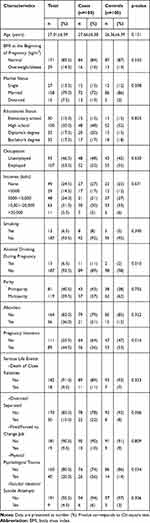 |
Table 1 Demographic Characteristics of Postpartum Women and Association with Preterm Birth |
Table 2 shows maternal stress level and mean perceived stress scores measured by T-PSS-10. Most postpartum women with preterm birth had moderate stress (83%), whereas most of those with term birth had low stress (65%). Maternal stress level was significantly higher in preterm birth than term birth (p<0.001). Mean prenatal perceived stress scores were 19.43±4.48 in preterm birth group and 12.08±4.06 in term birth group. Those with preterm birth reported significantly higher perceived stress scores than those with term birth (p<0.011).
 |
Table 2 Maternal Stress Level and Perceived Stress Scores During Pregnancy |
To analyze maternal stress level and associated factors predicting preterm birth, univariate regression analysis found that significant factors were maternal stress level (OR = 11.05, 95% CI 4.86–25.14), marital status (OR = 7.76, 95% CI 1.70–35.54), alcohol drinking (OR = 6.06, 95% CI 1.31–28.07), pregnancy intention (OR = 0.50, 95% CI 0.28–0.88), divorced/separated (OR = 3.24, 95% CI 1.37–7.69), and physiological/psychological trauma (OR = 2.16, 95% CI 1.05–4.44). After multiple logistic regression adjusting for maternal stress level, T-PSS-10 scores, marital status, alcohol drinking, pregnancy intention, divorce/separation, physical/psychological trauma and preterm birth were analyzed. This study found that significant predictive factors of preterm birth were maternal stress level (adjusted OR = 8.66, 95% CI 3.64–20.63) and T-PSS-10 scores (adjusted OR = 1.31, 95% CI 1.20–1.44) (Table 3).
 |
Table 3 Univariate and Multiple Logistic Regression Analyses of Factors Associated with Preterm Birth |
Discussion
This case–control study of how perceived prenatal stress affects preterm birth using T-PSS-10 found that most postpartum women with preterm birth had moderate stress making it difficult to evaluate the effect of high stress on preterm birth. The occurrence of preterm birth was significantly correlated with prenatal perceived stress scores (19.43±4.48 vs 12.08±4.06, p< 0.001). Comparisons with previous studies using Cohen’s PSS showed that this study is consistent with the results of two studies in America. They found that preterm birth was associated with prenatal stress (OR 1.49, 95% CI: 1.00–2.23, p = 0.05) and (OR 3.50, 95% CI: 1.38–8.87, p = 0.01).16,17 Moreover, this study is also consistent with the results of studies that used different stress measurement tools from Sweden (OR 2.15, 95% CI 1.18–3.92, p = 0.012),14 and China (OR 2.86, 95% CI 1.26–6.47, p = 0.01).18 Additionally, the results of this study are consistent with a recent systematic review and meta-analysis from 1966 to 2016, including two case–control and six cohort studies, which revealed that antenatal stress was significantly associated with preterm birth (OR 1.42, 95% CI 1.05–1.91).12 Although there are few reports of negative effects from India (OR 1.28, 95% CI 1.31–5.14)19 and America (OR 1.14; 95% CI 0.97–1.34),20 most studies demonstrate that perceived stress during pregnancy significantly increases the occurrence of preterm birth, with a risk ration between 1.2 and 2.1.11
In addition, this study revealed that higher maternal stress level was significantly associated with preterm birth occurrence (p < 0.001). This finding is consistent with a study from America, in which perceived stress scores were categorized into quartiles from low stress to high stress. They found that women with the highest stress were at more risk of preterm birth than those with the lowest risk (OR 3.50, 95% CI 1.38–8.87) with a linear trend for each increasing quartile of stress (ptrend =<0.01).17 This finding indicates that the higher the stress level the greater risk of preterm birth. Therefore, interventions targeted at reducing stress during pregnancy should be part of a strategy to decrease risk of preterm birth. All pregnant women attending antenatal clinic should be screened for psychosocial stress.21 Moreover, psychological counseling, psychotherapeutic support, family and social support should also be provided to high risk populations.11,22
In this study, significant associations were seen between marital status, alcohol drinking, pregnancy intention and preterm birth. These factors could be perceived as stressful events that affect the pregnancy outcome. However, after adjustment for confounders using multiple logistic regression to adjust for maternal stress level, PSS scores, marital status, alcohol drinking, pregnancy intention, divorce/separation, physical/psychological trauma and preterm birth, this study revealed that these factors were not significantly related to preterm birth. The significant predictive factors for preterm birth were perceived stress scores and maternal stress level.
Furthermore, this study found that serious life events did not increase the risk of preterm birth. This result is in contrast to previous studies. A report from Peru revealed that prenatal serious life events caused more than a two-fold increased risk of preterm birth (OR 2.29, 95% CI 1.65–3.18) and the magnitude of the association increased with the increased frequency of serious life events (ptrend,0.001).23 Another report from China revealed that risk of preterm birth increased with higher prenatal serious life events during the first trimester (OR 2.40, 95% CI 1.13–5.09) and second trimester (OR 2.86, 95% CI 1.26–6.47).18 The reason for different findings in this study may be that the impact of stressful life events varies depending on lifestyle, culture, intent of stressor, timing of stressor, and self-perceived stress.24,25
The results of this study showed the relationship between perceived stress during pregnancy and preterm birth; as such they have important clinical applications. To prevent and decrease preterm birth rate, reducing maternal perceived stress is one of the most important goals with which institutes should be concerned. Several interventions for psychosocial stress reduction should be achieved by cooperation between obstetricians, psychiatrists, all relevant medical personnel, and families. A screening protocol of perceived stress and other mental disorders might be initiated to detect early signs of stress in all pregnant women and, if possible, even earlier during pre-conception period. Appropriate management for stress reduction should then be performed as soon as possible.
This study provides supporting evidence that demonstrates the effect of perceived stress on preterm birth. These findings will help physicians realize the importance of perceived stress during pregnancy. Future research should study the effects of psychosocial stress reduction on preterm birth. Moreover, suggestions for future research should be extended to the study of family roles in psychosocial stress reduction and preterm birth.
Strengths and Limitations
The strength of this study is that it is the first study in Thailand about the relationship between maternal stress during pregnancy and preterm birth. Moreover, this study used a Thai version of Cohen’s perceived stress scale (T-PSS-10), which is accepted worldwide, and has good reliability and validity for estimating the level of stress perception within a Thai cultural context. There are many limitations of this study. Firstly, this study was a case–control study for which data were obtained from participant’s recall memory causing recall bias. Correcting for these limitations meant applying multivariate analysis to reduce bias and confounders and evaluating prenatal stress within the last month of pregnancy before preterm birth to reduce recall bias. Secondly, the participants were unblinded. Thirdly, maternal perceived stress score and stress level evaluation within the past month of pregnancy could not provide an adequate representation of stress throughout the whole pregnancy. Finally, factors that might affect psychosocial stress, such as attitude, beliefs, socioeconomic problems, life expectations, and family relationships were not evaluated in this study. Future research would study a larger sample size to support the connection of perceived stress and preterm birth. Moreover, a cohort design study is needed to evaluate the effects of maternal perceived stress throughout pregnancy on preterm birth. Suggested research should be extended to the study of maternal and neonatal outcomes of maternal perceived stress.
Conclusion
Preterm birth is a worldwide perinatal health problem. Maternal perceived stress during pregnancy was statistically greater in preterm birth. Perceived stress scores and stress levels were significant predictive factors for preterm birth.
Acknowledgments
The authors would like to thank all participants in the study. They also express their gratitude and thanks to Mr. Jason Cullen for proofreading the earlier drafts of the manuscript. Finally, this study was made possible through funding and support from Navamindradhiraj University Research Fund. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this research.
References
1. World Health Organization. WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56:247–253.
2. Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi:10.1016/S0140-6736(12)60820-4
3. Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37–46. doi:10.1016/S2214-109X(18)30451-0
4. Schetter CD. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–558. doi:10.1146/annurev.psych.031809.130727
5. Phillips AC. Perceived stress. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York, NY: Springer; 2013.
6. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. JHSB. 1983;24(4):385–396.
7. Wongpakaran N, Wongpakaran T. The Thai version of the PSS-10: an investigation of its psychometric properties. Biopsychosoc Med. 2010;4:1–6. doi:10.1186/1751-0759-4-6
8. Engidaw NA, Mekonnen AG, Amogne FK. Perceived stress and its associated factors among pregnant women in Bale zone Hospitals, Southeast Ethiopia: a cross‑sectional study. BMC Res Notes. 2019;12:356:1–6.
9. Pantha S, Hayes B, Yadav BK, et al. Prevalence of stress among pregnant women attending antenatal care in a tertiary maternity hospital in Kathmandu. J Women's Health Care. 2014;3:183. doi:10.4172/2167-0420.1000183
10. Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth. 2015;28:179–193. doi:10.1016/j.wombi.2015.02.003
11. Shapiro GD, Fraser WD, Frasch MG, Séguin JR. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J Perinat Med. 2013;41(6):631–645. doi:10.1515/jpm-2012-0295
12. Lima SAM, El Dib RP, Rodrigues MRK, et al. Is the risk of low birth weight or preterm labor greater when maternal stress is experienced during pregnancy? A systematic review and meta-analysis of cohort studies. PLoS One. 2018;13(7):e0200594. doi:10.1371/journal.pone.0200594
13. Wadhwa PD, Entringer S, Buss C, Lu MC. The contribution of maternal stress to preterm birth: issues and considerations. Clin Perinatol. 2011;38(3):351–384. doi:10.1016/j.clp.2011.06.007
14. Lilliecreutz C, Larén J, Sydsjö G, Josefsson A. Effect of maternal stress during pregnancy on the risk for preterm birth. BMC Pregnancy Childbirth. 2016;16(5):1–8. doi:10.1186/s12884-015-0775-x
15. IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013.
16. Seravalli L, Patterson F, Nelson DB. Role of perceived stress on the occurrence of preterm labor and preterm birth among urban women. J Midwifery Women's Health. 2014;59(4):374–379. doi:10.1111/jmwh.12088
17. Szegda K, Bertone-Johnson ER, Pekow P, et al. Prenatal perceived stress and adverse birth outcomes among puerto rican women. J Women's Health. 2018;27(5):699–708. doi:10.1089/jwh.2016.6118
18. Zhu P, Tao F, Hao J, Sun Y, Jiang X. Prenatal life events stress: implications for preterm birth and infant birthweight. Am J Obstet Gynecol. 2010;203:
19. Aneja J, Chavan BS, Garg J, Huria A, Goel P. Does prenatal maternal stress affect the outcome of pregnancy? A prospective study from North India. J Mental Health Hum Behav. 2018;23:12–18. doi:10.4103/jmhhb.jmhhb_55_17
20. Sealy-Jefferson S, Mustafaa FN, Misra DP. Early-life neighborhood context, perceived stress, and preterm birth in African American Women. SSM Popul Health. 2019;7:1–6.
21. American College of Obstetricians and Gynecologists Committee on Health Care for Undeserved Women. ACOG committee opinion no. 343: psychosocial risk factors; perinatal screening and intervention. Obstet Gynecol. 2006;108:469–477. doi:10.1097/00006250-200608000-00046
22. Mamelle NJ. Psychological prevention of early pre-term birth: a reliable benefit. Biol Neonate. 2001;79(3–4):268–273.
23. Barrios Y, ESanchez S, Qiu C, Gelaye B, Williams MA. Risk of spontaneous preterm birth in relation to maternal experience of serious life events during pregnancy. Int J Women's Health. 2014;6:249–257. doi:10.2147/IJWH.S54269
24. Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clin Obstet Gynecol. 2008;51(2):333–348. doi:10.1097/GRF.0b013e31816f2709
25. Class QA, Lichtenstein P, Långström N, D’Onofrio BM. Timing of prenatal maternal exposure to severe life events and adverse pregnancy outcomes: a population study of 2.6 million pregnancies. Psychosom Med. 2011;73(3):234–241. doi:10.1097/PSY.0b013e31820a62ce
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
