Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
The Effect of Longer Dosing Intervals for Long-Acting Injectable Antipsychotics on Outcomes in Schizophrenia
Authors Milz R, Benson C, Knight K, Antunes J , Najarian D , Lopez Rengel PM, Wang S, Richarz U, Gopal S , Kane JM
Received 29 October 2022
Accepted for publication 12 January 2023
Published 7 March 2023 Volume 2023:19 Pages 531—545
DOI https://doi.org/10.2147/NDT.S395383
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Ruth Milz,1 Carmela Benson,1 Karl Knight,1 Jose Antunes,2 Dean Najarian,3 Paola-Maria Lopez Rengel,4 Steven Wang,1 Ute Richarz,5 Srihari Gopal,1 John M Kane6,7
1Janssen Research & Development LLC, Titusville, NJ, USA; 2Janssen-Cilag, Porto Salvo, Portugal; 3Janssen Scientific Affairs, LLC, Raritan, NJ, USA; 4Janssen Cilag, Madrid, Spain; 5Janssen Global Medical Affairs, Cilag, Zug, Switzerland; 6Department of Psychiatry, The Zucker Hillside Hospital, Northwell Health, Queens, NY, USA; 7Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, NY, USA
Correspondence: Ruth Milz, Janssen Research & Development, LLC, 1125 Trenton-Harbourton Road, Titusville, NJ, 08560, USA, Email [email protected]
Abstract: Medication nonadherence in schizophrenia can have serious implications including relapses and hospitalization. Long-acting injectable (LAI) antipsychotics require fewer administrations, while ensuring sustained medication coverage. In this review, we summarize the expected real-world benefits of longer dosing intervals in the management of schizophrenia. LAIs are associated with improved clinical outcomes of less frequent relapses and reduced functional impairment, encouraging patients to regain control of their lives. Aripiprazole lauroxil and paliperidone palmitate three-monthly (PP3M) LAIs have longer dosing intervals of 2– 3 months and provide improved outcomes in patients with schizophrenia. Paliperidone palmitate six-monthly (PP6M) LAI provides the longest dosing interval, twice-yearly dosing, among existing LAIs. Decreasing the frequency of LAI administrations has the potential to reduce occurrence of serious outcomes associated with poor medication adherence. By eliminating the need for daily oral antipsychotic dosing, LAIs could increase the likelihood of patient acceptance, decrease stigma, and promote self-esteem. Longer intervals of medication coverage may be desirable for patients with higher risk of relapse including adults with recent-onset schizophrenia, those living in circumstances that may deprive them of regular access (eg, homeless), those that are in transitions between care settings or to reduce interpersonal contact during public health emergencies (eg, COVID-19 pandemic).
Keywords: adherence, long-acting injectable, paliperidone palmitate, schizophrenia
Introduction
Schizophrenia is a psychiatric illness with a heterogeneous presentation and an etiology and pathophysiology that are difficult to decipher. Patients with schizophrenia usually present negative symptom clusters, as well as lasting cognitive and functional disability.1,2 Most patients with schizophrenia are unable to reach at least one milestone in their lives, such as being in a stable relationship, having full-time competitive employment, or having self-supported independent living.3,4 Patients with schizophrenia also have a shorter life expectancy due to low levels of physical activity and associated comorbidities. Schizophrenia elevates the risk for substance abuse, homelessness, suicides, antisocial personality disorder or psychopathy, and aggression or violent behavior that can lead to arrest or incarceration.5 Progression of schizophrenia worsens total functioning and is associated with episodes of partial or full remission interrupted by relapses that often result in hospitalization and increasing risk of morbidity.3,6
Introduced in 1950s, antipsychotics have been the cornerstone of schizophrenia treatment. Complete adherence to prescribed antipsychotics reduces the severity and frequency of disease symptoms, and nonadherence to oral antipsychotics was soon established to be a most frequent cause of relapse.7,8 In the early stages of schizophrenia, 40–60% patients show nonadherence to oral antipsychotics. Subsequently, 74% discontinue treatment by 18 months, and approximately 42% discontinue within 1 year after the first psychotic episode.9–11 Nonadherence is known to have severe clinical and public health implications including personal suffering, increased caregiver burden, and utilization of acute-care services (emergency room, hospitalization).12 Long-acting injectable (LAI) antipsychotics were developed with an aim to achieve and maintain medication adherence and support better management of schizophrenia symptoms. LAIs eliminate the need for daily dosing, achieve stable medication exposure, and allow regular monitoring of dose administration. Furthermore, patients who are adherent to antipsychotics are more likely to be adherent to medications for comorbid cardiometabolic conditions including antihypertensives, antihyperlipidemics, and antidiabetics, thus predicting better outcomes.13
First-generation LAI antipsychotics including haloperidol decanoate, fluphenazine enanthate, fluphenazine decanoate, clopenthixol decanoate, and perphenazine enanthate have been approved for 1–4 weeks of dosing intervals. Of these, only generics – haloperidol decanoate and fluphenazine decanoate – are available in the United States. Although these LAIs offer prospects for improved adherence, lower discontinuation, and readmission rates, their clinical benefits are compromised by high rates of extrapyramidal adverse effects and tardive dyskinesia that can lead to treatment discontinuation.14,15 Among patients with schizophrenia, second-generation LAIs have an acceptable safety profile and an apparent advantage over first-generation LAIs, although efficacy is comparable among both classes of LAIs.16,17 Dosing intervals with currently available second-generation LAI antipsychotics vary from every 2 weeks (risperidone microsphere LAI), every 2–4 weeks (olanzapine pamoate), every 4 weeks (aripiprazole monohydrate and paliperidone palmitate once monthly [PP1M]), every 4–8 weeks (aripiprazole lauroxil), every 3 months (paliperidone palmitate three-monthly [PP3M]), and every 6 months (with the most recent paliperidone palmitate six-monthly [PP6M] formulation). When compared with their oral counterparts, second-generation LAI antipsychotics have been shown to achieve longer treatment continuity, reduced hospitalization, and relapse rates, as well as lower mortality among patients with schizophrenia.18–20
The efficacy of LAI antipsychotics in treating schizophrenia is supported by extensive evidence and long-standing clinical experience validating their reliable medication delivery, sustained symptom control, and relapse prevention in patients with schizophrenia.21–37 Early introduction of LAIs during treatment in recently diagnosed schizophrenia is associated with meaningful improvements in social functioning.38 LAI formulations are an effective strategy for patients with schizophrenia who relapse due to nonadherence, as well as to maintain long-term symptom control.39 Longer dosing intervals may be beneficial in different subgroups, such as patients with recent onset schizophrenia, high-risk of suicide or with severe psychotic or mood symptoms, as well as those with special circumstances such as limited access to healthcare (eg, homeless or patients without caregivers, remote communities), socially isolated people, or those with a history of violence or incarceration who may be more predisposed to be nonadherent.40,41 Given the increasing emphasis on treatment continuity, PP6M LAI with a 6-month dosing interval and a unique twice-yearly regimen were developed to achieve enhanced outcomes in the management of schizophrenia (Table 1). PP6M is intended for patients adequately stabilized on PP1M or PP3M. In a non-inferiority phase 3 study, PP6M demonstrated relapse prevention efficacy that was comparable to PP3M.42 This review was not intended to be an all-encompassing review article, but rather key studies have been highlighted to provide an overview of expected real-world benefits of longer dosing intervals of LAIs, such as adherence in the management of schizophrenia.
 |
Table 1 Marketed Doses of Paliperidone Palmitate LAIs |
The Effect of Longer-Acting LAIs on Adherence
The benefits of an LAI, and especially an LAI with a longer dosing interval, are best observed in real-world evidence studies, where typical patient adherence and persistence is imperfect. In this setting, the ability of the clinician to monitor and intervene in the event of nonadherence distinguishes LAIs from oral medications. With individual treatment plans and routine clinical visits, LAIs with longer dosing intervals reduce the frequency of monitoring and intervention by the clinician. In a post hoc analysis of real-world studies, patients on LAIs (aripiprazole, fluphenazine, haloperidol, olanzapine, risperidone, and paliperidone) were 89% more adherent to medications (proportion of days covered [PDC] ≥80%; OR [95% CI] 1.89 [1.52–2.35]) than oral antipsychotics and had lower odds of hospitalizations and emergency room admissions.43 In a cohort analysis of the Truven MarketScan database, patients with schizophrenia on the once-monthly aripiprazole monohydrate LAI had significantly higher (p<0.001) rates of adherence (PDC ≥0.80) and a lower risk of treatment discontinuation when compared with oral antipsychotics.44 Furthermore, in a mirror image study, switching to aripiprazole once-monthly LAI was associated with significantly lower (6.6% vs 28.1%, p<0.0001) psychiatric hospitalization rates during a 3-month prospective period compared with the 3-month retrospective period, when the same patients received oral antipsychotics (rate ratio = 0.24).45 Among Medicaid patients with schizophrenia from 6 states (2010–2015), those receiving once-monthly LAIs (aripiprazole monohydrate, olanzapine LAI and PP1M) had significantly higher odds (OR: 1.28; p<0.001) of being adherent (PDC ≥80%) to the antipsychotic treatment as compared to patients receiving oral antipsychotics. Patients receiving the twice-monthly risperidone LAI had higher odds of being adherent (OR: 1.16) than patients on oral antipsychotics, underscoring the benefits of a medication with a longer dosing interval. Although the OR of 1.28 and 1.16, is statistically significant it may not always translate into a clinically significant difference.46 In the pragmatic PRIDE study, the covariate-adjusted mean cumulative function for the number of treatment failures (p=0.007) and the number of institutionalizations (criminal justice encounters or psychiatric hospitalizations) (p=0.005) was statistically lower with PP1M versus oral antipsychotics.47 In a retrospective analysis of six-state Medicaid data of patients who recently experienced a schizophrenia relapse, the odds of at least 1 subsequent relapse was significantly lower (33%) in patients on PP1M (OR [95% CI]: 0.67 [0.49–0.92]; p=0.013) relative to those on oral antipsychotics.48 Patients on PP1M also had a 29% (p=0.004) reduction in all-cause inpatient admissions. The mean proportion of days covered was significantly higher in the PP1M versus the oral antipsychotics cohort (at 6 months: 52.6% vs 46.2%; p=0.013; at 12 months: 41.2% vs 34.7%, p=0.008), suggesting better medication adherence in patients on PP1M.48 Concordant results were observed in a similar study of patients with a history of schizophrenia relapses where the probability of an all-cause inpatient admission decreased by 89%, and the total number of inpatient days spent reduced by 31% (all p<0.01) from pre- to post-PP1M periods.49 The likelihood of adherence (mean PDC ≥80%) also increased by 93% (p<0.001) from pre- to post-PP1M periods.49 In an assessment of the IQVIA™ PharMetrics Plus claims database, switching patients from oral risperidone or oral paliperidone to PP1M was associated with higher adherence based on the mean proportion of days covered (pre-PP1M = 0.68 vs post-PP1M = 0.81; mean difference = 0.13, p<0.001), improved comorbidity-related outcomes, and a reduction in the healthcare resource utilization.50 Among veterans, improved clinical outcomes were also observed in patients with schizophrenia who transitioned from oral risperidone or paliperidone to PP1M with a significantly lower frequency of inpatient stays (3.5 vs 1.4, p<0.0001) and a reduced length of inpatient stays (43.4 vs 18.3 days, p<0.0001).51 Similarly, a retrospective analysis of electronic medical records from Atrium Health showed that initiation of PP1M significantly reduced (p<0.001) inpatient visits (67.6% to 22.4%), 30-day readmissions (12.4% to 2.4%), and emergency room visits (68.6% to 45.7%) with a more substantial reduction observed in patients with a prior relapse compared with the overall cohort.52
In an analysis of pharmacy and medical claims data in the Symphony Health Solutions database, patients with schizophrenia who transitioned from PP1M to PP3M reported reduced healthcare resource utilization.53 Patients initiated on PP3M demonstrated treatment persistence, with a high proportion of patients (>80%) adherent to their PP3M treatment (proportion of days covered [PDC] at 6 months ≥0.80).53 In a similar study of veterans with schizophrenia transitioning from PP1M to PP3M, a significant increase (p<0.0001) was displayed in adherence from 6 months before PP3M initiation (PDC: 0.90) to 6 months after PP3M initiation (PDC: 0.97).54 Notably, patients were taking PP1M prior to switching to PP3M, which indicates that the reduction of injection frequency can have a meaningful impact on adherence.54 During the 12-month follow-up period, patients with schizophrenia from a four-state Medicaid database who transitioned from PP1M to PP3M were 2.4 times more likely to be adherent (p<0.001) and 4.6 times more likely to be persistent than patients on PP1M.55 Patients initiated on the longer-acting PP3M had a significantly lower likelihood of at least one inpatient admission (p=0.0011), at least 1 day with home care services use (p=0.012), and at least 1 day of other healthcare services as compared to patients in the PP1M cohort.55
A large retrospective analysis of the IBM MarketScan Multi-State Medicaid database in the United States was performed to evaluate the relapse risk associated with PP1M and PP3M in adult patients with schizophrenia. Treatment with PP3M was associated with significantly greater rates of adherence as measured by PDC (Figure 1) and a lower risk of relapse as compared to PP1M and oral PP treatment;56 the relapse rate negatively correlated with the PDC (Figure 2). The proportion of patients with PDC >80% was 55.3% and 79.7% for patients treated with PP1M and PP3M, respectively. Although the rates of adherence in this real-world study were lower than those reported in clinical trials, visit reminders, blister packs, and extra time spent with study staff, among others, may have contributed to the more favorable outcomes in the latter.
 |
Figure 1 Distribution of patients by PDC category. Abbreviations: PDC, proportion of days covered; PP1M, paliperidone palmitate 1-month formulation; PP3M, paliperidone palmitate 3-month formulation. |
Impact of Adherence on Comorbidity-Related Outcomes
Being adherent to antipsychotics has been associated with better adherence to cardiometabolic medications and a potential reduction in emergency department utilization in patients with schizophrenia and pre-existing cardiometabolic conditions.57 Improved adherence to statins, hypertensives, and beta blockers is associated with a decreased risk of developing cardiovascular disease (25–19%) and all-cause mortality (29–45%).58 In an analysis of a nationwide Finnish database, the use of first and second-generation LAIs reduced discontinuation of statins (adjusted HR [95% CI]: risperidone LAI, 0.71 [0.52–0.97]; olanzapine LAI, 0.58 [0.28–1.21] aripiprazole LAI, 0.74 [0.25–2.25], PP1M, 1.19 [0.51–2.76]), antidiabetic (risperidone LAI, 0.29 [0.06–1.53]; olanzapine LAI, 0.38 [0.20–0.73], aripiprazole LAI, 0 0.59 [0.32–1.09], PP1M, 0.37 [0.28–0.50]), and antihypertensives (risperidone LAI, 0.38 [0.21–0.70]; olanzapine LAI, 0.57 (0.45–0.70) aripiprazole LAI, 0.58 [0.34–0.99], PP1M, 0.58 [0.35–0.96]).59 In a retrospective analysis, commercially insured patients with schizophrenia who transitioned from PP1M to PP3M were less likely to have future claims with a diagnosis for substance-related and addictive disorders, psychoses, drug abuse, and diabetes without chronic complications. PP3M patients were likely to be more adherent to antipsychotic medications compared to the period when they were taking PP1M (OR=2.01, p=0.007).51
Medication Adherence in Schizophrenia
Medication Continuation Rates with Longer Acting Formulations
It is important to understand the impact of lengthening the duration of dosing from daily to once every 2 weeks (ie, twice monthly), or once monthly, or three-monthly on medication continuation and the subsequent benefits. In a 2-year follow-up analysis of the Hungarian National Health Fund database, the median time to discontinuation of second-generation LAIs was longer as compared with oral formulations: 176 days (risperidone LAI), 287 days (olanzapine LAI); in the case of PP1M, the discontinuation rate did not reach the median value as more than 50% of the patients stayed on the treatment during the 2-year observation period. Notably, patients who were treated previously with LAI and switched to another LAI (373 median number of days to treatment discontinuation not reached) achieved a longer time on treatment than patients who were either switched from oral treatment or no previous treatment (172 to 503 days).60 More than half of patients initiated on aripiprazole LAI continued treatment and reported no hospital admissions during the 2-year follow-up versus the period before treatment initiation in a 4-year real-world study. In an indirect comparison, there were no significant differences in hospitalization rates between patients on aripiprazole LAI and PP1M at 2 years.61 In a mirror-image study of normal clinical practice, the use of PP3M in patients clinically stabilized on PP1M was associated with less frequent re-hospitalization during the 2-year follow-up period.62 Converging with these findings, the longer-acting LAI PP3M was associated with lower rates of hospitalization and required lower doses of concomitant medications as compared with the use of oral antipsychotics and shorter-acting LAIs – aripiprazole-1-month and biweekly LAIs in a Spanish real-world study.63 In a Medicaid claims database study, adult patients with schizophrenia using a once-monthly LAI had lower healthcare resource utilization, better adherence (proportion of days covered: 0.56 vs 0.50, p<0.01), and longer median persistence (7.5 months vs 5.5 months) compared to those using twice-monthly (risperidone) LAI.64 Kaplan–Meier rates of antipsychotic treatment persistence at 1 year were higher for patients on the once-monthly versus twice-monthly LAI (37.6% vs 29.6%, p<0.01).64
In a similar analysis of Truven MarketScan Commercial, Medicare Supplemental, and Medicaid Multi-State insurance databases, patients treated with PP1M had significantly lower discontinuation rates (36.5% vs 53.3%; p<0.001), longer days of LAI coverage (233.6 days vs 131.7 days; p<0.001) and were more likely to be adherent than patients on twice-monthly risperidone LAI.65 Patients in the PP1M cohort also had reduced odds of hospitalization (adjusted odds ratio [95% CI]: 0.72 [0.55–0.95]), fewer emergency department visits (adjusted incidence rate ratio [aIRR]: 0.67 [0.61–0.73]), and reduced length of inpatient stay (aIRR: 0.86 [0.82–0.90]) compared to the risperidone LAI cohort.65
In a nationwide analysis from South Korea comparing three LAIs—PP1M, risperidone (twice weekly), and haloperidol (once every 3–4 weeks)—patients on PP1M showed the highest continuation rates at 6 months (57.5%) versus those using the shorter-acting LAIs risperidone (34.5%) and haloperidol (36.8%).66
Effect of Longer Acting Formulations on Relapse
Extended dosing intervals are expected to provide a longer medication exposure and optimized patient-centric outcomes. Aripiprazole lauroxil (1064 mg dose) administered with a 2-month (8-week regimen) dosing interval achieved higher maximal plasma concentrations versus 4- and 6-week regimens (441 mg [4-week]: 125.8 ng/ml, 882 mg [6-week] 131.1 ng/ml, 1064 mg [8-week]: 140.7 ng/ml). Furthermore, multiple-dose simulations showed that aripiprazole lauroxil achieved concentrations within the range achieved by 4- and 6-week regimens that demonstrated efficacy in a phase 3 study.67 These findings were further substantiated in a pharmacokinetic study, wherein the 2-monthly aripiprazole lauroxil LAI provided continuous exposure with the highest average concentration of the drug (140.7 ng/mL) as compared with the 4- and 6-week regimens.68 Long-term treatment effectiveness of olanzapine monthly LAI when compared with oral olanzapine showed median time to all-cause discontinuation as olanzapine LAI: 645 days, oral: 678 days (p=0.61), discontinuation rate as olanzapine LAI: 53.8%, oral: 51.2% (p=0.60), and relapse rate as olanzapine LAI: 20.1%, oral: 18.5% (p=0.66).69 A systematic review and network meta-analysis found an absence of clear evidence for superiority between antipsychotics in terms of relapse prevention or other efficacy outcomes, suggesting clinicians consider tolerability when choosing an antipsychotic for the maintenance treatment of patients with schizophrenia.70
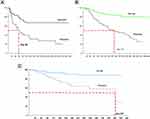
A post hoc analysis of three similarly designed primary relapse prevention studies of paliperidone ER, PP1M, and PP3M was conducted to indirectly compare the three formulations with an aim to determine if longer-acting formulations provide longer protection from relapse due to nonadherence and premature discontinuation.71 The three studies used a group sequential design that allowed early termination if significant evidence of efficacy was obtained based on a pre-planned interim analysis when 50% or 60% of the projected relapse events had occurred. This corresponded to 43 relapse events in the paliperidone ER study, 68 in the PP1M study, and 42 in the PP3M study. The median time to relapse in the placebo group during the double-blind phase provided an estimate of how long it would take for a patient with schizophrenia to relapse after suddenly discontinuing treatment (ie, a nonadherent patient in the real-world). The estimated median time to relapse in the placebo group was notably longer following the discontinuation of PP3M (395 days) than after the discontinuation of PP1M (172 days) or oral paliperidone ER (58 days) (Figure 3).71
Thus, a progressive increase in the estimated median time to relapse was observed that equated with the dosing intervals of the LAIs, suggesting that longer the dosing interval, longer the protection from relapse after discontinuation. Indirectly, this suggests that PP6M may offer an advantage over PP3M, PP1M (and paliperidone ER) in patients with schizophrenia who are nonadherent or vulnerable to relapse by potentially allowing more time for the healthcare treatment team to identify a patient who has missed an injection and to resume treatment prior to a relapse.
Effect on Quality of Life and Functionality
Functional remission along with adequate subjective well-being, quality of life, and treatment satisfaction are increasingly valued as important components of full clinical remission in schizophrenia.72 The convenience of LAIs is expected to have a greater impact on social functioning and quality of life that contribute to the overall clinical stability in patients with schizophrenia. Furthermore, by reducing hospitalizations and improving medication adherence, LAIs can improve long-term functionality and facilitate better social integration and patient empowerment. In a real-world observational study, early introduction of PP3M in recently diagnosed schizophrenia was associated with clinically meaningful improvements in social functioning and high level of treatment satisfaction, while maintaining symptomatic stability.38 Comparable findings were also observed in a 52-week naturalistic study wherein patients on continued use of PP3M achieved both symptomatic and functional remissions.26 Furthermore, switching from a shorter LAI (PP1M) to a longer LAI (PP3M) was associated with meaningful gains in symptom control and other aspects of schizophrenia management including quality of interpersonal communications (with physician, nurse, family, friends, and other people), patient activity, and reductions in caregiving time to support the patient.73 These observations place importance on early initiation and inclusion of LAIs in long-term treatment plan to address needs of patients with schizophrenia.
Effect of Longer Acting Formulations on Patients with Recent-Onset Schizophrenia
Treatment with LAIs has been shown to promote white matter development in patients with recent-onset schizophrenia, and therefore, potentially impede biological trajectories of decline into more chronic disease states.74,75 Despite their benefits, LAIs are often introduced later in the treatment course often in response to treatment failure, hospitalizations, or nonadherence. In a retrospective analysis of the large Truven Health Analytics MarketScan Medicaid, commercial, and Medicare databases, timely initiation (within the first year of a new schizophrenia episode) versus delayed initiation (>1 year following a new episode) of LAIs was associated with reduced all-cause hospitalization rates and healthcare utilization costs.76 These findings concur with European studies that have shown superior healthcare outcomes and enhanced medication adherence to LAI treatment in patients with recent-onset schizophrenia, highlighting the benefits of LAI use during early illness, a crucial period that determines the course and future outcomes of schizophrenia.77,78
Effect of Longer Acting Formulations on Other Specific Sub-Populations
Patients with schizophrenia and a history of recent incarceration are more likely to experience another arrest or incarceration as a treatment failure event rather than hospitalization or change in medication, consistent with the high rates of incarceration of the mentally ill in the United States.79,80 Previously incarcerated individuals with psychotic disorders including schizophrenia also have a higher risk of repeat offending. The risk of repeat offending among individuals with psychosis was observed to be 60% higher compared to those without a psychiatric disorder (OR=1.6, 95% CI=1.4–1.8).81
A combination of personalized behavioral interventions and LAI antipsychotics was associated with reduced rates of substance abuse and incarceration and improvements in medication adherence in homeless individuals with serious mental illnesses.82 In the PRIDE study, a 15-month prospective, real-world, randomized, comparative study of daily oral antipsychotics vs the PP1M LAI, PP1M delayed the median time to treatment failure (HR, 1.43; 95% CI, 1.09–1.88; log rank p=0.011). The results showed the longest period to relapse in the PP1M group. Also, the percentage of therapeutic failures in the PP1M group was also lower than in the group of orally treated patients (39.8% vs 53.7%). This, in turn, could decrease the chances of institutionalization in hospitals and incarceration, as continuous and effective treatments may reduce patients’ risk for relapse.83
In a study of jail records of Summit County, Ohio, patients treated with LAI antipsychotics after the initiation of treatment had a significantly lower risk of criminal justice encounters compared with the period prior to LAI initiation (relative risk [95% CI]: 1 year, 0.74 [0.59–0.93]; p<0.01; 2 years, 0.74 [0.62–0.88]; p<0.0001).84 In a retrospective community-based study comparing the pre- versus the post-LAI antipsychotic initiation period, a decline in the overall incidence of arrests from 8.7 (6-month), 13.5 (1-year), and 20.0 (2-year) to 7.5, 10.0, and 14.8 per 100 persons was observed at 6 months, 1 year, and 2 years, respectively.84
Mental illnesses including schizophrenia are among the most common risk factors for homelessness, which further acts as a psychosocial barrier in the management of schizophrenia.85 In a retrospective analysis of electronic health record data from the Veteran’s Health Administration, PP1M treatment in veterans with schizophrenia was associated with a lower likelihood of homelessness (OR = 0.82, p<0.001) compared to oral atypical antipsychotics.86 Furthermore, transitioning from oral antipsychotics to LAIs was also associated with improvements in criminal behavior, medication adherence, spirituality, and housing stability in a safety-net population of individuals experiencing trauma, homelessness, incarceration, and poverty.87
Effect of Longer Acting Formulations on Caregiver Burden
Suboptimal adherence and persistence of symptoms in patients with schizophrenia is associated with increasing burden on caregivers. In a national survey, caregivers of patients with schizophrenia in the United States, who considered themselves responsible for the patient’s adherence and treatment, identified fewer barriers with LAI use and viewed the patients as more capable of being treatment adherent when on LAIs.88 As seen from data pooled from two large clinical trials, caregiver burden can be substantially reduced by switching from an oral antipsychotic to either PP1M or PP3M.89 In the pragmatic REMISSIO study, patients stabilized on PP1M prior to the start of the study had mild-to-moderate caregiver burden, which reduced significantly (p<0.0001) when the patients were switched from PP1M to reduced dosing frequency with the longer acting PP3M.90 Post hoc analyses of a prospective phase 4 study conducted in patients with schizophrenia from the People’s Republic of China, who switched from oral antipsychotics to PP1M displayed substantial reduction in the caregiver burden.91 A pooled analysis in Asian patients also established that choosing either PP3M or PP1M reduced the psychosocial burden associated with caregiving.92
Development of a Twice-Yearly Long-Acting Injectable
The extensive clinical database of PP1M and PP3M LAIs has supported the development of the modified, longer acting LAI PP6M. PP6M was developed as a dorsogluteal intramuscular injection and is currently the only 6-monthly LAI antipsychotic approved by the US Food and Drug Administration for the treatment of schizophrenia in adults.
Efficacy of PP6M was evaluated in a 12-month, randomized, double-blind, non-inferiority phase 3 global study from 20 countries that randomized 702 adults (ages 18–70) living with schizophrenia. Patients were required to be stabilized with PP1M for at least 4 months or at least one injection cycle of PP3M before receiving PP6M. Clinically stabilized adult patients were randomized in a 2:1 ratio to receive PP6M (478 patients) or PP3M (224 patients). The results displayed non-inferiority of PP6M compared to PP3M on the primary endpoint of time to first relapse at the end of the 12-month period. Results demonstrated that 92.5% of patients treated with PP6M and 95% of those treated with PP3M were relapse-free at 12 months. The safety profile observed in the trial was consistent with previous studies of PP1M and PP3M with no new safety signals emerging.42
The unique proposition of PP6M is that patients need to receive an injection just twice per year. Decreasing the number of injections (lesser number of injections) is very useful for patients, considering convenience, especially for patients facing transportation issues to their healthcare provider (HCP) or injection center, patients living in rural areas with a low density of HCPs or injection centers. Some patients may prefer telehealth appointments and visit their HCPs or injection nurses less often. Patients with busy schedules may perceive frequent injections as a nuisance. Nevertheless, regular contact between patients and clinicians plays an important role in adherence to treatment. Therefore, the time saved for administration can be utilized for other therapeutic activities like rehabilitation and psychotherapy. Also, the PP6M administration schedule provides a more flexible dosing window compared to PP3M and PP1M to help avoid a missed maintenance dose.
Continuous exposure via an effective long-acting antipsychotic medication like PP6M may improve adherence and stabilize adult patients with schizophrenia and related comorbidities, thus preventing them from relapsing and/or requiring hospitalization and reducing caregiver/family burden. Although nonadherence is pervasive in schizophrenia, there are sub-populations that are specifically vulnerable, eg, homeless patients, patients with a history of violence or incarceration, patients at high risk of suicide due to nonadherence, patients in underserved rural areas with limited access to psychiatric care, and recent-onset patients. Fewer injections are associated with lesser social stigma, which is also a barrier in patients with severe mental illness. Thus, longer acting LAIs can potentially reduce the burden on patients, their families, caregivers, as well as the treating clinician.
Effect of Longer Acting LAIs in Public Health Emergencies Such as COVID-19
The Coronavirus Disease 2019 (COVID-19) global outbreak has unprecedented implications on the management of psychiatric illnesses including schizophrenia, necessitating treatment evolution to minimize the impact of psychosocial adversities and maintain continuous treatment monitoring. A clinical guideline recently issued by Serious Mental Illness (SMI) Adviser (an initiative from the American Psychiatric Association [APA] and the Substance Abuse and Mental Health Services Administration [SAMHSA]) suggested that longer acting formulations of antipsychotics may be helpful to limit the possibility of exposure to coronavirus.40,93 Older patients or those with pre-existing conditions, people in self-quarantine or isolation at their home, group home, or facility are particularly of concern. Under these circumstances, it is recommended that patients should have as few direct interpersonal contacts as medically prudent, while maintaining treatment continuity. Some solutions proposed to reduce the number of visits include switching patients on risperidone LAI (twice-monthly dosing) to PP1M or PP3M and switching patients on PP1M to PP3M. Thus, improved access to LAIs is recommended in the prevention of relapses in patients with previous nonadherence and for young patients in the early stages of schizophrenia, ensuring treatment continuity during pandemic restrictions.
Co-occurring medical conditions, such as heart disease, liver disease, and diabetes, contribute to the higher premature mortality rate among individuals with schizophrenia.94,95 The American Psychiatric Association (APA) Committee on Psychiatric Dimensions of Disaster and COVID-19, therefore, encourages hospitals and other facilities to include the ongoing use of LAIs for patients with high-risk chronic illness as a necessary procedure.96 The APA focuses on treatment continuity to reduce the risk of serious consequences (eg, hospitalization, relapse, agitation, violence, etc.). Tele-psychiatric practices (remote consultation via telephone or audio/visual platform, including motivational interviewing) and virtual follow-ups after LAI administration will be an essential part of schizophrenia management that could also continue post-pandemic. Psychiatrists may need to adopt a collaborative care approach with telehealth consultations by including general medical health services and counselling on cardiovascular health and comorbidities.97 Thus, longer-acting LAIs such as PP6M can greatly assist this model by reducing the need for patients with schizophrenia to come into the clinic biweekly, monthly or 3-monthly, and substantially decreasing the risk of contact and exposure during the pandemic. LAIs are extremely beneficial in a healthcare setting where there is an acute shortage of staffing as alternative models of care (eg, visiting injection nurses or mobile clinics) can be implemented. The once-every-6-months dosing frequency of PP6M could help ensure medication continuity in these patients and offer sustained symptom control.
Conclusion
In conclusion, having more LAI treatment options available for patients with schizophrenia will help achieve treatment continuity, relapse prevention, and reduced functional impairment via improved consistent medication delivery for extended intervals (or periods). Notably, having fewer (less frequent) injections is important to patients. Thus, there is evidence supporting the development of longer LAIs with extended dosing intervals to optimize clinical outcomes and address challenges in the management of schizophrenia. These longer acting treatments can have an advantage over existing oral or other LAIs in providing a longer safety net for clinicians to intervene and resume treatment, thereby reducing occurrences of more serious outcomes (eg, relapse and hospitalization) in vulnerable patients with schizophrenia who are nonadherent. By virtue of assured medication delivery, sustained therapeutic effects, and the reduced frequency of injections, longer-acting LAIs are expected to result in meaningful clinical benefits in terms of improved patient adherence and reduced risk of relapse compared with oral or other LAI antipsychotics. These LAIs may also provide a unique treatment option for adult patients with recent-onset schizophrenia, who are more likely nonadherent to antipsychotic medications and who may benefit more from consistent antipsychotic coverage to help prevent relapse. Fewer injections could also positively influence patient preference and help overcome social stigma associated with LAI use.98 Less frequent dosing may also be advantageous for patients from access-deprived rural areas who may receive services through telepsychiatry but have infrequent in-person contact with healthcare professionals. By preserving functionality and boosting self-esteem and overall quality of life, patients may be more accepting of the patient-centered care offered by PP6M and other longer-acting LAIs to achieve meaningful life goals. Nonetheless, further studies, two-arm head-to-head superiority trials, and mirror studies, based on real-world samples of patients, are needed to assess long-term safety, impact on quality of life and on functioning, and to define patient sub-populations that would benefit maximally from this new option of treatment. Large pragmatic trials, longer follow-up studies, etc. are needed to elucidate the true clinical benefits of PP6M and other longer acting injectable antipsychotics.
Expert Opinion
Antipsychotic medications are a mainstay of schizophrenia management; however, nonadherence can lead to increased number of relapses and exacerbation of symptoms. The consequences of exacerbation and increase of relapses caused by nonadherence to antipsychotic medication may include hospitalization, aggressive behavior, substance abuse, suicide, and disease progression. Addressing treatment nonadherence has been the catalyst for research and development of long-acting injectable (LAIs) medications. LAIs reduce risk of nonadherence, allowing healthcare professionals to monitor and intervene appropriately if patients fail to take their medication.12,13 Longer dosing regimens help patients with schizophrenia and their healthcare teams to focus less on medication administration and more on other aspects of their treatment plans, such as psychosocial interventions and physical health.12,13 Other benefits include more consistent bioavailability, predictable correlation between dosage and plasma levels, reduced peak-trough plasma levels, improved patient outcomes, improved patient and physician satisfaction, lower relapse rates, and more regular contact with the mental healthcare team.43–55,57–66 For most LAI the administration schedule also provides a more flexible dosing window to help avoid a missed maintenance dose compared to oral treatments.
Although LAI antipsychotics are often prescribed to patients with chronic schizophrenia who have been unable to adhere to oral medications, there is strong evidence supporting the use of LAI antipsychotics earlier in the disease process. Patients with recent-onset schizophrenia, who are more likely nonadherent to antipsychotic medications, may benefit from consistent antipsychotic coverage with LAIs to help prevent relapse, leading to improvements mid- and long-term in outcomes, especially in the first 2 to 3 years of illness.
Although LAIs have several therapeutic advantages over oral antipsychotics, their use may be limited by lack of awareness and negative perceptions including dose selection, time of initiation, resource and cost issues, stigma, and fear of needles.99 Educating clinicians, patients, and families/caregivers on the usage and potential benefits of LAIs can increase familiarity and its acceptance.100,101
LAI formulations that provide optimal efficacy to support early use, less frequent injection for better patient convenience, and improved safety and tolerability profiles are the current advances in this field. Currently, the PP6M LAI has the longest available dosing interval of 6 months and is intended for use in stable patients with schizophrenia who have been adequately treated with PP1M and PP3M for at least 4 and 3 months, respectively. Findings from real-world observational studies have shown that early introduction of PP3M in patients with recently diagnosed schizophrenia was linked to clinically significant improvements in social functioning and a high degree of treatment satisfaction, while maintaining symptomatic stability.26,38 Studies revealed that patients preferred less-frequent injectable over daily orals and preferred to switch from PP1M to PP3M, a less frequent and longer dosing intervals option.102 Similarly, the twice-yearly dosing regimen of PP6M represents a significant advancement over existing treatments for schizophrenia and therefore would allow patients with limited access to healthcare due to geographic or economic factors, pandemics such as COVID-19 and healthcare facilities anticipating or experiencing staffing shortages to have more consistent treatment coverage. Its widespread use will require a paradigm shift in how clinicians and patients place oral antipsychotics and LAIs in the management of schizophrenia.
Further long-term studies are warranted that can assess LAI treatment safety and impact on patients’ adherence, functioning, quality of life and satisfaction versus oral daily antipsychotics. Similarly, further studies in special populations (eg, young adults) could help to define new patient sub-populations that would benefit maximally from this new option of treatment. Adopting LAIs can be an impactful decision towards improved quality of life and overall outcomes for patients with schizophrenia and can potentially reduce overall costs and caregiver burden in the future.
Acknowledgments
We acknowledge Priya Ganpathy, MPharm CMPP, and Salgo Merin Ricki Elenjikamalil, PhD (SIRO Clinpharm Pvt. Ltd., India) for medical writing assistance and Ellen Baum, PhD (Janssen Global Services, LLC) for additional editorial support. We also thank the study patients and investigators for their support.
Funding
This study was supported by Janssen Research & Development, LLC.
Disclosure
John M. Kane has been a consultant for or received honoraria from Alkermes, Allergan, Boehringer-Ingelheim, Cerevel, Dainippon Sumitomo, HLS, Indivior, Intra-Cellular Therapies, Janssen, Johnson and Johnson, Karuna, LB Pharmaceuticals, Lundbeck, Lyndra, Merck, Minerva, Neurocrine Biosciences, Newron, Novartis, Otsuka, Pierre Fabre, Reviva, Roche, Saladex, Sunovion, Takeda, and Teva Pharmaceutical Industries; has received grant support from Otsuka, Lundbeck, Sunovion, and Janssen; and is a shareholder of LB Pharmaceuticals, North Shore Therapeutics, MedinCell, and Vanguard Research Group; royalties from Up to Date. Srihari Gopal was employed by Janssen Research & Development, LLC, USA when the study was conducted and is now employed by Regeneron Pharmaceuticals. All other authors are employees of Janssen and may hold company stocks or stock options. The authors report no other conflicts of interest in this work.
References
1. Tandon R, Gaebel W, Barch DM, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;150(1):3–10. doi:10.1016/j.schres.2013.05.028
2. McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia-an overview. JAMA Psychiatry. 2020;77(2):201–210. doi:10.1001/jamapsychiatry.2019.3360
3. Montemagni C, Frieri T, Rocca P. Second-generation long-acting injectable antipsychotics in schizophrenia: patient functioning and quality of life. Neuropsychiatr Dis Treat. 2016;12:917–929. doi:10.2147/NDT.S88632
4. Harvey PD, Heaton RK, Carpenter WT, Green MF, Gold JM, Schoenbaum M. Functional impairment in people with schizophrenia: focus on employability and eligibility for disability compensation. Schizophr Res. 2012;140(1–3):1–8. doi:10.1016/j.schres.2012.03.025
5. Volavka J, Citrome L. Pathways to aggression in schizophrenia affect results of treatment. Schizophr Bull. 2011;37(5):921–929. doi:10.1093/schbul/sbr041
6. Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br J Psychiatry. 2004;184:346–351. doi:10.1192/bjp.184.4.346
7. Brissos S, Veguilla MR, Taylor D, Balanza-Martinez V. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol. 2014;4(5):198–219. doi:10.1177/2045125314540297
8. Suzuki T, Uchida H, Takeuchi H, Tsuboi T, Hirano J, Mimura M. A review on schizophrenia and relapse--A quest for user-friendly psychopharmacotherapy. Hum Psychopharmacol. 2014;29(5):414–426. doi:10.1002/hup.2421
9. Brasso C, Bellino S, Bozzatello P, Montemagni C, Rocca P. Role of 3-monthly long-acting injectable paliperidone in the maintenance of schizophrenia. Neuropsychiatr Dis Treat. 2017;13:2767–2779. doi:10.2147/NDT.S150568
10. Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2–3):109–113. doi:10.1016/j.psychres.2009.05.004
11. Kahn RS, Fleischhacker WW, Boter H, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085–1097. doi:10.1016/S0140-6736(08)60486-9
12. Sun SX, Liu GG, Christensen DB, Fu AZ. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin. 2007;23(10):2305–2312. doi:10.1185/030079907X226050
13. Hansen RA, Maciejewski M, Yu-Isenberg K, Farley JF. Adherence to antipsychotics and cardiometabolic medication: association with health care utilization and costs. Psychiatr Serv. 2012;63(9):920–928. doi:10.1176/appi.ps.201100328
14. Altamura AC, Sassella F, Santini A, Montresor C, Fumagalli S, Mundo E. Intramuscular preparations of antipsychotics: uses and relevance in clinical practice. Drugs. 2003;63(5):493–512. doi:10.2165/00003495-200363050-00004
15. Taylor D. Psychopharmacology and adverse effects of antipsychotic long-acting injections: a review. Br J Psychiatry Suppl. 2009;52:S13–S19. doi:10.1192/bjp.195.52.s13
16. McEvoy JP, Byerly M, Hamer RM, et al. Effectiveness of paliperidone palmitate vs haloperidol decanoate for maintenance treatment of schizophrenia: a randomized clinical trial. JAMA. 2014;311(19):1978–1987. doi:10.1001/jama.2014.4310
17. Rauch AS, Fleischhacker WW. Long-acting injectable formulations of new-generation antipsychotics: a review from a clinical perspective. CNS Drugs. 2013;27(8):637–652. doi:10.1007/s40263-013-0083-9
18. Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry. 2021;8(5):387–404. doi:10.1016/S2215-0366(21)00039-0
19. Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr Res. 2018;197:274–280. doi:10.1016/j.schres.2017.12.010
20. Florida best practice psychotherapeutic medication guidelines for adults. The University of South Florida, Florida Medicaid drug therapy management program. Available from: https://floridabhcenter.org/wp-content/uploads/2021/04/2019-Psychotherapeutic-Medication-Guidelines-for-Adults-with-References_06-04-20.pdf.
21. Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830–839. doi:10.1001/jamapsychiatry.2015.0241
22. Gopal S, Hough DW, Xu H, et al. Efficacy and safety of paliperidone palmitate in adult patients with acutely symptomatic schizophrenia: a randomized, double-blind, placebo-controlled, dose-response study. Int Clin Psychopharmacol. 2010;25(5):247–256. doi:10.1097/YIC.0b013e32833948fa
23. Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M, Hough D. A 52-week open-label study of the safety and tolerability of paliperidone palmitate in patients with schizophrenia. J Psychopharmacol. 2011;25(5):685–697. doi:10.1177/0269881110372817
24. Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. doi:10.1016/j.schres.2009.10.026
25. Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority study. Int J Neuropsychopharmacol. 2016;19(7):pyw018. doi:10.1093/ijnp/pyw018
26. Garcia-Portilla MP, Llorca PM, Maina G, et al. Symptomatic and functional outcomes after treatment with paliperidone palmitate 3-month formulation for 52 weeks in patients with clinically stable schizophrenia. Ther Adv Psychopharmacol. 2020;10:2045125320926347. doi:10.1177/2045125320926347
27. Di Lorenzo R, Cameli M, Piemonte C, et al. Clinical improvement, relapse and treatment adherence with paliperidone palmitate 1-month formulation: 1-year treatment in a naturalistic outpatient setting. Nord J Psychiatry. 2018;72(3):214–220. doi:10.1080/08039488.2017.1420819
28. Attard A, Olofinjana O, Cornelius V, Curtis V, Taylor D. Paliperidone palmitate long-acting injection--prospective year-long follow-up of use in clinical practice. Acta Psychiatr Scand. 2014;130(1):46–51. doi:10.1111/acps.12201
29. Bioque M, Bernardo M. The current data on the 3-month paliperidone palmitate formulation for the treatment of schizophrenia. Expert Opin Pharmacother. 2018;19(14):1623–1629. doi:10.1080/14656566.2018.1515915
30. Mathews M, Gopal S, Nuamah I, et al. Clinical relevance of paliperidone palmitate 3-monthly in treating schizophrenia. Neuropsychiatr Dis Treat. 2019;15:1365–1379. doi:10.2147/NDT.S197225
31. Chue P, Eerdekens M, Augustyns I, et al. Comparative efficacy and safety of long-acting risperidone and risperidone oral tablets. Eur Neuropsychopharmacol. 2005;15(1):111–117. doi:10.1016/j.euroneuro.2004.07.003
32. Glick ID, Marder SR. Long-term maintenance therapy with quetiapine versus haloperidol decanoate in patients with schizophrenia or schizoaffective disorder. J Clin Psychiatry. 2005;66(5):638–641. doi:10.4088/jcp.v66n0515
33. Kane JM, Detke HC, Naber D, et al. Olanzapine long-acting injection: a 24-week, randomized, double-blind trial of maintenance treatment in patients with schizophrenia. Am J Psychiatry. 2010;167(2):181–189. doi:10.1176/appi.ajp.2009.07081221
34. Lauriello J, Lambert T, Andersen S, Lin D, Taylor CC, McDonnell D. An 8-week, double-blind, randomized, placebo-controlled study of olanzapine long-acting injection in acutely ill patients with schizophrenia. J Clin Psychiatry. 2008;69(5):790–799. doi:10.4088/jcp.v69n0512
35. Meltzer HY, Risinger R, Nasrallah HA, et al. A randomized, double-blind, placebo-controlled trial of aripiprazole lauroxil in acute exacerbation of schizophrenia. J Clin Psychiatry. 2015;76(8):1085–1090. doi:10.4088/JCP.14m09741
36. Rifkin A, Quitkin F, Rabiner CJ, Klein DF. Fluphenazine decanoate, fluphenazine hydrochloride given orally, and placebo in remitted schizophrenics. I. Relapse rates after one year. Arch Gen Psychiatry. 1977;34(1):43–47. doi:10.1001/archpsyc.1977.01770130045004
37. Schooler NR, Levine J, Severe JB, et al. Prevention of relapse in schizophrenia. An evaluation of fluphenazine decanoate. Arch Gen Psychiatry. 1980;37(1):16–24. doi:10.1001/archpsyc.1980.01780140018002
38. Garcia-Portilla MP, Benito Ruiz A, Gomez Robina F, Garcia Dorado M, Lopez Rengel PM. Impact on functionality of the paliperidone palmitate three-month formulation in patients with a recent diagnosis of schizophrenia: a real-world observational prospective study. Expert Opin Pharmacother. 2022;23(5):629–638. doi:10.1080/14656566.2021.2023496
39. Sajatovic M, Ross R, Legacy SN, et al. Initiating/maintaining long-acting injectable antipsychotics in schizophrenia/schizoaffective or bipolar disorder - expert consensus survey part 2. Neuropsychiatr Dis Treat. 2018;14:1475–1492. doi:10.2147/NDT.S167485
40. Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi:10.1016/S2215-0366(20)30307-2
41. Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. doi:10.4088/jcp.v63n1007
42. Najarian D, Sanga P, Wang S, et al. A randomized, double-blind, multicenter, noninferiority study comparing paliperidone palmitate 6-month versus the 3-month long-acting injectable in patients with schizophrenia. Int J Neuropsychopharmacol. 2021. doi:10.1093/ijnp/pyab071
43. Lin D, Thompson-Leduc P, Ghelerter I, et al. Correction to: real-world evidence of the clinical and economic impact of long-acting injectable versus oral antipsychotics among patients with schizophrenia in the United States: a systematic review and meta-analysis. CNS Drugs. 2021;35(8):923. doi:10.1007/s40263-021-00850-9
44. Yan T, Greene M, Chang E, Hartry A, Touya M, Broder MS. Medication adherence and discontinuation of aripiprazole once-monthly 400 mg (AOM 400) versus oral antipsychotics in patients with schizophrenia or bipolar i disorder: a real-world study using US claims data. Adv Ther. 2018;35(10):1612–1625. doi:10.1007/s12325-018-0785-y
45. Kane JM, Sanchez R, Zhao J, et al. Hospitalisation rates in patients switched from oral anti-psychotics to aripiprazole once-monthly for the management of schizophrenia. J Med Econ. 2013;16(7):917–925. doi:10.3111/13696998.2013.804411
46. Pilon D, Tandon N, Lafeuille MH, et al. Treatment patterns, health care resource utilization, and spending in Medicaid beneficiaries initiating second-generation long-acting injectable agents versus oral atypical antipsychotics. Clin Ther. 2017;39(10):1972–1985 e2. doi:10.1016/j.clinthera.2017.08.008
47. Alphs L, Mao L, Lynn Starr H, Benson C. A pragmatic analysis comparing once-monthly paliperidone palmitate versus daily oral antipsychotic treatment in patients with schizophrenia. Schizophr Res. 2016;170(2–3):259–264. doi:10.1016/j.schres.2015.12.012
48. Patel C, Emond B, Morrison L, et al. Risk of subsequent relapses and corresponding healthcare costs among recently-relapsed Medicaid patients with schizophrenia: a real-world retrospective cohort study. Curr Med Res Opin. 2021;37(4):665–674. doi:10.1080/03007995.2021.1882977
49. Zhdanava M, Lin D, Lafeuille MH, et al. Antipsychotic adherence, resource use, and costs before and after the initiation of once-monthly paliperidone palmitate therapy among Medicaid beneficiaries with prior schizophrenia relapse. Clin Ther. 2021;43(3):535–548. doi:10.1016/j.clinthera.2021.01.011
50. Patel C, Emond B, Lafeuille MH, et al. Real-world analysis of switching patients with schizophrenia from oral risperidone or oral paliperidone to once-monthly paliperidone palmitate. Drugs Real World Outcomes. 2020;7(1):19–29. doi:10.1007/s40801-019-00172-9
51. Emond B, El Khoury AC, Patel C, et al. Real-world outcomes post-transition to once-every-3-months paliperidone palmitate in patients with schizophrenia within US commercial plans. Curr Med Res Opin. 2019;35(3):407–416. doi:10.1080/03007995.2018.1560220
52. Mahabaleshwarkar R, Lin D, Fishman J, et al. The impact of once-monthly paliperidone palmitate on healthcare utilization among patients with schizophrenia treated in an integrated healthcare system: a retrospective mirror-image study. Adv Ther. 2021;38(4):1958–1974. doi:10.1007/s12325-021-01626-9
53. Joshi K, Lafeuille MH, Brown B, et al. Baseline characteristics and treatment patterns of patients with schizophrenia initiated on once-every-three-months paliperidone palmitate in a real-world setting. Curr Med Res Opin. 2017;33(10):1763–1772. doi:10.1080/03007995.2017.1359516
54. DerSarkissian M, Lefebvre P, Joshi K, et al. Health care resource utilization and costs associated with transitioning to 3-month paliperidone palmitate among US veterans. Clin Ther. 2018;40(9):1496–1508. doi:10.1016/j.clinthera.2018.07.011
55. Lin D, Pilon D, Zhdanava M, et al. Medication adherence, healthcare resource utilization, and costs among Medicaid beneficiaries with schizophrenia treated with once-monthly paliperidone palmitate or once-every-three-months paliperidone palmitate. Curr Med Res Opin. 2021;37(4):675–683. doi:10.1080/03007995.2021.1882412
56. Weiden PJ, Kim E, Bermak J, Turkoz I, Gopal S, Berwaerts J Does Half-Life Matter After Antipsychotic Discontinuation? A Relapse Comparison in Schizophrenia with 3 Different Formulations of Paliperidone. J Clin Psychiatry. 2017 Jul;78(7):e813–820. doi: 10.4088/JCP.16m11308.
57. Farley JF, Hansen RA, Yu-Isenberg KS, Maciejewski ML. Antipsychotic adherence and its correlation to health outcomes for chronic comorbid conditions. Prim Care Companion CNS Disord. 2012;14(3). doi:10.4088/PCC.11m01324
58. Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–2948. doi:10.1093/eurheartj/eht295
59. Solmi M, Tiihonen J, Lahteenvuo M, Tanskanen A, Correll CU, Taipale H. Antipsychotics use is associated with greater adherence to cardiometabolic medications in patients with schizophrenia: results from a nationwide, within-subject design study. Schizophr Bull. 2022;48(1):166–175. doi:10.1093/schbul/sbab087
60. Takacs P, Czobor P, Feher L, et al. Comparative effectiveness of second generation long-acting injectable antipsychotics based on nationwide database research in Hungary. PLoS One. 2019;14(6):e0218071. doi:10.1371/journal.pone.0218071
61. Mason K, Barnett J, Pappa S. Effectiveness of 2-year treatment with aripiprazole long-acting injectable and comparison with paliperidone palmitate. Ther Adv Psychopharmacol. 2021;11:20451253211029490. doi:10.1177/20451253211029490
62. Wallman P, Clark I, Taylor D. Effect of 3-monthly paliperidone palmitate on hospitalisation in a naturalistic schizophrenia cohort - A five-year mirror image study. J Psychiatr Res. 2022;148:131–136. doi:10.1016/j.jpsychires.2022.01.044
63. Garcia-Carmona JA, Simal-Aguado J, Campos-Navarro MP, Valdivia-Munoz F, Galindo-Tovar A. Evaluation of long-acting injectable antipsychotics with the corresponding oral formulation in a cohort of patients with schizophrenia: a real-world study in Spain. Int Clin Psychopharmacol. 2021;36(1):18–24. doi:10.1097/YIC.0000000000000339
64. Pilon D, Alcusky M, Xiao Y, et al. Adherence, persistence, and inpatient utilization among adult schizophrenia patients using once-monthly versus twice-monthly long-acting atypical antipsychotics. J Med Econ. 2018;21(2):135–143. doi:10.1080/13696998.2017.1379413
65. Joshi K, Pan X, Wang R, Yang E, Benson C. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin. 2016;32(11):1873–1881. doi:10.1080/03007995.2016.1219706
66. Joo SW, Shon SH, Choi G, Koh M, Cho SW, Lee J. Continuation of schizophrenia treatment with three long-acting injectable antipsychotics in South Korea: a nationwide population-based study. Eur Neuropsychopharmacol. 2019;29(9):1051–1060. doi:10.1016/j.euroneuro.2019.07.138
67. Hard ML, Mills RJ, Sadler BM, Wehr AY, Weiden PJ, von Moltke L. Pharmacokinetic profile of a 2-month dose regimen of aripiprazole lauroxil: a phase I study and a population pharmacokinetic model. CNS Drugs. 2017;31(7):617–624. doi:10.1007/s40263-017-0447-7
68. Weiden PJ, Du Y, von Moltke L, et al. Pharmacokinetics, safety, and tolerability of a 2-month dose interval regimen of the long-acting injectable antipsychotic aripiprazole lauroxil: results from a 44-week phase I study. CNS Drugs. 2020;34(9):961–972. doi:10.1007/s40263-020-00745-1
69. Detke HC, Weiden PJ, Llorca PM, et al. Comparison of olanzapine long-acting injection and oral olanzapine: a 2-year, randomized, open-label study in outpatients with schizophrenia. J Clin Psychopharmacol. 2014;34(4):426–434. doi:10.1097/JCP.0000000000000140
70. Schneider-Thoma J, Chalkou K, Dorries C, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta-analysis. Lancet. 2022;399(10327):824–836. doi:10.1016/S0140-6736(21)01997-8
71. Mathews M, Gopal S, Singh A, et al. Comparison of relapse prevention with 3 different paliperidone formulations in patients with schizophrenia continuing versus discontinuing active antipsychotic treatment: a post-hoc analysis of 3 similarly designed randomized studies. Neuropsychiatr Dis Treat. 2020;16:1533–1542. doi:10.2147/NDT.S221242
72. Pietrini F, Albert U, Ballerini A, et al. The modern perspective for long-acting injectables antipsychotics in the patient-centered care of schizophrenia. Neuropsychiatr Dis Treat. 2019;15:1045–1060. doi:10.2147/NDT.S199048
73. Pungor K, Sanchez P, Pappa S, et al. The Patient, Investigator, Nurse, Carer Questionnaire (PINC-Q): a cross-sectional, retrospective, non-interventional study exploring the impact of less frequent medication administration with paliperidone palmitate 3-monthly as maintenance treatment for schizophrenia. BMC Psychiatry. 2021;21(1):300. doi:10.1186/s12888-021-03305-z
74. Bartzokis G, Lu PH, Amar CP, et al. Long acting injection versus oral risperidone in first-episode schizophrenia: differential impact on white matter myelination trajectory. Schizophr Res. 2011;132(1):35–41. doi:10.1016/j.schres.2011.06.029
75. Bartzokis G, Lu PH, Raven EP, et al. Impact on intracortical myelination trajectory of long acting injection versus oral risperidone in first-episode schizophrenia. Schizophr Res. 2012;140(1–3):122–128. doi:10.1016/j.schres.2012.06.036
76. Munday J, Greene M, Chang E, Hartry A, Yan T, Broder MS. Early initiation of long-acting injectable antipsychotic treatment is associated with lower hospitalization rates and healthcare costs in patients with schizophrenia: real-world evidence from US claims data. Curr Med Res Opin. 2019;35(7):1231–1239. doi:10.1080/03007995.2019.1571295
77. Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–609. doi:10.1176/appi.ajp.2011.10081224
78. Willis M, Svensson M, Lothgren M, Eriksson B, Berntsson A, Persson U. The impact on schizophrenia-related hospital utilization and costs of switching to long-acting risperidone injections in Sweden. Eur J Health Econ. 2010;11(6):585–594. doi:10.1007/s10198-009-0215-9
79. Greenberg G, Rosenheck RA, Erickson SK, et al. Criminal justice system involvement among people with schizophrenia. Community Ment Health J. 2011;47(6):727–736. doi:10.1007/s10597-010-9362-9
80. Teplin LA. The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. Am J Public Health. 1990;80(6):663–669. doi:10.2105/ajph.80.6.663
81. Fazel S, Yu R. Psychotic disorders and repeat offending: systematic review and meta-analysis. Schizophr Bull. 2011;37(4):800–810. doi:10.1093/schbul/sbp135
82. Sajatovic M, Ramirez LF, Fuentes-Casiano E, et al. A 6-month prospective trial of a personalized behavioral intervention + long-acting injectable antipsychotic in individuals with schizophrenia at risk of treatment nonadherence and homelessness. J Clin Psychopharmacol. 2017;37(6):702–707. doi:10.1097/JCP.0000000000000778
83. Alphs L, Benson C, Cheshire-Kinney K, et al. Real-world outcomes of paliperidone palmitate compared to daily oral antipsychotic therapy in schizophrenia: a randomized, open-label, review board-blinded 15-month study. J Clin Psychiatry. 2015;76(5):554–561. doi:10.4088/JCP.14m09584
84. Bhatta MP, Bista S, El Khoury AC, Hutzell EG, Tandon N, Smith D. Long-acting injectable antipsychotic use in patients with schizophrenia and criminal justice system encounters. J Health Econ Outcomes Res. 2021;8(1):63–70. doi:10.36469/jheor.2021.22979
85. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370–376. doi:10.1176/appi.ajp.162.2.370
86. Young-Xu Y, Duh MS, Muser E, et al. Impact of paliperidone palmitate versus oral atypical antipsychotics on health care resource use and costs in veterans with schizophrenia. J Clin Psychiatry. 2016;77(10):e1332–e1341. doi:10.4088/JCP.16m10745
87. Yoshimatsu K, Elser A, Thomas M, et al. Recovery-oriented outcomes associated with long-acting injectable antipsychotics in an urban safety-net population. Commun Ment Health J. 2019;55(6):979–982. doi:10.1007/s10597-019-00412-w
88. Citrome L, Belcher E, Stacy S, Suett M, Mychaskiw M, Salinas GD. Perceived burdens and educational needs of caregivers of people with schizophrenia: results of a national survey study. Patient Prefer Adherence. 2022;16:159–168. doi:10.2147/PPA.S326290
89. Gopal S, Xu H, McQuarrie K, et al. Caregiver burden in schizophrenia following paliperidone palmitate long acting injectables treatment: pooled analysis of two double-blind randomized phase three studies. NPJ Schizophr. 2017;3(1):23. doi:10.1038/s41537-017-0025-5
90. Lencer R, Garcia-Portilla MP, Bergmans P, et al. Impact on carer burden when stable patients with schizophrenia transitioned from 1-monthly to 3-monthly paliperidone palmitate. Compr Psychiatry. 2021;107:152233. doi:10.1016/j.comppsych.2021.152233
91. Zhao J, Li L, Shi J, et al. Safety and efficacy of paliperidone palmitate 1-month formulation in Chinese patients with schizophrenia: a 25-week, open-label, multicenter, phase IV study. Neuropsychiatr Dis Treat. 2017;13:2045–2056. doi:10.2147/NDT.S131224
92. Srihari G, Haiyan X, Adam S, et al. PM511. determinants of caregiver burden in family carers of asian patients with schizophrenia treated with paliperidone palmitate 3-monthly injectable. Int J Neuropsychopharmacol. 2016;19(Suppl_1):85–86. doi:10.1093/ijnp/pyw041.511
93. SMI-Adviser. Serious Mental Illness Adviser. What are clinical considerations for giving LAIs during the COVID-19 public health emergency? American Psychiatric Association. Available from: https://smiadviser.org/knowledge_post/what-are-clinical-considerations-for-giving-lais-during-The-covid-19-public-health-emergency.
94. Gannon JM, Conlogue J, Sherwood R, et al. Long acting injectable antipsychotic medications: ensuring care continuity during the COVID-19 pandemic restrictions. Schizophr Res. 2020;222:532–533. doi:10.1016/j.schres.2020.05.001
95. Ifteni P, Dima L, Teodorescu A. Long-acting injectable antipsychotics treatment during COVID-19 pandemic - A new challenge. Schizophr Res. 2020;220:265–266. doi:10.1016/j.schres.2020.04.030
96. North Carolina Psychiatric Association. Position statement on long acting injectables. Available from: https://www.psychiatry.org/File%20Library/Psychiatrists/APA-Guidance-Long-Acting-Injectables-COVID-19.pdf.
97. Correll CU, Chepke C, Gionfriddo P, et al. The post COVID-19 healthcare landscape and the use of long-acting injectable antipsychotics for individuals with schizophrenia and bipolar I disorder: the importance of an integrated collaborative-care approach. BMC Psychiatry. 2022;22(1):32. doi:10.1186/s12888-022-03685-w
98. Kirschner M, Theodoridou A, Fusar-Poli P, Kaiser S, Jager M. Patients’ and clinicians’ attitude towards long-acting depot antipsychotics in subjects with a first episode of psychosis. Ther Adv Psychopharmacol. 2013;3(2):89–99. doi:10.1177/2045125312464106
99. Kane JM, McEvoy JP, Correll CU, Llorca PM. Controversies surrounding the use of long-acting injectable antipsychotic medications for the treatment of patients with schizophrenia. CNS Drugs. 2021;35(11):1189–1205. doi:10.1007/s40263-021-00861-6
100. De Risio A, Lang AP. History and therapeutic rationale of long acting antipsychotics. Curr Clin Pharmacol. 2014;9(1):39–52. doi:10.2174/15748847113089990057
101. Waddell L, Taylor M. Attitudes of patients and mental health staff to antipsychotic long-acting injections: systematic review. Br J Psychiatry Suppl. 2009;195:S43–50. doi:10.1192/bjp.195.52.s43
102. Blackwood C, Sanga P, Nuamah I, et al. Patients’ preference for long-acting injectable versus oral antipsychotics in schizophrenia: results from the patient-reported medication preference questionnaire. Patient Prefer Adherence. 2020;14:1093–1102. doi:10.2147/PPA.S251812
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.