Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
The Effect of Eye Movement Desensitization and Reprocessing (EMDR) on the severity of suicidal thoughts in patients with major depressive disorder: a randomized controlled trial
Authors Fereidouni Z , Behnammoghadam M, Jahanfar A , Dehghan A
Received 1 April 2019
Accepted for publication 12 August 2019
Published 27 August 2019 Volume 2019:15 Pages 2459—2466
DOI https://doi.org/10.2147/NDT.S210757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Zhila Fereidouni,1 Mohammad Behnammoghadam,2 Abdolhadi Jahanfar,1 Azizallah Dehghan3
1Department of Medical Surgical Nursing, Nursing School, Fasa University of Medical Sciences, Fasa, Iran; 2Department of Critical Care Nursing, Yasuj University of Medical Sciences, Yasuj, Iran; 3Noncommunicable Diseases Research Center, Fasa University of Medical Sciences, Fasa, Iran
Correspondence: Abdolhadi Jahanfar
Department of Medical Surgical Nursing, Nursing School, Fasa University of Medical Sciences, Fasa Ibn Sina Square, PO Box 7461686688, Fasa, Iran
Email [email protected]
Mohammad Behnammoghadam
Department of Critical Care Nursing, Yasuj University of Medical Sciences, Yasuj, Iran
Email [email protected]
Objective: Depression is a major risk factor for suicide and more than 90% of people who attempt suicide suffer from depression. The present study aimed to investigate the effect of eye movement desensitization and reprocessing (EMDR) therapy on the severity of suicidal thoughts in patients with major depressive disorder.
Study design: Randomized Clinical Trial.
Methods: This clinical trial was performed on 70 people with major depressive disorder who exhibited suicidal thoughts. The patients were selected via convenience sampling and were randomly divided into control (n=35) and experimental (n=35) groups. EMDR was performed individually in the experimental group for 45–90 min, 3 days per week, on alternate days, for 3 weeks (9 sessions in total), whereas the controls group received routine treatment without intervention. Both groups completed the Beck Scale for Suicide Ideation (BSSI) at pre- and post-test. The obtained data were analyzed with descriptive and inferential statistics using SPSS 22 (α=0.05).
Results: Mean BSSI score for the experimental group was reduced significantly at post-test (11.11±4.15) compared to pre-test (26.48±5.74) (p<0.001). Although the control group’s mean BSSI score was also reduced at post-test (24.93±4.42) compared to pre-test (26.68±5.05), this difference was not statistically significant (p>0.05).
Conclusion: EMDR therapy has been shown in this study to reduce the severity of suicidal feelings. Therefore, it can be recommended as an alternative treatment method for reducing the severity of suicidal thoughts in patients with major depressive disorder.
Keywords: major depressive disorder, suicidal thoughts, eye movement desensitization and reprocessing
Introduction
Major depressive disorder is a highly prevalent psychiatric illness. Along with multiple symptoms, this disorder is associated with recurrent thoughts of death or suicide.1,2 The prevalence of MDD differs among countries; the estimated lifetime prevalence of major depressive episodes was 1.5% in Taiwan, 7% in Korea, 19.0% in Lebanon, 9.2% in Germany, and 9.0% in Chile.3 The global prevalence of major depressive disorder is generally estimated to be between 3% and 6%.4 There is no accurate estimation about major depression in the Iranian population, but according to the results of a systematic review conducted in Iran, the MMD prevalence was 4.1%.5,6
Depression is one of the main risk factors for suicide in that more than 90% of people who commit suicide experience depression.7,8 Suicide is the process of deliberately ending one’s own life. Patients with depression are 20 times more likely to commit suicide than the general population.9 Furthermore, thoughts of suicide are a frequent and potentially dangerous indication of psychiatric emergencies.10 This is because a period of suicidal ideation often precedes suicidal behaviours or suicide attempts.11Suicidal thoughts are often related to childhood traumatic memories.12Suicide is a global health concern that affects more than one million people per year, which is compounded by the fact that approximately one quarter of people with suicidal thoughts and suicide attempts do not have access to mental health services.13 Furthermore, it is known that suicidal thoughts are relatively common experiences as nearly 9% of people experience suicidal thoughts during their lifetime.14 In addition, the rate of suicide in the past decade has increased by more than 16% in the United States, indicating the limited impacts of current preventive strategies.15
Iran has witnessed a high increase in suicide-related mortality reaching 4.7 per 100,000 in 2015.16
In clinical settings, patient reports of suicidal thoughts are often the only observable sign of suicide risk and, where the severity of suicidal thoughts are high, there is a greater probability of their translation into action. Therefore, suicidal thoughts are of clinical importance and can be used to assess the risk of suicidal behaviour. In this regard, the prevention of suicide behaviours in patients requires the identification and amelioration of suicidal thoughts.17,18 Since half of those who have committed suicide meet the diagnostic criteria for a concurrent depressive episode, diagnosis and treatment of depression is important in preventing suicide.19
Depression and suicidal thoughts can be treated both pharmacologically and non-pharmacologically. Although patients are often initially treated pharmacologically, about 20% of patients do not adhere to medication and many others simply do not complete the course.20 Certain antidepressants, such as serotonin reuptake inhibitors, which are used to treat depression and suicidal ideation are associated with side effects and may even increase suicidal thoughts and behaviors. The presenting symptoms may also recur after discontinuation of these drugs, therefore the Food and Drug Administration has warned physicians about their use.21
Given the risk of side effects, dependence, intolerability, and high costs of pharmaceutical options, non-pharmacological methods of suicidal ideation treatment in patients with depression garnered clinical research attention. These emphasize the use of cheap, non-invasive, and adverse effect-free approaches. There is evidence to suggest that psychiatric patients often prefer cognitive and behavioral therapies to pharmacological treatment.22
Eye movement desensitization and reprocessing (EMDR) therapy is an empirically validated trauma intervention which can be effective in treating suicidal thoughts.23 EMDR, first introduced in 1989 by psychologist Francine Shapiro, is a specialized, low-cost treatment to overcome the effects of emotional shock and distressing experiences. This approach involves reprocessing the past stressful events and replacing the negative beliefs with positive and informed ones chosen by the person himself.24 In this approach, using standardized procedures, the therapist asks patients to remember the distressing memories for short periods of time while moving their eyes, so that the level of stimulation is reduced and the thoughts are reorganized.25
Many patients with major depressive disorder experience suicidal thoughts, leading to delayed return to work, reduced quality of life,26 and increased risk of suicide and death.27 However, treatment of depression and reduction of suicidal ideation can accelerate recovery, increase quality of life.28,29 and reduce economic burden. EMDR has been widely researched for the treatment of PTSD23 but there are few studies evaluating the treatment of suicidal thoughts in patients with major depression. The present clinical trial aims to rigorously determine the effect of EMDR on the severity of suicidal thoughts in patients with major depressive disorder.
Materials and methods
This study was conducted from 2017 to 2018 in Shahid Rajaee Neurology Hospital of Yasuj, Iran on patients diagnosed with major depressive disorder. Using confidence level of 95%, a statistical power of 80%, and minimum clinically significant difference 5% as well as the standard deviation of the effect of EMDR in the Kikhavani et al study, a sample size of 31 was calculated for each group which was raised to 35 people considering the possibility of attrition. The study was launched after obtaining permission from the Fassa Medical University’s Ethics Committee (Ethics number: REC.1396.280.IR.FUMS) and registering it in Iran Clinical Trial Center (Registration number: IRCT20171231038152N1).
After a complete explanation of the study objectives and obtaining written informed consent, this study was conducted in accordance with the Declaration of Helsinki, seventy in-patients with major depressive disorder reporting suicidal thoughts were included in the study via convenience sampling, and were divided into two groups; experimental (n=35) and control (n=35). The samples were randomly based on parall and random allocation of block randomization (noted in Figure 1).
 |
Figure 1 Consort flow diagram. |
Inclusion criteria were the diagnosis of major depressive disorder by a psychiatrist (based on DSM-5 criteria), and self-reported suicidal thoughts (scores high than sex) and no previous history of suicide attempts, seizures, strabismus, or other vision problems. Exclusion criteria were intolerance to the treatment method, referral to other treatment centers. The data were collected using a self-report demographic questionnaire and the Beck Scale for Suicide Ideation (BSSI).
Demographic questionnaire
This self-report demographic questionnaire included items assessing age, gender, marital status, education, economic status, occupation, and family history of depressive disorder.
Beck scale for suicide ideation (BSSI)
The BSSI, which is used to assess the severity of suicidal thoughts, is a 19-item self-report questionnaire.30 It was developed to quantify the severity of attitudes, behaviors, and plans to commit suicide within the past week. Answers to items on the scale are based on three points from 0 to 2. The total score is calculated by summing the items’ scores resulting in an overall score from 0 to 38.31 Higher scores indicate higher severity of suicidal feelings.32 BSSI has a strong reliability and validity.32,33 Cronbach’s alpha coefficients ranged from 0.87 to 0.97 and test-retest reliability co-efficient has been assessed at 0.54.34
Procedure
EMDR was performed individually in the experimental group for 45–90 mins, three days per week, on alternate days, for three weeks (nine sessions in total). The severity of suicidal thoughts was measured before the first and after the final session with the BSSI. Safety conditions (presence of a companion, informing the department nurses, safety of the treatment room) were considered for patients and the researcher prior to intervention. To perform the intervention in the experimental group, the researcher first introduced the patients to EMDR and established rapport with them before recruiting them to participate in the study.
Shapiro (2014) described EMDR as a multidimensional approach that includes eight stages.
In the first stage, a patient history of their trauma and suicidal thoughts was taken.23 The second stage involved explaining EMDR’s process and effects, a description of treatment expectations, and preparation of patients for treatment. In the third stage, the memories, images, symbols, the most disturbing visual image related to suicidal thoughts, patient beliefs about the event, and physical sensations relating to post-event beliefs were identified and a positive belief was identified to replace the previous negative cognition.25 During this phase, the patient’s subjective units of distress (SUDs) in relation to subjective experiences around suicidal thoughts are high. The fourth stage involved asking the patient to focus on a specific negative belief while tracking the therapist’s fingertip in a series of 12–24 sets of horizontal eye movements until the self-reported SUDs reached zero (or an acceptable minimum).35 In the fifth stage, horizontal eye movements continued to be administered while the patient focused on a specific positive belief until it reached a maximum level of endorsement. In the sixth stage, horizontal eye movements were administered while the patient was asked to focus on any remaining discomfort or physical pressures until their reduction and disappearance was observed.36 In the seventh stage, the patient was asked to state any disturbing images, thoughts, or emotions experienced during the treatment, and preparations were made to ensure the patient’s emotional stability for the completion of the treatment session.37 In the eighth stage, the patient began a new EMDR session by focusing on previously processed goals and re-evaluating the extent to which therapeutic goals have been achieved.
After each set, the therapist asked patients to stop visualizing the scene, lean back into their chair and breathe deeply. The process was repeated according to the requirements and the patient’s level of motivation so that the levels of mental discomfort units reached zero or minimize.
No intervention was performed by the researcher in the control group. Usual treatment in both groups was only pharmacological treatment such as Fluoxetine, Amitriptyline and Maprotiline.
All patients were treated with antidepressants, and were not taking drugs with anti-suicidal effects, such as lithium.
In the control group, the demographic questionnaire and the BSSI were administered at the beginning of the first session and at the end of the third week. The experimental and control group received no other therapy during the period. The data were analyzed using descriptive and inferential statistics tests with SPSS version 22, using a confidence level of 95%. After normality assumptions were satisfied for BSSI scores, independent sample t-test was used for intergroup comparisons and paired t-test was used for intragroup comparisons.
Results
Scores from the demographic questionnaire indicated that the patients’ mean age was 35.94±12.29 years in the experimental group and 36.51±11.07 years in the control group. The minimum and maximum ages of participants in this study were 19 and 63 years, respectively. No significant differences were found between the experimental and control groups in terms of age by using independent sample t test, indicating that both groups were age-equivalent.
Eighty percent of patients had trauma only once and the rest had trauma more than once.
Sixty percent of traumas were related to adulthood and for some reason such as grief, divorce, physical and sexual abuse
Twenty five percent of traumas were in both childhood and adulthood and the rest was only for a childhood
Similarly, chi-squared tests found no statistically significant differences between the groups in terms of gender, education, marital status, family history of major depressive disorder, economic status, or employment status (p>0.05; Table 1). Hence, it can be said that no systematic differences were observed between the experimental versus control groups for these demographic variables.
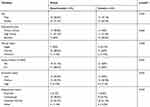 |
Table 1 Comparison of the demographic characteristics of the participants in the experimental and control group |
Table 2, shows the results of the analyses conducted on BSSI scores. Mean BSSI scores were quite similar to each other at pre-test. This observation was supported by an independent t-test which showed no statistically significant differences between groups as detected in the pre-test, indicating that groups were relatively equivalent in terms of the severity of their suicidal thoughts before the intervention. At post-test, the drop in severity of suicidal thoughts was greater in the experimental group compared to the control group. A second independent t-test found this post-test difference in BSSI mean scores to be statistically significant, indicating that the groups were no longer equivalent in terms of severity of suicidal thoughts at post-test. To further investigate this, two paired t-tests were conducted on the pre- versus post-test BSSI mean scores for the experimental and control groups, respectively. These found a statistically significant change in BSSI scores for the experimental group, which was not observed in the control group.
 |
Table 2 Between- and within-groups comparisonof mean scores (standard deviation in brackets) of the experimental and control groups at pre- and post-test for the BSSI |
Discussion
The present study aimed to investigate efficacy eye movement desensitization and reprocessing therapy on the severity of suicidal ideation in patients with major depressive disorder. To the author’s knowledge, this study is the first randomized clinical trial using EMDR therapy to treat suicidal ideation in patients with major depressive disorder.
The results show that the severity of suicidal thoughts for the control group remained unchanged with treatment as usual, whereas the experimental group experienced an observable improvement in scores from EMDR.
In all patients, the causes of Suicidal thoughts were often related to childhood traumatic memories (such as: sexual and physical abuse, grief and loss of parents).
The results showed that, compared to usual treatment, EMDR could be an appropriate first-line therapy to rapidly reduce the severity of suicidal thoughts in patients with major depressive disorder. This conclusion is based on the paired t-tests which demonstrated an observable improvement in the severity of suicidal ideation after EMDR, which was not observed in the group which received usual treatment. Furthermore, independent t-tests found that the group that had benefited from EMDR showed lower suicidal ideation after treatment compared to usual treatment which was not observed before each group received its respective intervention. In addition, these differences cannot be accounted for by intergroup differences in participant characteristics, as this was ruled out by the analyses on the demographic questionnaire results.
Suicidal thoughts most likely occur due to emotional trauma, and unpleasant experiences (such as suicidal thoughts) are unprocessed and lead to negative beliefs about oneself and others.38 Suicide attempts are likely to be experienced and stored as trauma and may lead to repetitive negative cognitions of unpleasant events resulting in the increased probability of committing suicide.11 The processing of distressing memories using EMDR dramatically reduces the mental discomfort associated with them, thereby decreasing the experience of suicidal thoughts as a coping strategy.37 In addition, patients gain hopeful and positive insights and attitudes through this therapeutic approach, where negative beliefs and expectations associated with those unpleasant events are replaced with positive cognitions.11
Where other related studies have usually been sparse and in the form of preliminary trials, this study is first attempt to systematically observe the effects of EMDR on suicidal ideation in patients with major depressive disorder in the form of a randomized clinical trial. For example, Tullis et al (2003) in their pilot study used cognitive behavioral therapy (CBT) and EMDR to reduce suicidal thoughts in five survivors of childhood trauma. They concluded that the combination of EMDR and CBT reduced or eliminated suicidal thoughts in patients. Although the findings of this study were in line with our results, its small sample size and lack of a control group permits little in the way of confidence.11 Similarly, in a case study on an 18-year-old woman with multiple years of self-harm conducted by Derek et al (2008) showed that after 2 sessions of treatment with EMDR, self-harm thoughts decreased with no traces of self-harm being observed at a 13-month follow up. The rapid reduction of distressing thoughts observed here supports the results of our study, even if the case study format makes it difficult to compare or generalize findings.39 The results of Yasmeen’s study (2016) into the effect of EMDR on the treatment of depression showed that this treatment modality is effective in treating depression symptoms in patients with major depressive disorder, and can improve the quality of life and eliminate unpleasant thoughts. Intuitively, by treating major depression in these patients, the probability of suicidal thoughts (and therefore suicide attempts) will decrease, a hypothesis which would be interesting to investigate in future studies.28 EMDR seems to be a good treatment for reducing or eliminating unpleasant and harmful thoughts.39 This is the explanation that is supported by Shapiro (2014), who states that EMDR can be used as a valid psychotherapy method for the treatment of psychological trauma and negative life experiences. EMDR can quickly treat unprocessed memories and undesirable experiences of life.23
One of the reasons for this research area experiencing a dearth of studies is because EMDR is not typically recommended for suicidal ideation due to the risk of increasing it. In an editorial entitled “Can EMDR be used for those who have suicidal thoughts?” Spectorj and Krermers stated that, this method can be useful in treating suicidal thoughts. Although, issues such as identifying suicidal ideation, therapist safety, and ceasing EMDR when the patient becomes restless must be addressed.40 In this study, much of the risk involved in treating patients with suicidal ideation was greatly mitigated by working with hospital in-patients. We recommend incorporating risk-reduction factors such as these in the designs of future studies in this area.
One of the limitations of the study was that patients in our study were selected using non-random sampling or convenience method due to the limited study population, so random sampling method is impossible.
Another limitation of the study was Axis I comorbidity for PTSD not being included in the list of exclusion criteria.
Conclusion
The results of this clinical trial showed that EMDR can reduce the severity of suicidal thoughts in patients with major depressive disorder and may be used as an effective and complementary treatment for these patients.
Data sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymized data may be granted following review.
Acknowledgments
The authors thank all the patients and Francine Shapiro for the assistance provided with this research. This article is derived from a Master’s Degree in Nursing in the Fassa University of Medical Sciences. The author would like to express his gratitude to the respected Research Deputy of the university who sponsored this thesis. The patients participating in the research are also appreciated.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Health QO. Psychotherapy for major depressive disorder and generalized anxiety disorder. AHealth Technol Assess Ontario Health Technol Assess Ser. 2017;17(15):1.
2. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–3105. doi:10.1001/jama.289.23.3095
3. Han C, Wang SM, Lee SJ, Jun TY, Pae CU. Optimizing the use of aripiprazole augmentation in the treatment of major depressive disorder: from clinical trials to clinical practice. Chonnam Med J. 2015;51(2):66–80. doi:10.4068/cmj.2015.51.2.66
4. Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1):90. doi:10.1186/1741-7015-9-90
5. Sadeghirad B, Haghdoost AA, Amin-Esmaeili M, et al. Epidemiology of major depressive disorder in Iran: a systematic review and meta-analysis. Int J Prev Med. 2010;1(2):81.
6. Sajjadi H, Kamal SHM, Rafiey H, Vameghi M, Forouzan AS, Rezaei M. A systematic review of the prevalence and risk factors of depression among iranian adolescents. Glob J Health Sci. 2013;5(3):16. doi:10.5539/gjhs.v5n3p16
7. Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: a clinical cohort study. Lancet Psychiatry. 2014;1(2):142–147. doi:10.1016/S2215-0366(14)70248-2
8. Reynolds CF
9. Chesney E, Goodwin GM, Fazel S. Risks of all‐cause and suicide mortality in mental disorders: a meta‐review. World Psychiatry. 2014;13(2):153–160. doi:10.1002/wps.20128
10. Ballard ED, Ionescu DF, Voort JLV, et al. Improvement in suicidal ideation after ketamine infusion: relationship to reductions in depression and anxiety. J Psychiatr Res. 2014;58:161–166. doi:10.1016/j.jpsychires.2014.07.027
11. Tullis KF, Westscott CL, Winton TR. 2003. A theory on the use of cognitive behavioral therapy (CBT) plus eye movement desensitization and reprocessing (EMDR) to reduce suicidal thoughts in childhood trauma victims. In: Tullis’s KF, editor. The Courage to Live Workbook. Memphis: KFT Press. Avalaible from: https://emdria.omeka.net/items/show/18283
12. Lopez-Castroman J, Jaussent I, Beziat S, et al. Posttraumatic stress disorder following childhood abuse increases the severity of suicide attempts. J Affect Disord. 2015;170:7–14. doi:10.1016/j.jad.2014.08.010
13. Johnston AK, Pirkis JE, Burgess PM. Suicidal thoughts and behaviours among Australian adults. findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry. 2009;43(7):635–643. doi:10.1177/1073191105274925
14. Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: a meta-analytic review. Clin Psychol Rev. 2016;43:30–46. doi:10.1016/j.cpr.2015.11.008
15. Baker SP, Hu G, Wilcox HC, Baker TD. Increase in suicide by hanging/suffocation in the US, 2000–2010. Am J Prev Med. 2013;44(2):146–149. doi:10.1016/j.amepre.2012.10.010
16. Karamouzian M, Rostami M. Suicide statistics in Iran: let’s get specific. Am J Men’s Health. 2019;13(1):1557988318807079. doi:10.1177/1557988318807079
17. Park S-M, Cho S-i, Moon -S-S. Factors associated with suicidal ideation: role of emotional and instrumental support. J Psychosom Res. 2010;69(4):389–397. doi:10.1016/j.jpsychores.2010.03.002
18. McAuliffe CM. Suicidal ideation as an articulation of intent: a focus for suicide prevention? Arch Suicide Res. 2002;6(4):325–338. doi:10.1080/13811110214524
19. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi:10.1001/archpsyc.56.7.617
20. Amick HR, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015;351:h6019. doi:10.1136/bmj.h6019
21. Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi:10.1001/archpsyc.63.3.332
22. McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs. pharmacological treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595. doi:10.4088/JCP.12r07757
23. Merlis DT. Eye Movement Desensitization and Reprocessing (EMDR) Therapy: Basic Principles, Protocols, and Procedures. Springer; 2018:87–88. doi:10.1891/1933-3196.12.2.87
24. Shapiro F. Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. J Trauma Stress. 1989;2(2):199–223. doi:10.1891/1933-3196.8.4.181
25. Zeighami R, Behnammoghadam M, Moradi M, Bashti S. Comparison of the effect of eye movement desensitization reprocessing and cognitive behavioral therapy on anxiety in patients with myocardial infarction. Eur J Psychiatry. 2018;32(2):72–76. doi:10.1016/j.ejpsy.2017.09.001
26. Gao K, Su M, Sweet J, Calabrese JR. Correlation between depression/anxiety symptom severity and quality of life in patients with major depressive disorder or bipolar disorder. J Affect Disord. 2019;244(1):9–15. doi:10.1016/j.jad.2018.09.063
27. van Spijker BA, van Straten A, Kerkhof AJ, Hoeymans N, Smit F. Disability weights for suicidal thoughts and non-fatal suicide attempts. J Affect Disord. 2011;134(1–3):341–347. doi:10.1016/j.jad.2011.05.020
28. Gauhar YWM. The efficacy of EMDR in the treatment of depression. J EMDR Pract Res. 2016;10(2):59–69. doi:10.1891/1933-3196.10.2.59
29. Solvason H, Husain M, Fitzgerald P, et al. Improvement in quality of life with left prefrontal transcranial magnetic stimulation in patients with pharmacoresistant major depression: acute and six month outcomes. Brain Stimul. 2014;7(2):219–225. doi:10.1016/j.brs.2013.10.008
30. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343. doi:10.1037/0022-006X.47.2.343
31. de Beurs DP, Fokkema M, de Groot MH, de Keijser J, Kerkhof AJ. Longitudinal measurement invariance of the Beck Scale for Suicide Ideation. Psychiatry Res. 2015;225(3):368–373. doi:10.1016/j.psychres.2014.11.075
32. Healy DJ, Barry K, Blow F, Welsh D, Milner KK. Routine use of the Beck Scale for Suicide Ideation in a psychiatric emergency department. Gen Hosp Psychiatry. 2006;28(4):323–329. doi:10.1016/j.genhosppsych.2006.04.003
33. Holden RR, DeLisle MM. Factor analysis of the Beck Scale for Suicide Ideation with female suicide attempters. Assessment. 2005;12(2):231–238. doi:10.1177/1073191105274925
34. Esfahani M, Hashemi Y, Alavi K. Psychometric assessment of beck scale for suicidal ideation (BSSI) in general population in Tehran. Med J Islam Repub Iran. 2015;29:268.
35. Solomon RM, Shapiro F. EMDR and the adaptive information processing modelpotential mechanisms of change. J EMDR Pract Res. 2008;2(4):315–325. doi:10.1891/1933-3196.2.4.315
36. Shapiro F. EMDR therapy humanitarian assistance programs: treating the psychological, physical, and societal effects of adverse experiences worldwide. J EMDR Pract Res. 2014;8(4):181. doi:10.1891/1933-3196.8.4.181
37. Rostaminejad A, Behnammoghadam M, Rostaminejad M, Behnammoghadam Z, Bashti S. Efficacy of eye movement desensitization and reprocessing on the phantom limb pain of patients with amputations within a 24-month follow-up. Int J Rehabil Res. 2017;40(3):209–214. doi:10.1097/MRR.0000000000000227
38. Van der Kolk BA. The body keeps the score: memory and the evolving psychobiology of posttraumatic stress. Harv Rev Psychiatry. 1994;1(5):253–265.
39. McLaughlin DF, McGowan IW, Paterson MC, Miller PW. Cessation of deliberate self harm following eye movement desensitisation and reprocessing: a case report. Cases J. 2008;1(1):177. doi:10.1186/1757-1626-1-177
40. Spector J, Kremer S. Can I use EMDR with clients who report suicidal ideation? J EMDR Pract Res. 2009;3(2):107. doi:10.1891/1933-3196.3.2.107
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
