Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
The Effect of Counseling on Stigma in Psychiatric Patients Receiving Electroconvulsive Therapy: A Clinical Trial Study
Authors Sadeghian E , Rostami P, Shamsaei F , Tapak L
Received 1 October 2019
Accepted for publication 26 November 2019
Published 6 December 2019 Volume 2019:15 Pages 3419—3427
DOI https://doi.org/10.2147/NDT.S233094
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Efat Sadeghian,1 Parisa Rostami,2 Farshid Shamsaei,3 Lily Tapak4
1Assistant Professor, Chronic Diseases (Home Care) Research Centre, Hamadan University of Medical Sciences, Hamadan, Iran; 2MSc of Psychiatric Nursing, Department of Nursing, Hamadan University of Medical Sciences, Hamadan, Iran; 3Associate Professor, Behavioral Disorders and Substance Abuse Research Center, Hamadan University of Medical Sciences, Hamadan, Iran; 4Assistant Professor, Department of Biostatistics, School of Public, Hamadan University of Medical Sciences, Hamadan, Iran
Correspondence: Farshid Shamsaei
School of Nursing & Midwifery, Hamadan University of Medical Sciences, Shahid Fahmideh Bulv., Hamadan 65178, Iran
Tel +98-81-38381941
Email [email protected]
Purpose: Despite its efficacy and safety, electroconvulsive therapy (ECT) is underutilized, in part, due to the stigma associated with the treatment. This study aimed to evaluate the effect of counseling on stigma in patients with psychiatric disorders receiving ECT.
Patients and methods: A total of 114 patients with psychiatric disorders undergoing ECT were randomly divided into two groups. Both the groups received routine care and treatment, but the intervention group (n=57) received four counseling sessions. At the beginning and end of the study (6 weeks, post-treatment), patients completed the Internalized Stigma of Mental Illness scale. The data were analyzed using independent and paired sample t-tests.
Results: There was no significant difference in the mean stigma scores of participants in the control and intervention groups before counseling (P>0.08). However, post-intervention, there was a significant difference in the mean stigma scores between both the groups (P<0.001).
Conclusion: The findings demonstrate that the counseling intervention is effective in decreasing stigma in patients undergoing ECT. Therefore, it is recommended to use this therapeutic method in such patients.
Keywords: counseling, stigma, mental illness, electroconvulsive therapy
Introduction
Patients with psychiatric disorders experience multifaceted problems. One of these problems is the community’s response to these patients in the form of stigmatizing them, which affects patients’ self-concept.1 Stigma refers to negative attitudes and discriminatory judgments or negative thoughts and feelings, such as anxiety or hatred, adopted by a majority group against a minority group.2 Stigma of mental illness is a worldwide concern in global health care. Based on the evidence, 47% and 30% of the general population are reluctant to work and have social relationships with people suffering from depression, respectively.3
In addition to the social stigma that occurs through discriminatory judgments in the social and occupational relationships of people with mental disorders, such patients may also face internal stigma. Internalized stigma occurs as a result of believing negative messages sent by the community and applying them for oneself.4,5 Patients involved with internal stigma isolate themselves and abandon their jobs due to having negative emotions, such as shame and worthlessness.5 Moreover, they lose the opportunity of independent living because of self-discriminatory judgments.6 The behavioral consequences of internalized stigma can cause disabilities related to the primary symptoms of mental illness and low self-esteem and also can lead to disadvantages in many aspects of life, such as personal relationships, education, and work. This, in turn, can lead to experiencing social exclusion, being unable to participate in important life activities, and having a poor tendency to seek treatment, which, ultimately, hamper a major dimension of quality of life. Strong internalized stigma is associated with a lower level of self-efficacy and poor recovery of people living with mental illness, which, finally, result in unemployment.8
Internalized stigma is highly prevalent among psychiatric patients. Findings of studies in Iran have revealed the prevalence of internalized stigma to be 40% among people with mental illness.8 Electroconvulsive therapy (ECT) is one of the common treatments in psychiatry, which results in higher stigmatization among patients undergoing ECT due to negative attitudes toward this treatment.9 Despite the multiple benefits of this therapeutic approach, it causes anxiety for patients and their family. The most common causes of concerns in the community and in the development of negative attitudes toward this therapeutic method are incidence of seizure and possibility of brain damage due to treatment with electric convulsion, which lead to low acceptability of this treatment.10
The misperceptions about ECT are the results of a negative image of this procedure as an inhumane or even sadistic therapy presented by the media, early practices of this method in the past, fear of electricity and exaggerated fear following memory loss.11,12 Therefore, despite the great attention of psychiatrists to ECT as a safe, effective treatment, a significant stigma surrounds this therapeutic approach, which is likely to be the biggest barrier to the general acceptability of this method.13
As the literature indicates, various approaches have been used to reduce stigma in patients with psychiatric disorders. Some of the examined approaches are social skill training, cognitive behavioral therapy, goal achievement program, peer education, and narrative therapy. While some studies have introduced these approaches as effective, others have described them as unreliable.14,15 However, psychoeducation is considered more promising among the implemented interventions.16 Counseling is also recognized as one of the effective interventions for changing lifestyle in patients.17
In a study, Mittal et al investigated 14 articles related to strategies of reducing stigma and found that psychotherapy was the most commonly used psychiatric intervention. According to the results of the mentioned study, the interventions effective in stigma reduction entailed two dominant approaches, including attempting to change individual attitudes and beliefs and increasing skills of coping with internalized stigma by promoting self-esteem, sense of power, self-confidence, independence, coping skills, knowledge, and help-seeking behaviors.18
Therefore, one of the effective strategies to help mentally ill patients has a normal life is the provision of counseling and education sessions. Psychiatric nurses do not offer counseling services, and psychiatric patients receiving ECT experience stigma due to the treatment nature. Based on these reasons and because studies are rare in this field, the present study was conducted to determine the effect of counseling on stigma in patients with psychiatric disorders receiving ECT. The results of this study could be helpful in improving the quality of healthcare services.
Methods
Study Design and Sample
This clinical trial was conducted on patients with psychiatric disorders undergoing ECT at the Farshchian Psychiatry Hospital of Hamadan, Iran, in 2017.
A total of 114 patients with psychiatric disorders undergoing ECT were randomly divided equally into an intervention and a control group. Both the groups received routine care and treatment, but the intervention group additionally received four counseling sessions. Patients under study suffered from schizophrenia, schizoaffective, bipolar disorders, major depressive disorder and obsessive-compulsive disorders, diagnosed by a psychiatrist based on the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, the Fifth Edition (DSM-5). Moreover, the patients had a past history of hospitalization.
Following a similar study,19 the sample size was calculated to be 57 individuals in each group with a confidence level of 95%, test power of 95%, and sample loss of 10%, using the following formula:
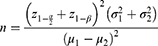
The inclusion criteria were the ability to communicate in Persian and indication of ECT, aged 18 years or older, lack of physical disability, no history of using psychoactive substances and no emergent need to receive ECT. However, the exclusion criteria were absence for more than one session and deterioration of the illness. The participants were assigned into an intervention and a control group through using the block randomization method in the R software (A=intervention; B=control). After the determination of the random sequences, each sequence was captured on a card and sealed in an envelope. Finally, 114 sealed envelopes were delivered to the main researcher (Figure 1).
 |
Figure 1 Consort flowchart. |
Measures
The data were collected using a demographic questionnaire and the Internalized Stigma of Mental Illness (ISMI) scale.20 The demographic questionnaire included age, gender, marital status, education level, diagnosis, occupation, duration of illness, duration of current hospital stay, number of admissions during the past year, infliction with other physical diseases, history of receiving ECT, and history of committing suicide.
ISMI is a 29-item self-report questionnaire developed by Ritsher et al to measure self-stigmatization in patients with mental disorders. This instrument consists of five subscales, including alienation, stereotype endorsement, perceived discrimination, social withdrawal, and stigma resistance. The tool is scored through summing up the scores of all the items divided by the number of the responded items. The items related to the subscale of stigma resistance are scored reversely. The minimum and maximum scores in the scale are 1 and 4, representing the lowest and highest levels of internalized stigma, respectively.20
Jacobsson et al (2013) confirmed the validity and reliability of the ISMI scale after translating it into Persian in an experimental study conducted on 30 patients. They reported the Cronbach’s alpha coefficient of 0.87 for the instrument.21 In the present study, after receiving permission via email, the questionnaire was translated by the researcher under the supervision of the supervisor and then back-translated by a fluent English speaker in order to assure the linguistic validity of the instrument; subsequently, the necessary modifications were made.
To evaluate the content and face validities of the questionnaire, it was submitted to ten faculty members at the Nursing and Midwifery Faculty of Hamadan University of Medical Sciences, Hamadan, Iran. After receiving the opinions of the professors, the scale was re-examined under the supervision of the supervisor and counselor, and the content and face validities of the instrument were affirmed by replacing appropriate terms. Furthermore, the internal reliability of the ISMI scale was examined by administering it to 30 patients, rendering a Cronbach’s alpha coefficient of 0.897, which indicated a proper internal consistency.
After the approval of the research project, the researcher attended the hospital departments in the morning shift when the visiting time was over and no special procedures were required. First, the researcher introduced herself and expressed her professional expertise to establish a trustworthy relationship with the patients. In the next step, the questionnaires were completed before the intervention under the researcher’s supervision. The intervention group was subjected to four individual and face-to-face mental health counseling sessions conducted by the researcher. The counseling sessions were held in one of the counseling and visiting rooms of the psychiatric ward once a week for 60 min (45 min for counseling, 5 min for review, and 10 min for questions and answers). The ISMI scale was filled out again by both the groups immediately and 2 weeks after the last session. The control group was provided with the current and routine methods of nursing and care.
Intervention
Participants allocated to the intervention group received 4 weeks of counseling intervention. The counseling program focused on reducing internalized stigma. The scientific content of mental health counseling on ECT was derived from a book written by Carson and investigation of the related articles about strategies for reducing stigma.22–24 The content of the counseling sessions in the intervention group is presented in Table 1. Patients in the control group continued to receive routine care. No specific intervention was implemented in the control group to avoid possible overlap (contamination) with components of the counseling intervention.
 |
Table 1 The Content of the Counseling Sessions in the Intervention Group |
Statistical Analysis
Data analysis was performed using SPSS software (version 20). Accordingly, the data were analyzed using paired sample and independent t-tests, mixed effects logistic regression model, and Bonferroni’s post hoc test.
Results
According to the results, in the control group, most of the patients were male (56.1%) and single (35.1%) and had junior high school education (35.1%). Regarding the intervention group, the majority of the participants were male (52.6%) and married (45.6%) and had elementary education (36.8%). The results of the Chi-square test revealed no significant difference between the two groups in terms of gender, marital status, and education level (P>0.05). The majority of the patients in the control (47.4%) and intervention (52.6%) groups had bipolar disorder. Furthermore, 50.9% and 54.4% of the patients in the control and intervention groups had no history of receiving ECT, respectively. According to the results of the Chi-square test, there was a significant difference between the two groups in terms of other physical illnesses (P=0.049) and history of suicide (P=0.014) (Table 2). The age mean was 39.29±14.07 in the control group and 38.71±3.37 in the intervention group. Based on the results of the independent t-test, there was no significant difference between the two groups in this regard before the intervention (P=0.822).
 |
Table 2 Comparative of Socio-Demographic and Clinical Characteristics of the Study Sample |
The Kolmogorov–Smirnov test was used to verify the normal distribution of the data (P<0.05). Prior to the intervention, the mean scores of internalized stigma were 2.7±0.33 and 2.68±0.33 in the control and intervention groups, respectively. Based on the results of the independent t-test, there was no significant difference between the two groups in this regard before the intervention (P=0.811).
However, immediately post-intervention, the intervention and control groups had the mean internalized stigma scores of 2.47±0.33 and 2.75±0.26, respectively. The results of the independent t-test revealed a significant difference between the two groups in this respect (P<0.001). This difference was also significant between both the groups 2-weeks post-intervention (P<0.001) (Table 3; Figure 2).
 |
Table 3 Comparison of Mean Scores of Internalized Stigma of the Study Sample |
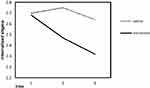 |
Figure 2 Change in internalized stigma before and after the intervention. |
The regression model of mixed effects was used to control the effect of confounding variables. The results showed that the score of internalized stigma was significantly different between the two groups, even after adjusting for the effect of three variables, namely other physical illnesses, number of suicide attempts, and number of hospital stay days (P<0.001) (Table 4).
 |
Table 4 Relationship Between Internalized Stigma and Demographic and Clinical Variables |
Considering the significance of time effect (P<0.001), the Bonferroni’s post hoc test was run. Regarding the intervention group, the results demonstrated a significant difference in the mean score of internalized stigma 1-month post-intervention, compared to that 2-weeks post-intervention (P<0.001). In addition, the mean score of internalized stigma was significantly different immediately and 2-weeks post-intervention, compared to that before the intervention (P<0.001). However, regarding the control group, the mean scores of internalized stigma were significantly different 2 weeks and 1-month post-intervention, compared to that per-intervention (P=0.33 and P=0.56, respectively) (Table 5).
 |
Table 5 Comparison of Internalized Stigma by Bonferroni’s Post Hoc Test |
Discussion
The results of the present study showed no significant difference between the intervention and control groups regarding the stigma score pre-intervention. In other words, both the groups were homogeneous in terms of internalized stigma. However, the two groups showed a significant difference in this regard immediately and 2-weeks post-intervention. The investigation of the demographic data showed that both the groups were comparable in this respect. The only three confounding variables that were significant included suffering from other physical illnesses, number of suicide attempts, and number of hospital stay days, the effects of which were adjusted using the mixed effects model. However, after the adjustment of the effect of these three variables, the score of internalized stigma was significantly different between the two groups.
The mean score of internalized stigma was also evaluated in each of the control and intervention groups. In the intervention group, the internalized stigma scores were significantly different immediately and 2-weeks post-intervention, compared to that pre-intervention. Nonetheless, no significant difference was observed between these stages in the control group. As a result, there was a significant difference between the intervention and control groups in terms of the total scores of stigma. In this regard, the mean score of stigma significantly decreased in the intervention group, compared to that in the control group. Prior to the intervention, the participants reported higher levels of internalized stigma, while the mean score significantly decreased post-intervention. Therefore, counseling resulted in the improvement of internalized stigma in mentally ill patients.
To the best of our knowledge, there exists no study investigating the impact of counseling on patients with mental disorders. Nevertheless, some studies examined the impact of counseling on other populations, such as pregnant women, patients with heart disease, and university students, and reported results in agreement with our findings.25–27 In line with the results of the present study, in a clinical trial conducted in Mashhad, Iran, Vagheyi et al investigated 60 home caregivers of patients with schizophrenia in two groups of control and intervention. They observed a reduction in the stigma score after the implementation of psychiatric training.28 Likewise, there exists evidence regarding the positive effect of psychiatric training programs on patients with bipolar disorder.29 Accordingly, Tsang et al reported that most of the programs targeted toward reduction of internalized stigma were effective in this regard. Although it is not possible to recognize a certain intervention as definitely more effective, mental health training appears to be the most promising method.16 Shamsaei et al investigated the effect of training interventions of the stigma associated with mental illness on family caregivers. They indicated that the difference in the stigma questionnaire scores was statistically significant between pre- and post-intervention times (P<0.001).30
On the other hand, in a systematic study, Boucher and Mesmer considered the impact of such interventions as unreliable on the reduction of stigma. Furthermore, they believed that this impact was not measurable due to the high risk of bias.14 In a meta-analysis, Wood et al reported that the interventions had negligible effects on internalized stigma due to the small sample size.31 However, the results of two studies conducted by Luckestead et al and Wood et al on patients with mental disorders are consistent with our findings.32 Overall, ECT is shrouded in myths and misconception. The notion of ECT often generates high levels of stress, anxiety and stigma among patients and their families. Counseling is of great importance in the ECT intervention because it reduces stigma and increases patient satisfaction. For this reason, counseling is recommended to be provided for patients undergoing ECT.
One of the limitations of this study was the lack of proper cooperation of the patients due to the nature of the disease. The researcher attempted to minimize this limitation by the establishment of a rapport with the patients. Another limitation was the inherent problems of the questionnaire data. The researcher attempted to mitigate this restriction by providing the patients with complete information about the objective of the study and assuring them about the confidentiality of the information contained in the questionnaire.
Furthermore, the implementation of counseling sessions with a researcher of opposite sex-created problems in the patient–counselor relationship. Therefore, it is suggested to perform counseling sessions with patients using a researcher of the same sex. In addition, the presence of grandiose delusions in most of the patients with mental disorders was a barrier to obtaining accurate information about the variables under investigation. The other limitations of the study entailed the time limitation of the counseling sessions, the low number of the sessions, and the short duration of the follow-up. As a result, it is recommended to perform a similar study in a longer time period. Moreover, since our study was restricted to patients undergoing ECT, it is recommended to perform a similar study on other mental illnesses.
Conclusion
Results showed that counseling is much helpful to psychiatric patients receiving ECT as they become more relaxed and better accept ECT. Additionally, counseling can decrease resistance in patients and reduce internalized stigma in them. Counseling affects stigma in such patients by providing them with the opportunity to express their attitudes and beliefs, guiding their mindset, and improving their individual and social performance. The results of this study can be used to inform healthcare managers and health providers to take necessary measures in order to reduce internalized stigma in patients with mental disorders.
Ethical Approval and Consent to Participate
This study was registered at the Iranian Registry of Clinical Trials with the code of IRCT2017041133378N1, and approved by the Ethics Committee of the Hamadan University of Medical sciences, approval no. IR.UMSHA.REC.1396.16. This study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The subjects were assured of the following: their participation was voluntary, they could withdraw at any time without facing any negative consequences. All participants provided their written informed consent.
Consent for Publication
Informed consent for the publication of these has been obtained from all participants. All the patients have signed for agreement.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
The authors were grateful for all the participants in this study for their cooperation and all the clinical staff for providing the intervention place and the assistance with data collection. This article is resulted from an MSc thesis supported by Hamadan University of Medical Sciences. This work was supported by vice-chancellor of research and technology of Hamadan University of Medical Sciences [No. 9603021435].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–2161. doi:10.1016/j.socscimed.2010.09.030
2. Gronholm PC, Henderson C, Deb T, et al. Interventions to reduce discrimination and stigma: the state of the art. Soc Psychiatry Psychiatr Epidemiol. 2017;52(3):249–258. doi:10.1007/s00127-017-1341-9
3. Barke A, Nyarko S, Klecha D. The stigma of mental illness in Southern Ghana: attitudes of the urban population and patients’ views. Soc Psychiatry Psychiatr Epidemiol. 2011;46(11):1191–1202. doi:10.1007/s00127-010-0290-3
4. Korkmaz G, Küçük L. Internalized stigma and perceived family support in acute psychiatric in-patient units. Arch Psychiatr Nurs. 2016;30(1):55–61. doi:10.1016/j.apnu.2015.10.003
5. Asrat B, AE A, Yimer T. Internalized stigma among patients with mental illness attending psychiatric follow-up at Dilla University Referral Hospital, Southern Ethiopia. Psychiatry J. 2018;23(2018):1987581. doi:10.1155/2018/1987581
6. Korkmaz G, Küçük L. Internalized stigma and perceived family support in acute psychiatric in-patient units. Arch Psychiatr Nurs. 2016;30(2):113–120. doi:10.1111/j.1440-1819.2011.02307.x
7. Shamsaei F, Mohamad Khan Kermanshahi M, Vanaki Z, et al. Experiences of family caregivers of patients with bipolar disorder. Asia Pac Psychiatry. 2010;2(4):201–220. 1758–5872.2010.00092.x
8. Young DK-W, Ng PY-N. The prevalence and predictors of self-stigma of individuals with mental health illness in two Chinese cities. Int J Soc Psychiatry. 2016;62:176–185. doi:10.1177/0020764015614596
9. Payne NA, Prudic J. Electroconvulsive therapy part II: a biopsychosocial perspective. J Psychiatr Pract. 2009;15(5):369–390. doi:10.1097/01
10. Shamsaei F, Kazemian H, Cheragh F, et al. The effect of family teaching on depression, anxiety and stress in caregivers of patients received electroconvulsive therapy. JMHTEP. 2019;14(4):289–296. doi:10.1108/JMHTEP-10-2018-0061
11. Wilhelmy S, Rolfes V, Grözinger M, et al. Knowledge and attitudes on electroconvulsive therapy in Germany: a web based survey. Psychiatr Res. 2018;262:407–412. doi:10.1016/j.psychres.2017.09.015
12. Solomon S, Simiyon M, Vedachalam A. Effectiveness of an educational intervention on medical students’ knowledge about and attitude towards electroconvulsive therapy. Acad Psychiatry. 2016;40(2):295–298. doi:10.1007/s40596-015-0415-9
13. Wo NKH, Guyitt B, Owen R. Cognitive behavioral therapy as a treatment for electroconvulsive therapy phobia: case report and review of literature. J Ect. 2015;31(4):273–276. doi:10.1097/YCT.0000000000000221
14. Büchter RB, Messer M. Interventions for reducing self-stigma in people with mental illnesses: a systematic review of randomized controlled trials. Ger Med Sci. 2017;24(15):Doc07. doi:10.3205/000248
15. McKinnon SA, Conner KO, Roker R, et al. The reduction of public and internalized stigma in late-life depression. J Appl Gerontol. 2017;1:733464816687079. doi:10.1177/0733464816687079
16. Tsang HW, Ching S, Tang K, et al. Therapeutic intervention for internalized stigma of severe mental illness: a systematic review and meta-analysis. Schizophr Res. 2016;173(1–2):45–53. doi:10.1016/j.schres.2016.02
17. Ylimäki E-L, Kanste O, Heikkinen H, et al. The effects of a counselling intervention on lifestyle change in people at risk of cardiovascular disease. Eur J Cardiovasc Nurs. 2015;14(2):153–161. doi:10.1177/1474515114521725
18. Mittal D, Sullivan G, Chekuri L, et al. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatr Serv. 2012;63(10):974–981. doi:10.1176/appi.ps.201100459
19. Assefa D, Shibre T, Asher L, et al. Internalized stigma among patients with schizophrenia in Ethiopia: a cross-sectional facility-based study. BMC Psychiatry. 2012;12:239. doi:10.1186/1471-244X-12-239
20. Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatr Res. 2003;121(1):31–49. doi:10.1016/j.psychres.2003.08.008
21. Jacobsson L, Ghanean H, Törnkvist B. Internalized stigma of mental illness in Sweden and Iran: a comparative study. OJPSYCH. 2013;3(4):370–374. doi:10.4236/ojpsych.2013.34039
22. Carson VB. Mental Health Nursing: The Nurts-Patient Journey. Philadelphia: W.B Sunders Co; 2000.
23. Rüsch N, Abbruzzese E, Hagedorn E, et al. Efficacy of coming out proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br J Psychiatry. 2014;204(5):391–397. doi:10.1192/bjp.bp.113.135772
24. Singh A, SK M, Grover S. Stigma associated with mental illness: conceptual issues and focus on stigma perceived by the patients with schizophrenia and their caregivers. Indian J Soc Psychiatry. 2016;32(2):134. doi:10.4103/0971-9962.181095
25. Parsa P, Saeedzadeh N, Masoumi SZ, et al. The effectiveness of counseling in reducing anxiety among nulliparous pregnant women. J Family Reprod Health. 2016;10(4):198–205. PMID: 28546819; PMCID: PMC5440819.
26. Hardcastle S, Taylor A, Bailey M, et al. A randomised controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and CHD risk factors. Patient Educ Couns. 2008;70(1):31–39. doi:10.1016/j.pec.2007.09.014
27. Strepparava MG, Bani M, Zorzi F, et al. Cognitive counselling intervention: treatment effectiveness in an Italian university centre. Br J Guid Counc. 2016;44(4):423–433. doi:10.1080/03069885.2015.1110561
28. Vaghee S, Salarhaji A, Asgharipour N, et al. Effects of psychoeducation on stigma in family caregivers of patients with schizophrenia: a clinical trial. Evidence Based Care. 2015;5(3):63–76. doi:10.22038/EBCJ.2015.5159
29. Cuhadar D, Cam MO. Effectiveness of psychoeducation in reducing internalized stigmatization in patients with bipolar disorder. Arch Psychiatr Nurs. 2014;28(1):62–66. doi:10.1016/j.apnu.2013.10.008
30. Shamsaei F, Nazari F, Sadeghian E. The effect of training interventions of stigma associated with mental illness on family caregivers: a quasi-experimental study. Ann Gen Psychiatry. 2018;17:48. doi:10.1186/s12991-018-0218-y
31. Wood L, Byrne R, Varese F, et al. Psychosocial interventions for internalised stigma in people with a schizophrenia-spectrum diagnosis: a systematic narrative synthesis and meta-analysis. Schizophr Res. 2016;176(2–3):291–303. doi:10.1016/j.schres.2016.05.001
32. Lucksted A, AL D, CH B, et al. Outcomes of a psychoeducational intervention to reduce internalized stigma among psychosocial rehabilitation clients. Psychiatr Serv. 2016;68(4):360–367. doi:10.1176/appi.ps.201600037
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
