Back to Journals » ClinicoEconomics and Outcomes Research » Volume 13
The Economic Implications of Introducing Single-Patient ECG Systems for Cardiac Surgery in Australia
Authors Saunders R, Hansson Hedblom A
Received 22 June 2021
Accepted for publication 26 July 2021
Published 13 August 2021 Volume 2021:13 Pages 727—735
DOI https://doi.org/10.2147/CEOR.S325257
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Rhodri Saunders, Amanda Hansson Hedblom
Coreva Scientific GmbH & Co. KG, Königswinter, Germany
Correspondence: Rhodri Saunders
Coreva Scientific GmbH & Co. KG, Im Mühlenbruch 1, Königswinter, 53639, Germany
Tel +49 2223 781 8010
Fax +49 761 76999421
Email [email protected]
Introduction: Sternal wound infections (SWIs) are severe adverse events of cardiac surgery. This study aimed to estimate the economic burden of SWIs following coronary artery bypass grafts (CABG) in Australia. It also aimed to estimate the national and hospital cost-benefit of adopting single-patient electrocardiograph (spECG) systems for CABG monitoring, a measure that reduces the rate of surgical site infections (SSIs).
Material and Methods: A literature review, which focused on CABG-related SSIs, was conducted to identify data which were then used to adapt a published Markov cost-effectiveness model. The model adopted an Australian hospital perspective.
Results: The average SWI-related cost of care increase per patient was estimated at 1022 Australian dollars (AUD), and the annual burden to the Australian health care system at AUD 9.2 million. SWI burden comprised 360 additional intensive care unit (ICU) days; 1979 additional general ward (GW) days; and 186 readmissions. Implementing spECG resulted in 103 fewer ICU days, 565 fewer GW days, 48 avoided readmissions, and a total national cost saving of AUD 2.5 million, annually. A hospital performing 200 yearly CABGs was estimated to save AUD 54,830.
Conclusion: SWIs cause substantial costs to the Australian health care system. Implementing new technologies shown to reduce the SWI rate is likely to benefit patients and reduce costs.
Keywords: sternal wound infection, surgical site infection, electrocardiography, patient readmission, patient safety, medical economics
Introduction
Healthcare-associated infections are a major issue in Australia,1,2 with more than 165,000 annual cases, making it the most common complication for hospital patients.3 A 2018 study which included 2767 patients from 19 Australian hospitals found that surgical site infections (SSIs) were the most common hospital-acquired infections, making up almost a third of total infections. SSIs are infections occurring after surgery, at the part of the body where the surgery was performed. They are avoidable but occur too frequently, impairing patient recovery and placing a substantial burden on hospital budgets.4,5
Extensive work is being undertaken in Australia to decrease the avoidable demand for healthcare, including infections and readmissions. An avoidable readmission is defined as a readmission that could have been evaded through improved clinical management.6 The Australian Commission on Safety and Quality in Health Care (ACSQHC) consider an SSI within 30 days of index admission an avoidable SSI-related readmission. In an effort to reduce healthcare-associated complications (HACs) and integrate safety and quality into hospital reimbursement, the Independent Hospital Pricing Authority (IHPA) has introduced funding penalties. They apply to 16 different HACs including SSI.7 With the penalties in place, hospitals no longer receive reimbursement for costs incurred as a consequence of SSIs.8
Coronary artery bypass graft (CABG) is the most common cardiac surgery in Australia, with almost 9000 procedures performed annually in public hospitals.9–11 Sternal wound infections (SWIs), a subset of SSIs where the infection occurs at the sternal wound site, are one of the most costly and severe cardiac surgery adverse events and their occurrence will have a large impact on hospital finances. SWIs increase patient length of stay (LoS), may lead to patients requiring expensive treatment, and can present after discharge leading to unplanned readmission. Postoperative mortality rates for deep SWIs have been estimated at up to 30%, and SWIs have been shown to more than double treatment costs.12 Reports indicate that circa 3.6% of Australian CABG patients develop SWIs.13
Several care improvement initiatives have been successful in reducing the rate of SWIs,14–16 showing that the introduction of new medical technologies has the potential to eliminate a subset of avoidable infections. Key changes which have proven effective include the introduction of impregnated sutures, new wound dressings, and single-patient-use electrocardiograph (spECG) cable and lead systems.17 All CABG patients are monitored with ECG during hospitalization. Reusable ECG (rECG) systems are standard in most Australian hospitals, despite the literature indicating that rECG can be vectors for cross contamination.18–20 In Australia, the use of rECG has been linked to an intensive care unit (ICU) outbreak of Vancomycin-Resistant Enterococcus (VRE).21 Lower contamination rates are seen with spECG.14,15 A United States (US) analysis of 27,000 CABG procedures found a 25% reduction in SSI following CABG in hospitals implementing spECG.16
Evidence to date indicates that spECG may be a relatively easy-to-implement update to patient monitoring that has the potential to improve patient safety and health system efficiency. This study explores the impact of implementing spECG utilizing a model simulating the Australian CABG care pathway. The aim of the study was to estimate the economic burden of SWIs following CABG in the Australian healthcare system, and to estimate the national and organization-specific cost-benefit of adopting a new medical technology that reduces the rate of SSIs.
Materials and Methods
Literature Review
An integrative literature review was undertaken using PubMed, with the objective to identify data to populate the simulation model. The review, conducted in 2018, focused on recent studies of CABG-related SSI in Australia. The search strategy was limited to literature published in English language between 2008 and 2018. A total of 71 unique articles were selected for screening. After excluding articles: not related to CABG or SSI, not containing incidence or cost data, specific to harvest-site infection, presenting data from before 2000, and not focused on Australia, 23 articles remained for full-text review (Figure 1). Model input data extracted from the sources included incidence rates, LoS, and costs. The literature review was rerun in November 2019, with no newer data relevant to the model identified.
 |
Figure 1 Literature review screening flow-chart. Abbreviations: CABG, Coronary Artery Bypass Graft; SSI, Surgical Site Infection. |
Markov Model
The CABG care pathway in Australia was simulated using a previously published cost-effectiveness Markov model,22 which was adapted to take an Australian hospital perspective. The adaptation was informed by the clinical experience of infection control specialist Prof Shaban and the clinical practice of his group. The model simulates the progression of a patient cohort undergoing CABG and receiving ECG monitoring with either spECG or rECG. The initial model cycle length was 1 day, until day 91, after which the cycle length was quarterly (91.3 days). The model simulated outcomes over 1 year, a time period relevant to hospital budgets.
As depicted in Figure 2, patients start in the “CABG” state, representing the procedure day. During each cycle, patients either remain in their current state or transition to another as indicated by the arrows. Following the standard CABG pathway, patients are initially transitioned from the CABG procedure to the ICU with mechanical ventilation (MV), followed by ICU without MV, after which they are moved to the general ward (GW) and finally discharged, either to home or to a care facility. Some patients require prolonged MV before returning to the above-described standard pathway. Each health state is associated with specific costs. At any stage of the simulation, patients may suffer an incident SWI, either superficial or deep. In the inpatient setting, the SWI creates costs related to prolonged GW and ICU stays. Outpatient SWIs result in either outpatient care (superficial) or readmission (deep). The potential for patient mortality exists in every health state.
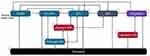 |
Figure 2 Model overview. Abbreviations: CABG, Coronary Artery Bypass Graft; ICU, Intensive Care Unit; MV, Mechanical Ventilation; GW, General Ward; SWI, Sternal Wound Infection. |
The probability of transitioning from one health state to another is calculated from data found in peer-reviewed literature. Calculation of transition probabilities is explained in the original model publication.22 In this instance, data from Australian sources (Table 1) were used in the calculations.
 |
Table 1 Base-Case Parameters |
As it was considered implausible to have CABG procedures on consecutive days, patients cannot “re-enter” the “CABG” state. Additionally, reoperation after day 91 is not included in the model. This modelling choice was based on the SYNTAX trial, in which only 0.1% of patients had repeated CABG over a 5-year period.22
The model was designed to be flexible and accept local inputs, with the purpose of enabling tailored outcomes for specific local settings. Populating the model with Australian data derived a base case for the clinical (additional hospital days and readmissions) and economic (cost) burden of SWIs in the Australian healthcare system. In the cases where no Australian data could be identified, US data from the original model was utilized. The input data and sources used are presented in Table 1. The population base case values were based on data from the Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) registry. Registry data were collected in 2001 to 2010 from 23 hospitals, with 109 surgeons, and included 20,619 patients with isolated CABG surgery.23 The average age was 68 years, 24.8% of patients were female, 3.3% were morbidly obese (Body Mass Index [BMI]>40), and 29% had diabetes. As per clinical data, morbidly obese patients remained on average an additional 4 days in the ICU and were at additional risk of deep SWI (DSWI) and mortality.24,25 Diabetes was associated with an additional risk of DSWI.26 The additional LoS due to SSIs was 7.5. Two inputs from different sources were identified for additional LoS due to DSWI: 16 days27 and 42 days.28 The base case conservatively assumes 16 days. The impact of assuming 42 days was explored in a sensitivity analysis.
The risk of SSI (3.6% after 30 days) and the DSWI proportion of SSIs (36.1%) were based on data on CABG surgeries performed between 2003 and 2012 in three public hospitals in Queensland.13 The impact of using spECG was sourced from a Medicare analysis which indicated an odds ratio (OR) for developing SSI of 0.74, indicating a 26% reduction of the odds of infection compared to rECG.16,22 In-hospital mortality was sourced from ANZSCTS data,23 and mortality risks were modelled using gender and age stratified life tables.42 Costs were sourced from public tariffs and published literature and presented in 2019 Australian dollars (AUD). The analysis adopted a hospital perspective, only considering costs to the hospital administration.
One-way (OWSA) and probabilistic (PSA) sensitivity analyses were undertaken to evaluate how potential variation in input values would impact the results, and to determine key outcome drivers with respect to the cost burden. Details on parameter sampling for the PSA can be found in the original model publication.22 Results are reported as the median (95% credible interval [CrI]) outcome.
Results
The average per patient LoS under current standard of care using rECG was estimated at 8.7 days (95% CrI 6.8–11.0), with a per patient cost of AUD 37,595 (95% CrI AUD 31,076–AUD 44,922) and a total annual national cost of AUD 336,548,332 for the modelled procedures. The results closely correspond to official figures of 8.6 days LoS and a per patient cost of AUD 36,775 published by the Australian government.10
The average increase in the cost of care per patient due to SWIs was estimated at AUD 1022. With 8952 CABG separations annually in Australia, the resulting annual burden of SWIs to the Australian health care system was AUD 9.2 million (95% CrI AUD 6.4–AUD 15.1 million). The SWI costs were comprised of 360 additional ICU days, 1979 additional GW days and 186 readmissions, of which 41 occurred within 30 days of the CABG procedure, and 55 within 30 days of discharge.
As presented in Table 2, over a 1-year time horizon, the implementation of spECG resulted in 103 fewer ICU days (95% CrI 44–223), 565 fewer GW days (95% CrI 230–1372), 48 avoided readmissions (95% CrI 23–82) and a total national cost saving of AUD 2.5 million (95% CrI AUD 1.2 million–AUD 5.0 million).
 |
Table 2 Base Case Results, ICU Days, GW Days and Readmissions, spECG versus rECG |
Taking a single-hospital perspective over 1 year, a hospital performing 200 CABG procedures annually was estimated to save AUD 54,830 with the implementation of spECG. This was due to fewer ICU days (−2), GW days (−13) and readmissions (−1). The mean cost saving per patient was AUD 274, representing a 26-fold return on investment.
OWSA varying the cost inputs by 50% showed that the cost of an additional DSWI day had the largest impact on the results. Reducing the DSWI cost by 50% resulted in 23% lower cost savings and increasing it by 50% to 28% higher cost savings. Cost of DSWI days was followed by GW costs (±20% change in cost savings), cost of readmissions (±20%), cost of ICU (−10, +11%), and cost of SSI (−10%, +11%). In the scenario analysis using the alternative source for additional LoS related to DSWI, the annual burden of SWIs to the Australian health care system almost doubled to AUD 16.3 million. The implementation of spECG resulted in 202 fewer ICU days, 1436 fewer hospital days, 48 fewer readmissions, and a total national cost saving of AUD 4.6 million per annum.
A PSA with 2000 iterations was run to test the robustness of the results. The PSA results were in line with the base case, with spECG use associated with a median of 105 fewer ICU days (95% CrI 44 to 223), 49 (95% CrI 23 to 82) fewer readmissions and a total cost saving of AUD 2.6 million (95% CrI AUD 1.2–AUD 5.0 million).
Discussion
SWIs incur an immense burden, significantly contributing to mortality and morbidity, increased treatment costs, and severely reduced quality of life of the affected. The Australian rate of DSWIs (1.3%) is in line with international figures, between the UK (0.8%43,44) and the US (2.0%45–51), with rates most similar to Germany (1.2%43,52) and France (1.3%43,53). As previously estimated in other settings,22 there are considerable potential cost-savings in reducing the number of SWIs. This study confirmed that CABG-related SWIs lead to a substantial cost and resource burden and identified DSWIs as a major driver. The results also indicated that the introduction of spECG may reduce healthcare costs and improve patient outcomes. The Australian & New Zealand Society of Cardiac & Thoracic Surgeons (ANZSCTS) reported that in 2018 hospitals performed on average 185 (range 60 to 440) isolated CABG procedures.54 Our analysis indicated that hospitals performing 200 procedures per year could save up to AUD 55,000 by switching to spECG.
The Australian healthcare system recognizes the impact of SSIs and has taken far-reaching measures against hospital-acquired, avoidable infections. Hospital budgets are being reduced as a direct consequence of HACs, with healthcare costs incurred by SSIs no longer reimbursed by the state, territory, or Australian governments. As the Australian financing models evolve, the cost impact of SWIs will likely become even greater, further signifying the importance of investing in improved strategies to reduce infection rates. SSIs make up almost one-third of all hospital-acquired infections. While SSI prophylaxis is a well-established concept, with national guidelines for infection prevention in place and almost ubiquitous antibiotics use, SWIs remain a considerable issue.
Due to lack of patient data availability, this computational analysis was not based on primary data, but on peer-reviewed, published literature. This is a potential limitation but one common to most health-economic analyses. The model outcomes were validated against Australian government data not used in the model inputs. Simulation outcomes closely aligned with the government results, signifying that the model can be considered a suitable representation of the Australian clinical reality. Another limitation in this analysis was the difficulty in determining proportions of SSIs which are SWIs. Case for case, SWI likely represents a higher cost than an average SSI. However, despite being one of the most common cardiac surgery adverse events, the literature on SWIs contribution to total SSIs in Australia is limited. Studies on CABG related SSIs do not always differentiate between SWIs and SSIs of the incision made in the CABG patient’s leg to attain a vein section for the graft. Finally, efficacy data for spECG are based of analyses of patient outcomes in the US and might not fully reflect the situation in Australia.
While there will always be inherent uncertainty in economic modelling, this study has taken several measures to ensure robustness and validity. PSA and OWSA showed that the results are robust to variations in parameter values, reducing the uncertainty of the outcomes. Prof. Shaban, currently Clinical Chair of the Infection Prevention and Disease Control at the Marie Bashir Institute for Infectious Diseases & Biosecurity, and his clinical group, were closely involved in the adaptation of the model to an Australian setting – hopefully, strengthening the model’s harmonization with real-world practice.
Conclusions
The cost and resource burden of SWI following CABG in Australia is substantial, but there is potential to provide patient benefit and reduce healthcare costs through the implementation of new technologies shown to reduce the rate of SWIs. Future research should further explore the impact of spECG as it is introduced in Australian hospitals.
Abbreviations
ANZSCTS, Australian And New Zealand Society Of Cardiac And Thoracic Surgeons; AUD, Australian Dollar; BMI, Body Mass Index; CABG, Coronary Artery Bypass Grafts; Cri, Credible Interval; DSWI, Deep Sternal Wound Infection; ECG, Electrocardiograph; GW, General Ward; HAC, Healthcare-Associated Complications; ICU, Intensive Care Unit; IHPA, Independent Hospital Pricing Authority; Los, Length Of Stay; MV, Mechanical Ventilation; ACSQHC, The Australian Commission On Safety And Quality In Health Care; PSA, Probabilistic Sensitivity Analysis; rECG, Reusable Electrocardiograph; RR, Relative Risk; spECG, Single-Patient Electrocardiograph; SSI, Surgical Site Infection; SWI, Sternal Wound Infection; US, United States; VRE, Vancomycin-Resistant Enterococcus.
Acknowledgments
We thank Professor Ramon Z. Shaban, Clinical Chair, Infection Prevention and Disease Control at the University of Sydney and Western Sydney Local Health District, for his invaluable contribution in suggesting and reviewing data, assumptions, and the simulated pathway to as closely as possible reflect the Australian clinical reality.
Funding
Coreva Scientific received consultancy fees from Cardinal Health for work related to this manuscript.
Disclosure
Dr Saunders is the owner of Coreva Scientific, a health-economics and value-based healthcare consultancy that focuses on medical devices. Dr Saunders also reports consultancy fees from Cardinal Health Inc and Medtronic Inc, outside the submitted work. Ms Hansson Hedblom is an employee of Coreva Scientific. The authors report no other conflicts of interest in this work.
References
1. Commission on Safety A, in Health Care Q. Approaches to surgical site infection surveillance for acute care settings in Australia; 2017.
2. Mitchell BG, Shaban RZ, Macbeth D, Wood C-J, Russo PL. The burden of healthcare-associated infection in Australian hospitals: a systematic review of the literature sciencedirect. Infection. 2017;22:117–128. doi:10.1016/j.idh.2017.07.001
3. The National Health and Medical Research Council in collaboration with the Australian Commission on Safety and Quality in Health Care. Australian guidelines for the prevention and control of infection in healthcare (2019) NHMRC. Available from: https://www.nhmrc.gov.au/about-us/publications/australian-guidelines-prevention-and-control-infection-healthcare-2019#block-views-block-file-attachments-content-block-1.
4. Coskun D, Aytac J, Aydinli A, Bayer A. Mortality rate, length of stay and extra cost of sternal surgical site infections following coronary artery bypass grafting in a private medical centre in Turkey. J Hosp Infect. 2005;60(2):176–179. doi:10.1016/j.jhin.2004.10.017
5. Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96:1–15. doi:10.1016/j.jhin.2017.03.004
6. Avoidable hospital readmissions. Australian commission on safety and quality in health care. Available from: https://www.safetyandquality.gov.au/our-work/indicators/avoidable-hospital-readmissions#list-of-conditions-considered-to-be-avoidable-hospital-readmissions.
7. Hospital-acquired complications (HACs). Australian commission on safety and quality in health care. Available from: https://www.safetyandquality.gov.au/our-work/indicators/hospital-acquired-complications.
8. Independent Hospital Pricing Authority. Independent hospital pricing authority pricing framework for Australian public hospital services; 2019.
9. The Australian Institute of Health and Welfare. Hospital resources 2017–18: Australian hospital statistics, summary - Australian institute of health and welfare. Available from: https://www.aihw.gov.au/reports/hospitals/hospital-resources-2017-18-ahs/contents/summary.
10. Independent Hospital Pricing Authority. Independent hospital pricing authority national hospital cost data collection Australian public hospitals cost report 2013–2014 round 18.
11. National Hospital Cost Data Collection. AR-DRG cost weight tables v8.0x, round 21 (financial year 2016-17) IHPA. Available from: https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-ar-drg-cost-weight-tables-v80x-round-21. Accessed June 16, 2020.
12. Sears ED, Wu L, Waljee JF, Momoh AO, Zhong L, Chung KC. The impact of deep sternal wound infection on mortality and resource utilization: a population-based study. World J Surg. 2016;40(11):2673–2680. doi:10.1007/s00268-016-3598-7
13. Si D, Rajmokan M, Lakhan P, Marquess J, Coulter C, Paterson D. Surgical site infections following coronary artery bypass graft procedures: 10 years of surveillance data. BMC Infect Dis. 2014;14:1–9. doi:10.1186/1471-2334-14-318.
14. Albert NM, Slifcak E, Roach JD, et al. Infection rates in intensive care units by electrocardiographic lead wire type: disposable vs reusable. Am J Crit Care. 2014;23(6):460–468. doi:10.4037/ajcc2014362
15. Albert NM, Murray T, Bena JF, et al. Differences in alarm events between disposable and reusable electrocardiography lead wires. Am J Crit Care. 2015;24(1):67–74. doi:10.4037/ajcc2015663
16. Lankiewicz JD, Wong T, Moucharite M. The relationship between a single-patient-use electrocardiograph cable and lead system and coronary artery bypass graft surgical site infection within a Medicare population. Am J Infect Control. 2018;46(8):949–951. doi:10.1016/j.ajic.2018.01.023
17. Kles CL, Murrah CP, Smith K, Baugus-Wellmeier E, Hurry T, Morris CD. Achieving and sustaining zero: preventing surgical site infections after isolated coronary artery bypass with saphenous vein harvest site through implementation of a staff-driven quality improvement process. Dimens Crit Care Nurs. 2015;34(5):265–272. doi:10.1097/DCC.0000000000000131
18. Reshamwala A, McBroom K, Il CY, et al. Microbial colonization of electrocardiographic telemetry systems before and after cleaning. Am J Crit Care. 2013;22(5):382–389. doi:10.4037/ajcc2013365
19. Lestari T, Ryll S, Kramer A. Microbial contamination of manually reprocessed, ready to use ECG lead wire in intensive care units. GMS Hyg Infect Control. 2013;8(1):Doc07. doi:10.3205/dgkh000207
20. Jancin B. Antibiotic-resistant pathogens found on 77 % of ECG lead wires. Cardiol News. 2004;2:14.
21. Lee AS, White E, Monahan LG, Jensen SO, Chan R, Van Hal SJ. Defining the role of the environment in the emergence and persistence of vanA vancomycin-resistant enterococcus (VRE) in an intensive care unit: a molecular epidemiological study. Infect Control Hosp Epidemiol. 2018;39(6):668–675. doi:10.1017/ice.2018.29
22. Saunders R, Lankiewicz J. The cost effectiveness of single-patient-use electrocardiograph cable and lead systems in monitoring for coronary artery bypass graft surgery. Front Cardiovasc Med. 2019;6:61. doi:10.3389/fcvm.2019.00061
23. Ch’ng SL, Cochrane AD, Wolfe R, Reid C, Smith CI, Smith JA. Procedure-specific cardiac surgeon volume associated with patient outcome following valve surgery, but not isolated CABG surgery. Hear Lung Circ. 2015;24(6):583–589. doi:10.1016/j.hlc.2014.11.014
24. Yap CH, Zimmet A, Mohajeri M, Yii M. Effect of obesity on early morbidity and mortality following cardiac surgery. Hear Lung Circ. 2007;16(1):31–36. doi:10.1016/j.hlc.2006.09.007
25. Ghanta RK, LaPar DJ, Zhang Q, et al. Obesity increases risk-adjusted morbidity, mortality, and cost following cardiac surgery. J Am Heart Assoc. 2017;6(3). doi:10.1161/JAHA.116.003831
26. Harrington G, Russo P, Spelman D, et al. Surgical-site infection rates and risk factor analysis in coronary artery bypass graft surgery. Infect Control Hosp Epidemiol. 2004;25(6):472–476. doi:10.1086/502424
27. Floros P, Sawhney R, Vrtik M, et al. Risk factors and management approach for deep sternal wound infection after cardiac surgery at a tertiary medical centre. Hear Lung Circ. 2011;20(11):712–717. doi:10.1016/j.hlc.2011.08.001
28. Lonie S, Hallam J, Yii M, et al. Changes in the management of deep sternal wound infections: a 12-year review. ANZ J Surg. 2015;85(11):878–881. doi:10.1111/ans.13279
29. Raza S, Sabik JF, Ainkaran P, Blackstone EH. Coronary artery bypass grafting in diabetics: a growing health care cost crisis. J Thorac Cardiovasc Surg. 2015;150(2):304–312.e2. doi:10.1016/j.jtcvs.2015.03.041
30. Jenney AWJ, Harrington GA, Russo PL, Spelman DW. Cost of surgical site infections following coronary artery bypass surgery. ANZ J Surg. 2001;71(11):662–664. doi:10.1046/j.1445-1433.2001.02225.x
31. Independent Hospital Pricing Authority. National efficient price determination 2018-19 IHPA. Available from: https://www.ihpa.gov.au/publications/national-efficient-price-determination-2018-19. Accessed June 3, 2020.
32. Bailey ML, Richter SM, Mullany DV, Tesar PJ, Fraser JF. Risk factors and survival in patients with respiratory failure after cardiac operations. Ann Thorac Surg. 2011;92(5):1573–1579. doi:10.1016/j.athoracsur.2011.04.019
33. McNeely C, Markwell S, Vassileva C. Trends in patient characteristics and outcomes of coronary artery bypass grafting in the 2000 to 2012 medicare population. Ann Thorac Surg. 2016;102(1):132–138. doi:10.1016/j.athoracsur.2016.01.016
34. Grabowski DC.Post-acute and long-term care: a primer on services, expenditures and payment methods ASPE; 2010. Available from: https://aspe.hhs.gov/basic-report/post-acute-and-long-term-care-primer-services-expenditures-and-payment-methods.
35. Medship Australia. Medical supplies & equipment - shop medical products & devices. Available fom: https://www.medshop.com.au/.
36. Independent Hospital Pricing Authority. National hospital cost data collection report, public sector, round 21 (financial year 2016-17) IHPA. Available from: https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-report-public-sector-round-21-financial-year.
37. New South Wales Health Department. NSW Costs of Care Standards 2009/10.Available from: https://www1.health.nsw.gov.au/pds/ArchivePDSDocuments/GL2011_007.pdf.
38. Hicks P, Huckson S, Fenney E, Leggett I, Pilcher D, Litton E. The financial cost of intensive care in Australia: a multicentre registry study. Med J Aust. 2019;211(7):324–325. doi:10.5694/mja2.50309
39. Territory Ac. ACT public service nursing and midwifery enterprise agreement 2013-2017 ACTPS nursing and midwifery agreement 2013-2017; 2018.
40. Sandy-Hodgetts K, Leslie GD, Lewin G, Hendrie D, Carville K. Surgical wound dehiscence in an Australian community nursing service: time and cost to healing. J Wound Care. 2016;25(7):377–383. doi:10.12968/jowc.2016.25.7.377
41. Atkins ER, Geelhoed EA, Knuiman M, Briffa TG. One third of hospital costs for atherothrombotic disease are attributable to readmissions: a linked data analysis. BMC Health Serv Res. 2014;14(1):338. doi:10.1186/1472-6963-14-338
42. Australian Bureau of Statistics. 3302.0.55.001- life tables, states, territories and Australia, 2016-2018. Available from: https://www.abs.gov.au/ausstats/[email protected]/mf/3302.0.55.001.
43. European Centre for Disease Prevention and Control. Annual epidemiological report for 2016. Healthcare-associated infections: surgical site infections; 2018.
44. Ariyaratnam P, Bland M, Loubani M. Risk factors and mortality associated with deep sternal wound infections following coronary bypass surgery with or without concomitant procedures in a UK population: a basis for a new risk model? Interact Cardiovasc Thorac Surg. 2010;11(5):543–546. doi:10.1510/icvts.2010.237883
45. Lemaignen A, Birgand G, Ghodhbane W, et al. Sternal wound infection after cardiac surgery: incidence and risk factors according to clinical presentation. Clin Microbiol Infect. 2015;21(7):
46. Huang SS, Placzek H, Livingston J, et al. Use of medicare claims to rank hospitals by surgical site infection risk following coronary artery bypass graft surgery. Infect Control Hosp Epidemiol. 2011;32(8):775–783. doi:10.1086/660874
47. Berríos-Torres SI, Mu Y, Edwards JR, Horan TC, Fridkin SK. Improved risk adjustment in public reporting: coronary artery bypass graft surgical site infections. Infect Control Hosp Epidemiol. 2012;33(5):463–469. doi:10.1086/665313
48. Feng TR, White RS, Gaber-Baylis LK, Turnbull ZA, Rong LQ. Coronary artery bypass graft readmission rates and risk factors - A retrospective cohort study. Int J Surg. 2018;54(Pt A):7–17. doi:10.1016/j.ijsu.2018.04.022
49. Itagaki S, Cavallaro P, Adams DH, Chikwe J. Bilateral internal mammary artery grafts, mortality and morbidity: an analysis of 1 526 360 coronary bypass operations. Heart. 2013;99(12):849–853. doi:10.1136/heartjnl-2013-303672
50. Williams JB, Peterson ED, Brennan JM, et al. Association between endoscopic vs open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA. 2012;308(5):475–484. doi:10.1001/jama.2012.8363
51. Likosky DS, Wallace AS, Prager RL, et al. Sources of variation in hospital-level infection rates after coronary artery bypass grafting: an analysis of the society of thoracic surgeons adult heart surgery database. Ann Thorac Surg. 2015;100(5):1570–1576. doi:10.1016/j.athoracsur.2015.05.015
52. Kerwat K, Geffers C, Gastmeier P, Wulf H. Krankenhaushygiene–Das Krankenhaus-Infektions-Surveillance-System (KISS). AINS-Anästhesiologie Intensivmedizin [AINS anesthesiology Intensive care Emergency medicine]. Notfallmedizin Schmerztherapie. 2010;45(09), 562–563. German.
53. Cossin S, Malavaud S, Jarno P, et al. Surgical site infection after valvular or coronary artery bypass surgery: 2008-2011 French SSI national ISO-RAISIN surveillance. J Hosp Infect. 2015;91(3):225–230. doi:10.1016/j.jhin.2015.07.001
54. Shardey G, Williams-Spence J, Tran L, et al. ANZSCTS cardiac surgery database program the Australian and New Zealand society of cardiac and thoracic surgeons cardiac surgery database program national annual report; 2018.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
