Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
The current state of physical activity and exercise programs in German-speaking, Swiss psychiatric hospitals: results from a brief online survey
Authors Brand S , Colledge F, Beeler N, Pühse U, Kalak N, Sadeghi Bahmani D , Mikoteit T, Holsboer-Trachsler E, Gerber M
Received 27 February 2016
Accepted for publication 23 March 2016
Published 3 June 2016 Volume 2016:12 Pages 1309—1317
DOI https://doi.org/10.2147/NDT.S107313
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Serge Brand, 1,2 Flora Colledge, 2 Nadja Beeler, 2 Uwe Pühse, 2 Nadeem Kalak, 1 Dena Sadeghi Bahmani, 1 Thorsten Mikoteit, 1 Edith Holsboer-Trachsler, 1 Markus Gerber 2
1Psychiatric Clinics of the University of Basel, Center for Affective, Stress and Sleep Disorders, 2Department of Sport, Exercise and Health, Sport Science Section, University of Basel, Basel, Switzerland
Background: Physical activity and exercise programs (PAEPs) are an important factor in increasing and maintaining physical and mental health. This holds particularly true for patients with psychiatric disorders undergoing treatment in a psychiatric hospital. To understand whether the benefits reported in the literature are mirrored in current treatment modalities, the aim of the present study was to assess the current state of PAEPs in psychiatric hospitals in the German-speaking part of Switzerland.
Methods: All psychiatric hospitals (N=55) in the German-speaking part of Switzerland were contacted in spring 2014. Staff responsible for PAEPs were asked to complete an online questionnaire covering questions related to PAEPs such as type, frequency, staff training, treatment rationale, importance of PAEPs within the treatment strategy, and possible avenues to increase PAEPs.
Results: Staff members of 48 different psychiatric hospitals completed the survey. Hospitals provided the following therapeutic treatments: relaxation techniques (100%), sports therapy (97%), activity-related psychotherapeutic interventions (95%), physiotherapy (85%), body therapies (59%), far-east techniques (57%), and hippotherapy (22%). Frequencies ranged from once/week to five times/week. Approximately 25% of patients participated in the PAEPs. Interventions were offered irrespective of psychiatric disorders. PAEP providers wanted and needed more vocational training.
Conclusion: All participating psychiatric hospitals offer a broad variety of PAEPs in their treatment curricula. However, the majority of inpatients do not participate in PAEPs. Furthermore, those who do participate cannot continue to do so following discharge. PAEP providers need specific extended vocational trainings and believe that the potential of PA should be improved.
Keywords: physical activity, psychiatric disorders, psychiatric hospitals, German-speaking part of Switzerland, sport participation
Corrigendum for this paper has been published
Introduction
There is both growing recognition and scientific evidence that interventions of physical activity and exercise programs (PAEPs) have a favorable impact on patients with psychiatric disorders.1–7 These findings have been reported among groups of patients with major depressive disorders (MDDs),6,8,9 schizophrenia,10,11 post-traumatic stress disorder (PTSD),12,13 alcohol abuse,14,15 sleep disorders,16 or autism spectrum disorders.17 The neurophysiological mechanisms underlying the beneficial effects of PA on psychological functioning and wellbeing are complex, although there is increasing evidence that regular, acute, and chronic PA does have an impact at the molecular level18,19 and on brain plasticity.1,20,21 In parallel, psychological mechanisms are involved; specifically, regular PA has a favorable influence of self-esteem among patients with psychiatric disorders,22 on body image and physical self-concept,23 and, most importantly, on dimensions of anxiety and depression.6,9,24
However, it is widely reported that patients with psychiatric disorders are less physically active and do exercise less than healthy peers,25–27 potentially increasing and maintaining the risk for further physical and mental health problems. Among those seeking treatment, psychiatric hospitals provide an excellent environment to initiate physical activity, as they offer supervised free training during a phase in which patients are under few time constraints. In view of the potential of PAEPs as adjunct treatment reported in the literature to date, our aim in this study was to explore the extent to which these programs are implemented in the inpatient treatment of psychiatric disorders in the German-speaking part of Switzerland. An understanding of the implementation of PAEPs in practice, and the experiences of program staff, is an important factor for the future translation of research findings to clinical practice.
Methods
Sampling
During spring 2012, all psychiatric hospitals of the German-speaking part of Switzerland (N=55) were identified via publicly accessible lists on the Internet. To be enrolled in the study, the minimum requirement was that psychiatric hospitals treated not only outpatients but also inpatients and that the official language was German; that is to say, staff and inpatients communicate in German or Swiss German.
Next, NB contacted all identified hospitals by phone calls and asked for a brief talk with the staff member responsible for the PAEPs. The aim of the phone call and the study were explained, and, if agreed, the URL of an online survey was transmitted via email. All participants were informed that participation was voluntary and that all data would be gathered anonymously; written informed consent was obtained on the first page of the questionnaire. Furthermore, they were informed that they could withdraw from the study at any time. To improve participation, participants could take part in a prize draw (ten vouchers of CHF 30.00 [approximately USD 30.00] from a known national supermarket), although to do so they needed to provide an email address. Ethical approval was not required by the Institutional Review Board of the University of Basel because the survey was not addressed to patients or underage people.
Online survey
Data collection was done online, as this was judged to be both time saving for participants and a reliable method to gather data.28 We used commercially available software (Unipark®; http://www.unipark.de), as this is an easily applied tool for the creation of Internet-based studies. Furthermore, the software provider guarantees that all data are stored on a server that is not accessible to any third party. Importantly, the user of the software receives the raw data of the answers but not participants’ IP address, ensuring both data security and participants’ anonymity. Moreover, the online survey was designed to avoid repeated participation (IP addresses already used are automatically blocked). Participants needed ~15–20 minutes to complete the survey.
Questionnaire
A questionnaire with multiple choice response options was developed expressly for this study, in order to address the specific areas of inquiry. Table 1 reports all items.
  | Table 1 Overview of the questionnaire |
Statistical analysis
The findings are based on descriptive statistics such as mean, standard deviation, median, or percentage. Furthermore, chi-square tests were performed to calculate associations between dimensions as specified in more detail in the text. All statistical analyses were performed with SPSS® 22.0 (IBM Corporation, Armonk, NY, USA) for Apple Mac®.
Results
Part 1: general information about the psychiatric hospital
Of the 55 psychiatric hospitals in German-speaking Switzerland approached, staff members of 48 (87.3%) took part in the survey. In all, 42 respondents (87.5%) were physiotherapists, three (6.25%) had a master’s degree in sports science, and three (6.25%) did not answer to this item.
Of the 48 respondents, 32 (66%) were working in a general psychiatric hospital, eight (17%) were working in a university psychiatric hospital, and eight (17%) were working in psychiatric wards of a somatic hospital. Twenty (43%) hospitals had >200 beds for inpatients, nine (19%) hospitals had 99–200 beds, 15 (32%) had between 50 and 99 beds, and three hospitals reported <50 beds for psychiatric inpatients.
Seventeen (35.5%) psychiatric hospitals were located in the Canton Berne, eight (17%) were located in the Canton Zürich, five (10%) in the Canton Thurgau, four (8%) each in the Cantons St Gallen and Aargau, three (6%) each in Basel City and in Aarau (city and close surroundings), two (4%) each in the Cantons Basel Country and Grisons, and one (2%) each in the Cantons of Appenzell-Ausserrhoden and Zug.
Regarding the disorders most frequently treated at the hospital, 80% of respondents reported personality disorders and mood disorders, ~78% reported anxiety, stress-related, and somatoform disorders, ~65% reported substance use disorders, 55% reported schizophrenia and nonmood psychotic disorders, 50% reported mental disorders due to existing physiological conditions, and 5%–15% reported intellectual disabilities, pervasive and specific developmental disorders, behavioral and emotional disorders, and unspecific mental disorders. Note that multiple answers were possible. A chi-square test revealed that there was no association between most frequently treated disorders and the number of beds of the hospital (χ2(N=48, df=27)=0.45; P=0.67).
Part 2: PAEPs
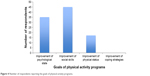
As depicted in Figure 1, all psychiatric hospitals (100%) offered relaxation techniques, and 47 (97%) offered sports therapy (fitness, swimming, ball sports, and endurance training), 46 (96%) offered general physical activity, 40 (85%) offered physiotherapy/remedial gymnastics, 28 (59%) offered so called body therapies such as Feldenkrais or bioenergetics, 27 (57%) offered far-east techniques (Tai Chi and Qigong), and ten (22%) offered hippotherapy. Therefore, the majority of hospitals offered more than one type of PAEP content.
As regards the frequency with which PAEPs took place, responses ranged from once per week to five times per week. Factors that were reported as limiting the frequency of sessions were staff availability, sports hall and/or equipment availability, and the size of the hospital: hospitals with a lower number of beds offered fewer and less frequent PAEPs (χ2 (N=48, df=18) =16.45; P<0.05).
As regards the group size of participants, a range of one to seven participants was the most frequently reported group size. One-to-one sessions were chiefly offered as personal training or for therapeutic interventions such as physiotherapy or other body therapies. Of the 48 participants, 40 (83.3%) answered that <25% of all inpatients participated in the PAEPs, and eight (16.7%) estimated that between 25% and 50% of all inpatients participated in the PAEPs (Figure 2).
All PAEPs were attended on a voluntary basis (100%), although 40 (83.3%) respondents emphasized that patients were made aware of the programs and encouraged to attend the PAEPs. Furthermore, participants reported that patients seemed generally moderately to rather highly motivated to participate in the PAEPs.
Thirty-six (75%) participants reported that the availability and equipment of the current PAEP infrastructure were sufficient, five (10.4%) reported that the infrastructure was well to very well equipped, whereas seven (14%) reported that the availability and equipment of the infrastructure were not or not at all sufficient.
Part 3: impact of PAEPs on patients’ status and aftercare
All participants responded that in their view, PAEPs improved patients’ physical and psychological status. Regarding the hypothesized importance of the programs, answers ranged from a little importance (n=8; 16.6%), to moderate importance (n=38; 79%); two (4.16%) answered that the importance of PAEPs was large (Figure 3). All participants reported that after discharge, their patients no longer had access to the PAEPs offered as part of inpatient treatment.
  | Figure 3 Number (blue) and percentages (red) of respondents reporting the importance of physical activity programs. |
Thirty-five (72.9%) answered that the main goal of a PAEP was to improve patients’ psychological state, 45 (93.75%) answered that a further main goal was to improve patients’ social skills, and 17 (35.42%) answered that a further main goal was to improve patients’ physical status. None of the participants answered that a PAEP was aimed at improving patients’ coping strategies (note that multiple answers were possible; Figure 4). No associations between the main goals of PAEPs and the most frequently treated disorders were observed (χ2 (N=48; df=27) =0.45; P=0.78).
  | Figure 4 Number of respondents reporting the goals of physical activity programs. |
Part 4: personal skills and knowledge
All participants answered that they rely on their own experience and vocational training to plan and organize the PAEP sessions. Furthermore, the majority (n=40, 83.3%) also reported benefiting from the experiences and advice of their peers. No respondent stated that they sought or obtained information from specific Internet sites or scientific publications.
Part 5: reasons to offer PAEPs
All participants answered that PAEPs were an integrated treatment modality of the hospital. In all, 38 (79.16%) reported that they were particularly motivated to lead PAEPs and 30 (62.5%) reported that the hospital’s medical staff recognized the beneficial effects of PAEPs. Nobody answered that PAEPs were offered because supplementary vocational training was available, because the hospital had the existing infrastructure, or because of scientific evidence supporting the benefits of such programs.
Part 6: main treatment regimen
All participants reported that the main treatment regimen of the hospital comprised medication (100%), psychotherapy (100%), and occupational therapy (100%). Forty (83.3%) reported that music therapy and art therapy were also included.
Thirty (62.5%) answered that within the main treatment regimen, the potential benefits of PAEPs was fairly well accepted; ten (20.83%) answered that it was well accepted, four (8.3%) answered that it was not well accepted, and four (8.3%) did not know.
Part 7: outlook
All participants reported that in order to improve the PAEPs offered by the hospital, staff would require advanced vocational training in sport and exercise sciences and advanced vocational training in adapted physical activity for psychiatric patients.
Discussion
The key findings of the present survey are that all psychiatric hospitals of the German-speaking part of Switzerland whose staff participated in this survey offer a broad variety of PAEPs. Furthermore, ~25% of all patients are reported to participate in such programs. Staff involved in these programs also felt that specific extended vocational training would allow them to improve their skills and optimize the existing programs.
The present survey is the first to give an overview of the existence and role of PAEPs in psychiatric hospitals of the German-speaking part of Switzerland. Specifically, the pattern of results shows that PAEPs are well established and integrated in the treatment regimen.
All respondents reported that they felt that participation in PEAPs impacted favorably on patients’ psychological status. While anecdotal, this observation is in line with the increasing wealth of studies showing a favorable influence of PAEPs on a broad variety of psychiatric disorders,1–7 such as MDDs,6,8,9 schizophrenia,10,11 PTSD,12,13 alcohol abuse,14,15 sleep disorders,16 or autism spectrum disorders.17
Next, in our opinion, a major issue is patients’ participation rate: 83% reported that only up to 25% of patients participated in the offered PEAPs, and further 16.7% reported that 25%–50% of patients did so. Or simply put: we estimate that 50%–75% of inpatients do not attend the PEAPs, and we claim that this rate of participation is low. The quality of the data does not allow a deeper understanding of patients’ underlying decisions, although if we combine the result that participating patients seemed moderately to rather highly motivated to participate in the PEAPs, the key factor of patients’ (non-) participation may be their motivation.
Nevertheless, the low participation rates were not surprising. For instance, studies consistently show that people with psychiatric disorders have lower physical activity29,30 and cardiorespiratory fitness levels.31,32 This is critical, because low physical activity and cardiorespiratory fitness are considered important factors which may link psychiatric and comorbid somatic disorders.33 A recent meta-analysis showed that exercise interventions have the capacity to improve cardiorespiratory fitness in people with MDD in clinically meaningful ways.34
Taken together, the use of PAEP in the treatment of psychiatric disorders is supported by strong empirical evidence.35–37 For instance, studies show that among patients with clinical depression, exercise seems to have similar effects to antidepressants and psychotherapy.38 Thus, integrating exercise as an add-on to standard care during inpatient treatment, as well as efforts to promote lifestyle physical activity to prevent relapses after the end of hospitalization, seem promising. A major challenge, however, is that it is particularly difficult to initiate and maintain regular exercise among patients with psychiatric disorders, because their psychiatric symptoms interfere with their motivation and capacity to self-regulate health-related behaviors.33,39 Given this background, we claim that intervention programs specifically tailored to motivate psychiatric patients to achieve a more physically active lifestyle should be key among psychiatric hospitals. In this regard, from intervention studies on motivational processes among patients with somatic complaints, we learned that specific psychoeducational inputs were able to increase patients’ motivation to exercise also after discharge.40 Similarly, future studies might focus on applying such motivational programs in patients with psychiatric disorders.
In this vein, all participants reported that after patients’ discharge, no further options of aftercare were available. In light of the fact that all respondents felt that PAEPs were beneficial for patients and comprise activities, which can be protective against psychological complaints, the potential to extend PAEP offers for patients after the inpatient phase could represent a long-term element of health promotion for this population. Since many psychological disorders are relapsing conditions, long-term interventions must be explored as potentially protective against recurrence. The knowledge that PEAPs can be extended following the inpatient phase may also be an important motivator for patients to begin with such programs, as they will not have to face a loss of facilities as soon as their treatment ends.
Furthermore, several participants reported that an aim of the PEAPs was to bolster patients’ social skills. This observation is interesting, as, to the best of our knowledge, research on this particular aspect of functioning is sparse. Data from a Finnish study suggest that individuals who reported frequent exercise also felt more socially integrated than their less active peers, while participation in exercise has been reported to both foster social integration and be a means of maintaining existing social contacts. Specific research into the possible mechanisms for this effect, and with clinical populations, is currently lacking. This issue is of particular importance, as compared to adults without psychiatric disorders, patients with psychiatric disorders have a fourfold risk of suffering from social anxiety and adverse social interactions.41–45 Future research should focus therefore on the extent to which PAEPs in psychiatric hospitals might favorably impact on patients’ social skills.
Finally, a further result demands particular attention: participants reported wanting and needing extended vocational training, specifically as regards the state-of-the-art of PEAPs for patients with psychiatric disorders. Accordingly, one might claim that institutions such as departments of sports science, in collaboration with psychiatric institutions, might organize specific extended vocational trainings.
The strengths of the present results should be balanced against the limitations of the study. First, the present data do not reflect the current application of PAEPs in psychiatric hospitals in non-German-speaking Swiss areas, as we sought to avoid the risk of methodological issues related to the translation of the items into French, Italian, and Rhaeto-Romanic. Second, only hospitals and participants willing and able to complete the questionnaire took part on the study, and accordingly, results might also be biased. Third, the quality of the data did not allow a deeper understanding of which patients with which psychiatric disorder did participate and not participate in the PAEPs. Such a distinction would have allowed more insight into the possible relations between patients’ psychiatric characteristics (their disorders), motivation and (non-)participation in specific PEAPs. Specifically, one might assume, that for instance, the framework of PAEPs of patients with addiction disorders is different from that of PAEPs of patients with anxiety and affective disorders. Fourth, the online survey did not assess patients’ perception of how useful or detrimental PEAPs were. Finally, it is questionable to what extent domains such as relaxation techniques, physiotherapy, or far-east (meditation) techniques should be considered as PEAPs, or if they should be considered and discussed apart.
Conclusion
The pattern of results of the present online survey suggests that psychiatric hospitals of the German-speaking part of Switzerland offer a broad variety of physical activity and exercising programs to their inpatients, although only 25%–50% of inpatients take part in programs. Staff are unanimous in the view that these programs are physically and psychologically beneficial. After discharge, patients can no longer take part in these programs. Staff responsible for PAEPs state that specific extended vocational training is required to offer activities suited to patients with psychiatric disorders. Finally, given that many psychiatric patients may have motivational and volitional deficits, more systematic efforts seem warranted to increase exercise motivation and promote behavioral skills to maintain a more physically active lifestyle among inpatients in psychiatric care settings.
Acknowledgment
The entire study has been performed without external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
Deslandes A, Moraes H, Ferreira C, et al. Exercise and mental health: many reasons to move. Neuropsychobiology. 2009;59(4):191–198. | ||
Vancampfort D, Stubbs B, Ward PB, Teasdale S, Rosenbaum S. Integrating physical activity as medicine in the care of people with severe mental illness. Aust N Z J Psychiatry. 2015;49(8):681–682. | ||
Rosenbaum S, Tiedemann A, Stanton R, et al. Implementing evidence-based physical activity interventions for people with mental illness: an Australian perspective. Australas Psychiatry. 2016;24(1):49–54. | ||
Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):964–974. | ||
Knochel C, Oertel-Knochel V, O’Dwyer L, et al. Cognitive and behavioural effects of physical exercise in psychiatric patients. Prog Neurobiol. 2012;96(1):46–68. | ||
Archer T, Josefsson T, Lindwall M. Effects of physical exercise on depressive symptoms and biomarkers in depression. CNS Neurol Disord Drug Targets. 2014;13(10):1640–1653. | ||
Silveira H, Moraes H, Oliveira N, Coutinho ES, Laks J, Deslandes A. Physical exercise and clinically depressed patients: a systematic review and meta-analysis. Neuropsychobiology. 2013;67(2):61–68. | ||
Joseffson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports. 2014;24(2):259–272. | ||
Mota-Pereira J, Carvalho S, Silverio J, et al. Moderate physical exercise and quality of life in patients with treatment-resistant major depressive disorder. J Psychiatr Res. 2011;45(12):1657–1659. | ||
Pajonk FG, Wobrock T, Gruber O, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67(2):133–143. | ||
Battaglia G, Alesi M, Inguglia M, et al. Soccer practice as an add-on treatment in the management of individuals with a diagnosis of schizophrenia. Neuropsychiatr Dis Treat. 2013;9:595–603. | ||
Rosenbaum S, Vancampfort D, Steel Z, Newby J, Ward PB, Stubbs B. Physical activity in the treatment of post-traumatic stress disorder: a systematic review and meta-analysis. Psychiatry Res. 2015;230(2):130–136. | ||
Martin EC, Dick AM, Scioli-Salter ER, Mitchell KS. Impact of a yoga intervention on physical activity, self-efficacy, and motivation in women with PTSD symptoms. J Altern Complement Med. 2015;21(6):327–332. | ||
Vancampfort D, De Hert M, Stubbs B, et al. A systematic review of physical activity correlates in alcohol use disorders. Arch Psychiatr Nurs. 2015;29(4):196–201. | ||
Giesen ES, Deimel H, Bloch W. Clinical exercise interventions in alcohol use disorders: a systematic review. J Subst Abuse Treat. 2015;52:1–9. | ||
Buman MP, Hekler EB, Bliwise DL, King AC. Exercise effects on night-to-night fluctuations in self-rated sleep among older adults with sleep complaints. J Sleep Res. 2011;20(1 Pt 1):28–37. | ||
Brand S, Jossen S, Holsboer-Trachsler E, Puhse U, Gerber M. Impact of aerobic exercise on sleep and motor skills in children with autism spectrum disorders – a pilot study. Neuropsychiatr Dis Treat. 2015;11:1911–1920. | ||
Haslacher H, Michlmayr M, Batmyagmar D, et al. Physical exercise counteracts genetic susceptibility to depression. Neuropsychobiology. 2015;71(3):168–175. | ||
Moon HY, van Praag H. Muscle over mind. Cell Metab. 2014;20(4):560–562. | ||
Voss MW, Erickson KI, Prakash RS, et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav Immun. 2013;28:90–99. | ||
Chaddock-Heyman L, Erickson KI, Holtrop JL, et al. Aerobic fitness is associated with greater white matter integrity in children. Front Hum Neurosci. 2014;8:584. | ||
Knapen J, Van de Vliet P, Van Coppenolle H, et al. Comparison of changes in physical self-concept, global self-esteem, depression and anxiety following two different psychomotor therapy programs in nonpsychotic psychiatric inpatients. Psychother Psychosom. 2005;74(6):353–361. | ||
Babic MJ, Morgan PJ, Plotnikoff RC, Lonsdale C, White RL, Lubans DR. Physical activity and physical self-concept in youth: systematic review and meta-analysis. Sports Med. 2014;44(11):1589–1601. | ||
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41(1):15–28. | ||
de Wit LM, Fokkema M, van Straten A, Lamers F, Cuijpers P, Penninx BW. Depressive and anxiety disorders and the association with obesity, physical, and social activities. Depress Anxiety. 2010;27(11):1057–1065. | ||
Nyboe L, Lund H. Low levels of physical activity in patients with severe mental illness. Nord J Psychiatry. 2013;67(1):43–46. | ||
Mangerud WL, Bjerkeset O, Lydersen S, Indredavik MS. Physical activity in adolescents with psychiatric disorders and in the general population. Child Adolesc Psychiatry Ment Health. 2014;8(1):2. | ||
Brand S, Beck J, Kalak N, et al. Dream recall and its relationship to sleep, perceived stress, and creativity among adolescents. J Adolesc Health. 2011;49(5):525–531. | ||
Lindwall M, Gerber M, Jonsdottir I, Börjesson M, Ahlborg GJ. The relationships of change in physical activity with change in depression, anxiety, and burnout: a longitudinal study of Swedish healthcare workers. Health Psychol. 2014;33(11):1309–1318. | ||
Gerber M, Jonsdottir IH, Lindwall M, Ahlborg G. Physical activity in employees with differing occupational stress and mental health profiles: a latent profile analysis. Psychol Sport Exerc. 2014;15(6):649–658. | ||
Gerber M, Lindwall M, Lindegård A, Börjesson M, Jonsdottir IH. Cardiovascular fitness protects from stress-related symptoms of burnout and depression. Patient Educ Couns. 2013;93(1):146–152. | ||
Voderholzer U, Dersch R, Dickhut HH, Herter A, Freyer T, Berger M. Physical fitness in depressive patients and impact of illness course and disability. J Affect Disord. 2011;128(1–2):160–164. | ||
Krämer LV, Helmes AW, Seelig H, Fuchs R, Bengel J. Correlates of reduced exercise behaviour in depression: the role of motivational and volitional deficits. Psychol Health. 2014;29(10):1206–1225. | ||
Stubbs B, Rosenbaum S, Vancampfort D, Ward PB, Schuch FB. Exercise improves cardiorespiratory fitness in people with depression: a meta-analysis of randomized controlled trials. J Affect Disord. 2016;190:249–253. | ||
Rosenbaum S, Tiedemann A, Ward PB, Curtis J, Sherrington C. Physical activity interventions: an essential component in recovery from mental illness. Br J Sports Med. 2015;49(24):1544–1545. | ||
Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports. 2014;24(2):259–272. | ||
Rethorst CD, Wipfli BM, Landers DM. The antidepressive effects of exercise: a meta-analysis of randomized trials. Sports Med. 2009;39(6):491–511. | ||
Knapen J, Vancampfort D. Evidence for exercise therapy in the treatment of depression and anxiety. Int J Psychosoc Rehabil. 2013;17(2):75–87. | ||
Knapen J, Vancampfort D, Moriën Y, Marchal Y. Exercise therapy improves both mental and physical health in patients with major depression. Disabil Rehabil. 2015;37(16):1490–1495. | ||
Fuchs R, Goehner W, Seelig H. Long-term effects of a psychological group intervention on physical exercise and health: the MoVo concept. J Phys Act Health. 2011;8(6):794–803. | ||
Simning A, Seplaki CL, Conwell Y. The association of an inability to form and maintain close relationships due to a medical condition with anxiety and depressive disorders. J Affect Disord. 2016;193:130–136. | ||
Tak EC, van Hespen AT, Verhaak PF, Eekhof J, Hopman-Rock M. Development and preliminary validation of an observation list for detecting mental disorders and social problems in the elderly in primary and home care (OLP). Int J Geriatr Psychiatry. Epub 2015 Nov 10. | ||
Ipser JC, Wilson D, Akindipe TO, Sager C, Stein DJ. Pharmacotherapy for anxiety and comorbid alcohol use disorders. Cochrane Database Syst Rev. 2015;1:CD007505. | ||
Levy B, Tsoy E, Brodt M, Petrosyan K, Malloy M. Stigma, social anxiety, and illness severity in bipolar disorder: implications for treatment. Ann Clin Psychiatry. 2015;27(1):55–64. | ||
Lowengrub KM, Stryjer R, Birger M, Iancu I. Social anxiety disorder comorbid with schizophrenia: the importance of screening for this under recognized and under treated condition. Isr J Psychiatry Relat Sci. 2015;52(1):40–45. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


