Back to Journals » Vascular Health and Risk Management » Volume 12
The cost of inpatient death associated with acute coronary syndrome
Authors Page II R, Ghushchyan V, Van Den Bos J, Gray T, Hoetzer G, Bhandary D, Nair K
Received 8 August 2015
Accepted for publication 19 November 2015
Published 3 February 2016 Volume 2016:12 Pages 13—21
DOI https://doi.org/10.2147/VHRM.S94026
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Daniel Duprez
Robert L Page II,1 Vahram Ghushchyan,2 Jill Van Den Bos,3 Travis J Gray,3 Greta L Hoetzer,4 Durgesh Bhandary,4 Kavita V Nair1
1Department of Clinical Pharmacy, Skaggs School of Pharmacy and Pharmaceutical Sciences, University of Colorado Anschutz Medical Campus, Aurora, CO, 2College of Business and Economics, American University of Armenia, Yerevan, Armenia; 3Milliman, Inc, Denver, CO, 4AstraZeneca, US Medical Affairs, Wilmington, DE, USA
Background: No studies have addressed the cost of inpatient mortality during an acute coronary syndrome (ACS) admission.
Objective: Compare ACS-related length of stay (LOS), total admission cost, and total admission cost by day of discharge/death for patients who died during an inpatient admission with a matched cohort discharged alive following an ACS-related inpatient stay.
Methods: Medical and pharmacy claims (2009–2012) were used to identify admissions with a primary diagnosis of ACS from patients with at least 6 months of continuous enrollment prior to an ACS admission. Patients who died during their ACS admission (deceased cohort) were matched (one-to-one) to those who survived (survived cohort) on age, sex, year of admission, Chronic Condition Index score, and prior revascularization. Mean LOS, total admission cost, and total admission cost by the day of discharge/death for the deceased cohort were compared with the survived cohort.
A generalized linear model with log transformation was used to estimate the differences in the total expected incremental cost of an ACS admission and by the day of discharge/death between cohorts. A negative binomial model was used to estimate differences in the LOS between the two cohorts. Costs were inflated to 2013 dollars.
Results: A total of 1,320 ACS claims from patients who died (n=1,320) were identified and matched to 1,319 claims from the survived patients (n=1,319). The majority were men (68%) and mean age was 56.7±6.4 years. The LOS per claim for the deceased cohort was 47% higher (adjusted incidence rate ratio: 1.47, 95% confidence interval: 1.37–1.57) compared with claims from the survived cohort. Compared with the survived cohort, the adjusted mean incremental total cost of ACS admission claims from the deceased cohort was US$43,107±US$3,927 (95% confidence interval: US$35,411–US$50,803) higher.
Conclusion: Despite decreasing ACS hospitalizations, the economic burden of inpatient death remains high.
Keywords: death, acute coronary syndrome, hospitalization, cost, health resource utilization
Introduction
Acute coronary syndrome (ACS) is an umbrella term that encompasses patients with coronary heart disease (CHD) who present with either unstable angina (UA) or an acute myocardial infarction (MI) consisting of ST-segment elevation myocardial infarction (STEMI) or non-ST-segment elevation myocardial infarction (NSTEMI).1,2 ACS begins with the rupture of an unstable plaque within the coronary artery, with subsequent development of associated intravascular thrombus and potential for ischemic myocardial injury, resulting in significant morbidity and mortality. Based on data from 2009, the American Heart Association reported approximately 1.2 million hospital discharges with a diagnosis of ACS.3 Moreover, in 2015, it is estimated that 635,000 Americans will experience a new coronary attack (defined as the first hospitalized MI or CHD death) and approximately 300,000 will have a recurrent event.4,5 In terms of death, CHD was associated with one in every seven Americans in 2011, accounting for approximately 375,295 deaths, with approximately 27% of these deaths occurring in the hospital setting.4,5
The cost of hospitalization for ACS is expensive and continues to rise. In terms of direct medical expenditures, ACS costs Americans more than US$150 billion annually, with approximately 60%–75% of these costs related to hospital admission and readmission.6–8 Several studies have been published evaluating the direct and indirect costs for patients who have been admitted for ACS.6–10 However, the majority of these studies have only gauged the cost of the index hospitalization or costs at 30 days or 1 year following the index admission (eg, patients who have survived). None of these studies have directly calculated the cost of inpatient mortality for an ACS admission. The cost of inpatient death is an important consideration, as many of the large therapeutic ACS studies used to develop evidenced-based guidelines and health-system quality core measures take into account the outcome of cardiovascular mortality, which includes in-hospital death.11–17
While hospitalization and in-hospital mortality for ACS continue to decline due to implementation of medical and pharmacological interventions, the economic burden of inpatient mortality could remain high.1–2 To fill this gap in the literature regarding the cost of in-patient death due to ACS, we compared the length of stay (LOS), total admission cost, and total admission cost by day for patients who died during an ACS-related inpatient admission with a matched cohort of those who were discharged alive following an ACS-related inpatient stay.
Methods
This study was a retrospective between-group comparison of inpatient admissions with a primary diagnosis for ACS in which patients were discharged alive (survived) or died during the hospitalization. As all patient data were de-identified, this study was reviewed and determined to be institutionally exempt.
Data source
The data for the study were obtained from the Truven Health MarketScan dataset. This data set includes medical, pharmacy, and enrollment claims from 100 employers nationwide, representing 40 million commercially insured patient lives.
Cohort identification
The study period was from January 1, 2009 to December 31, 2012. The unit of analysis for the study was inpatient admission claims, rather than patients. Inpatient hospitalizations with ACS in the primary diagnosis field (henceforth referred to as the index admission date) using International Classification of Diseases – 9th Revision, Clinical Modification (ICD 9) codes for STEMI, NSTEMI, and UA (Table S1) during the study period were initially identified. From this group, the sample was narrowed further to admissions for patients who had a minimum of 6 months of continuous enrollment prior to their index ACS admission. The study cohorts consisted of two groups of admissions: those for which the patients died during the ACS admission and those for which the patients survived and were discharged alive following the hospitalization. Deaths were classified based on the Truven Health MarketScan discharge status. Admissions with a discharge status of “death” (the deceased cohort) were matched to remaining admissions (the survived cohort) on age categories (under 40, 40–44, 45–49, 50–54, 55–59, 60–64, or ≥65 years), sex, year of admission (2009, 2010, 2011, and 2012), CCI score (0, 1, 2, 3, 4, 5, or ≥6), and the presence of any revascularization – percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) – in the 6 month period prior to the index admission date to ensure statistically comparable samples of the deceased and survived cohorts. A one-to-one matching was performed on the mentioned variables. Only one claim from the deceased cohort was not matched to an equivalent claim from the survived cohort; thus, the final sample consisted of two cohorts: 1,320 admissions for the deceased cohort, and 1,319 matched admissions for the survived cohort. This resulted in 1,320 patients in the deceased cohort and 1,319 patients in the survived cohort.
Measures
Length of stay
The LOS for an ACS hospitalization for the survived and deceased cohorts was determined.
Cost of hospitalization
The total cost associated with an ACS hospitalization was determined, which included all costs incurred during the admission by claim. The total cost was also determined based on diagnosis of STEMI and NSTEMI.
Cost of hospitalization by day of discharge/death
The total cost of an ACS hospitalization for the survived and deceased cohorts, which included all costs incurred by claim during the admission, was stratified by the day of discharge/death. Stratification was done from 2 to 6 or more hospital days.
Analysis
Both descriptive and adjusted analyses were conducted between deceased and survived cohorts.
The unadjusted analyses compared means for all specified outcome variables. Depending on the type of outcome variable, different statistical models were employed for the adjusted regression analyses to estimate the incremental effect of ACS-related inpatient mortality. A generalized linear model with log transformation was used to estimate the additional cost (the incremental effect of ACS-related inpatient mortality) for the deceased compared with the survived cohort. The same model was also used to estimate the mean incremental cost of ACS-related hospitalization for each day of hospitalization. A negative binominal regression model was used to estimate the differences in the expected ACS LOS between the two cohorts. The explanatory variables for all models included at baseline (in the 6 month period prior to the index admission date): sex; CCI score; age categories (45–49 years, 50–54 years, 55–59 years, and 60–64 years); region of the United States; type of insurance coverage (health maintenance organization, point of service, preferred provider organization), presence of revascularization procedures (PCI or CABG); and industry employment (manufacturing, transportation, services; see Table S2 for revascularization codes). All costs were inflated to 2013 dollar values.
Results
Study population
From January 1, 2009 to December 31, 2012, a total of 99,924 claims (n=97,746) for an ACS admission were identified, of which 1,320 claims for deceased patients (n=1,320) were matched to claims for patients who survived their ACS admission (n=1,319; Figure 1). Table 1 shows that the baseline characteristics of age groups, sex, year of admission, CCI score, and prior revascularization were well-matched between deceased and survived cohorts. The majority of admissions were for male patients (68%) with a mean age of 57 years residing within the southern United States (41%–45%). The type of medical coverage varied between cohorts, with the majority of admissions for patients having point of service plans (60%–63%). Between 58% and 60% of admissions were for patients who worked within the oil and gas, mining, retail trade, finance, insurance, real estate, construction, wholesale, agriculture, forestry, or fishing industry.
  | Figure 1 Flow diagram of survived and deceased cohort allocation. |
Six months prior to hospitalization, the number of admissions for patients who had experienced a previous ACS event varied between groups. Of admissions in the deceased cohort (n=112), 8% had a previous diagnosis of STEMI, whereas 14% of admissions in the survived cohort (n=180) were for patients who had a history of an NSTEMI (Table 1). Revascularization procedures and prior all-cause hospitalization during this time period were low for both groups: 6%–7% (P=0.996) had a PCI, 1% CABG (P=0.853), and 24%–26% a prior hospitalization (P=0.210). Compared with the survived cohort, a greater number of patients in the deceased cohort had a history of cardiac arrhythmias (8% vs 14%, P<0.001, respectively) and heart failure (HF) (9% vs 12%, P=0.012, respectively).
During hospitalization, the majority of admissions for patients in the deceased cohort carried a diagnosis of STEMI (64%), compared with only 33% in the survived cohort (P<0.001).
Although no difference existed in the number of CABG procedures during the admission between groups, 57% in the survived cohort had a PCI compared with 44% in the deceased cohort (P<0.001). However, when stratifying based on the diagnosis of STEMI and NSTEMI, the majority of patients with STEMI received PCI in both the deceased (57%) and survived cohorts (84%) compared to patients with NSTEMI (22% vs 46%, P<0.001, respectively; Figure 2). Patients in the NSTEMI cohort had a slightly higher percentage of CABG (13%) compared to patients with STEMI (7%–9%). The incidence of both cardiac arrhythmias (69% vs 22%, P<0.001) and HF (36% vs 15%, P<0.001) was significantly higher during hospitalization for both the deceased and survived cohorts, respectively. In the deceased cohort, stroke increased from 3% prior to admission to 13% during hospitalization.
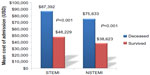
Unadjusted admission costs and total length of stay
The unadjusted total mean admission cost was US$82,965±US$138,104 for the deceased cohort, compared with US$40,568±US$53,415 for the survived cohort (P<0.001; Figure 3A). The mean LOS was also significantly longer for those who died (7.5±9.9 days) compared with those who were discharged alive (5.2±4.9 days; P<0.001; Figure 3B).
  | Figure 3 Unadjusted mean cost of an ACS inpatient admission (A) and length of stay (B) for the deceased and survived cohorts. |
When evaluating in-hospital death or discharge by day, the unadjusted mean cost for those who died climbed from US$32,285±US$29,732 on day 1 to US$60,817±US$75,393 by day 4 and remained relatively constant through day 6 (US$65,613±US$49,397; Figure 4). A similar trend was seen in those who survived. The mean unadjusted cost at day 1 was US$14,779±US$11,690, which climbed to US$31,914±US$20,116 by day 5 and then increased to US$50,554±US$40,885 on day 6. However, on all days of discharge/death, the unadjusted mean cost of hospitalization was consistently higher on each day for the deceased cohort compared with the survived cohort and was statistically significant from days 1 to 5 (P<0.001; Figure 4).
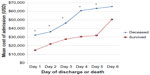  | Figure 4 Unadjusted mean cost of an acute coronary syndrome admission by day of discharge/death. |
When stratifying based on the diagnosis of STEMI and NSTEMI, mean costs of admission were higher for patients with STEMI compared to NSTEMI particularly for with the deceased cohort (Figure 5). Compared to the survived cohort (n=434) with a diagnosis of STEMI, those in the deceased cohort (n=841) had a 1.8-fold higher mean admission cost (US$48,229±US$74,110 vs US$87,392±US$148,838, P<0.001). Similarly, findings were seen in those with NSTEMI, in which compared to those who survived (n=812), those who died (n=475) during their admission had a 1.9-fold higher mean admission cost (US$38,623±US$39,665 vs US$75,633±US$117,020, P<0.001).
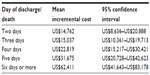
Adjusted admission costs
Compared with the survived cohort, the adjusted mean incremental total cost of an ACS admission was US$43,107±US$3,927 (95% CI: US$35,411–US$50,803) higher for the deceased cohort. When stratified by day of discharge/death, the adjusted mean incremental cost was US$14,762 (95% CI: US$8,636–US$20,888), US$15,037 (95% CI: US$10,361–US$19,713), US$22,819 (95% CI: US$15,217–US$30,421); US$31,675 (95% CI: US$20,728–US$42,623), and US$62,411 (95% CI: US$41,643–US$83,178) higher in the deceased cohort for the day of discharge/death at days 2, 3, 4, 5, and 6, respectively, compared with the claims for the survived cohort (Table 2).
Discussion
To our knowledge, our study is the first to evaluate the economic ramifications of inpatient death associated with ACS within a commercially insured population. Although many economic analyses have evaluated the direct and indirect costs of hospitalization associated with ACS, particularly in a Medicare population, these studies have not determined an estimate of the claim cost associated with inpatient death when ACS was a primary diagnosis.6–10 We found that those with a primary diagnosis of ACS who died were more likely to have a STEMI and carried a high comorbidity burden, especially HF and cardiac arrhythmias, when compared with those who survived their ACS hospitalizations. Additionally, expected LOS for admissions during which patients died was 47% higher than those admissions during which patients survived. Compared with admissions during which the patient survived, the adjusted mean incremental total cost of an ACS admission was US$43,107±US$3,927 higher in claims for deceased patients. The adjusted mean incremental total cost of an ACS admission continued to climb for each additional hospital day, increasing approximately twofold by day 6. When taking into account ACS diagnosis, the mean cost of admission for those who died during their admission was approximately twofold higher compared to those who survived for both STEMI and NSTEMI.
In terms of characteristics of patients who died, our data are consistent with the literature, as approximately one-third of patients with STEMI die within 24 hours of onset of ischemia compared with only 15% of patients with UA/NSTEMI who either die or experience a reinfarction within 30 days of hospitalization.18 Cardiac arrhythmias, especially atrial fibrillation (AF), and HF are both common yet deadly comorbidities associated with ACS. In an analysis of the Global Registry of Acute Coronary Events registry, Steg et al found that the presence of HF in patients with ACS increased hospitalization by 2 days compared with those without HF (9 vs 7 days, P<0.0001, for STEMI; 8 vs 6 days, P<0.0001, for NSTEMI; and 5 days for both, P=0.317, for UA, respectively).19 Furthermore, HF on admission was associated with a fourfold increase in crude hospital mortality rates (12.0% vs 2.9%; odds ratio: 4.6; 95% CI: 3.85–5.40). This increase in mortality was seen regardless of an ACS subset. For AF, Jabre et al20 found in a meta-analysis of 43 studies involving 278,854 patients with MI that AF was associated with at least a 40% increase in mortality compared with that in control patients in normal sinus rhythm.19 This finding persisted regardless of the timing of AF development.20
Additionally, we found that patients in the deceased cohort had a significantly lower rate of PCI when compared to those who survived (44% vs 57%, P<0.001). However, this finding might be expected as patients within the deceased cohort had a statistically higher rate of comorbid conditions such as cardiac dysrhythmias (P<0.001), HF (P<0.001), and chronic kidney disease (P=0.023), which could preclude them from being an eligible candidate for revascularization in lieu of conservative medical management.1,2 When stratified based on the diagnosis of STEMI and NSTEMI, our data are consistent with the 2011 Acute Coronary Treatment and Intervention Outcomes Network – Get with the Guidelines registry, which consisted of 119,967 patients 18 years or older who had been admitted with a diagnosis of STEMI or NSTEMI.21 Based on patients eligible for revascularization, 87.9% of patients with STEMI received PCI during admission compared to 49% with NSTEMI in the registry. Within our analysis, 84% of patients with STEMI and 46% of patients with NSTEMI in the survived cohort received PCI during their ACS admission.
Finally, the mean LOS was significantly longer for those who died (7.5±9.9 days) compared with those who were discharged alive (5.2±4.9, P<0.001). In terms of LOS, our survived cohort findings are consistent with national data. In a recent analysis of Medicare data for all fee-for-service patients 65 years or older with a diagnosis of ACS, Krumholz et al estimated that the length of hospitalization for STEMI/NSTEMI to have decreased from 6.5 days in 1999 to 5.3 days in 2011.22
Although several analyses have suggested a trend toward a reduction in ACS hospitalization and in-hospital mortality, having an estimate of the direct cost of inpatient death is an important consideration at many levels.22–24 First, several of the clinical trials and analyses evaluating lifesaving pharmacotherapies and medical interventions in ACS have used inpatient mortality as a primary end point. Therefore, having a projected cost of in-patient mortality in patients with ACS, provides an estimate to gauge such benefits. For example, in the Gruppo Italiano per lo Studio della Steptochinasi nell’Infarto Micardico trial, streptokinase reduced in-hospital mortality by 18% when compared with standard of care (P=0.0002) and by 51% when administered within less than 1 hour of chest pain (P=0.0001).25 Furthermore, many of the clinical trials of pharmacotherapeutic agents that are used acutely within the hospital setting and continued at discharge have used cardiovascular mortality as a composite of their primary outcome end points. In the Platelet Inhibition and Patient Outcomes trial, ticagrelor compared with placebo was associated with a 16% relative risk reduction in the composite end point of death from vascular causes, MI, or stroke (P<0.001).14 Finally, in a meta-analysis of 23 trials consisting of 7,739 patients with STEMI that compared primary PCI with thrombolytic therapy, primary PCI resulted in a reduced short-term (4–6 weeks) overall mortality (P=0.0002) and long-term (6–18 months) overall mortality (P=0.0019) compared with fibrinolytic therapy.16,17
Second, from a policy perspective, the Centers for Medicare and Medicaid Services uses 30-day mortality for MI as a quality core measure to compare hospitals.26 For example, the 30-day Centers for Medicare and Medicaid Services mortality measure currently includes deaths regardless of whether the patient dies while still in the hospital or after discharge.27 With this in mind, having an estimate of the cost of in-hospital deaths that are due to ACS provides further evidence that the economic burden of ACS inpatient death still remains high. These data also suggest that additional strategies to potentially reduce these costs should be explored such as better management of high-risk patients prior to admission through disease and care management models, as well as, potential implementation of evidence-based therapies and addressing comorbid conditions during admission.10,28
Nonetheless, our analysis does have the following limitations. First, although ACS was the primary admission and discharge diagnosis for both cohorts, other comorbidities could have contributed to the death, ie, multiorgan failure or sudden cardiac death, which may not have been captured as a primary diagnosis for the discharge status. Additionally, as we are using claims data, we could not ascertain the exact timing of a patient’s ACS symptoms, time to possible reperfusion, and patient-level risk factors such as blood pressure, weight, electrocardiogram changes, elevations in biomarkers, which could influence a patient’s prognosis.1–2 However, we were able to match between groups based on age, comorbidity burden through the chronic condition index and previous history of coronary artery disease through the presence of any previous revascularization prior to admission. Second, we did not match the deceased and survived cohorts for ACS subtype, as the uneven number of patients with STEMI, NSTEMI, and UA did not allow for an even matching across both cohorts. Third, in the adjusted analyses of the outcomes of interest, we did not control for specific comorbidities such as HF or cardiac arrhythmias that occurred either in the baseline period or during the ACS admission that could contribute to death. Rather, we took into account the total comorbidity burden through the CCI score. Also, within the survived cohort, we did not follow these patients longitudinally after discharge and the possibility exists that these patients could have been readmitted. Fourth, we also did not control all-cause prior hospitalization in the 6 month baseline period (prior to the index admission date), which has been associated with increased mortality for ACS patients.29 However, our study population did not show any differences for this measure between the two cohorts (see Table 1). Finally, while total mean cost of hospitalization was evaluated, we were not able to identify specific contributors to these additional costs. The nature of the claim data only allowed us to determine the bundled cost for a total hospital admission. Additionally, the database utilized was not an inpatient database.
Conclusion
In-hospital death associated with ACS is extremely costly. Our study described critical and previously unknown characteristics of an ACS hospital admission for patients who survived compared with those who died during the admission. Our findings demonstrate the economic consequences of in-hospital mortality for ACS patients. Additional studies are needed in this population to determine if better management during an ACS admission is needed or if other approaches such as care management programs prior to admission can potentially reduce in-patient mortality-associated hospitalizations for ACS which may in turn impact costs.
Disclosure
Dr Hoetzer and Mr Bhandary are employed by AstraZeneca. All other authors report no conflicts of interest in this work.
References
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-st-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139–e228. | |
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of st-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):485–510. | |
Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics, 2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. | |
Go A, Mozaffarian D, Roger V, et al. Heart disease and stroke statistics, 2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. | |
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics, 2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. | |
Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care. 2009;15(2 Suppl):S36–S41. | |
Page RL 2nd, Ghushchyan V, Gifford B, et al. The economic burden of acute coronary syndromes for employees and their dependents: medical and productivity costs. J Occup Environ Med. 2013;55(7):761–767. | |
Zhao Z, Winget M. Economic burden of illness of acute coronary syndromes: medical and productivity costs. BMC Health Serv Res. 2011;11:35. | |
Johnston SS, Curkendall S, Makenbaeva D, et al. The direct and indirect cost burden of acute coronary syndrome. J Occup Environ Med. 2011;53(1):2–7. | |
Wang G, Zhang Z, Ayala C, Dunet D, Fang J. Costs of hospitalizations with a primary diagnosis of acute myocardial infarction among patients aged 18–64 years in the United States. In: Gaze D, editor. Ischemic Heart Disease. 2013. Available from: http://www.intechopen.com/books/ischemic-heart-disease/costs-of-hospitalizations-with-a-primary-diagnosis-of-acute-myocardial-infarction-among-patients-age. Accessed October 3, 2015. | |
Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992;327(10):669–677. | |
Kober L, Torp-Pedersen C, Carlsen JE, et al. A clinical trial of the angiotensin-converting-enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril cardiac evaluation (trace) study group. N Engl J Med. 1995;333(25):1670–1676. | |
Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357(20):2001–2015. | |
Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–1057. | |
The Beta-Blocker Heart Attack Trial Investigators. A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA. 1982;247(12):1707–1714. | |
Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with st-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004;110(9):e82–e293. | |
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20. | |
Turpie AG. Burden of disease: medical and economic impact of acute coronary syndromes. Am J Manag Care. 2006;12(16 Suppl):S430–S434. | |
Steg PG, Dabbous OH, Feldman LJ, et al. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the global registry of acute coronary events (GRACE). Circulation. 2004;109(4):494–499. | |
Jabre P, Roger VL, Murad MH, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123(15):1587–1593. | |
Masoudi FA, Ponirakis A, Yeh RW, et al. Cardiovascular care facts. A report from the national cardiovascular data registry: 2011. J Am Coll Cardiol. 2013;62(21):1931–1947. | |
Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130(12):966–975. | |
Wang OJ, Wang Y, Chen J, Krumholz HM. Recent trends in hospitalization for acute myocardial infarction. Am J Cardiol. 2012;109(11):1589–1593. | |
Talbott EO, Rager JR, Brink LL, et al. Trends in acute myocardial infarction hospitalization rates for US States in the CDC tracking network. PLoS One. 2013;8(5):e64457. | |
GISSI Investigators. Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Gruppo Italiano per lo Studio della Streptochinasi nell’infarto Miocardico (GISSI). Lancet. 1986;1(8478):397–402. | |
Centers for Medicare and Medicaid. Outcome Measures. 2014. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html. Accessed August 5, 2015. | |
Centers for Medicare and Medicaid. 30-day unplanned readmission and death measures. 2015. Available at: http://www.medicare.gov/hospitalcompare/Data/30-day-measures.html. Accessed August 6, 2015. | |
Ciccone MM, Aquilino A, Cortese F, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297–305. | |
Bawamia B, Mehran R, Qiu W, Kunadian V. Risk scores in acute coronary syndrome and percutaneous coronary intervention: a review. Am Heart J. 2013;165(4):441–450. |
Supplementary materials
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.