Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 15
The Correlation of Pain, Psychological Aspects, and Sleep in Fibromyalgia: A Cross-Sectional Analysis
Authors Meresh ES , Xu S, Palomino A , Artin H, Padiyara J, Stasieluk C, Khurshid A
Received 28 September 2023
Accepted for publication 13 December 2023
Published 19 December 2023 Volume 2023:15 Pages 237—246
DOI https://doi.org/10.2147/OARRR.S438931
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Edwin S Meresh,1 Sarah Xu,2 Angelina Palomino,2 Hewa Artin,2 Julia Padiyara,3 Conrad Stasieluk,1 Abid Khurshid4
1Department of Psychiatry, Loyola University Medical Center, Maywood, IL, 60153, USA; 2Loyola Stritch School of Medicine, Maywood, IL, 60153, USA; 3Loyola Medicine Center for Sleep Disorders, Loyola University Medical Center, Maywood, IL, 60153, USA; 4Pulmonary Medicine, Loyola University Medical Center, Maywood, IL, 60153, USA
Correspondence: Edwin S Meresh, Email [email protected]
Background: This pilot study measures pain perception, somatosensory amplification and its relationship to health anxiety in patients with fibromyalgia (FM) and patients with FM and obstructive sleep apnea (OSA); this study also examines the effects of OSA on pain perception in patients with FM.
Methods: In this pilot study, patients diagnosed with FM or FM and OSA, completed three self-reported questionnaires: Short-Form McGill Pain Questionnaire (SF-MPQ), Somatosensory Amplification Scale (SSAS), and Illness Behavior Questionnaire (IBQ). Sleep study results were analyzed. Scores were summarized using medians and interquartile ranges and are compared using Wilcoxon rank sum tests.
Results: Overall FM (n = 25), female n=23 male n=3 mean age, 57.48 years. OSA n=17 (68%) and 8 (32%) were not. The SF-MPQ Sensory sub-scale scores and the SF-MPQ overall scores differed significantly between patients with and without OSA. The SF-MPQ Sensory sub-scale scores were significantly lower for patients with OSA (p=0.03), as were SF-MPQ overall scores (p=0.04). SSAS overall scores and IBQ overall scores did not differ significantly by OSA diagnosis. Correlations of the different dimensions of IBQ with SSAS and mean number of diagnoses in FM and FM+OSA, mean number of diagnoses in problem list of SSAS ≤ 30 was 29.5, mean number of diagnoses in SSAS ≥ 30 was 34.9.
Discussion: Developing a better understanding of the effects of OSA on pain perception in patients with FM is needed for improved health status. More research is needed to see if higher pain perception and SSAS score lead to increased health care utilization and to evaluate the relationship between untreated disordered sleeping and pain perception in patients with FM.
Conclusion: Our findings highlight the need for more research to evaluate the relationship between treated and untreated disordered sleeping, pain perception, somatization and illness behavior in the health status of individuals with FM.
Keywords: fibromyalgia, obstructive sleep apnea, pain perception, symptom amplification, illness behavior
Introduction
Fibromyalgia syndrome (FMS) is a disabling chronic pain disorder associated with high levels of pain and suffering. Individuals often experience symptoms of widespread pain, mood changes, sleep disturbances, and fatigue. Co-morbidities such as IBS, headache, and sleep disorders are often coupled with and complicate FM treatment.1 Patients report experiencing functional limitations which can affect productivity and ultimately economic costs.2 The impact of FMS on health status can be assessed through tools that translate a patient’s qualitative experience into objective measures. Quality and severity of FM pain symptoms can be evaluated through self-assessments including the Short-Form McGill Pain Questionnaire (SF-MPQ), Somatosensory Amplification Scale (SSAS), and Illness Behavior Questionnaire (IBQ).3–5
Disordered sleeping is commonly experienced in FMS and is part of the American College of Rheumatology’s diagnostic criteria for FMS. Symptoms are specified as waking unrefreshed, fatigue, tiredness, and insomnia.6 Although sleep recording is not part of the routine evaluation in patients with FMS, polysomnography may disclose primary sleep disorders in these patients. A research study of a general rheumatology practice found that a large proportion of women with FMS also had sleep-disordered breathing and that FMS may also be a marker for obstructive sleep apnea (OSA) in males.7–10 It has also been recommended that patients with FMS receive sleep study referrals as part of standard care.11
The relationship between FMS and OSA is important because research findings suggest that disordered sleep may worsen the sensation of pain.12 Loss of Rapid Eye Movement (REM) sleep is associated with hyperalgesia suggesting sleep abnormalities and pain perception are related.13 The relationship between REM sleep loss and hyperalgesia is complex but is hypothesized to be related to the cholinergic system, which is involved in both REM sleep and pain perception in addition to other neurotransmitter interaction.13 Increased REM sleep correlates to improved health, with most individuals averaging 70 min per night which is 25% of total sleep time (TST).14–16 Additionally, when FMS patients perceived sleep as restful, they reported improved daytime symptoms.6 Unique Electroencephalograph (EEG) findings have also been observed in patients with OSA and FMS with a study identifying abnormalities in Non-Rapid Eye Movements (NREM).17 FMS patients with undiagnosed OSA may be at risk of worse pain symptoms given untreated OSA and disordered sleeping. It is important to determine the pain and psychological correlates of FMS patients who also have OSA (NREM and REM apneas and decreased REM apnea) and see if pain and psychological factors are the same, less or increased in fibromyalgia patients without OSA.
Due to the psychiatric co-morbidities of both OSA and FMS, patients are commonly under the care of psychiatrists and pain specialists and can be taking multiple psychotropic medications, including benzodiazepines and opioids. FMS symptoms are often managed with benzodiazepines and opioids, both known to decrease REM sleep.18 This presents a problem given that OSA may be the cause of sleep problems experienced in patients with FMS and that benzodiazepines are contraindicated in OSA. These patients may inappropriately end up on benzodiazepines further complicating health status. Developing a better understanding of the effects of OSA on pain perception in patients with FMS for improved health status with appropriate treatment and avoid unnecessary polypharmacy.
This study aims to 1) determine the relationship between FMS and OSA comorbidities with pain perception; 2) determine the behavior and healthcare utilization of FMS patients. Based on previous literature and our clinical experience, this study hypothesized that patients with FMS and OSA have increased pain perception in comparison to patients with FMS alone and furthermore, Continuous Positive Airway Pressure (CPAP) therapy can help treat OSA and thus will decrease pain perception in patients with FMS and OSA. We also hypothesize that patients with higher SSA will have increased illness behavior and healthcare utilization.
Methods
Institutional Board Approval was obtained for this study. The Institutional Review Board of Loyola University Medical Center approved the study. Patients included in our study had a diagnosis of FM or FM and OSA and were attending routine appointments from 2017 to 2020 at the Loyola University Chicago Department of Psychiatry or LUMC Burr Ridge Sleep Clinic. All participants were age 18 years or older and met the ICD-10 diagnostic criteria for FMS in their patient condition list, reported and assessed by a previous clinician. FM codes (ICD 10: M79.7 and ICD 9: 729.1) and OSA codes (ICD 10: G47.33 and ICD 9: 327.23) were used to identify FM patients diagnosed with OSA between 2012 and 2018. Patients considered to have fibromyalgia were diagnosed by their primary care physician based on a clinical evaluation, physical exam, and ruling out conditions with similar symptoms.
Patients considered to have OSA were diagnosed after a sleep study (polysomnography). Individuals with OSA met the ICD-9 or ICD-10 diagnostic criteria for OSA as reported by a previous pulmonologist or a sleep specialist. For FM patients without OSA, available sleep studies were reviewed and negative results were confirmed. FM patients without OSA patients in whom sleep study was not done, we confirmed that these patients were not referred (no referral identified).
Patients diagnosed with obstructive sleep apnea without diagnosis of fibromyalgia were excluded. Patients with pain-related symptoms like pelvic floor dysfunction and chronic back pain were excluded if there was no explicit fibromyalgia diagnosis in their patient chart. At the end of their visit and after informed consent, participants were invited to complete three self-reported questionnaires, SF-MPQ, SSAS, and IBQ, assessing the quality and severity of their pain symptoms. Informed consent was obtained from the study participants. Guidelines outlined in the Declaration of Helsinki were followed.
The SF-MPQ has 15 descriptors of pain including 11 from sensory categories and 4 from affective categories. Descriptors of pain are rated on an intensity scale of 0 = None, 1 = Mild, 2 = Moderate, 3 = Severe.3 Total scores ranging from a sum of 0 to 45. Pain scores are derived from the sum of the intensity rank values of the words chosen for sensory, affective and total descriptors are used to compose pain scores. The SF-MPQ also includes the Present Pain Intensity (PPI) index of the standard MPQ and a visual analogue scale (VAS).3
SF-MPQ is reliable and valid.19–22 The SASS scale is a 10-item assessment of the tendency to experience a somatic sensation as intense, noxious, and disturbing. The respondent rates the degree to which each statement is “characteristic of you in general” on a scale of one to five. Total scores range from a sum of 10 to 50, with high scores indicate a greater somatic sensation.4 SASS is reliable and valid.23 The IBQ consists of 62 yes or no questions assessing patient’s attitudes, ideas, affects, and attributions concerning their illness.4 IBQ is reliable and valid.24 Subjects were informed that they could stop any of the questionnaires if they became uncomfortable, fatigued, or bored. In addition to survey responses, name, visit date, and diagnosis of FM or FM and OSA were recorded. After data collection, information was entered and stored in REDcap. The SF-MPQ, including sensory sub-scale scores, affective sub-scale scores, and total overall scores, the SSAS overall scores, and the IBQ overall scores were all calculated as simple arithmetic sums of all corresponding survey items for each respective survey. Scores are summarized using medians and interquartile ranges and are compared using Wilcoxon rank sum tests. From the IBQ, 14 questions are associated with the Whiteley Index of Hypochondriasis and 5 questions are associated with Psychological vs Somatic perception of illness. Available sleep study results of FM and OSA undergoing CPAP therapy and their MPQ score were analyzed retrospectively.
Results
Demography: In this sample n=25 (female n=23, male n=3). Mean age: 57.48 with FM, 17 (68.00%) were also diagnosed with OSA (female n=14, male n=3), and 8 (32.00%) were not (FM alone) (female n=8) (Table 1).
 |
Table 1 Demographics of Included Fibromyalgia Patients w/OSA, Median SASS and IBQ Score |
Pain Perception
SF-MPQ Overall Scores (Table 2)
Overall, both groups: Median: 24.00 (IQR 18.00–29.00).
 |
Table 2 Fibromyalgia Patient’s with and without Sleep Apnea Median Scores of Self-Reported Current Pain Sliding Scale, SF-MPQ, SSAS, and IBQ Questionnaires |
Individuals with both FM and OSA (Median: 21.00, IQR: 15.00–25.00).
Individuals with FM only had a higher score (Median: 28.00, IQR: 26.00–31.00).
Specifically, the median SF-MPQ overall score was higher for individuals with FM only (patients with no OSA) (Median: 28.00, IQR: 26.00–31.00) than individuals with both FM and OSA (Median: 21.00, IQR: 15.00–25.00). This difference was statistically significant (p=0.04).
SF-MPQ Affective Sub-Scale Scores (Table 2)
Overall: 6.00 (3.00–9.00).
FM+OSA: 4.00 (3.00–9.00).
FM only: 7.00 (5.50–9.50).
p = 0.19.
SF-MPQ Sensory Sub-Scale Scores (Table 2)
Overall: 18.00 (14.00–21.00)
FM+OSA:15.00 (9.00–20.00)
FM Only: 20.50 (19.50–23.50)
SF-MPQ sensory sub-scale scores were significantly lower for patients diagnosed with OSA (p=0.03).
SF-MPQ Present Pain Intensity (Table 3)
Overall, most patients described their present pain intensity as distressing (52.00%).
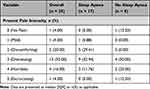 |
Table 3 Sleep Apnea and Present Pain Intensity of Fibromyalgia Patients with and without OSA |
FM+OSA
Among patients with OSA, the most frequently reported present pain intensity was distressing (52.94%), followed by discomforting (29.41%), horrible (11.76%), mild (5.88%), and then no pain (0.00%) and excruciating (0.00%).
OSA (FM only):
Among patients without OSA (FM only), the most frequently reported present pain intensity (Table 3) was distressing (50.00%) followed by horrible (25.00%), then no pain (12.50%) and excruciating (12.50%), and then mild (0.00%) and discomforting (0.00%).
SF-MPQ Visual Analog Current Pain Sliding Scale Score
Overall, for all participants, the median visual analog current pain sliding scale score was 5.90 (3.30–6.80).
The median visual analog current pain sliding scale score was higher for patients without OSA (FM only) (Median: 6.60, IQR: 4.60–7.10) than for patients with an OSA diagnosis (Median: 4.70, IQR: 3.30–6.50). However, this difference was not statistically significant (p=0.41).
SSAS Score (Table 2)
The SSAS overall score had a median (IQR) of 32.00 (29.00–36.00).
FM+OSA: 32.00 (28.00–36.00)
FM Only: 32.50 (30.50–36.50)
p=0.64
IBQ Score (Table 2)
Overall: 34.00 (30.00–42.00)
FM+OSA: 31.00 (29.00–40.00)
FM only: 38.50 (31.00–42.50)
IBQ overall score in participants with FM only (Median: 38.50, IQR: 31.00–42.50) was higher than individuals with both FMS and OSA (Median: 31.00, IQR: 29.00–40.00). However, this difference was not statistically significant (p=0.25).
SSAS overall scores and IBQ overall scores did not differ significantly by OSA diagnosis.
Correlations of the Different Dimensions of IBQ with SSAS (Table 4)
In the terms of correlations of the different dimensions of IBQ with SSAS in FM and FM+OSA patients, the SSAS diagnosis were group in two groups, SSAS ≤30 and SSAS ≥30. Mean number of diagnoses in problem list of SSAS ≤30 was 29.5 (Table 4). Mean number of diagnoses in problem list of SSAS ≥30 was 34.9. SSAS ≤30 (n=9) had a mean score of 25.22; the Whiteley Index of Hypochondriasis had a mean of 6.11; and the Psychological vs Somatic perception of illness had a mean of 1.88. SSAS score ≥30 (n=16) had a mean score of 34.81; the Whiteley Index had a score of 10.12 which was a 65.63% increase compared to the scores ≤30; the Psychological vs Somatic perception of illness mean was 3.12 which was a 65.96% increase from the SSAS score ≤30.
 |
Table 4 Stratified SSAS Scores and Comparisons in Mean Number of Diagnosis, Whitely Index, and Psychological vs Somatic Perception in FM and FM+OSA Patients |
Polysomnography Data of Categorized Patients into FM with OSA Group or FM Only Group (Table 5)
For FM and OSA patients (15 available results), average apnea-hypopnea index (AHI) was 16.53 events/hour. Average total sleep time (TST) was 293.47 minutes. Average rapid eye movement (REM) latency was 206.64 minutes. Average Stage N1 sleep was 67.02 minutes. Average Stage N2 sleep was 176.55 minutes. Average Stage N3 sleep was 16.17 minutes. Average REM sleep was 35.7 minutes, and average REM % of TST was 11.28% (Table 5).
 |
Table 5 Polysomnography Data of Categorized Patients into FM with OSA Group or FM Only Group |
For FM only patients (4 available results), average AHI was 1.775 events/hour. Average TST was 348.75 minutes. Average REM Latency was 133.75 minutes. Average Stage N1 sleep was 27.56 minutes. Average Stage N2 sleep was 233.7 minutes. Average Stage N3 sleep was 35.5 minutes. Average REM sleep was 50.93 minutes, and average REM % of TST was 14.33% (Table 5).
Discussion
Our study has brought some light to the different pain experiences of individuals with both FM and OSA when compared to individuals with FM only. In FM only patients, we found that SSAS could be useful as a tool to assess somatic symptom attribution and health care utilization. Furthermore, by using the SF-MPQ, we found that sensory and affective pain levels were significantly lower for our study participants with both FM and OSA.
Individuals with OSA in our study had a confirmed ICD-9 or ICD-10 OSA diagnosis. Given that their sleep disorder was identified and diagnosed, it is likely that they were also receiving standard treatment of OSA through CPAP. Marvisi et al reported that Fibromyalgia responds to CPAP therapy.25 Given the potential of chronic opioid use in patients with FM, studies are needed to see if treatment of OSA with CPAP may be a nonpharmacological alternative to pain management
Further assessment is necessary to see if higher SSAS scores lead to increased health care utilization. Additionally, future research in sleep patterns between individuals with FM to individuals with both FM and OSA before and after CPAP treatment may provide a better understanding of REM impact on pain perception in FM patients.
Our findings may be limited due to our sample size and small geographic region. As this is a pilot study, a sample size was not calculated, and this study was performed in order to determine feasibility. Patients were not categorized based on opioid or benzodiazepine use which could potentially confound their pain assessments. Alternatively, for the diagnosis of FM, patients considered to have FM were diagnosed by their primary care physician based on a clinical evaluation, physical exam and ruling out conditions with similar symptoms. In this pilot study, instruments that assess function or quality of life like Fibromyalgia Impact Questionnaire was not used. Furthermore, because this study retrospectively analyzed sleep study results, we are unable to make conclusive statements on whether OSA or CPAP usage contributed to the decreased pain perception results of FM patients with OSA, although we hypothesize based on prior research results CPAP usage is a likely cause. Participants were not screened for the presence of depression, anxiety, level of fatigue, and impact of FM on their function and quality of life. Another limitation is not looking at other sleep disturbances and other aspects that greatly affect sleep and pain perception. Future studies should address these while looking at the OSA. Future prospective study must measure perception of sleep.
Did OSA led to increased pain in FM or is OSA protective or decreases pain are factors raised by the preliminary findings of this pilot study. Only a prospective study with a bigger n can address this in FM pts with OSA. To address limitations in this study, a larger study with sample size and power is required to allow for broader assessment. A prospective study could include a greater number of patients with FM only, and screen these patients for sleep difficulties such as baseline snoring. If they qualify, patients can be referred to a sleep study. These patients would then be separated into two groups, patients with a positive sleep study for OSA, and patients with a negative sleep study including patients whose screening was negative. Base line pain measurement can be done for the study and then can compare their baseline pain perception before CPAP treatment. Pain scale should be periodically administered and pain serially measured and see if pain goes down for the CPAP group compared to the FM alone group without CPAP. In our study, we have 17 OSA patients with history of fibromyalgia. Can CPAP decrease pain in FM+OSA? CPAP decreases pain in FM according to one study.25 If it decreases pain, what could be the mechanism? Could REM rebound, weight loss, decreased fatigue, increased physical activity all play a role? Our pilot study could be the basis for a future study. The focus of our preliminary pilot project was primarily on pain perception, somatosensory amplification and illness behavior. These topics are related but not over-encompassing. This study focused on pain, somatosensory amplification, and illness behavior, and future directions would be to explore other behavior and impacts such as quality of life, physical activity, perception of sleep, and comorbidities like depression and anxiety.
Pain perception and somatosensory amplification are implicated in FM. Following is a review of literature which suggest the theory of central sensitization (CS), the result of abnormal operation of pain pathways, plays a role in FM.26 CS is an amplification of nociceptive neuron response to low-stimuli or low-threshold inputs causing increased pain.27 Clauw et al use the analogy of a “volume control” in which FMS patients have an abnormally high setting which reduces inhibitory mechanisms for pain and increases excitation mechanisms of central neurons.26 Studies have found that FM patients have a lower threshold to induced pressure pain compared to control groups and a lower threshold at tender point sites compared to control groups.28,29 Neuroimaging has also shown that FMS patients have increased blood flow in the cerebral pain processing areas at lower pain-inducing pressures compared to healthy control groups.26 Studies have also shown that nociceptive sensory input is augmented and prolonged in FM patients and maintaining the painful state requires little additional input, which is why seemingly non-painful activities of daily living can contribute to the chronic pain FMS patients experience.30 While it is not completely understood why CS develops, after it occurs, low stimuli to A- β nerve fibers, fibers that normally do not illicit a pain response, are recruited to stimulate neurons to transmit pain.31
Other theories that account for fibromyalgia include somatosensory amplification (SA) in which somatic sensations are experienced as intense, noxious, and disturbing.32 SA has three major components: 1) hypervigilance of the body, 2) a focus on rare or weak sensations, 3) attributing vague sensations as abnormal and symptomatic of disease rather than normal.4 Ciaramella et al have discovered that FM patients have greater SA scores than control groups and that these scores are positively associated with pain persistence and increased tender points.27 SA contributes to the development of CS and high scores of SA may reduce pain tolerance and increase pain intensity affectively and evaluatively.27 SA is further supported in previous literature where FM patients tended to evaluate their symptoms with increased severity and importance compared to osteoarthritis patients, and FMS patient scores for the Barsky amplification scale were similar or elevated to hypochondriac patients.33
Not only are pain perception and somatosensory amplification implicated in FM, but abnormal illness behavior (AIB) is also implicated in FMS. Pilowsky defines such behavior as a maladaptive or inappropriate experience, perception, or evaluation of health and illness.34 Such behavior is most commonly found in situations where there is no indication of a pathological basis and there exists variability due to psychological, somatic, and sociocultural influences.35 Common behaviors include inappropriate daily functioning, mood states, and illness beliefs; previous literature commonly used the Illness Behavior Questionnaire (IBQ), as a measurement of AIB.36 Although AIB was originally formulated in the context of hypochondriasis and hysteria, literature has shown that FM patients often show similar behavior patterns and consideration of such is important for FM treatment.37,38 Using the IBQ designed by Pilowski, Ercolani et al found that FM patients believe their pain stems from a physical cause, reject the idea that their disease is psychological, and deny difficulties in their lives that are not caused by FM.39 These patients have maladaptive behavior which is related but not proportional to their disease and can be classified as cognitive and behavior disorders according to the AIB.39 FM patients may often seek medical care, protest at ineffective treatments and request more suitable treatments.39 This behavior is often due to their mistrust of others due to their persistent belief that their pain is severe, even in the face of contrary evidence.39 Other literature corroborates these findings, where a measure of illness worry, a subset of questions from the IBQ found that illness worry was strongly associated with disability in FM patients.40
Conclusion
Our findings highlight the need for more research to evaluate the relationship between treated and untreated disordered sleeping, pain perception, somatization and illness behavior in the health status of individuals with FM. Developing a better understanding of the effects of OSA on pain perception in patients with FM is needed for improved health status with appropriate treatment and avoid unnecessary polypharmacy. More research is needed to see if higher pain perception and SSAS score lead to increased health care utilization and to evaluate the relationship between untreated disordered sleeping and pain perception in patients with FM. This reinforces the importance of identifying and treating OSA in FM patients and could prevent the use of polypharmacy in pain management.
Acknowledgment
Michael Wesolowski, MS, for his help with Statistics.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Robinson RL, Kroenke K, Mease P, et al. Burden of illness and treatment patterns for patients with fibromyalgia. Pain Med. 2012;13(10):1366–1376. doi:10.1111/j.1526-4637.2012.01475.x
2. Chandran A, Schaefer C, Ryan K, Baik R, McNett M, Zlateva G. The comparative economic burden of mild, moderate, and severe fibromyalgia: results from a retrospective chart review and cross-sectional survey of working-age US adults. J Manag Care Pharm. 2012;18(6):415–426. PMID: 22839682. doi:10.18553/jmcp.2012.18.6.415
3. Melzack R. The short-form McGill pain questionnaire. Pain. 1987;30(2):191–197. doi:10.1016/0304-3959(87)91074-8
4. Nakao M, Barsky AJ. Clinical application of somatosensory amplification in psychosomatic medicine. Biopsychosoc Med. 2007;1:17. doi:10.1186/1751-0759-1-17
5. Pilowsky I, Spence N, Cobb J, Katsikitis M. The illness behavior questionnaire as an aid to clinical assessment. Gen Hosp Psychiatry. 1984;6(2):123–130. doi:10.1016/0163-8343(84)90070-7
6. Roizenblatt S, Neto NSR, Tufik S. Sleep disorders and fibromyalgia. Curr Pain Headache Rep. 2011;15(5):347–357. doi:10.1007/s11916-011-0213-3
7. May KP, West SG, Baker MR, Everett DW. Sleep apnea in male patients with fibromyalgia syndrome. Am J Med. 1993;94(5):505–508. doi:10.1016/0002-9343(93)90085-4
8. Shah MA, Feinberg S, Krishnan E. Sleep-disordered breathing among women with fibromyalgia syndrome. J Clin Rheumatol. 2006;12(6):277–281. doi:10.1097/01.rhu.0000249771.97221.36
9. Greenberg-Dotan S, Reuveni H, Simon-Tuval T, Oksenberg A, Tarasiuk A. Gender differences in morbidity and health care utilization among adult obstructive sleep apnea patients. Sleep. 2007;30(9):1173–1180. doi:10.1093/sleep/30.9.1173
10. Tarasiuk A, Greenberg-Dotan S, Simon-Tuval T, Oksenberg A, Reuveni H. The effect of obstructive sleep apnea on morbidity and health care utilization of middle-aged and older adults. J Am Geriatr Soc. 2008;56(2):247–254. doi:10.1111/j.1532-5415.2007.01544.x
11. Meresh ES, Artin H, Joyce C, et al. Obstructive sleep apnea co-morbidity in patients with fibromyalgia: a single-center retrospective analysis and literature review. Open Access Rheumatol. 2019;11:103–109. doi:10.2147/OARRR.S196576
12. Aytekin E, Demir SE, Komut EA, et al. Chronic widespread musculoskeletal pain in patients with obstructive sleep apnea syndrome and the relationship between sleep disorder and pain level, quality of life, and disability. J Phys Ther Sci. 2015;27(9):2951–2954. doi:10.1589/jpts.27.2951
13. Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. Sleep. 2006;29(2):145–151. doi:10.1093/sleep/29.2.145
14. Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk DJ. Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Front Psychiatry. 2018;9:255. doi:10.3389/fpsyt.2018.00255
15. Pamidi S, Knutson KL, Ghods F, Mokhlesi B. Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnea: cross-sectional analysis of a large clinical population. Sleep Med. 2011;12(9):827–831. PMID: 21978724. doi:10.1016/j.sleep.2011.08.003
16. Nigam G, Camacho M, Riaz M. Rapid Eye Movement (REM) rebound on initial exposure to CPAP therapy: a systematic review and meta-analysis. Sleep Sci Pract. 2017;1:13. doi:10.1186/s41606-017-0014-7
17. Rosenfeld VW, Rutledge DN, Stern JM. Polysomnography with quantitative EEG in patients with and without fibromyalgia. J Clin Neurophysiol. 2015;32(2):164–170. PMID: 25233248.16/0304-3959(88)90176-5. PMID: 3165524. doi:10.1097/WNP.0000000000000134
18. Fitzcharles MA, Ste-Marie PA, Gamsa A, Ware MA, Shir Y. Opioid use, misuse, and abuse in patients labeled as fibromyalgia. Am J Med. 2011;124(10):955–960. doi:10.1016/j.amjmed.2011.05.031
19. Melzack R. The McGill pain questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. PMID: 1235985. doi:10.1016/0304-3959(75)90044-5
20. Dworkin RH, Turk DC, Trudeau JJ, et al. Validation of the Short-form McGill Pain Questionnaire-2 (SF-MPQ-2) in acute low back pain. J Pain. 2015;16(4):357–366. PMID: 25640290. 21J. doi:10.1016/j.jpain.2015.01.012
21. Katz R, Melzack R. The McGill pain questionnaire: development, psychometric properties, and usefulness of the long form, short form, and short form-2; 2011.
22. Turk DC, Melzack R, editors. Handbook of Pain Assessment.
23. Barsky AJ, Wyshak G, Klerman GL. The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatr Res. 1990;24(4):323–334. PMID: 2090830. doi:10.1016/0022-3956(90)90004-a
24. Boyle GJ, Le Déan L. Discriminant validity of the illness behavior questionnaire and million clinical multiaxial inventory-III in a heterogeneous sample of psychiatric outpatients. J Clin Psychol. 2000;56(6):779–791. doi:10.1002/(SICI)1097-4679(200006)56:6<779::AID-JCLP7>3.0.CO;2-7
25. Marvisi M, Balzarini L, Mancini C, Ramponi S, Marvisi C. Fibromyalgia is frequent in obstructive sleep apnea and responds to CPAP therapy. Eur J Intern Med. 2015;26(9):e49–e50. PMID: 26129987. doi:10.1016/j.ejim.2015.06.010
26. Clauw DJ, Arnold LM, McCarberg BH; FibroCollaborative. The science of fibromyalgia. Mayo Clin Proc. 2011;86(9):907–911. doi:10.4065/mcp.2011.0206
27. Ciaramella A, Silvestri S, Pozzolini V, Federici M, Carli G. A retrospective observational study comparing somatosensory amplification in fibromyalgia, chronic pain, psychiatric disorders and healthy subjects. Scand J Pain. 2020;21(2):317–329. PMID: 33130631. doi:10.1515/sjpain-2020-0103
28. Scudds RA, Rollman GB, Harth M, McCain GA. Pain perception and personality measures as discriminators in the classification of fibrositis. J Rheumatol. 1987;14(3):563–569. PMID: 3476752.
29. Tunks E, Crook J, Norman G, Kalaher S. Tender points in fibromyalgia. Pain. 1988;34(1):11–19. doi:10.1016/0304-3959(88)90176-5
30. Staud R. Abnormal pain modulation in patients with spatially distributed chronic pain: fibromyalgia. Rheum Dis Clin North Am. 2009;35(2):263–274. doi:10.1016/j.rdc.2009.05.006
31. Cook AJ, Woolf CJ, Wall PD, McMahon SB. Dynamic receptive field plasticity in rat spinal cord dorsal horn following C-primary afferent input. Nature. 1987;325(7000):151–153. PMID: 3808072. doi:10.1038/325151a0
32. Barsky AJ, Goodson JD, Lane RS, Cleary PD. The amplification of somatic symptoms. Psychosom Med. 1988;50:510–519. doi:10.1097/00006842-198809000-00007
33. Wolfe F, Hawley DJ. Evidence of disordered symptom appraisal in fibromyalgia: increased rates of reported comorbidity and comorbidity severity. Clin Exp Rheum. 1999;17:297–303. 48.
34. Pilowsky I. Abnormal illness behaviour (dysnosognosia). Psychother Psychosom. 1986;46(1–2):76–84. PMID: 3602339. doi:10.1159/000287964
35. Prior KN, Bond MJ. The measurement of abnormal illness behavior: toward a new research agenda for the illness behavior questionnaire. J Psychosom Res. 2008;64(3):245–253. PMID: 18291238. doi:10.1016/j.jpsychores.2007.10.013
36. Pilowsky I, Spence ND. Manual for the Illness Behaviour Questionnaire (IBQ).
37. Pilowsky I. Abnormal illness behaviour: a 25th anniversary review. Aust N Z J Psychiatry. 1994;28:566–573. doi:10.1080/00048679409080780
38. van Wilgen CP, van Ittersum MW, Kaptein AA, van Wijhe M. Illness perceptions in patients with fibromyalgia and their relationship to quality of life and catastrophizing. Arthritis Rheum. 2008;58(11):3618–3626. PMID: 18975315. doi:10.1002/art.23959
39. Ercolani M, Trombini G, Chattat R, et al. Fibromyalgic syndrome: depression and abnormal illness behavior. Multicenter investigation. Psychother Psychosom. 1994;61(3–4):178–186. PMID: 8066155. doi:10.1159/000288887
40. Robbins JM, Kirmayer LJ, Kapusta MA. Illness worry and disability in fibromyalgia syndrome. Int J Psychiatry Med. 1990;20(1):49–63. PMID: 2373594. doi:10.2190/1527-ATRN-Q3NU-GPNN
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
