Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Contribution of Procalcitonin, C-Reactive Protein and Interleukin-6 in the Diagnosis and Prognosis of Surgical Sepsis: An Observational and Statistical Study
Authors Tocu G , Mihailov R , Serban C , Stefanescu BI , Tutunaru D , Firescu D
Received 12 June 2023
Accepted for publication 27 July 2023
Published 15 August 2023 Volume 2023:16 Pages 2351—2359
DOI https://doi.org/10.2147/JMDH.S422359
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
George Tocu,1,2,* Raul Mihailov,3,4 Cristina Serban,4,5 Bogdan Ioan Stefanescu,5,6,* Dana Tutunaru,1,2 Dorel Firescu4,5,*
1Department of Pharmaceutical Sciences, Faculty of Medicine and Pharmacy, “Dunarea de Jos” University, Galați, Romania; 2Clinical Laboratory of Medical Analysis, Emergency County Clinical Hospital “Sf. Ap. Andrei” Galati, Galați, Romania; 3Department of Morphological and Functional Sciences, Faculty of Medicine and Pharmacy, “Dunarea de Jos” University of Galati, Galați, Romania; 4Department of Surgery, Emergency County Clinical Hospital “Sf. Ap. Andrei” Galati, Galați, Romania; 5Department of Clinical Surgery, Faculty of Medicine and Pharmacy, “Dunarea de Jos” University of Galati, Galați, Romania; 6Department of Obstetrics and Gynecology, Emergency County Clinical Hospital “Sf. Ap. Andrei” Galati, Galați, Romania
*These authors contributed equally to this work
Correspondence: Raul Mihailov, Department of Morphological and Functional Sciences, Faculty of Medicine and Pharmacy, “Dunarea de Jos” University, 47 Domneasca Street, Galați, 800008, Romania, Tel +40745250391, Email [email protected] Cristina Serban, Department of Clinical Surgery, Faculty of Medicine and Pharmacy, “Dunarea de Jos” University, 47 Domneasca Street, Galați, 800008, Romania, Tel +40728249228, Email [email protected]
Background: Sepsis affects over 30 million people worldwide each year, causing approximately 6 million deaths. Challenges in clinical diagnosis and the need for an early diagnosis to prevent mortality due to sepsis have led to dependence on inflammatory biomarkers like Procalcitonin (PCT), C-reactive protein (CRP), and Interleukin-6 (IL-6).
Objective: This study was performed to observe the contribution of inflammatory biomarkers in the diagnosis and prognosis of patients with surgical sepsis.
Methods: We performed a retrospective observational study in a Clinical Emergency Hospital, which included a number of 125 patients with surgical sepsis admitted between January 2020 and December 2021. The patients were included in the study based on the Sepsis-3 definition. PCT, CRP, IL-6, Sepsis-related Organ Failure Assessment (SOFA) score, Charlson Comorbidity Index (CCI), the time up to surgery, the days of treatment in Intensive Care Unit (ICU) and the total days of hospitalization had been statistically analyzed.
Results: The mean age of all patients was 65.14 years. The mean value in all patients for PCT was 20.08 ng/mL, for CRP was 175.42 mg/l, and for IL-6 was 799.6 pg/mL. The strongest correlation between biomarkers was between CRP and IL-6 (r = 0.425; p < 0.0001). Of all biomarkers, the CRP correlated the strongest with patient outcomes (r = 0.544; p < 0.0001). The area under curve (AUC) for the mean values of the inflammatory biomarkers was calculated and the best diagnostic performance was for CRP with 0.816 (95% CI: 0.744– 0.887).
Conclusion: CRP and IL-6 were the most efficient in sepsis diagnosis. The association of PCT, CRP and IL-6 has increased the range of certainty in sepsis diagnosis. CRP was the most efficient biomarker in the prognosis of sepsis.
Keywords: inflammatory biomarkers, SOFA score, septic shock, surgical sepsis, postoperatively
Introduction
Sepsis is known as an organ dysfunction due to the host’s inadequate response to infection, which endangers patients’ lives. Septic shock is a subtype of sepsis that includes circulatory, cellular, and metabolic abnormalities which are profound enough to induce a great increase in the mortality rate.1 Sepsis and especially septic shock still remain increased risk factors for mortality.2,3 Sepsis affects over 30 million people worldwide each year, causing approximately 6 million deaths.3 The incidence of sepsis varies between 20% and 80%, and of septic shock between 10% and 30%, while the mortality in sepsis goes up to 50%, and in the septic shock up to 63%.4
Challenges in clinical diagnosis and the need for an early diagnosis to prevent mortality in sepsis have led to the dependence upon inflammatory biomarkers like Procalcitonin (PCT), C-reactive protein (CRP) and Interleukin-6 (IL-6), which are among the most used, both in diagnosis, and in the management of antibiotic therapy, evolution and prognosis.5–8 The increase in the concentration of these biomarkers can suggest the occurrence of sepsis and the clinicians will be able to initiate the appropriate and early treatment and thus the mortality in sepsis could be significantly reduced.9
PCT is the most frequently investigated biomarker of sepsis and has demonstrated the best reliability in early diagnosis, especially for the detection of bacterial infections, compared to other inflammatory biomarkers.10,11 However, many studies recommend the association of PCT with other inflammatory biomarkers for increasing the reliability in early diagnosis.12–14 Other authors have disputed the use of PCT as a diagnostic instrument or to begin the antibiotic therapy, but they support the use of PCT in the decision of stopping the antibiotics,15 as well as in the prognosis of sepsis.16–18
CRP is an acute-phase protein, synthesized by the liver, following the activation of IL-6 during inflammation,19 and has also been studied as an inflammatory biomarker in sepsis. A multitude of different opinions exist regarding the use of CRP in sepsis. Some authors claim that CRP has a low specificity in sepsis diagnosis, and is not a certain indicator for the systemic inflammation,20 while other authors support the effectiveness of CRP, both in monitoring the antibiotic therapy and in sepsis diagnosis.21,22 Also, some studies claim that the assessment of CRP is not suitable for predicting death in sepsis, while other studies claim that CRP would be a good predictor for death in sepsis.23
IL-6 is a cytokine with multifunctional roles, being recognized as a primary mediator in the inflammatory response.24 The IL-6 associates with inflammation severity, organ dysfunction and mortality in sepsis.25 Some studies claim that IL-6 can be successfully used in the diagnosis and prognosis of sepsis, and would also be more effective than PCT and CRP in monitoring the antibiotic therapy and in predicting the therapeutic success.6,25
Methods
Design, Population and Variables
We performed a retrospective observational study between January 2020 and December 2021 in the Emergency County Clinical Hospital “Sf. Ap. Andrei” Galati, Romania, which included patients with surgical sepsis, diagnosed in the emergency surgical department and then hospitalized and treated in clinical surgical departments. A total of 125 patients were included in the study based on the Sepsis Survival Campaign 2016 (Sepsis-3) definition. The sociodemographic variables included gender and age. The laboratory variables included values of the PCT, CRP, and IL-6 inflammatory biomarkers. The clinical variables included the SOFA score (score ≥2), Charlson Comorbidity Index (CCI) which includes a number of 19 comorbidities with an index between 0 and 33,26 the time from presentation to hospital to surgery, the days of treatment in the ICU and the total hospitalization days. The methods of this study were designed in compliance with the STROBE guidelines.27 The main objective was to observe the contribution of PCT, CRP and IL-6 in the diagnosis and prognosis of the patients with surgical sepsis.
Determination of Inflammatory Biomarkers
The determination of inflammatory biomarkers was performed dynamically, at the admission to the hospital, postoperatively after 24 hours, and at 24–48 hours before discharge from hospital. The collection of venous blood for biomarkers’ determination was made in 6 mL vacutainers without anticoagulant, centrifuged at 4000 rpm for 5/10 minutes to obtain the serum. The PCT and IL-6 serum levels were measured with the Atellica IM-1600 analyzer, based on chemiluminescence method. The measure range for PCT was 0.04–50.0 ng/mL and values >50.0 ng/mL were diluted 1/20 with Multi-diluent 2. The measure range for IL-6 was between 2.7 and 5500 pg/mL and the values greater than 5500 pg/mL were diluted 1/10 with Multi-diluent 13. CRP’s serum levels were measured with the Konelab Prime 60i analyzer based on photometric method, at 340 nm wavelength. The measure range for CRP was 0.01–630 mg/L and the values >210 mg/L were diluted 1/2 with distilled water. Normal biomarker values were defined as PCT < 0.05 ng/mL, IL-6 < 17.4 pg/mL, and CRP < 10 mg/l.
Statistical Analysis
We used the XLSTAT 2016 software to perform the statistical analysis of the data. The quantitative variables were expressed as mean and standard deviation (SD), and categorical variables were expressed as numbers with percentages in parentheses. The comparison between survivors and non-survivors was made with Student’s t-test for quantitative variables and with Chi-Square test for categorical variables. The Pearson correlation coefficient analysis method was used for the correlation between biomarkers and patient outcomes. The area under curve (AUC) of the receiver operating characteristic (ROC) was used for determining biomarkers’ performance in the diagnostic. A 95% confidence interval (CI) was used and a p-value <0.05 was appreciated as being statistically significant.
Results
We divided the patients into two groups (survivors and non-survivors) (Table 1). Of the 125 patients, 70 (56%) were discharged as cured, while 55 (44%) died in hospital. Of the total patients, 35 (28%) had sepsis and 90 (72%) had septic shock at the time of admission to the hospital. We expressed the mean ± SD and the minimum and maximum value for sociodemographic and clinical variables. The mean age of all patients was 65.14 years (22–89 years). The mean age of non-survivors was 68.43 years, compared to survivors, who had a lower mean of 62.55 years. In the total number of patients, men predominated in 70 cases (56%), compared to women in only 55 cases (44%). The mean value of the Charlson Comorbidity Index (CCI) was 6.24 in all patients, and 5.12 in the case of non-survivors, compared to survivors who had a mean of 2.92. The mean SOFA score was 6.24 in all patients, a mean of 9.27 in non-survivors and a lower mean of 3.87 in survivors. The time elapsed from admission to hospital to surgery was less than 6 hours for 112 (89.6%) patients and between 6 and 12 hours for 13 (10.4%) patients. The survivors had a time to surgery of less than 6 hours in 48% of cases, versus non-survivors in 41.6% of cases. ICU treatment averaged 6.27 days in all patients, with survivors recovering faster with an average of 4.34 days compared to non-survivors, who had an average of 8.74 days. The mean total days of hospitalization was 19.84 days in all patients, the survivors recording a higher mean compared to non-survivors (21.42 vs 17.81 days).
 |
Table 1 Results of the Characteristics in the Total Patients, Survivors and Non-Survivors |
Table 2 shows the mean ± SD and the minimum and maximum values for the inflammatory biomarkers in dynamics. The means of inflammatory biomarkers were calculated from admission, 24 hours postoperatively, and the values at discharge from hospital for each patient. The average value in all patients for PCT was 20.08 ng/mL, for CRP was 175.42 mg/l, and for IL-6 was 799.6 pg/mL. The serum concentrations of biomarkers in all patients at admission showed increases well above normal limits, having a moderate tendency to decrease at 24 hours postoperatively, and at discharge, the values correlated with patient outcomes. At admission to hospital, all biomarkers were increased in non-survivors much more than at survivors for PCT (33.70 vs 28.06 ng/mL) and IL-6 (2346.64 vs 1352.76 pg/mL), while the difference was not significant for CRP (262.49 vs 249.67 mg/l). At 24 hours postoperatively, serum concentrations decreased compared to the initial values, but were significantly increased for non-survivors than survivors for PCT (24.61 vs 14.73 ng/mL) and IL-6 (1712.4 vs 544.63 pg/mL), while the difference was not significant, but with proclivity towards CRP (203.83 vs 149.18 mg/l). At discharge from the hospital, the serum concentrations remained elevated in non-survivors for PCT with 23.18 ng/mL, IL-6 with 1796.79 pg/mL, and CRP with 194.66 mg/l, while in survivors they returned to normal only for IL-6 with 16.09 pg/mL and PCT with 0.77 ng/mL, and CRP was slightly above the normal limit with 21.60 mg/l.
 |
Table 2 Distribution of the Mean and Dynamic Values of the PCT, CRP and IL-6 in the Total Patients, Survivors and Non-Survivors |
The Pearson correlation coefficient showed statistically significant correlations between inflammatory biomarkers, SOFA score, and patient outcome. The strongest correlation for biomarkers was recorded between CRP and IL-6 (r = 0.425; p < 0.0001) followed by PCT and CRP (r = 0.361; p < 0.0001) and, respectively, PCT and IL-6 (r = 0.341; p < 0.0001). Patient outcomes correlated strongly with the SOFA score (r = 0.743; p < 0.0001), moderately with CRP values (r = 0.544; p < 0.0001), poorly with IL-6 (r = 0.336; p = 0.0001) and the poorest with PCT (r = 0.184; p = 0.04).
The AUC for estimating the diagnostic performance of the mean values of inflammatory biomarkers (Figure 1, Table 3), identified the best performance for CRP with an optimal cut-off of 179.36 mg/l (AUC = 0.816; 95% CI 0.744–0.887; p < 0.0001), sensitivity 0.727 and specificity 0.786. IL-6 had an optimal cut-off of 1052.86 pg/mL (AUC = 0.797; 95% CI 0.718–0.877; p < 0.0001), sensitivity 0.600 and specificity 0.929. The lowest diagnostic performance was for PCT with an optimal cut-off of 6.42 ng/mL (AUC = 0.622; 95% CI 0.526–0.719; p < 0.0001), sensitivity 0.873 and specificity 0.329.
 |
Table 3 Comparisons of Discrimination Capabilities for the Mean and Dynamic Values of the Biomarkers Presented as Area Under Curve |
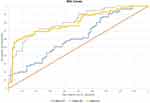 |
Figure 1 AUC for distinguishing patient outcomes discriminated by the mean values of the PCT, CRP and IL-6. |
The AUC for discriminating among the values of biomarkers in dynamics, in estimating diagnostic performance (Figure 2, Table 3), identified the strongest performance for the value at discharge from hospital, followed by the value at 24 hours after surgery, the weakest being the value at admission to hospital. At discharge, the PCT had an optimal cut-off of 1.75 ng/mL (AUC = 0.996; 95% CI 0.996–0.996; p < 0.0001), sensitivity 1.00 and specificity 0.986; the CRP had an optimal cut-off of 43.5 mg/l (AUC = 0.986; 95% CI 0.986–0.986; p < 0.0001), sensitivity 0.982 and specificity 0.929; IL-6 had an optimal cut-off of 64.5 pg/mL (AUC = 1.00; 95% CI 1.00–1.00; p < 0.0001), sensitivity 1.00 and specificity 0.986. At 24 h postoperatively, the PCT had an optimal cut-off of 16.13 ng/mL (AUC = 0.577; 95% CI 0.477–0.677; p = 0.132); CRP had an optimal cut-off of 178 mg/l (AUC = 0.710; 95% CI 0.620–0.800; p < 0.0001); IL-6 had an optimal cut-off of 1162.5 pg/mL (AUC = 0.759; 95% CI 0.676–0.841; p < 0.0001). At admission, the PCT had an optimal cut-off of 78.54 ng/mL (AUC = 0.477; 95% CI 0.375–0.578; p = 0.657); the CRP had an optimal cut-off of 347.9 mg/l (AUC = 0.542; 95% CI 0.441–0.642; p = 0.419), and the IL-6 had an optimal cut-off of 1684.3 pg/mL (AUC = 0.625; 95% CI 0.527–0.723; p = 0.012).
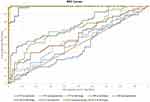 |
Figure 2 AUC for distinguishing patient outcomes discriminated by the dynamic values of the PCT, CRP and IL-6. |
The correlations between the inflammatory biomarkers and AUC for diagnostic performance indicate that mean CRP and IL-6 values were superior in diagnosis, compared to PCT values. In dynamics, the values at admission were more elevated, above normal limits for all biomarkers, but did not show satisfactory curves for diagnostic performance, and then as patients were treated surgically and with antibiotics, at subsequent measurements, postoperatively at 24 hours and at discharge, the biomarker values achieved stronger diagnostic performance.
Discussion
In our study, the serum concentrations of PCT, IL-6 and CRP were found to be significantly increased in non-survivors, compared to survivors. A significant reduction in the IL-6 serum concentrations was observed in dynamics, with a considerable halving at 24 hours postoperatively and reaching normal concentrations at discharge, for survivors, whereas in non-survivors, discharge concentrations were slightly increased compared to concentrations at 24 hours postoperatively. Jekarl et al reported that in sepsis, the dynamic measurements of IL-6 had better kinetics in the survivor group and decreased in more than 86% of survivors within 24 hours, and for non-survivors, elevated IL-6 concentrations had persisted.6,28 Higher levels of IL-6 are associated with the diagnosis of sepsis, severity of organ dysfunction and mortality.29 Song et al showed that IL-6 has a better diagnostic and prognosis value in sepsis patients than PCT,30 also confirmed by Takahashi et al who showed that the value of IL-6 in sepsis diagnosis is higher than PCT and CRP.31 PCT had a proclivity similar to IL-6 in survivors, except that at discharge, the serum concentrations of PCT were slightly above the normal range. Trásy et al reported that PCT was more reliable in diagnosis compared to CRP or IL-6, and the sensitivity and specificity of PCT for bacterial infection were superior to other biomarkers.32 Also, Jekarl et al revealed that PCT can support the diagnosis of bacterial infection in sepsis patients, but that IL-6 would be more effective in monitoring antibiotic therapy.6 The reduction of CRP serum concentrations in our study was slower compared to PCT or IL-6, but it was more reliable in diagnosis than PCT and IL-6, confirmed by the correlation between the mean values of CRP and the patient outcomes, as well as by the area under curve (cut-off 179.36 mg/l; AUC = 0.816; p < 0.0001).
The biomarker values at admission had a poor performance in sepsis diagnosis, having low sensitivity and specificity, but among the three biomarkers, IL-6 had the best diagnostic performance (cut-off 1684.3 pg/mL; AUC = 0.625; p = 0.012). The performance in diagnostic increased as patients were treated surgically and with antibiotics, and in this case, IL-6 also had the best performance, both 24 hours postoperatively (cut-off 1162.5 pg/mL; AUC = 0.759; p < 0.0001), and at discharge (cut-off 64.5 pg/mL; AUC = 1.00; p < 0.0001). Also, both PCT (cut-off 1.75 ng/mL; AUC = 0.996; p < 0.0001) and CRP (cut-off 43.5 mg/l; AUC = 0.986; p < 0.0001) have shown very increased performance for the values at discharge from hospital.
In surgical sepsis, an early diagnosis – as subjective as possible – is crucial in order to intervene urgently in the focal point of infection, thus increasing the patients’ chances of survival. Given that clinical symptoms or signs may not be evident in surgical sepsis, especially in elderly patients, a single baseline value of a biomarker could point to the diagnosis of sepsis, but there is also the possibility that the dosing of a single biomarker may not help the clinician too much, but the value of the diagnosis can be increased by the association of as many biomarkers as possible.5
The serum concentrations of biomarkers were highly elevated at the admission to hospital, in both survivors and non-survivors. Thus, one could induce the hypothesis of a useful role in diagnosis by a single initial value of a single biomarker. The diagnostic performance was better for CRP in terms of average values, and in terms of dynamic values, IL-6 was the best performing in diagnosis. Thus, we consider that the association between IL-6 and CRP values had the best diagnostic performance, which was also the most strongly correlated (r = 0.425; p < 0.0001); in addition, the association with PCT contributed much better to the diagnosis. Certainly, the association of these biomarkers increased the area of certainty in the diagnosis and thus emergency surgery was performed in less than 6 hours for 89.6% of patients. Lee et al revealed that CRP or PCT alone have limitations in the diagnosis of infection and its severity and recommend their association with IL-6 for better utility in assessing the infectious or inflammatory state, appropriately and in a timely manner.5 Zeng et al reported that the association of IL-6, CRP and PCT increased the diagnostic sensitivity to 96.55% and specificity to 94.03%.33
In our study, weak positive correlations between patient outcomes with PCT and IL-6 values (r = 0.184; p = 0.04 and r = 0.336; p = 0.0001, respectively) had been observed, suggesting that PCT and IL-6 did not have an effective role in the prognosis of sepsis. Only CRP had a better correlation with patient outcomes (r = 0.544; p < 0.0001), thus CRP was most useful in the prognosis of sepsis. According to our study, Ryoo et al revealed that CRP was more predictive than PCT, and the increase of both CRP and PCT was associated with the highest mortality rate.20 Devran et al revealed that CRP appears to be a predictor of mortality as valuable as the SOFA score.23 In this case, we are in agreement with the study of Devran et al, because also in our case, the CRP was approximately as effective in prognosis as the SOFA score, having a strong positive correlation with the patient outcomes (r = 0.743; p < 0.0001). Anush et al concluded that serial monitoring of CRP helps to establish prognosis and predict possible outcome even on the third day of hospitalization,22 and Silvestre et al revealed that the CRP from the day when the sepsis diagnosis was established is not a good marker of prognosis.34
As a slight conclusion and recommendation following this study, we suggest that the serum levels of biomarkers at the admission to hospital are not recommended for being used for prognosis purposed, instead of the values at admission, while the values measured in dynamics at 24 hours would be much more useful to clinicians in the prognosis of sepsis. Therefore, we do not recommend using the values at admission of any biomarker as a final indicator of prognosis. In the future, new biomarkers and biomarker associations should be sought, and even the creation of bio-scores, that would be useful both in the early diagnosis and in the prognosis of sepsis.
The limitations of the present study are related first of all to the fact that the study was carried out in one single center, thus it could be possible that our results do not resemble the results of other centers, and secondly, due to the “COVID-19 pandemic”, the number of patients was low, only 125 patients, of which 27 (21.6%) presented to hospital in 2020 and 98 (78.4%) in 2021. A larger sample would increase the value of the study and thus the results would be more plausible. Therefore, further multicenter studies with larger sample sizes are needed.
Conclusion
The mortality rate was quite high in our study, consistent with the elevated serum biomarker concentrations, which were higher in non-survivors compared with survivors. CRP and IL-6 were the most effective in the sepsis diagnosis. PCT alone had no good effectiveness, but in combination with CRP and IL-6 has increased the area of certainty in the sepsis diagnosis. CRP was the most effective in the sepsis prognosis, while PCT and IL-6 had no good effectiveness. However, the combination of these biomarkers could bring an important benefit in the sepsis prognosis. Further studies are needed to demonstrate the effectiveness of the combination of these biomarkers in the sepsis prognosis.
Data Sharing Statement
The information will be granted access to under reasonable request.
Ethics Approval
This retrospective observational study was approved by the Ethics Committee of the Emergency County Clinical Hospital “Sf. Ap. Andrei” of Galati, Romania (registration number: 11777/30.05.2023). All followed procedures were conducted in accordance with the institution law and with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to this work, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
2. Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–1249. doi:10.1001/jama.2017.13836
3. Bauer M, Gerlach H, Vogelmann T, et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019— results from a systematic review and meta-analysis. Crit Care. 2020;24(1):239. doi:10.1186/s13054-020-02950-2
4. Mirea L, Grinţescu I, Dumitrache C. The opportunity of substitutive doses of cortisone to septic patients. Practica Medicala. 2013;2:30. Romania.
5. Lee E-H, Lee K-H, Song Y-G, et al. Discrepancy of C-reactive protein, procalcitonin and interleukin-6 at hospitalization: infection in patients with normal C-reactive protein, procalcitonin and high interleukin-6 values. J Clin Med. 2022;11(24):7324. doi:10.3390/jcm11247324
6. Jekarl DW, Lee SY, Lee J, et al. Procalcitonin as a diagnostic marker and IL-6 as a prognostic marker for sepsis. Diagn Microbiol Infect Dis. 2013;75(4):342–347. doi:10.1016/j.diagmicrobio.2012.12.011
7. Plesko M, Suvada J, Makohusova M, et al. The role of CRP, PCT, IL-6 and presepsin in early diagnosis of bacterial infectious complications in paediatric haemato-oncological patients. Neoplasma. 2016;63(5):752–760. doi:10.4149/neo_2016_512
8. Carcò D, Castorina P, Guardo P, et al. Combination of interleukin-6, C-reactive protein and procalcitonin values as predictive index of sepsis in course of fever episode in adult haematological patients: observational and statistical study. J Clin Med. 2022;11(22):6800. doi:10.3390/jcm11226800
9. George AA, Thomas TP, Gaffoor A. The role of neutrophil/lymphocyte ratio in predicting the severity of sepsis in a tertiary care hospital in south India: a retrospective study. Int J Res Med Sci. 2020;8(5):1624–1628. doi:10.18203/2320-6012.ijrms20201490
10. Gupta S, Jaswani P, Sharma RK, et al. Procalcitonin as a diagnostic biomarker of sepsis: a tertiary care centre experience. J Infect Public Health. 2019;12(3):323–329. doi:10.1016/j.jiph.2018.11.004
11. Yunus I, Fasih A, Wang Y, Lazzeri C. The use of procalcitonin in the determination of severity of sepsis, patient outcomes and infection characteristics. PLoS One. 2018;13(11):e0206527. doi:10.1371/journal.pone.0206527
12. Chen W, Zhao L, Niu S, et al. 不同炎症因子对细菌性血流感染所致脓毒症患者的早期诊断价值 [The diagnostic value of different pro-inflammatory factor in early diagnosis of sepsis in patients with bloodstream infection]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26(3):165–170. Chinese. doi:10.3760/cma.j.issn.2095-4352.2014.03.008
13. Liu TB, Wang MQ, Guan W, et al. [Diagnostic values of procalcitonin, C-reactive protein and interleukin-6 in hematological diseases with bacterial infection]. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2018;26(5):1548–1552. Chinese. doi:10.7534/j.issn.1009-2137.2018.05.048
14. Zhao Y, Li C. 生物标志物组合对急诊脓毒症和重度脓毒症患者的诊断价值 [Diagnostic value of a combination of biomarkers in patients with sepsis and severe sepsis in emergency department]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26(3):153–158. Chinese. doi:10.3760/cma.j.issn.2095-4352.2014.03.006
15. Paudel R, Dogra P, Montgomery-Yates AA, et al. Procalcitonin: a promising tool or just another overhyped test? Int J Med Sci. 2020;17(3):332–337. doi:10.7150/ijms.39367
16. Suranadi IW, Sinardja CD, Suryadi IA. Role of procalcitonin in predicting mortality and organ dysfunction at intensive care admission. Int J Gen Med. 2022;15:4917–4923. doi:10.2147/IJGM.S362558
17. Liang P, Yu F. Value of CRP, PCT, and NLR in prediction of severity and prognosis of patients with bloodstream infections and sepsis. Front Surg. 2022;9:857218. doi:10.3389/fsurg.2022.857218
18. Jekarl DW, Lee S, Kim M, et al. Procalcitonin as a prognostic marker for sepsis based on SEPSIS-3. J Clin Lab Anal. 2019;33(9):e22996. doi:10.1002/jcla.22996
19. Yang Y, Xie J, Guo F, et al. Combination of C-reactive protein, procalcitonin and sepsis-related organ failure score for the diagnosis of sepsis in critical patients. Ann Intensive Care. 2016;6(1):51. doi:10.1186/s13613-016-0153-5
20. Ryoo SM, Han KS, Ahn S, et al. The usefulness of C-reactive protein and procalcitonin to predict prognosis in septic shock patients: a multicenter prospective registry-based observational study. Sci Rep. 2019;9(1):6579. doi:10.1038/s41598-019-42972-7
21. Póvoa P. C-reactive protein: a valuable marker of sepsis. Intensive Care Med. 2002;28(3):235–243. doi:10.1007/s00134-002-1209-6
22. Anush MM, Ashok VK, Sarma RI, et al. Role of C-reactive protein as an Indicator for determining the outcome of sepsis. Indian J Crit Care Med. 2019;23(1):11–14. doi:10.5005/jp-journals-10071-23105
23. Devran Ö, Karakurt Z, Adıgüzel N, et al. C-reactive protein as a predictor of mortality in patients affected with severe sepsis in intensive care unit. Multidiscip Respir Med. 2012;7(1):47. doi:10.1186/2049-6958-7-47
24. Didion SP. Cellular and oxidative mechanisms associated with interleukin-6 signaling in the vasculature. Int J Mol Sci. 2017;18(12):2563. doi:10.3390/ijms18122563
25. Weidhase L, Wellhöfer D, Schulze G, et al. Is Interleukin-6 a better predictor of successful antibiotic therapy than procalcitonin and C-reactive protein? A single center study in critically ill adults. BMC Infect Dis. 2019;19(1):150. doi:10.1186/s12879-019-3800-2
26. Stavem K, Hoel H, Skjaker SA, et al. Charlson comorbidity index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017;9:311–320. doi:10.2147/CLEP.S133624
27. von Elm E, Altman DG, Egger M, et al.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi:10.1016/S0140-6736(07)61602-X
28. Jekarl DW, Kim JY, Lee S, et al. Diagnosis and evaluation of severity of sepsis via the use of biomarkers and profiles of 13 cytokines: a multiplex analysis. Clin Chem Lab Med. 2015;53(4):575–581. doi:10.1515/cclm-2014-0607
29. Yu B, Chen M, Zhang Y, et al. Diagnostic and prognostic value of interleukin-6 in emergency department sepsis patients. Infect Drug Resist. 2022;15:5557–5566. doi:10.2147/IDR.S384351
30. Song J, Park DW, Moon S, et al. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect Dis. 2019;19(1):968. doi:10.1186/s12879-019-4618-7
31. Takahashi W, Nakada TA, Yazaki M, et al. Interleukin-6 levels act as a diagnostic marker for infection and a prognostic marker in patients with organ dysfunction in intensive care units. Shock. 2016;46(3):254–260. doi:10.1515/cclm-2014-0607
32. Trásy D, Tánczos K, Németh M, et al. Delta procalcitonin is a better indicator of infection than absolute procalcitonin values in critically ill patients: a prospective observational study. J Immunol Res. 2016;2016:3530752. doi:10.1155/2016/3530752
33. Zeng G, Chen D, Zhou R, et al. Combination of C-reactive protein, procalcitonin, IL-6, IL-8, and IL-10 for early diagnosis of hyperinflammatory state and organ dysfunction in pediatric sepsis. J Clin Lab Anal. 2022;36(7):e24505. doi:10.1002/jcla.24505
34. Silvestre J, Póvoa P, Coelho L, et al. Is C-reactive protein a good prognostic marker in septic patients? Intensive Care Med. 2009;35(5):909–913. doi:10.1007/s00134-009-1402-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
