Back to Journals » International Journal of General Medicine » Volume 17
The Clinical Value of Systemic Immune Inflammation Index (SII) in Predicting the Severity of Hospitalized Children with Mycoplasma Pneumoniae Pneumonia: A Retrospective Study
Authors Wang S , Wan Y, Zhang W
Received 29 November 2023
Accepted for publication 20 February 2024
Published 12 March 2024 Volume 2024:17 Pages 935—942
DOI https://doi.org/10.2147/IJGM.S451466
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shuye Wang,1,2 Yu Wan,2 Wenbo Zhang2
1Bengbu Medical University, Bengbu, 233000, People’s Republic of China; 2Department of Pediatrics, Changzhou No.2 People’s Hospital, the Affiliated Hospital of Nanjing Medical University, Changzhou, 213000, People’s Republic of China
Correspondence: Wenbo Zhang, Email [email protected]
Objective: The Systemic Immune Inflammation Index (SII), as a novel inflammation biomarker that comprehensively reflects the inflammatory and immune status of the body, has not been reported in studies on Mycoplasma pneumoniae pneumonia (MPP) in children. This study aims to investigate whether SII can serve as an effective indicator for evaluating the condition of MPP.
Methods: This study recruited a total of 304 hospitalized patients with mycoplasma pneumoniae pneumonia (MPP), including 78 patients with severe MPP (SMPP) and 226 patients with non-SMPP. Univariate analysis using chi-square test, t-test, and Mann–Whitney U-test was conducted to analyze the clinical data of the patients. Logistic regression analysis was employed to identify the main risk factors for SMPP. Receiver operating characteristic curves were plotted to evaluate the potential of using neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), systemic immune-inflammation index (SII), and systemic immune response index (SIRI) to predict the severity of MPP.
Results: The ROC curve results show that patients with SII values ≥ 699.00 are more likely to develop severe MPP (sensitivity=0.876, specificity=0.987, AUC=0.940), and the predictive value of SII is significantly better than that of NLR, PLR, and SIRI. The results of multivariate logistic regression analysis indicate that SII can serve as a major risk factor for distinguishing non-SMPP from SMPP.
Conclusion: This study suggests that SII may be an effective indicator for predicting the severity of MPP in children. SII is more sensitive and specific than NLR, PLR, and SIRI in evaluating the condition of MPP.
Keywords: systemic immune-inflammation index, mycoplasma pneumoniae pneumonia, severity, predictive value
Introduction
Mycoplasma pneumoniae pneumonia is an acute infectious disease, accounting for 10–40% of children and adolescents’ community acquired pneumonia, and the incidence rate is increasing year by year.1,2 Scholars have confirmed that compared with non-SMPP, SMPP is more likely to induce multiple system injuries in and out of the lungs, such as bronchiectasis, pulmonary embolism, obliterative bronchiolitis, encephalitis, myocarditis, hemophagocytic syndrome, etc,3 seriously endangering the health of children. Multiple studies have shown that cellular immune mediated inflammatory responses play an important role in the occurrence and development of SMPP, and the balance between anti-inflammatory and pro-inflammatory systems directly affects the changes in the condition and clinical outcomes of pneumonia patients.4,5 Therefore, evaluating the inflammatory status caused by MP infection can help predict the occurrence of SMPP. White blood cells are an important component of the body’s response to immune inflammation. Among them, neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) have been confirmed to have the potential to predict early treatment response and prognosis in CAP patients.6–8 Systemic immune inflammation Index (SII) is a new indicator that reflects inflammation and immune balance in the body, obtained by integrating neutrophil count, lymphocyte count, and platelet count. Compared with NLR and PLR, SII can better reflect the level of inflammation.9,10 SII has been proved to be related to the severity and prognosis of malignant tumors and many inflammatory diseases such as sepsis, COVID-19, etc.11,12 However, there are currently no reports on the potential of SII in MPP disease assessment both domestically and internationally.
Method
Patients and Participants
The study retrospectively studied 304 children with MPP who were hospitalized in the Pediatrics Department of Changzhou Second People’s Hospital affiliated with Nanjing Medical University from July 2022 to July 2023. According to the severity of the patient’s condition, they are divided into the SMPP group (n=78) and the non SMPP group (n=226). Inclusion criteria: (1) Meets the diagnostic criteria in the “Guidelines for the Diagnosis and Treatment of Mycoplasma Pneumonia in Children (2023 Edition)”;13 (2) 1–14 years old. (3) Criteria for the diagnosis of SMPP: The definition of SMPP refers to the Guidelines for the ‘Diagnosis and Treatment of Mycoplasma Pneumoniae Pneumonia in Children (2023 Edition)’.13 Exclusion criteria: (1) Patients with congenital heart disease, chromosomal disease, metabolic disease, immune deficiency disease, hematological tumor disease, bronchopulmonary dysplasia, neurological dysplasia, epilepsy, and other diseases; (2) Previously had neonatal respiratory distress syndrome, bacterial encephalitis, or other serious infectious diseases; (3) Patients with incomplete clinical data.
Data Collection
(1) General information: We collected demographic characteristics (age, gender), body mass index (BMI), onset season, medical history data, and clinical features of patients, including clinical pulmonary infection score (CPIS) (the higher the score, the more severe the clinical condition). (2) All patients were collected fasting blood within 24 hours of admission and tested for each indicator using a fully automated analyzer: white blood cell count (WBC), neutrophil count (Neu), lymphocyte count (Lym), monocyte count (Mono), platelet count (PLT), C-reactive protein (CRP), fibrinogen (FIB), D-dimer. And calculate the systemic immune-inflammation index (SII=platelet count multiplied by neutrophil count divided by lymphocyte count), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and systemic inflammation response index (SIRI=Neutrophil Count * Monocyte Count/Lymphocyte Count). (3) Clinical Pulmonary Infection Score (CPIS): It includes 6 indicators: body temperature, WBC count, secretion, oxygenation index, chest X-ray infiltrates, and bacterial culture of airway secretions. Each indicator is scored from 0 to 2, with a total score of 12. A higher score indicates a more severe clinical condition.8
Statistical Methods
Statistical analysis was conducted using SPSS 26.0 and GraphPad Prism 9.0 statistical software. Continuous variables that follow a normal distribution are represented by mean ± standard deviation (SD) and analyzed using an independent sample t-test; The continuous variables of skewed distribution are represented by median and interquartile spacing (IQR), and Continuous variables that do not conform to normal distribution are represented by median and interquartile intervals (IQR) and analyzed using Mann Whitney U-test. The categorical variables are represented by frequency (%), and inter group comparisons are made using χ2 test. Perform multivariate logistic regression analysis on variables with significant differences in univariate analysis to obtain pre-adjusted data models and post-adjusted data models for other confounding factors. Use Spearman correlation to determine the correlation between NLR, SII, PLR, SIRI, and CPIS. Exploring the risk factors affecting the severity of MPP in children using multivariate logistic regression analysis, Analyze the predictive potential of variables on SMPP through the receiver operating characteristic (ROC) curve. The difference was statistically significant with P<0.05.
Results
Comparison of Demographic and Laboratory Parameters Between SMPP and Non-SMPP Patients
A total of 304 patients were included, with a median age of 5.0 (3.0–7.0) years. There were 146 males (48.03%) and 158 females (51.97%). The basic demographic and clinical characteristics of the participants are shown in Table 1. There were no statistically significant difference in gender, age, BMI, and onset season between the two groups of children (P>0.05). There were significant statistical differences in the course of disease outside the hospital, duration of high fever, total fever, WBC count, neutrophil count, lymphocyte count, monocyte count, PLT count, NLR, PLR, SII, SIRI, Alb, CRP, D-dimer, PCT, FIB, and SII, NLR, PLR, SIRI values of the SMPP group were significantly higher than those of the non-SMPP group (P<0.001).
 |
Table 1 Baseline Characteristics of the 304 Patients with Mycoplasma Pneumoniae Pneumonia |
The Predictive Capabilities of NLR, PLR, SII, and SIRI on SMPP
ROC curves were drawn to evaluate the predictive ability of SII, NLR, PLR, and SIRI on the severity of MPP (Figure 1). The results showed that the AUC of SII, NLR, PLR, and SIRI were 0.940 [95% CI (0.914, 0.965)], 0.885 [95% CI (0.850, 0.921)], 0.818 [95% CI (0.765, 0.870)], 0.883 [95% CI (0.846, 0.921)], respectively. The optimal cutoff values were 699.00, 2.26, 154.70 and 1.23, with sensitivity of 0.87, 0.74, 0.85, and 0.75, and specificity of 0.99, 0.92, 0.65 and 0.94, respectively (Table 2). It can be seen that SII has a better predictive ability for the severity of MPP than NLR, PLR, and SIRI.
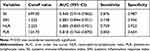 |
Table 2 Diagnostic Performance of SII, NLR, PLR and SIRI for SMPP in Children |
Logistic Regression Models for SMPP Occurrence
Multivariate logistic regression analysis was used to determine the risk factors for the severity of MPP (Table 3). Binary logistic regression analysis showed that after adjusting for confounding factors including duration of high fever, total fever, out of hospital course, CRP, PCT, D-dimer, and fibrinogen, the admission SII value (adjusted odds ratio [OR]=1.006, 95% confidence interval [CI]: 1.004–1.008, P<0.001) The NLR value (adjusted odds ratio [OR]=0.403, 95% confidence interval [CI]: 0.224–0.772, P=0.002) and SIRI value (adjusted odds ratio [OR]=1.900, 95% confidence interval [CI]: 1.400–2.578, P<0.001) still have statistical significance.
 |
Table 3 Logistic Regression Models for Severe Mycoplasma Pneumonia Occurrence |
Correlations of NLR, PLR, SII and SIRI with CPIS in MPP Patients
Spearman correlation analysis was used to evaluate the relationship between CPIS and NLR, PLR, SII, SIRI (Figure 2). The results showed that SII (r=0.4064, 95% CI: 0.3050–0.4987) had the highest correlation with CPIS, indicating a significant correlation between SII and disease severity, followed by NLR, SIRI, and PLR.
Discussion
SMPP has a rapid onset and progression, can lead to multiple system injuries, and is difficult to treat with poor prognosis. Therefore, early identification of SMPP is beneficial for clinical doctors to intervene early and improve the prognosis of patients. Inflammatory factors are key indicators for evaluating the occurrence and development of pneumonia, and are closely related to patient prognosis. Although multiple studies have confirmed that CRP, LDH, and D-dimer can be used as indicators to predict the severity of MPP, chest imaging is also used to evaluate the severity of pulmonary infections. However, in clinical practice, some children with SMPP have no obvious abnormalities in early chest imaging, and outpatient patients generally only test blood routine. SII is an inflammatory index that can be obtained solely based on neutrophil count, lymphocyte count, and platelet count. It can represent different inflammatory and immune response states in the body,9 and plays an important role in the occurrence and development of MPP. In this retrospective study, we compared the predictive value of NLR, SII, PLR, and SIRI for childhood SMPP for the first time, and evaluated the relationship between these four inflammatory indicators and the severity of MPP through CPIS. The results showed that SII can be used to predict the severity of MPP, with better prediction accuracy, sensitivity, and specificity than PLR, NLR, and SIRI.
Most cases of SMPP occur within a week of the course of the disease, and its complex pathogenesis is still unclear. It is usually a combination of multiple factors, closely related to the direct damage of MP and the disorder of the body’s immune response.4 After MP infection, the innate and adaptive immune functions of the body are disrupted, leading to excessive inflammatory reactions in the lungs and the whole body. The cytokines and chemokines released by the body produce an inflammatory cascade amplification effect, causing imbalance of neutrophils, lymphocytes, and platelets in the patient’s peripheral blood, ultimately leading to multi-system damage both inside and outside the lung.14 The increase in SII levels primarily results from elevated neutrophils and platelets, along with a decrease in lymphocytes. Neutrophils are the key to the progression of pneumonia.15 Studies have shown that the membrane lipoprotein of MP binds to Toll-like receptors (TLRs) on alveolar macrophages (AM), which can activate the nuclear factor-κB(NF-κB) signaling pathway, leading to the release of pro-inflammatory cytokines such as interleukin-8 (IL-8), tumor necrosis factor-α (TNF-α), interferon (IFN), and granulocyte-macrophage colony-stimulating factor (GM-CSF), thereby promoting neutrophils aggregation and pathogens phagocytosis.16,17 As the severity of MP infection escalates, there is a concurrent increase in the levels of IL-8 and TNF-α in the patients’ serum.16,18 Lee et al have also confirmed that after MP adheres to alveolar epithelial cells (AECs), ACEs can produce a significant amount of extracellular vesicles rich in miRNA. These miRNA-enriched extracellular vesicles are actively delivered to alveolar macrophages (AM), promoting neutrophil recruitment and inflammasome activation, leading to excessive inflammatory response and subsequent impairment of the host’s immune function.19,20 Platelets come from mature megakaryocytes in the bone marrow and play a crucial role in hemostasis and coagulation. In addition, it is also an important mediator of inflammatory response.21,22 When pneumonia occurs, MP and its toxins, inflammatory mediators, and hypoxia can cause endothelial damage, leading to platelet activation, aggregation, and excessive consumption. At this point, megakaryocytes in the bone marrow are activated to produce more platelets to compensate for the loss. Studies have found a positive correlation between PLT levels and hospital stay, mortality, and prognosis in MPP patients.23,24 Persistent inflammatory reactions can lead to cellular immune dysfunction, thereby inducing lymphocyte depletion. This is consistent with the results of this study, that is, the lymphocyte count of SMPP patients is lower than that of non SMPP patients. Therefore, inflammatory markers based on these inflammatory cells, including NLR, PLR, SII, and SIRI, can be used to evaluate the systemic inflammatory level and immune balance status of MPP patients.
Previous studies have shown that high levels of PLR are associated with 90-day mortality in CAP patients,7 and NLR can predict the prognosis and early treatment response of CAP patients.8 NLR and SII have good guiding value for the early diagnosis and condition assessment in children with CAP.25 E. Acar’s26 study confirmed that SII>3551 is an independent risk factor affecting 28-day mortality in CAP patients, with predictive sensitivity and specificity of 63.8% and 68.1%, respectively. The area under the ROC curve is 0.737 [95% CI (0.672–0.802), P<0.001], indicating that dynamic monitoring of SII levels is beneficial for evaluating the condition and prognosis of children. Our research shows that NLR [0.885, 95% CI (0.850, 0.921)], PLR [0.818, 95% CI (0.765, 0.870)], SII [0.940, 95% CI (0.914, 0.965)], and SIRI [0.883, 95% CI (0.846, 0.921)] all have good predictive ability for SMPP. The adjusted multivariate logistic regression analysis results showed that SII, NLR, and SIRI were independent risk factors for predicting the severity of MPP, indicating that among the four inflammatory indicators, SII, NLR, and SIRI had better predictive ability for SMPP. Therefore, MPP patients should evaluate the NLR, SII, and SIRI values at admission to determine early strengthening of anti-inflammatory and anti-infective treatment, and improve the prognosis of the patients.
In addition, in order to further discuss the clinical practical value of SII, NLR, SIRI, and PLR, this study explored the correlation between them and the severity of MPP through CPIS. CPIS has 6 indicators, including body temperature, WBC count, airway secretions, oxygenation index, chest X-ray infiltration shadow, and bacterial culture of airway aspirates, with each indicator scoring 0–2 points and a total score of 12 points; The higher the score, the more severe the pulmonary infection and the need for active anti infection treatment. Our results found the strongest correlation between SII and CPIS, indicating that the higher the SII value of hospitalized MPP patients, the more severe the pulmonary infection.
In severe pneumonia, the interaction between inflammation and the coagulation system can exacerbate lung injury. CRP, D-dimer, FIB are commonly used indicators to evaluate the inflammatory status of MPP patients, which can be used for early identification and prediction of SMPP cases. The higher the detection value, the greater the risk of developing SMPP.3,27 In our study, the serum CRP, D-dimer, and FIB levels in SMPP patients were significantly higher than those in non SMPP patients, indicating that there may be excessive inflammatory response in SMPP patients.
However, this study has some limitations. Firstly, this is a single center retrospective study, and the study only focuses on hospitalized children with MPP. Further research is needed to determine whether it is equally applicable to outpatient children. Secondly, the sample size of this study is limited. Therefore, further large-scale prospective studies are needed to further explore the relationship between SII and the severity of MPP patients’ conditions to validate our conclusions. Thirdly, the SII value is only calculated based on the peripheral blood cell count at admission, and further research is needed on the dynamic changes of SII with the evolution of the condition.
Conclusion
In conclusion, SII can be used as a clinical predictor of disease severity in hospitalized MPP children, and its predictive performance is better than that of NLR, SIRI, and PLR.
Data Sharing Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding authors.
Ethics Statement
This study was approved by the Clinical Research Ethics Committee of Changzhou Second People’s Hospital (No. [2023]KY016-01) and was in accordance with the principles of the Helsinki Declaration. Informed consent was waived by the ethics committee as all the data were collected after de-identification. The data were only accessible to the principal investigator, ensuring confidentiality. The information was kept confidential throughout the entire study.
Funding
This study is funded by Changzhou Municipal Health Commission Science and Technology Project (grant number: QN202028).
Disclosure
All authors declare that there is no conflict of interest for this research.
References
1. Chen YC, Hsu WY, Chang TH. Macrolide-resistant Mycoplasma pneumoniae infections in pediatric community-acquired pneumonia. Emerg Infect Dis. 2020;26(7):1382–1391. doi:10.3201/eid2607.200017
2. Gao LW, Yin J, Hu YH, et al. The epidemiology of paediatric Mycoplasma pneumoniae pneumonia in North China: 2006 to 2016. Epidemiol Infect. 2019;147:e192. doi:10.1017/S0950268819000839
3. Lee KL, Lee CM, Yang TL, et al. Severe Mycoplasma pneumoniae pneumonia requiring intensive care in children, 2010–2019. J Formos Med Assoc. 2021;120(1 Pt 1):281–291. doi:10.1016/j.jfma.2020.08.018
4. Jiang Z, Li S, Zhu C, Zhou R, Leung PHM. Mycoplasma pneumoniae infections: pathogenesis and vaccine development. Pathogens. 2021;10(2):119.
5. Hu J, Ye Y, Chen X, Xiong L, Xie W, Liu P. Insight into the pathogenic mechanism of Mycoplasma pneumoniae. Curr Microbiol. 2022;80(1):14. doi:10.1007/s00284-022-03103-0
6. Kuikel S, Pathak N, Poudel S, et al. Neutrophil-lymphocyte ratio as a predictor of adverse outcome in patients with community-acquired pneumonia: a systematic review. Health Sci Rep. 2022;5(3):e630. doi:10.1002/hsr2.630
7. Enersen CC, Egelund GB, Petersen PT, et al. The ratio of neutrophil-to-lymphocyte and platelet-to-lymphocyte and association with mortality in community-acquired pneumonia: a derivation-validation cohort study. Infection. 2023. doi:10.1007/s15010-023-01992-2
8. Lee H, Kim I, Kang BH, Um SJ. Prognostic value of serial neutrophil-to-lymphocyte ratio measurements in hospitalized community-acquired pneumonia. PLoS One. 2021;16(4):e0250067. doi:10.1371/journal.pone.0250067
9. Wu J, Yan L, Chai K. Systemic immune-inflammation index is associated with disease activity in patients with ankylosing spondylitis. J Clin Lab Anal. 2021;35(9):e23964. doi:10.1002/jcla.23964
10. Geraghty JR, Lung TJ, Hirsch Y, et al. Systemic immune-inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2021;89(6):1071–1079. doi:10.1093/neuros/nyab354
11. Cogliati Dezza F, Oliva A, Cancelli F, et al. Determinants of prolonged viral RNA shedding in hospitalized patients with SARS-CoV-2 infection. Diagn Microbiol Infect Dis. 2021;100(2):115347. doi:10.1016/j.diagmicrobio.2021.115347
12. Bittoni A, Pecci F, Mentrasti G, et al. Systemic immune-inflammation index: a prognostic tiebreaker among all in advanced pancreatic cancer. Ann Transl Med. 2021;9(3):251. doi:10.21037/atm-20-3499
13. Zhao S, Chen Z, Liu H. Key interpretation of “Guidelines for the diagnosis and treatment of Mycoplasma pneumoniae pneumonia in children (2023)” by the National Health Commission. J Clin Pediatr. 2023;41(3):224–228. doi:10.12372/jcp.2023.22e0475
14. Lee YC, Chang CH, Lee WJ, et al. Altered chemokine profile in refractory Mycoplasma pneumoniae pneumonia infected children. J Microbiol Immunol Infect. 2021;54(4):673–679. doi:10.1016/j.jmii.2020.03.030
15. Cacciotto C, Cubeddu T, Addis MF, et al. Mycoplasma lipoproteins are major determinants of neutrophil extracellular trap formation. Cell Microbiol. 2016;18(12):1751–1762. doi:10.1111/cmi.12613
16. Xue Y, Wang M, Han H. Interaction between alveolar macrophages and epithelial cells duringMycoplasma pneumoniae infection. Front Cell Infect Microbiol. 2023;13:1052020. doi:10.3389/fcimb.2023.1052020
17. Allard B, Panariti A, Martin JG. Alveolar macrophages in the resolution of inflammation, tissue repair, and tolerance to infection. Front Immunol. 2018;9:1777. doi:10.3389/fimmu.2018.01777
18. Yu B, Zhao Y, Zhang H, Xie D, Nie W, Shi K. Inhibition of microRNA-143-3p attenuates myocardial hypertrophy by inhibiting inflammatory response. Cell Biol Int. 2018;42(11):1584–1593. doi:10.1002/cbin.11053
19. Lee H, Groot M, Pinilla-Vera M, Fredenburgh LE, Jin Y. Identification of miRNA-rich vesicles in bronchoalveolar lavage fluid: insights into the function and heterogeneity of extracellular vesicles. J Control Release. 2019;294:43–52. doi:10.1016/j.jconrel.2018.12.008
20. Sadikot RT, Bedi B, Li J, Yeligar SM. Alcohol-induced mitochondrial DNA damage promotes injurious crosstalk between alveolar epithelial cells and alveolar macrophages. Alcohol. 2019;80:65–72. doi:10.1016/j.alcohol.2018.08.006
21. Sato T, Okamura T, Kojima-Shibata C, et al. Correlated response of peripheral blood cytokines with selection for reduced mycoplasma pneumonia of swine lesions in Landrace pigs. Anim Sci J. 2016;87(4):477–483. doi:10.1111/asj.12462
22. Liu F, Zhang X, Zhang B, et al. TREM1: a positive regulator for inflammatory response via NF-kappaB pathway in A549 cells infected with Mycoplasma pneumoniae. Biomed Pharmacother. 2018;107:1466–1472. doi:10.1016/j.biopha.2018.07.176
23. Mirsaeidi M, Peyrani P, Aliberti S, et al. Thrombocytopenia and thrombocytosis at time of hospitalization predict mortality in patients with community-acquired pneumonia. Chest. 2010;137(2):416–420. doi:10.1378/chest.09-0998
24. Qiu J, Ge J, Cao L. D-dimer: the risk factor of children’s severe mycoplasma pneumoniae pneumonia. Front Pediatr. 2022;10:828437. doi:10.3389/fped.2022.828437
25. Li L, Miao H, Chen X, Yang S, Yan X. Research on the Correlation of peripheral blood inflammatory markers with PCT, CRP, and PCIS in infants with community-acquired pneumonia. Evid Based Complement Alternat Med. 2022;2022:9024969. doi:10.1155/2022/9024969
26. Acar E, Gokcen H, Demir A, Yildirim B. Comparison of inflammation markers with prediction scores in patients with community-acquired pneumonia. Bratisl Lek Listy. 2021;122(6):418–423. doi:10.4149/BLL_2021_069
27. Liu J, He R, Wu R, et al. Mycoplasma pneumoniae pneumonia associated thrombosis at Beijing Children’s hospital. BMC Infect Dis. 2020;20(1):51. doi:10.1186/s12879-020-4774-9
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


