Back to Journals » Infection and Drug Resistance » Volume 16
The Clinical Presentations of Liver Abscess Development After Endoscopic Retrograde Cholangiopancreatography with Choledocholithiasis: A 17-Year Follow-Up
Authors Liu AC, Tai WC , Chiu SM, Sou FM, Yang SC, Lu LS, Kuo CM, Chiu YC, Chuah SK, Liang CM , Wu CK
Received 25 July 2023
Accepted for publication 7 September 2023
Published 13 September 2023 Volume 2023:16 Pages 6167—6174
DOI https://doi.org/10.2147/IDR.S428125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
An-Che Liu,1 Wei-Chen Tai,1,2 Shao-Ming Chiu,1 Fai-Meng Sou,1 Shih-Cheng Yang,1 Lung-Sheng Lu,1 Chung-Mou Kuo,1 Yi-Chun Chiu,1,2 Seng-Kee Chuah,1,2 Chih-Ming Liang,1,2 Cheng-Kun Wu1,2
1Division of Hepato-Gastroenterology, Department of Internal Medicine, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 2College of Medicine, Chang Gung University, Taoyuan, Taiwan
Correspondence: Cheng-Kun Wu, Division of Hepato-Gastroenterology, Department of Internal Medicine, Kaohsiung Chang Gung Memorial Hospital, 123 Ta Pei Road, Niao Sung Dist, Kaohsiung, 833, Taiwan, Tel +886-7-731-7123 Ext 8301, Fax +886-7-732-2402, Email [email protected]
Background: Endoscopic Retrograde Cholangiopancreatography (ERCP), used for choledocholithiasis treatment, carries a risk of pyogenic liver abscess (PLA) due to communication between the biliary system and bowel contents. However, limited data exists on this issue. This study aims to identify the risk factors pertaining to liver abscesses following ERCP lithotomy.
Methods: We conducted a retrospective case series across multiple centers to evaluate patients who developed PLA after ERCP for choledocholithiasis. Data was obtained from the Chung Gung Research Database (January 2001 to December 2018). Out of 220 enrolled patients, 195 were categorized in the endoscopic sphincterotomy (ES) group, while 25 were in the non-ES group for further analysis.
Results: The non-ES group had significantly higher total bilirubin levels compared to the ES group (4.3 ± 5.8 vs 1.9 ± 2.0, p< 0.001). Abscess size, location, and distribution (single or multiple) were similar between the two groups. The most common pathogens were Klebsiella pneumoniae and Escherichia coli. Pseudomonas infection was significantly less prevalent in the ES group compared to the non-ES group (3.6% vs 16.7%, p=0.007). Patients with concurrent malignancies (HR: 9.529, 95% CI: 2.667– 34.048, p=0.001), elevated total bilirubin levels (HR: 1.246, 95% CI: 1.062– 1.461, p=0.007), multiple abscess lesions (HR: 5.146, 95% CI: 1.777– 14.903, p=0.003), and growth of enterococcus pathogens (HR: 4.518, 95% CI: 1.290– 15.823, p=0.001) faced a significantly higher risk of in-hospital mortality.
Conclusion: PLA incidence was higher in the ES group compared to the non-ES group following ERCP for choledocholithiasis. Attention should be given to significant risk factors, including concurrent malignancies, elevated total bilirubin levels, multiple abscess lesions, and growth of enterococcus pathogens, to reduce in-hospital mortality.
Keywords: endoscopic retrograde cholangiopancreatography, pyogenic liver abscess, risk factors
Introduction
The standard management for bile duct stones involves the use of ERCP with ES as the widely accepted procedure.1,2 Despite its overall safety profile, ERCP with ES is not completely free from the risk of complications. Although uncommon, the development of liver abscess is recognized as a late but potentially life-threatening complication of ERCP, particularly in patients who have a compromised barrier between the hepatobiliary system and duodenum following ES.3,4 Given the low occurrence rate of liver abscess following ERCP for choledocholithiasis, our prior research has primarily concentrated on investigating its prevalence and risk factors.5 However, limited attention has been directed towards exploring the clinical presentations of liver abscesses in these patients, which would aid in comprehending the symptoms and facilitating early diagnosis.
In recent times, there has been a growing focus on investigating the correlation between the occurrence of liver abscess and ERCP, specifically among patients diagnosed with choledocholithiasis. This research endeavor aims to bridge existing knowledge gaps by examining the clinical manifestations associated with the development of liver abscess in individuals who underwent ERCP for choledocholithiasis. Additionally, the study endeavors to identify the risk factors, treatment modalities, and preventive strategies pertaining to liver abscesses following ERCP lithotomy.
Methods
Compliance with Ethical Requirements
This current study adhered to the principles outlined in the Declaration of Helsinki. The study protocol received approval from both the Institutional Review Board and the Ethics Committee of Chang Gung Memorial Hospital in Taoyuan, Taiwan (Approval number: 201900919B0). The Ethics Committee waived the need for informed consent in this study, and data analysis was conducted anonymously to ensure privacy and confidentiality.
Data Sources
Patient data for this study were obtained from the Chang Gung Research Database (CGRD), which is the largest healthcare system in Taiwan. The CGRD is a comprehensive repository of de-identified medical records encompassing outpatient and inpatient treatment, laboratory results, interventional procedures, and medication prescriptions. The diagnosis of diseases is coded according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) for data before 2016 and ICD-10-CM for subsequent data. To ensure patient confidentiality, the data in the CGRD are encrypted and de-identified upon entry, and can be decrypted if necessary to access medical information.
Study Cohort, Inclusion and Exclusion Criteria
The identification of liver abscess and choledocholithiasis cases relied on the International Classification of Diseases, 9th Revision Clinical Modification (ICD-9-CM) for data prior to 2016 and ICD-10-CM for subsequent data shown. A cohort of patients with choledocholithiasis who underwent endoscopic retrograde cholangiopancreatography (ERCP) examination with either endoscopic sphincterotomy (ES) or non-ES procedure (endoscopic papillary balloon dilation) was selected from January 1, 2001, to December 31, 2018. Exclusion criteria included individuals under 18 years old, previous history of ERCP procedure, pyogenic liver abscess, amebic liver abscess, alcoholism, history of hepatopancreaticobiliary system surgery, and malignancies such as hepatocellular carcinoma (HCC), gallbladder and extrahepatic bile duct malignancies, small intestine (including duodenum) malignancies, and pancreatic malignancies. After enrollment, the data underwent additional validation analysis to ensure the accuracy of the initial diagnosis of liver abscess. Furthermore, comprehensive details including age, comorbidities (diabetes mellitus (DM), pancreas, liver disease and other malignancy), medication history, laboratory data (white blood counts, platelet, creatinine, hepatobiliary functions and CRP level), characteristics of the liver abscess, treatment modalities, presence of extra-hepatic complications, mortality rates, and culture results were obtained to facilitate in-depth analysis. A total of 220 individuals were confirmed to have liver abscess. Of these, 195 patients were classified into the ES group, while an additional 25 patients were assigned to the non-ES group for subsequent analysis.
Statistical Analysis
Continuous data were presented as means ± standard deviation (SD) and categorical data are presented as frequencies and percentages. Pearson’s chi-square or Fisher’s exact 2-tailed tests were used for the analysis of categorical data, while continuous variables were analyzed using the t-test, where appropriate. Factors associated with in-hospital mortality were determined using the Cox proportional hazards model. Two-tailed p-values < 0.05 were considered statistically significant. All analyses were performed using the Statistical Package for Social Sciences (IBM SPSS®, version 22.0 for Windows).
Results
Patient Characteristics
The patient cohort is visually represented in Figure 1. Among the 17,829 patients with choledocholithiasis who underwent ERCP and were enrolled from the Chung Gung Research Database between January 1, 2001, and December 31, 2018, a total of 11,697 patients were included after applying strict exclusion criteria. Over the course of 17 years, 220 cases (1.88%) developed pyogenic liver abscess (PLA). For analysis purposes, the liver abscess cases were further categorized into two groups: the endoscopic sphincterotomy (ES) group (n=195, 88.6% of the cohort) and the non-ES group (n=25, 11.4%), consisting of other ERCP procedures.
 |
Figure 1 Schematic Flowchart of Enrolled Patients with the Development of Pyogenic Liver Abscess (PLA) with or without Endoscopic Sphincterotomy (ES). |
The demographic data of the two groups are presented in Table 1. There was a trend towards older age in the endoscopic sphincterotomy (ES) group compared to the non-ES group (70.1 ± 12.7 versus 65.4 ± 11.8, p=0.077). The non-ES group exhibited significantly higher total bilirubin levels compared to the ES group (4.3 ± 5.8 versus 1.9 ± 2.0, p<0.001). No significant differences were observed in terms of underlying comorbidities (pancreatic disease, liver disease, other malignancy, diabetes mellitus), medications (aspirin, statin, or proton pump inhibitor), and laboratory data (glycated hemoglobin, white blood count, liver function, creatinine, and C-reactive protein) between the two groups at the time of PLA admission.
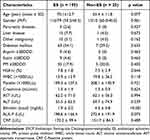 |
Table 1 Demographic Characteristics of Two Liver Abscess Groups Following ERCP |
Clinical Presentations and Outcomes
As shown in Table 2, there was no significant difference observed between the two groups in terms of complications such as lung infection, retinitis, or meningitis (22 (11.3%) versus 2 (8.0%), p=0.743). There was no significant difference in the size of the abscess (5.2 ± 2.7 versus 5.3 ± 1.8, p=0.793). The majority of patients had unilocular abscess lesions, and there was no significant difference between the two groups (158 (84.9%) versus 20 (83.3%), p=0.836). The ES group had a significantly higher proportion of patients with a history of previous endoscopic retrograde biliary drainage (ERBD) before index PLA hospitalization compared to the non-ES group (147 (75.4%) versus 9 (36.0%), p<0.001). It is worth mentioning that patients in the non-ES group exhibited a significantly higher level of total bilirubin compared to the ES group. There were no significant differences between the two groups in terms of antibiotic regimen, aspiration or pigtail drainage method, or repeat ERCP during hospitalization for treatment modalities. Additionally, no significant differences were observed in terms of hospital stay (18.5 ± 13.2 days vs 22.2 ± 10.4, p =0.182) or in-hospital mortality (12.8% vs.12.0%, p =0.908).
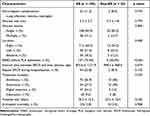 |
Table 2 Clinical Presentations and Outcome Summary |
Culture Results Between the Two Groups
The most common pathogens identified in both groups were Klebsiella pneumoniae and Escherichia coli (Table 3). There was a trend towards a higher incidence of enterococcus growth in the non-ES group (5 (20.0%) versus 18 (9.2%), p=0.098), although this difference did not reach statistical significance. Furthermore, the prevalence of Pseudomonas infection was significantly lower in the ES group compared to the non-ES group (3.6% versus 16.7%, p=0.007). Other pathogens showed similar distribution between the two groups.
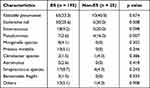 |
Table 3 Differences in Cultures Between Two Groups (Culture Rate: 67.1%) |
Factors Associated with in-Hospital Mortality
Table 4 demonstrated the factors associated with In-Hospital mortality. In the univariate analysis, several factors were found to be significantly associated with an increased risk of in-hospital mortality. These factors include pancreatic disease (hazard ratio [HR]: 9.871, 95% confidence interval [CI]: 3.313–29.407, p<0.001), other malignancy (HR: 4.060, 95% CI: 1.372–12.015, p=0.011), elevated total bilirubin (HR: 1.126, 95% CI: 1.015–1.248, p=0.025), presence of multiple abscess lesions (HR: 3.298, 95% CI: 1.419–7.665, p=0.006), growth of E. coli (HR: 4.161, 95% CI: 1.881–9.207, p<0.001), growth of enterococcus pathogen (HR: 4.866, 95% CI: 2.092–11.320, p<0.001) based on blood or pus cultures, and the presence of extrahepatic manifestations of complications (HR: 4.599, 95% CI: 1.979–10.687, p<0.001).
 |
Table 4 Factors Associated with in-Hospital Mortality |
After conducting further multivariate analysis, adjusting for other variables, the following factors remained significant risk factors associated with increased in-hospital mortality: other malignancy (HR: 9.529, 95% CI: 2.667–34.048, p=0.001), elevated total bilirubin (HR: 1.246, 95% CI: 1.062–1.461, p=0.007), presence of multiple abscess lesions (HR: 5.146, 95% CI: 1.777–14.903, p=0.003), and growth of enterococcus pathogen (HR: 4.518, 95% CI: 1.290–15.823, p=0.001).
Discussion
Pyogenic liver abscess (PLA) is a potentially life-threatening infectious disease. Risk factors for PLA include diabetes mellitus (DM), underlying hepatobiliary or pancreatic diseases, and gastrointestinal cancers involving the biliary tract.6–8 In recent years, biliary tract diseases, such as choledocholithiasis, hepatobiliary malignancy, strictures, and congenital biliary anomalies, have emerged as the predominant causes of PLA.9 Regarding long-term complications associated with ERCP, our previous study showed a significantly increased risk of pyogenic liver abscess (PLA) in patients who underwent ES compared to those without ES.5 The underlying mechanism involves the disruption of the barrier between the hepatobiliary system and the duodenum following ES, which promotes duodenal-biliary reflux.10,11 This reflux leads to the backflow of enteric fluid into the bile duct, facilitating bacterial colonization, cholangitis, and potentially resulting in the development of liver abscess. Additionally, an increased incidence of gastrointestinal (GI) cancers has been reported in patients with liver abscesses, including those who have undergone ERCP with choledocholithiasis.12–14 In a population-based study, the incidence of GI cancer was found to be more than four times higher in patients with pyogenic liver abscess (PLA) compared to controls.12 It was reported that patients with PLA were also found to have a higher incidence of colorectal cancer, followed by cancers of the biliary tract, pancreas, and small intestine.12 It is crucial to monitor patients with liver abscesses, including those who have undergone ERCP with choledocholithiasis.
In light of the infrequent incidence of liver abscess after ERCP for choledocholithiasis, previous studies have predominantly emphasized the investigation of its prevalence and identification of risk factors.5,15 This study represents a pioneering effort, encompassing a substantial patient cohort, to investigate the long-term follow-up of patients who developed PLA following ERCP, with or without ES, for the management of choledocholithiasis. Diabetes mellitus was a well-known risk factor of development of PLA with specific growth of Klebsiella pneumoniae.6,16 On the contrary, patients with PLA after ERCP treatment tend to be caused by a broader range of microorganisms, including Escherichia coli, extended-spectrum beta-lactamase-producing Enterobacteriaceae, and other Gram-negative bacteria.17 The present study yielded consistent findings, as multiple microorganisms were identified in the study population. Moreover, notable findings include a significantly higher total bilirubin level and an increased prevalence of pseudomonas pathogen growth in the non-endoscopic sphincterotomy (non-ES) group. Our findings provide compelling evidence that patients with concurrent malignancies, elevated levels of total bilirubin, multiple abscess lesions, and positive cultures indicating the growth of enterococcus pathogens face a markedly elevated risk of in-hospital mortality. These results suggest that patients with compromised immune function and more severe clinical presentations necessitate urgent interventions, including targeted antibiotic therapy against enterococcus species. Understanding the clinical presentation of PLA is essential for aiding clinical physicians in the early diagnosis of PLA and facilitating the design of appropriate treatment modalities. Preventive measures for the development of liver abscess after ERCP encompass several key strategies. These include scrupulous adherence to aseptic techniques during the procedure, cautious administration of antibiotics, and the identification and effective management of risk factors such as diabetes mellitus and immunosuppression. Additionally, meticulous patient selection, comprehensive pre-procedure evaluation, and prompt identification of post-procedure complications are pivotal in minimizing the likelihood of liver abscess formation.
This study had certain limitations that should be acknowledged. Firstly, its retrospective design may introduce inherent biases. The smaller number of cases with PLA in the non-ES group may introduce a potential bias leading to false negatives. In this manuscript, it’s important to note that all patients were hospitalized and diagnosed with liver abscess. Additionally, considering the relatively low incidence of pyogenic liver abscess (PLA) following ERCP for choledocholithiasis treatment, this study still holds substantial clinical significance and maintains adequate statistical power. We have incorporated these points into the limitation section of the manuscript. Secondly, the data were obtained from the Chang Gung Research Database, which may include patients with more severe clinical conditions and thus may not be representative of the entire cohort.
Conclusions
Liver abscesses associated with ES procedures demonstrated a higher incidence of PLA following ERCP for choledocholithiasis removal compared to the non-ES group, reflecting biliary defense system damage. Moreover, the non-ES group exhibited a higher rate of Pseudomonas infection and more elevated levels of jaundice. Attention should be given to significant risk factors for in-hospital mortality, including concurrent malignancies, elevated total bilirubin levels, multiple abscess lesions, and positive cultures indicating the growth of enterococcus pathogens. Future research endeavors should focus on developing enhanced diagnostic and therapeutic strategies aimed at mitigating the risk of liver abscess formation and optimizing patient outcomes.
Acknowledgments
The authors appreciate Miss Yi-Hsuan Tsai in the Division of Gastroenterology, Kaohsiung Chang Gung Memorial Hospital for the assistance with programming and analyses.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declared that they have no conflicts of interest in this work. All authors have no commercial association, such as consultancies, stock ownership or other equity interests or patent-licensing arrangements.
References
1. Manes G, Paspatis G, Aabakken L, et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51(5):472–491. doi:10.1055/a-0862-03463
2. Tringali A, Costa D, Fugazza A, et al. Endoscopic management of difficult common bile duct stones: where are we now? A comprehensive review. World J Gastroenterol. 2021;27(44):7597–7611. doi:10.3748/wjg.v27.i44.7597
3. Tanaka M, Takahata S, Konomi H, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48(5):465–469. doi:10.1016/S0016-5107(98)70086-018
4. Yasuda I, Fujita N, Maguchi H, et al. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72(6):1185–1191. doi:10.1016/j.gie.2010.07.00619
5. Wu C-K, Hsu C-N, Cho W-R, et al. Increased Risk of Pyogenic Liver Abscess after Endoscopic Sphincterotomy for Treatment of Choledocholithiasis. Infect Drug Resist. 2021;14:2121–2131. doi:10.2147/IDR.S312545
6. Thomsen RW, Jepsen P, Sorensen HT. Diabetes mellitus and pyogenic liver abscess: risk and prognosis. Clin Infect Dis. 2007;44:1194–1201. doi:10.1086/513201
7. Tsai FC, Huang YT, Chang LY, et al. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis. 2008;14(10):1592–1600. doi:10.3201/eid1410.07125412
8. Heneghan HM, Healy NA, Martin ST, et al. Modern management of pyogenic hepatic abscess: a case series and review of the literature. BMC Res Notes. 2011;4:80–88. doi:10.1186/1756-0500-4-80
9. Rahimian J, Wilson T, Oram V, et al. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39:1654–1659. doi:10.1086/42561610
10. Kim KY, Han J, Kim HG, et al. Late complications and stone recurrence rates after bile duct stone removal by endoscopic sphincterotomy and large balloon dilation are similar to those after endoscopic sphincterotomy alone. Clin Endosc. 2013;46:637–642. doi:10.5946/ce.2013.46.6.637
11. Itokawa F, Itoi T, Sofuni A, et al. Mid-term outcome of endoscopic sphincterotomy combined with large balloon dilation. J Gastroenterol Hepatol. 2015;30:223–229. doi:10.1111/jgh.12675
12. Lai HC, Lin CC, Cheng KS, et al. Increased incidence of gastrointestinal cancers among patients with pyogenic liver abscess: a population-based cohort study. Gastroenterology. 2014;146(1):129–137.e1. doi:10.1053/j.gastro.2013.09.058
13. Yeh TS, Jan YY, Jeng LB, et al. Pyogenic liver abscesses in patients with malignant disease: a report of 52 cases treated at a single institution. Arch Surg. 1998;133(3):242–245. doi:10.1001/archsurg.133.3.242
14. Qu K, Liu C, Wang Z-X, et al. Pyogenic liver abscesses associated with nonmetastatic colorectal cancers: an increasing problem in Eastern Asia. World J Gastroenterol. 2012;18(23):2948–2955. doi:10.3748/wjg.v18.i23.2948
15. Peng YC, Lin CL, Sung FC. Risk of pyogenic liver abscess and endoscopic sphincterotomy: a population-based cohort study. BMJ Open. 2018;8(3):e018818. doi:10.1136/bmjopen-2017-018818
16. Li W, Chen H, Wu S, et al. A comparison of pyogenic liver abscess in patients with or without diabetes: a retrospective study of 246 cases. BMC Gastroenterol. 2018;18(1):144. doi:10.1186/s12876-018-0875-y
17. Lam YH, Wong SK, Lee DW, et al. ERCP and pyogenic liver abscess. Gastrointest Endosc. 1999;50(3):340–344. doi:10.1053/ge.1999.v50.98065
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
