Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
The Changing and Predicted Trends in Chronic Obstructive Pulmonary Disease Burden in China, the United States, and India from 1990 to 2030
Authors Guo B , Gan H, Xue M, Huang Z , Lin Z, Li S, Zheng P , Sun B
Received 10 November 2023
Accepted for publication 1 March 2024
Published 8 March 2024 Volume 2024:19 Pages 695—706
DOI https://doi.org/10.2147/COPD.S448770
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Baojun Guo,1,2 Hui Gan,1 Mingshan Xue,1,3 Zhifeng Huang,1 Zhiwei Lin,1 Shiyun Li,1 Peiyan Zheng,1 Baoqing Sun1
1Department of Clinical Laboratory of the First Affiliated Hospital of Guangzhou Medical University, State Key Laboratory of Respiratory Disease, National Center for Respiratory Medicine, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, Guangzhou, 510120, People’s Republic of China; 2School of Medicine, Henan University, Kaifeng, 475004, People’s Republic of China; 3Guangzhou Eighth People’s Hospital, Guangzhou Medical University, Guangzhou, 510060, People’s Republic of China
Correspondence: Baoqing Sun; Peiyan Zheng, Email [email protected]; [email protected]
Background: This study analyzed the burden of chronic obstructive pulmonary disease (COPD) in China, the United States, and India from 1990 to 2019 and projected the trends for the next decade.
Methods: This study utilized the GBD 2019 to compare the age-standardized incidence rate (ASIR), age-standardized mortality rate (ASMR), age-standardized disability-adjusted life years (DALYs) rate, and the proportion attributed to different risk factors in China, the United States, and India. Joinpoint models and autoregressive integrated moving average (ARIMA) models were employed to capture the changing trends in disease burden and forecast outcomes.
Results: From 1990 to 2019, China’s age-standardized COPD incidence and mortality rates decreased by 29% and 70%, respectively. In the same period, India’s rates decreased by 8% and 33%, while the United States saw an increase of 9% in COPD incidence and a 22% rise in mortality rates. Smoking and ambient particulate matter pollution are the two most significant risk factors for COPD, while household air pollution from solid fuels and low temperatures are the least impactful factors in the United States and India, respectively. The proportion of risk from household air pollution from solid fuels is higher in India than in China and the United States. Predictions for 2030 suggest that the age-standardized DALY rates, ASIR, and ASMR in the United States and India are expected to remain stable or decrease, while China’s age-standardized incidence rate is projected to rise.
Conclusion: Over the past three decades, the incidence of COPD has been decreasing in China and India, while showing a slight increase in the United States. Smoking and ambient particulate matter pollution are the primary risk factors for men and women, respectively. The risk of household air pollution from solid fuels in India needs attention.
Keywords: COPD, global burden of disease, risk factors, DALYs
Introduction
COPD is a severe respiratory disease characterized by airway obstruction and progressive breathing difficulties. It is primarily caused by various factors, including smoking, air pollution, and genetic factors.1 As of 2019, more than 200 million people worldwide were suffering from COPD, with over 3 million deaths attributed to this condition. This has placed a significant burden on public health and healthcare resources globally.2
There are noticeable differences in the trends of COPD between developed and developing countries. In developed countries, especially in Europe and North America, the primary causes of COPD are long-term smoking and occupational exposure. Developed countries have relatively advanced healthcare systems with better diagnostic and treatment facilities. This results in more widespread early diagnosis and treatment of COPD, reducing both its prevalence and mortality rates. However, in developing countries, the patterns of COPD incidence differ from those in developed countries. Developing countries often face high levels of environmental pollution and indoor air pollution, particularly due to biomass burning. Additionally, their lower economic development level leads to limited healthcare facilities and resources, resulting in insufficient early diagnosis and treatment of COPD. As a consequence, the incidence of COPD is on the rise in these countries.3 Furthermore, different climate conditions may also influence the trends of COPD. Dry and cold climates can exacerbate airway irritation and inflammation, worsening COPD symptoms. In contrast, warm and humid climates may be more favorable for individuals with COPD.4
In summary, COPD is a significant global health issue. Developed and developing countries exhibit differences in the characteristics of COPD incidence, including varying influences of factors such as smoking, occupational exposure, and environmental pollution. Climate conditions, the level of social development, economic development, and healthcare systems can also impact the trends of COPD.3
China, the United States, and India, being significant global economies and populous nations, possess distinct demographic structures, socioeconomic levels, and healthcare systems. Consequently, they may exhibit varying COPD risk factors and management challenges. The objective of this study is to utilize GBD 2019 to analyze the incidence, mortality, DALYs, and risk factors of COPD in China, the United States, and India from 1990 to 2019. Furthermore, it aims to predict the disease burden for the next decade, with a particular focus on the unique characteristics of these three countries regarding COPD incidence. This research aims to provide a scientific basis for the development of relevant prevention and management strategies. By implementing improved preventive and therapeutic measures, it seeks to reduce the incidence of COPD, enhance the quality of life for patients, and alleviate the burden on healthcare systems.
Method
Data Sources
The data on the disease burden and risk factors of COPD were obtained from the Global Health Data Exchange (GHDx), an institution under the University of Washington in the United States. GHDx is dedicated to assessing the disease burden of 369 diseases, injuries, and risk factors in 204 countries and regions worldwide (https://ghdx.healthdata.org/gbd-2019/data-input-sources). It regularly releases data including incidence rates, mortality rates, and DALYs by country, year, gender, disease cause, and age group. The database covers annual incidence rates, mortality rates, DALYs, and risk factors from January 1, 1990, to December 31, 2019. The GBD estimation process involves identifying multiple relevant data sources for each disease or injury, including population censuses, household surveys, healthcare service usage, air pollution monitoring, satellite imaging, disease notifications, and other sources. In this study, data on COPD disease burden and risk factors were extracted and analyzed from the years 1990 to 2019 for China, the United States, and India.
Disability-Adjusted Life-Years (DALYs)
The Disability-Adjusted Life Year (DALY) serves as a holistic measure encompassing the impact of both fatal and non-fatal outcomes on health. It quantifies the overall burden of disease by combining Years Lived with Disability (YLDs) and Years of Life Lost (YLLs). Each lost year of health is represented as a single DALY. This cumulative figure effectively illustrates the disparity between the existing health condition and the ideal state across all populations.
Age-Standardized Rate
The age-standardized rate (ASR) serves as a valuable metric for gauging shifts in disease prevalence across varying population distributions. ASR is particularly well-suited for facilitating comparisons among diverse demographic groups. The precise techniques employed to compute the ASR remain consistent with those documented in earlier research endeavors.5
Statistical Analysis
Considering the original data source, data manipulation, measurement errors, and the uncertainty involved in model selection, this database was subjected to analysis, modeling, and estimation using the Institute for Health Metrics and Evaluation (IHME) Bayesian regression tool DisMod-MR V.2.1. This was carried out for various indicators, including incidence, prevalence, mortality, and DALYs, which were standardized for the global population and reported as age-standardized rates per 100,000 population. The data used for this study were carefully cleaned and organized, after which they were tabulated and graphed using GraphPad 8.0.2. Given that the GBD database is age-standardized and provided with a 95% uncertainty interval (UI), the data can be directly subjected to statistical analysis and graphical representation.6
The Joinpoint regression model is a set of linear statistical models used to assess the temporal trends in disease burden attributed to COPD. The calculation methodology of this model involves employing the least squares method to estimate the changing patterns of disease rates, thus avoiding the subjectivity inherent in typical trend analyses reliant on linear trends. The turning point of the shifting trend is derived by computing the sum of squared residuals between the estimated and actual values.7 We utilized Joinpoint (version 4.9.1.0; National Cancer Institute, Rockville, MD, USA) to construct this model. Additionally, we calculated the Annual Percentage Change (APC), Average Annual Percentage Change (AAPC), and their corresponding 95% uncertainty intervals (UI).
The autoregressive integrated moving average (ARIMA) model is one of the classic methods in time series analysis. It is based on past values of a series and previous forecasting errors and can be utilized to predict the changing trends in COPD burden. We used data from 1990 to 2019 as the training sample to fit the ARIMA model. Using the Expert Modeler feature of SPSS version 26, we aimed to find the most suitable time series model. The stationarity of the data was examined through the autocorrelation function (ACF) and partial autocorrelation function (PACF).8
Result
The Disease Burden of COPD in China, the United States, and India in 2019
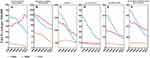
In 2019, the peak of COPD incidence number in China, the United States, and India was concentrated in the 65–69 age group. China had the highest number of new cases, followed by India and the United States. The COPD incidence rates in China and India increased with age, while in the United States, the incidence rate of COPD reaches its peak with increasing age, followed by a trend of initially decreasing and then increasing. Among males, the peak incidence rate was in the 75–79 age group, while among females, it was in the 70–74 age group. In all age groups, the incidence rate of COPD in these three countries was higher in males compared to females. In 2019, the mortality rates for both male and female individuals with COPD in China, the United States, and India increased with age. In each age group, males in these three countries had higher mortality rates than females. The highest number of COPD-related deaths in China and India occurred in the 80–84 age group, while in the United States, the most significant number of COPD-related deaths was in the 75–79 age group. China had higher mortality rates and death numbers than India and the United States across all age groups. In these three countries, DALYs number for COPD reached their peak in the 70–74 age group. Chinese males experienced a peak in DALYs rates in the 90–94 age group before declining. In contrast, Indian males and females had continuous increases in DALYs rates with age, with a brief decline in the 85–89 age group before continuing to rise to their peak (Figure 1; Supplementary Tables 1–6).
 |
Figure 1 In 2019, the numbers and rates of incidence, mortality, and DALYs of COPD by age and sex in China, the United States, and India. (A–C) China; (D–F) the United States; (G–I) India. |
Trends in ASIR, ASMR, and Age-Standardized DALYs Rate from 1990 to 2019 in China, the United States, and India
The total population age-standardized incidence rate of COPD in China and India decreased by 29% and 8%, respectively, from 1990 to 2019. The mortality rate in these countries also declined by 70% and 33%, and the DALYs rate decreased by 69% and 31%. In contrast, the United States experienced an increase in the total population ASIR, ASMR, and Age-Standardized DALYs rate, with a rise of 9%, 22%, and 6%, respectively, during the same period (Table 1).
 |
Table 1 In 1990 and 2019, the ASIR, ASMR, Age-Standardized DALYs Rate, and Percentage Change for COPD in China, the United States, and India |
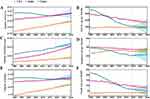
We constructed a Joinpoint regression model to analyze the trends in ASIR, ASMR, and age-standardized DALYs rates of patients with chronic obstructive pulmonary disease (COPD) in three different countries (Supplementary Tables 7–9). The AAPC for ASIR for the total population, males, and females in China are −1.16 (95%UI: −1.24 to −1.09), −1.21 (95%UI: −1.30 to −1.12), and −1.14 (95%UI: −1.21 to −1.07), respectively. Notably, the ASIR for Chinese males exhibited the most significant declines in the intervals 2004–2010 (APC = −2.05 [95%UI: −2.18 to −1.93]), 2010–2014 (APC = −1.18 [95%UI: −1.48 to −0.87]), and 2014–2017 (APC = −2.91 [95%UI: −3.57 to −2.25]). Conversely, for Chinese females, the ASIR showed a slight increase in the 2010–2014 interval (APC = 0.38 [95%UI: 0.15 to 0.60]), while decreasing in all other intervals. The AAPC for ASIR for the total population, males, and females in India are −0.28 (95%UI: −0.29 to −0.26), −0.29 (95%UI: −0.31 to −0.27), and −0.26 (95%UI: −0.27 to −0.25), respectively. ASIR for Indian males increased in the 1990–1995 interval but have consistently decreased since then. In contrast, Indian females have shown a consistent decline in ASIR across all six intervals. The AAPC for ASIR for the total population, males, and females in the United States are 0.30 (95%UI: 0.27 to −0.33), −0.13 (95%UI: −0.14 to −0.12), and 0.61 (95%UI: 0.57 to 0.65), respectively. ASIR for US males increased in the 1990–1996 and 1996–2004 intervals but have consistently decreased since then. US females, on the other hand, saw an increase in ASIR in the 1990–1995, 1995–2004, and 2004–2010 intervals, followed by a consistent decline. It is worth noting that the ASIR for both genders in India are higher than those in China and the United States.
Over the past three decades, the AAPC for ASMR in China for the total population, males, and females are −4.12 (95%UI: −4.39 to −3.85), −3.60 (95%UI: −3.93 to −3.27), and −4.67 (95%UI: −4.95 to −4.38), respectively. In India, the AAPC for ASMR for the total population, males, and females are −1.42 (95%UI: −2.32 to −0.52), −1.48 (95%UI: −2.49 to −0.44), and −1.18 (95%UI: −2.14 to −0.21), respectively. In the United States, the AAPC for ASMR for the total population, males, and females are 0.67 (95%UI: 0.61 to 0.73), −0.13 (95%UI: −0.25 to −0.003), and 1.37 (95%UI: −1.20 to −1.55), respectively. It is important to note that the ASMR in both China and India have consistently been higher than those in the United States over the past 30 years. However, in the case of China, the ASMR for the total population and females have been lower than those in India since 2006.
Over the past three decades, the AAPC for age-standardized DALYs rates in China for the total population, males, and females are −4.05 (95%UI: −4.26 to −3.84), −3.73 (95%UI: −4.03 to −3.42), and −4.29 (95%UI: −4.61 to −3.97), respectively. In India, the AAPC for age-standardized DALYs rates for the total population, males, and females are −1.28 (95%UI: −1.48 to −1.07), −1.23 (95%UI: −1.45 to −1.00), and −1.07 (95%UI: −1.73 to −0.42), respectively. In the United States, the AAPC for age-standardized DALYs rates for the total population, males, and females are 0.2 (95%UI: −0.16 to −0.24), −0.36 (95%UI: −0.41 to −0.31), and 0.61 (95%UI: 0.46 to 0.75), respectively. It is important to note that the age-standardized DALYs rates for the total population, males, and females in both China and India have consistently been higher than those in the United States over the past 30 years. However, for China, the age-standardized DALYs rates for the total population and females have been lower than those in India since 2001, and for Chinese males, it has been lower than that of India since 2002 (Figure 2).
 |
Figure 2 ASIR (A), age-standardized DALYs rate (B), and ASMR (C) of COPD per 100,000 population by sex in China, the United States, and India from 1990 to 2019. |
Risk Factors for COPD in China, the USA, and India
According to data from the GBD 2019 Study, the six leading risk factors contributing to DALYs in COPD are Smoking, Secondhand smoke, Ambient particulate matter pollution, Occupational particulate matter, gases, and fumes, Low temperature, and Household air pollution from solid fuels. In 2019, the most significant risk factor for COPD DALYs in males aged 30 and above in China, the United States, and India was Smoking, while for females, it was Ambient particulate matter pollution. In India, the proportion of risk attributable to Household air pollution from solid fuels is higher than in China and the United States. This risk factor does not show a clear correlation with age. Additionally, its declining trend since 1990 is not as pronounced as observed in China. Among these factors, Smoking exhibited the strongest correlation with age-related changes in all three countries, with a noticeable increase in its contribution from ages 30 to 55. The DALYs attributed to Household air pollution from solid fuels in the United States and those resulting from Low temperature in India were significantly lower compared to other countries. In comparison to males, females had a relatively higher risk factor associated with Secondhand smoke, while the risk associated with Occupational particulate matter, gases, and fumes was relatively lower (Figure 3).
 |
Figure 3 Proportion of DALYs attributable to risk factors by age and sex in 2019. (A) China; (B) the United States; (C) India. |
Trends in COPD Risk Factors in China, the United States, and India from 1990 to 2019
From 1990 to 2019, the trends in DALYs rates of COPD attributed to the six risk factors in the United States remained relatively stable. In China, the DALYs rates attributed to all six risk factors showed significant decreases. In India, the DALYs rates related to Ambient particulate matter pollution increased, those due to Low temperature remained stable, while the other risk factors exhibited decreasing trends. Notably, there has been a reversal in disease burden between China and India for four risk factors: Ambient particulate matter pollution, Occupational particulate matter, gases, and fumes, Secondhand smoke, and Smoking. These risk factors, which initially led to a higher disease burden in China, have gradually declined to levels lower than those in India (Figure 4).
Predictions for the Disease Burden of COPD in China, the United States, and India
We have predicted the disease burden of COPD, and the results show that by 2030, the estimated COPD incidence in China, the United States, and India will be 4,697,469.37 (95% UI: 4,233,785.63 to 5,161,153.10), 1,655,453.58 (95% UI: 1,460,145.00 to 1,850,762.16), and 4,211,599.662 (95% UI: 4,041,274.24 to 4,381,925.08), respectively. The estimated number of deaths due to COPD in these countries will be 1,390,158.47 (95% UI: 656,794.04 to 2,123,522.90), 235,782.21 (95% UI: 225,493.57 to 246,070.85), and 1,078,195.61 (95% UI: 966,191.37 to 1,190,199.85), respectively. The estimated number of DALYs for COPD will be 25,944,890.39 (95% UI: 14,007,858.53 to 37,881,922.24), 5,900,368.95 (95% UI: 5,726,650.24 to 6,074,087.65), and 24,889,247.92 (95% UI: 23,345,240.37 to 26,433,255.46), in the same order. These figures represent an increase compared to 2019. However, the ASIR, ASMR, and age to standardized DALY rates for COPD in these three countries have remained stable or shown a decreasing trend (Figure 5).
In addition, we made predictions for the incidence rate, mortality rate, and DALYs rate of chronic obstructive pulmonary disease (COPD) in different age groups (Supplementary Figure 1). The results show that in the 25–49 age group, the incidence rate among Chinese females has increased. In the 50–69 age group, the incidence rate for Chinese females, American males, and American females has increased, along with an increased mortality rate for American males. In the 70+ age group, the incidence rate for American females and Chinese females has increased. In the remaining cohorts, the rates have either exhibited stability or witnessed a decline.
These predictive findings provide crucial insights into future trends of chronic obstructive pulmonary disease. However, it’s important to note that these predictions are based on current data and model assumptions, which could be influenced by various factors. Therefore, further research is still required to consider potential influencing factors for a more accurate assessment of the changing trends in the incidence, mortality, and DALY rates of chronic obstructive pulmonary disease in different populations.
Discussion
As of 2019, the global prevalence of COPD was 212.3 million people, with an annual incidence of 16.2 million, resulting in 3.3 million deaths worldwide.3 In the same year, China had 45.16 million COPD cases, with 4 million new cases annually and 1.04 million deaths.9 Globally, countries with low sociodemographic index (SDI) had lower COPD prevalence compared to high SDI countries, but their mortality rates were higher than those of high SDI countries. In this study, different trends were observed in the incidence rates, mortality rates, and DALY rates, as well as the number of new cases, deaths, and DALYs for COPD across various age groups in China, the United States, and India. These variations may be attributed to differences in the population base in different age groups in each country. The significant decrease in the incidence rate of COPD in males over 75 in the United States may be related to the screening effect in the elderly population and a greater emphasis on early diagnosis and management of COPD in high-risk individuals.
Based on the GBD 2019 database, we found that smoking is the primary causative factor of COPD. Chemical components found in tobacco, such as nicotine, carbon monoxide, benzene, cyanide, and polycyclic aromatic hydrocarbons, lead to airway inflammation and damage when they enter the respiratory system. This results in airway mucosal inflammation, bronchial constriction, and pulmonary tissue fibrosis, ultimately leading to airflow limitation and breathing difficulties. Secondhand smoke refers to non-smokers being exposed to the smoke released by smokers, and long-term exposure carries similar risks.10 To mitigate the hazards caused by smoking, many countries have strengthened tobacco control measures since the 1990s. These measures include banning smoking in public places, requiring health warning images and text on tobacco packaging, and gradually increasing tobacco taxes. Moreover, countries have enhanced regulation of the tobacco industry, restricted tobacco advertising and promotional activities, promoted smoking prevention and cessation education, and provided smoking cessation support and services.11 Both China and India require that individuals under the age of 18 are not allowed to purchase, smoke, or provide tobacco products.12,13 In the United States, federal law prohibits the sale of tobacco products to individuals under 18, but some states have raised the legal smoking age to 21.14
Fine particulate matter (PM2.5) is an air pollutant originating from sources such as industrial emissions, vehicular exhaust, and the combustion of coal and wood.15 Specific particles and chemicals exist in certain occupational environments, with coal miners exposed to coal dust, farmers handling pesticides and fertilizers, and construction workers inhaling cement dust. PM2.5 consists of tiny particles that can remain suspended in the air and be inhaled into the lungs. Prolonged exposure to PM2.5 can irritate the airway mucosa, leading to airway inflammation, decreased lung function, and an accelerated aging and damage of lung tissues.16,17 Furthermore, low temperatures can result in airway constriction, increased mucus secretion, and a heightened risk of respiratory infections. This intensifies the inflammatory response in the airways, exacerbating symptoms and breathing difficulties for COPD patients.4
Over the past three decades, we have observed a significant decline in the ASIR of COPD in China, which has now fallen below the levels seen in the United States. At the same time, the ASMR has transitioned from a higher level to one lower than that of India but still higher than that of the United States. These data indicate that China has made positive progress in the prevention and control of COPD. This achievement can be attributed to the Chinese government and society’s emphasis on health issues, including the strengthening of anti-smoking campaigns and increased investment in healthcare. These efforts have contributed to reducing the incidence and mortality rates of COPD, thus improving the quality of life for patients.18 However, despite the reduction in COPD incidence and mortality rates, China still faces some challenges. Compared to the United States, the COPD mortality rate in China remains relatively high. This could be influenced by various factors such as smoking rates, environmental pollution, early diagnosis of patients, and the extent of healthcare coverage. In order to further enhance the prevention and control of COPD and reduce the risk of patient mortality, China has implemented a series of measures. This includes reducing coal and petroleum consumption, developing clean energy sources, strengthening forest protection, and promoting practices such as straw mulching to replace the burning of crop residues.19 In addition, China actively participates in international cooperation, signing and fulfilling its commitments under the “Paris Agreement”.20 The implementation of these measures further highlights China’s commitment to addressing climate change and health issues, providing strong support for the prevention and control of COPD.
As of 2020, the urbanization rate in India was approximately 35%, with a rural population of around 868 million people, accounting for 26.5% of the world’s total rural population. In comparison, China and the United States had urbanization rates of approximately 61.9% and 82.3%, respectively.21,22 Despite a gradual decline in age-standardized incidence and mortality rates, India faces significant challenges such as insufficient healthcare resources, healthcare service inequality, and low diagnostic coverage. These challenges may lead to delayed diagnosis and treatment of COPD, preventing patients from receiving timely and effective management and care. Furthermore, many households in rural areas still rely on traditional biomass fuels like firewood and charcoal as their primary sources of fuel. The combustion of such fuels produces harmful substances and indoor air pollution. Long-term exposure to indoor air pollution may increase the risk of COPD.23 Developed countries with higher urbanization rates use clean energy as fuel, along with centralized heating and home air purification systems, which significantly reduce the incidence of COPD caused by solid fuel-induced indoor air pollution.24,25 According to surveys, in 2011, only 11.4% of Indian households had access to liquefied petroleum gas, while in 2016 and 2020, 41% and 92% of the population in India, respectively, had access to clean cooking fuel. The Pradhan Mantri Ujjwala Yojana (PMUY) initiative introduced by the Indian government in 2016 provided subsidies for the use of liquefied petroleum gas, benefiting over 80 million households by 2019.26 Another study indicated that from 2005 to 2016, the use of clean energy in urban and rural areas of India increased by 21% and 15%, respectively.27 Despite the higher proportion of the risk factor of Household air pollution from solid fuels compared to the United States and China, these findings highlight significant achievements in India’s efforts to address household air pollution. Additionally, most regions in India have a tropical monsoon climate, with an average winter temperature ranging from 10°C to 20°C. As a result, the proportion of COPD cases due to low temperatures is much lower in India compared to temperate and cold climate countries. India is currently in a phase of rapid industrialization, with significant industrial emissions, traffic exhaust, and construction dust contributing to air pollution, leading to an increase in COPD DALYs rates. In contrast, the United States is in a post-industrial phase, with upgraded industrial structures at the national and regional levels and a shift toward a service and knowledge-based economy. This has led to some alleviation of environmental particulate matter pollution issues.
We described the trends in the burden of COPD in China, the United States, and India over the past 30 years and made predictions. We found that in China, the COPD incidence rate for females across all age groups is expected to increase in the next 11 years, while it is noteworthy that the incidence rate for males is projected to decline. In the United States, the incidence rates for males and females in the 50–69 age group are expected to increase in the future. Furthermore, over the past 30 years, in the three countries of China, the United States, and India, the DALYs for COPD caused by Occupational particulate matter, gases, and fumes, as well as smoking, have been significantly higher for males than for females. This may be attributed to the higher smoking rates among males and the fact that high-exposure risk occupations are predominantly male-dominated. However, research has found that under equivalent tobacco or smoke exposure, females have a higher incidence rate of COPD and experience a greater decline in lung function.28 This may be related to the ability of estradiol to upregulate cytochrome P450 enzymes, making lung tissue more susceptible to oxidative damage from cigarette smoke. Moreover,29 in comparison to males, female smokers are more likely to experience thickening of bronchial walls,30 and female COPD patients are more prone to airway narrowing while experiencing less emphysema.31
In addition to the risk factors for COPD discussed above, there are still many non-smoking-related risk factors not included in the GBD 2019 database. Examples of these factors include asthma, infections (tuberculosis, HIV, recurrent respiratory infections in children), dietary factors, low maximally attained lung growth, genetic factors, and others. Reports have shown that the prevalence of COPD in individuals who have never smoked ranges from 4% to 16%. Additionally, among individuals with COPD, 22% to 51% have never smoked. Never-smokers with COPD are typically younger, exhibit fewer respiratory symptoms and cardiovascular complications, show less evident emphysema, and often have small airway pathology. Generally, the lower the level of economic development in a region, the greater the proportion of risk factors associated with non-smoking-related COPD. However, there is currently limited research on the pathogenesis of non-smoking-related COPD, and further investigation is necessary.32 However, this study still has limitations. Due to the vast geographical expanse and complex ethnic diversity in China, the United States, and India, there are significant variations in environmental, economic, healthcare conditions, and lifestyle habits among different regions and ethnic groups, which can influence disease susceptibility differently. Additionally, the GBD database is a global resource for disease and injury data, providing researchers with the ability to compare disease burdens across different regions and countries and identify global and regional disease trends and risk factors. However, the GBD database also has limitations, including data constraints, model estimations, and other shortcomings. GBD data sources include population censuses, household surveys, healthcare service usage, air pollution monitoring, satellite imaging, disease notifications, and other methods of data capture. The choice of data capture methods may also impact the results, and data obtained through surveys can be influenced by subjective factors, memory biases, or social expectations of the respondents. It may have limited coverage and analysis for specific diseases or health issues in certain populations. Therefore, there is a need to enhance data quality control, refine and localize data, promote data sharing and collaboration, and integrate research findings with real-world scenarios to formulate more accurate and targeted policy measures.
Conclusion
In summary, from 1990 to 2019, the ASIR of COPD in the total populations of China and India have consistently shown a declining trend, while the United States has demonstrated a relatively stable and slightly increasing trend, surpassing China in 2004. However, the ASMR from COPD in the United States has consistently remained lower than that in China and India. The mortality rate for COPD increases with age, emphasizing the need for a focused approach to addressing the burden of COPD among the elderly. Smoking and Ambient particulate matter pollution are identified as the primary risk factors for male and female COPD, respectively. The trends in risk factors for COPD over the past thirty years indicate significant success in China in controlling tobacco and air particulate pollution. India has made considerable progress in addressing household air pollution from solid fuels, although the proportion of risk factors remains significantly higher than in China and the United States. Additionally, there is a rising trend in environmental particulate pollution in India, which requires specific attention.
Data Sharing Statement
This research is based on publicly available data from the Global Burden of Disease Study 2019. The data can be freely downloaded from the IHME data repository (http://ghdx.healthdata.org/gbd-results-tool) without requiring any download permissions.
Ethics Statement
The Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University has granted an exemption from ethical approval, as the Global Burden of Disease Research Database is publicly accessible, and all participant data is based on non-interventional studies and is anonymous.
Acknowledgments
The authors extend their gratitude to the Global Burden of Disease Study team for providing this data, enabling us to conduct our research smoothly. Baojun Guo and Hui Gan should be regard as co-first authors.
Funding
This study was supported by Zhong Nanshan Medical Foundation of Guangdong Province (ZNSXS-20220015).
Disclosure
The authors declare that this work has no conflicts of interest.
References
1. Fazleen A, Wilkinson T. Early COPD: current evidence for diagnosis and management. Ther Adv Respir Dis. 2020;14:1753466620942128. doi:10.1177/1753466620942128
2. Momtazmanesh S, Moghaddam SS, Ghamari S-H. Global burden of chronic respiratory diseases and risk factors, 1990–2019: an update from the Global Burden of Disease Study 2019. EClinicalMedicine. 2023;59:101936. doi:10.1016/j.eclinm.2023.101936
3. Zou J, Sun T, Song X, et al. Distributions and trends of the global burden of COPD attributable to risk factors by SDI, age, and sex from 1990 to 2019: a systematic analysis of GBD 2019 data. Respir Res. 2022;23(1):90. doi:10.1186/s12931-022-02011-y
4. Hansel NN, McCormack MC, Kim V. The effects of air pollution and temperature on COPD. COPD. 2016;13(3):372–379. doi:10.3109/15412555.2015.1089846
5. Liu Z, Jiang Y, Yuan H, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–683. doi:10.1016/j.jhep.2018.12.001
6. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
7. Irimata KE, Bastian BA, Clarke TC, Curtin SC, Badwe R, Rui P. Guidance for selecting model options in the national cancer institute joinpoint regression software. Vital Health Stat Ser 1. 2022;194:1–22.
8. Ilie O-D, Ciobica A, Doroftei B. Testing the accuracy of the ARIMA models in forecasting the spreading of COVID-19 and the associated mortality rate. Medicina. 2020;56(11):566. doi:10.3390/medicina56110566
9. Li M, Hanxiang C, Na Z, et al. Burden of COPD in China and the global from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. BMJ Open Respir Res. 2023;10(1):e001698. doi:10.1136/bmjresp-2023-001698
10. Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi:10.1164/rccm.200703-456SO
11. Mehrotra R, Yadav A, Sinha DN, et al. Smokeless tobacco control in 180 countries across the globe: call to action for full implementation of WHO FCTC measures. Lancet Oncol. 2019;20(4):e208–e217. doi:10.1016/S1470-2045(19)30084-1
12. Chaly PE. Tobacco control in India. Indian J Dent Res. 2007;18(1):2–5. doi:10.4103/0970-9290.30913
13. Yang G, Wang Y, Wu Y, Yang J, Wan X. The road to effective tobacco control in China. Lancet. 2015;385(9972):1019–1028. doi:10.1016/S0140-6736(15)60174-X
14. Marynak K, Mahoney M, Williams KS, Tynan MA, Reimels E, King BA. State and territorial laws prohibiting sales of tobacco products to persons aged <21 years - United States, December 20, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(7):189–192. doi:10.15585/mmwr.mm6907a3
15. Li R, Zhou R, Zhang J. Function of PM2.5 in the pathogenesis of lung cancer and chronic airway inflammatory diseases. Oncol Lett. 2018;15(5):7506–7514. doi:10.3892/ol.2018.8355
16. Zock JP, Sunyer J, Kogevinas M, Kromhout H, Burney P, Antó JM. Occupation, chronic bronchitis, and lung function in young adults. An international study. Am J Respir Crit Care Med. 2001;163(7):1572–1577. doi:10.1164/ajrccm.163.7.2004195
17. Fullerton DG, Semple S, Kalambo F, et al. Biomass fuel use and indoor air pollution in homes in Malawi. Occup Environ Med. 2009;66(11):777–783. doi:10.1136/oem.2008.045013
18. Lv J, Su M, Hong Z, et al. Implementation of the WHO framework convention on tobacco control in mainland China. Tob Control. 2011;20(4):309–314. doi:10.1136/tc.2010.040352
19. Li Z, Zhang Q, Li Z, et al. Effects of straw mulching and nitrogen application rates on crop yields, fertilizer use efficiency, and greenhouse gas emissions of summer maize. Sci Total Environ. 2022;847:157681. doi:10.1016/j.scitotenv.2022.157681
20. Rice MB, Motto Malea N, Pinkerton KE, et al. Realizing the Paris climate agreement to improve cardiopulmonary health. Where science meets policy. Ann Am Thoracic Soc. 2018;15(7):791–798. doi:10.1513/AnnalsATS.201803-203PS
21. Qi G, Wang Z, Wei L, Wang Z. Multidimensional effects of urbanization on PM(2.5) concentration in China. Environ Sci Pollut Res Int. 2022;29(51):77081–77096. doi:10.1007/s11356-022-21298-4
22. Shao Q, Tao R, Luca MM. The effect of urbanization on health care expenditure: evidence from China. Front Public Health. 2022;10:850872. doi:10.3389/fpubh.2022.850872
23. Qiu AY, Leng S, McCormack M, Peden DB, Sood A. Lung effects of household air pollution. J Allergy Clin Immunol Pract. 2022;10(11):2807–2819. doi:10.1016/j.jaip.2022.08.031
24. Hansel NN, Putcha N, Woo H, et al. Randomized clinical trial of air cleaners to improve indoor air quality and chronic obstructive pulmonary disease health: results of the CLEAN AIR Study. Am J Respir Crit Care Med. 2022;205(4):421–430. doi:10.1164/rccm.202103-0604OC
25. Fazlzadeh M, Hassanvand MS, Nabizadeh R, Shamsipour M, Salarifar M, Naddafi K. Effect of portable air purifier on indoor air quality: reduced exposure to particulate matter and health risk assessment. Environ Monit Assess. 2022;194(9):638. doi:10.1007/s10661-022-10255-w
26. Ali J, Khan W. Factors affecting access to clean cooking fuel among rural households in India during COVID-19 pandemic. Energy Sustain Dev. 2022;67:102–111. doi:10.1016/j.esd.2022.01.006
27. Islam S, Rana MJ, Shupler M. Deepened socioeconomic inequality in clean cooking fuel use in India from 2005–2006 to 2015–2016. Heliyon. 2023;9(6):e17041. doi:10.1016/j.heliyon.2023.e17041
28. Aryal S, Diaz-Guzman E, Mannino DM. COPD and gender differences: an update. Transl Res. 2013;162(4):208–218. doi:10.1016/j.trsl.2013.04.003
29. Tam A, Morrish D, Wadsworth S, Dorscheid D, Man SF, Sin DD. The role of female hormones on lung function in chronic lung diseases. BMC Womens Health. 2011;11:24. doi:10.1186/1472-6874-11-24
30. Sayiner A, Hague C, Ajlan A, et al. Bronchiolitis in young female smokers. Respir Med. 2013;107(5):732–738. doi:10.1016/j.rmed.2012.12.023
31. de Torres JP, Casanova C, Montejo de Garcini A, Aguirre-Jaime A, Celli BR. Gender and respiratory factors associated with dyspnea in chronic obstructive pulmonary disease. Respir Res. 2007;8(1):18. doi:10.1186/1465-9921-8-18
32. Yang IA, Jenkins CR, Salvi SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. 2022;10(5):497–511. doi:10.1016/S2213-2600(21)00506-3
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.