Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
The Association Between Metabolic Dysfunction-Associated Fatty Liver Disease and Peripheral Arterial Disease in the Chinese Population
Authors Song XH, Liu B, Lei F, Liu YM, Zhang X, Chen Z, Zhang P, Zhang XJ, She ZG , Cai J, Wang JH, Li H
Received 21 October 2022
Accepted for publication 5 January 2023
Published 10 February 2023 Volume 2023:16 Pages 373—384
DOI https://doi.org/10.2147/DMSO.S394414
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Professor Gian Paolo Fadini
Xiao-Hui Song,1,* Bo Liu,2,3,* Fang Lei,2,4 Ye-Mao Liu,2,5,6 Xingyuan Zhang,2,4 Ze Chen,7 Peng Zhang,2,4 Xiao-Jing Zhang,2,4 Zhi-Gang She,1,2 Jingjing Cai,2,8 Jin-Hua Wang,9 Hongliang Li1– 3,6
1Department of Cardiology, Renmin Hospital of Wuhan University, Wuhan, People’s Republic of China; 2Institute of Model Animal, Wuhan University, Wuhan, People’s Republic of China; 3Medical Science Research Center, Zhongnan Hospital of Wuhan University, Wuhan, People’s Republic of China; 4School of Basic Medical Science, Wuhan University, Wuhan, People’s Republic of China; 5Department of Cardiology, Huanggang Central Hospital of Yangtze University, Huanggang, People’s Republic of China; 6Huanggang Institute of Translational Medicine, Huanggang Central Hospital of Yangtze University, Huanggang, People’s Republic of China; 7Department of Cardiology, Zhongnan Hospital of Wuhan University, Wuhan, People’s Republic of China; 8Department of Cardiology, The Third Xiangya Hospital, Central South University, Changsha, People’s Republic of China; 9Department of Neurology, Huanggang Central Hospital of Yangtze University, Hubei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongliang Li, Department of Cardiology, Renmin Hospital of Wuhan University, Luojia Mount Wuchang, Wuhan, 430072, People’s Republic of China, Tel/Fax +86-27-68759302, Email [email protected] Jin-Hua Wang, Department of Neurology, Huanggang Central Hospital of Yangtze University, Hubei, 438000, People’s Republic of China, Email [email protected]
Purpose: Emerging evidence suggested that metabolic dysfunction-associated fatty liver disease (MAFLD) was significantly associated with atherosclerotic diseases. Atherosclerosis in the peripheral arteries is the most common cause of peripheral arterial disease (PAD), which has not been substantially controlled in the past. We aimed to investigate the association between MAFLD and PAD in the Chinese population.
Patients and Methods: This observational study covered 102,115 participants who underwent health checkups with detailed examinations for PAD and MAFLD. PAD was measured by ankle-brachial index, and MAFLD was diagnosed by abdominal ultrasound. The generalized linear mixed models and random-effects Cox proportional hazards models were used to analyze the relationship between MAFLD and PAD.
Results: The baseline characteristics showed that patients with MAFLD had higher prevalence of PAD compared with those without MAFLD (2.7% vs 2.2%). Compared to non-MAFLD, the individuals with MAFLD were associated with a higher risk of the presence of PAD (adjusted odds ratio: 1.30, 95% confidence interval (CI): 1.19– 1.42, P < 0.001). In the prospective cohort study, 6833 participants underwent a follow-up of 2.76 (standard deviation: 1.36) years, and MAFLD at baseline was a higher risk of associated with incident PAD (adjusted hazards ratio: 1.67, 95% CI: 1.17– 2.38, P = 0.005). Moreover, with the accumulation of metabolic abnormalities, the risk of the PAD was increased in the individuals with MAFLD. Furthermore, MAFLD attributed risk of PAD was more evident in participants without metabolic comorbidities.
Conclusion: MAFLD was associated with a significantly higher risk for the prevalence and incidence of PAD in the Chinese population. The finding suggested that individuals with MAFLD are not only have a higher risk of coronary heart diseases but also have an increased risk of atherosclerosis in peripheral arteries.
Keywords: chronic liver disease, metabolic disorder, arteriosclerosis, cross-sectional study, prospective cohort study
Introduction
Non-alcoholic fatty liver disease (NAFLD) remains the most common chronic liver disease worldwide.1 In recent years, the global prevalence of NAFLD had increased to 25%, drawing great public health concern.2 Metabolic dysfunction-associated fatty liver disease (MAFLD), is an updated term for NAFLD, and its inclusion criteria highlight systemic metabolic disorder (MD) regardless of alcohol consumption or other liver diseases.3,4
MAFLD is not only a liver disease but also a major metabolic disease that leads to cardiovascular diseases (CVD).5–7 Peripheral arterial disease (PAD), a common manifestation of systemic atherosclerosis, has been reported associated with a significantly elevated risk of CVD events and all-cause mortality.8–10 For instance, in a community-based cohort of participants aged 45–64 years, PAD was significantly associated with higher risks of stroke, coronary heart disease (CHD) and heart failure (HF), independent of traditional cardiovascular risk factors.11 Nonetheless, most patients with PAD are asymptomatic but undergo rapid progression in the early stage, which leads to PAD remaining under-recognized and under-treated.9 Therefore, it is important to take detection and prevention of PAD as soon as possible.
Previous studies demonstrated that there was an increased risk of atherosclerosis in NAFLD patients.12 For instance, a systematic review reported that NAFLD increases the risk of subclinical atherosclerosis.13 In addition, a cross-sectional study demonstrated that patients with NAFLD were associated with higher risks of PAD compared with those without NAFLD.14 Recently, a prospective analysis indicated that MAFLD was significantly associated with higher risks of developing subclinical atherosclerosis, including elevated carotid intima-media thickness and elevated brachial ankle pulse wave velocity.15
However, the evidence regarding the association between MAFLD and the risks of PAD diagnosed by ankle-brachial index (ABI) has not been reported. This study aimed to explore the association between MAFLD and PAD. We performed cross-sectional design and prospective cohort design, respectively, based on a multi-center Chinese health check-up population to assess this relationship. The hypothesis of this study is that MAFLD is positively associated with the risk of PAD, and this risk increased with the number of metabolic comorbidities in individuals with MAFLD.
Materials and Methods
Study and Population
This study was designed as a multi-centered, observational study. Initially, we enrolled 102,115 adults with PAD and MAFLD check-up records in 4 hospitals from Beijing and Hubei province, during January 2011 and December 2017. In the cross-sectional study, we excluded 650 subjects with a history of cerebral ischemic stroke, arrhythmia, atrial fibrillation (AF), left ventricular hypertrophy (LVH), valvular heart disease (VHD), rheumatic heart disease (RHD), HF and CHD. At last, 101,465 participants were included in the cross-sectional analysis of the association between PAD and MAFLD (Figure 1A).
The prospective cohort study included adults (age ≥18) with diagnosis of MAFLD and PAD, who underwent the health check-ups between January 2011 and December 2017. Further inclusion criterion was participants without a history of cardiac-cerebral vascular diseases and had at least one follow-up check-up including both MAFLD and PAD before December 2017. In total, 7771 participants were enrolled in the prospective study. Then, the exclusion criteria were as follows: 1) with PAD at baseline examination; 2) follow-up time <1 year. Finally, 6833 participants were involved in the analyses of the relationship between baseline MAFLD and the development of PAD during follow-up (Figure 1B).
Our study complies with the Declaration of Helsinki and was approved by the central ethics board of the Renmin Hospital of Wuhan University and each collaborating hospital in the ethics center. The informed consent of each patient was waived by the ethics committees, which were just for analysis after excluding personally identifiable data.
Data Collection
Anthropometric, blood test, medical history and abdominal ultrasound data were collected from each medical health screening center in the hospital. Every institution was equipped with professional and experienced medical teams. Anthropometric measurements included height, weight, waist circumference (WC) and blood pressure (BP). Body-mass index (BMI) was calculated as weight divided by the square of height (kg/m2). The blood data were measured after overnight fasting, which included fasting blood glucose (FPG), total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), total bilirubin, liver enzyme, creatinine and blood cell. Fibrosis-4 (FIB-4) index was calculated using the published formula: age (years) × aspartate aminotransferase (IU/L) / [platelet count (×109/L) × alanine aminotransferase (IU/L)1/2].16 The estimated glomerular filtration rate (eGFR) was calculated according to the Modification of Diet in Renal Disease equations.17
Diabetes mellitus type 2 (T2DM) was defined as the personal history and the guidelines for the prevention and control of T2DM in China (2017).18 Hypertension was diagnosed according to the Chinese Guidelines for the Prevention and Treatment of Hypertension in 2018.19 Dyslipidemia was defined as at least one of the criteria: 1) LDL-c ≥4.14 mmol/L; 2) HDL-c <1.04 mmol/L; 3) TC ≥6.22 mmol/L; 4) TG ≥2.26 mmol/L; 5) use of lipid-lowering medications.20
MAFLD Definition and Grouping
Fatty liver disease was diagnosed using abdominal ultrasound in accordance with Asia-Pacific guidelines.21 MAFLD was diagnosed by the presence of both fatty liver disease and MD.22 The MD was defined as including any one of the following three conditions: overweight or obesity (defined as BMI ≥ 23 kg/m2); the presence of T2DM; and the presence of the metabolic dysregulation.22 Metabolic dysregulation was defined as the presence of at least two of following: 1) WC ≥90 cm in men and ≥80 cm in women, 2) BP ≥130/85 mmHg or usage of specific drug treatment, 3) TG ≥1.70 mmol/L or usage of specific drug treatment, 4) HDL-c ≥1.0 mmol/L in men and ≥1.3 mmol/L in women or usage of specific drug treatment, 5) prediabetes (FBG = 5.6–6.9 mmol/L or 2-hour post-load glucose levels = 7.8–11.0 mmol/L or hemoglobin A1c = 5.7–6.4%).4
The participants were divided into two groups according to the presence of MAFLD. Furthermore, we divided MAFLD participants into three groups according to the number of MDs: MAFLD with one MD, MAFLD with two MDs and MAFLD with three MDs.
Definitions of PAD
In this study, ABI was determined using an arteriosclerosis detection device from each hospital. It was measured in participants by the specialist during the health examination. We defined participants with PAD as participants with ABI <0.9 (indicative of peripheral atherosclerosis) or ABI ≥1.3 (indicative of vascular calcification) in either leg, in combination with diagnosis standards or results from check-up records.23–25
Statistical Analysis
Data were analyzed in R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria). All continuous variables were expressed as mean (standard deviation), and categorical variables were presented as number (percentage). The t-test or one-way ANOVA was used to evaluate the continuous variables, and Pearson’s chi-squared test or Kruskal–Wallis test was used to evaluate the categorical variables for the comparisons between two or four groups. All P values <0.05 was considered statistically significant.
A generalized linear mixed model was used to calculate the odds ratio (OR) with 95% confidence interval (CI) to analyze the relationship between MAFLD and the presence of PAD in the cross-sectional study. Then, the random-effects Cox proportional hazards model was used for incident PAD in the cohort study. The hazard ratio (HR) and 95% CI were calculated accordingly. In both the generalized linear mixed model and random-effects Cox proportional hazards model, model 1 was adjusted for age and gender, while model 2 was further adjusted for red blood cell, leukocyte count, hemoglobin, platelet count, and eGFR. Furthermore, we performed the stratified analyses in the subgroups, including BMI category, diabetes, hypertension and dyslipidemia, and examined the interactive effects between metabolic factor and MAFLD on the risk for PAD.
Some sensitivity analyses were performed to verify the relationship of MAFLD with the PAD. First, we further adjusted for FIB-4 scores in the models to estimate the relationship between MAFLD and PAD. Second, the MAFLD participants were regrouped into five groups according to the number of metabolic dysregulations in the whole sample and subgroups, including T2DM, non-T2DM, obesity and lean/normal weight. Finally, the subjects with other liver diseases (liver cancer, hepatitis B virus, hepatitis C virus) were excluded, and we reanalysis the association between MAFLD and PAD.
Results
Baseline Characteristics of Individuals in the Cross-Sectional Study
The cross-sectional study participants’ characteristics were shown in Tables 1 and S1. Among the 101,465 participants, 66,235 (65.3%) subjects were male with the mean age was 49.8 (standard deviation [SD] 10.0) years. MAFLD was found in 51.0% of the total population. Compared with non-MAFLD group, those with MAFLD had significantly higher levels of BMI, WC, BP, blood glucose, creatinine, liver enzymes, and more lipid profiles of atherogenic (all P<0.001). Notably, a higher proportion of PAD was found in participants with MAFLD (2.7%) in comparison with those without MAFLD (2.2%).
 |
Table 1 Baseline Characteristics of Participants in the Cross-Sectional Study |
Association Between MAFLD and the Presence of PAD in the Cross-Sectional Population
Risks of the presence of PAD associated with the MAFLD are shown in Table 2. Compared with the non-MAFLD group, after full adjustments, the MAFLD group was significantly associated with the risk of presence of PAD (OR, 1.30; 95% CI, 1.19–1.42) in the generalized linear mixed models. In addition, using the group of non-MAFLD as reference, MAFLD with three MD group (OR, 1.65; 95% CI, 1.43–1.90, P < 0.001) had higher odds for PAD compared MAFLD with two MD group (OR, 1.31; 95% CI, 1.19–1.44, P < 0.001), whereas the MAFLD with one MD group without a significant risk of PAD (OR, 1.06; 95% CI, 0.91–1.23, P = 0.435). The P values for the trends were all significant (Tables S5 and S6).
 |
Table 2 Association Between MAFLD and the Presence of PAD in the Cross-Sectional Analysis |
Baseline Characteristics of Individuals in the Prospective Cohort Study
The detailed clinical characteristics of the prospective cohort were shown in Tables S2 and S3. The proportions of non-MAFLD and MAFLD were 37.3% (2551 participants) and 62.7% (4282 participants), respectively. The mean follow-up period was 2.76 (SD: 1.36) years. Compared to other groups, the participants with MAFLD were more likely to be older and male, accompanied by higher levels of BMI, WC, BP, FBG, LDL-c, TC, TG, creatinine and lower levels of HDL-c at baseline than non-MAFLD. Amongst participants with MAFLD, 17.3% were diabetics, 25.0% with hypertension and 62.0% with dyslipidemia, which were significantly higher compared with non-MAFLD.
Association of MAFLD and the Incidence of PAD in the Prospective Cohort Population
Risks of the incidence of PAD related to MAFLD are shown in Table 3. During the follow-up period, the incident rate of PAD in the non-MAFLD and MAFLD groups was 1.8% (47/2551) and 3.3% (144/4282), respectively. Using the non-MAFLD group as the reference, MAFLD group had an increased risk with the incident of PAD (HR, 1.67; 95% CI, 1.17–2.38; P = 0.005) after adjustments for age, sex, red blood cell, leukocyte count, hemoglobin, platelet count and eGFR. Compared with the non-MAFLD group, the MAFLD with one MD group was not significantly associated with the risk of incident PAD after full adjustment (HR, 1.31; 95% CI, 0.74–2.31; P = 0.350). Participants who have MAFLD with two MDs had a 1.64-fold increased risk of developing PAD (95% CI, 1.13–2.38; P = 0.009). MAFLD with three MD group had a higher risk for PAD than MAFLD with two MD group (HR, 2.27; 95% CI, 1.39–3.71; P = 0.001).
 |
Table 3 The Association Between Baseline MAFLD and the Incidence of PAD in the Prospective Cohort Analysis |
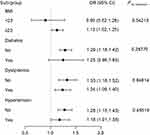
Stratified Analyses of the Association Between MAFLD and PAD
The results of stratified analysis among the participants in the cross-section study and cohort study are shown in Figure 2 and Table S4. When stratified according to metabolic factors, MAFLD was significantly associated with an increased risk of PAD in the BMI ≥ 23 subgroup (OR, 1.13; 95% CI, 1.02–1.25; P < 0.05) but was not in the BMI <23 subgroup (OR, 0.90; 95% CI, 0.62–1.28). In addition, the association between MAFLD and increased risk of the presence of PAD was more evident in subgroups without diabetes (OR, 1.29; 95% CI, 1.18–1.42), without dyslipidemia (OR, 1.33; 95% CI, 1.16–1.52), and without hypertension (OR, 1.28; 95% CI, 1.15–1.43). There was a significant interaction between MAFLD and BMI was detected (Figure 2).
In the prospective cohort sub-group analysis, a significant association between MAFLD and increased risk of incident PAD was observed in subgroups without diabetes (HR, 1.64; 95% CI, 1.13–2.37), with dyslipidemia (HR, 1.92; 95% CI, 1.04–3.52), and without hypertension (HR, 1.61; 95% CI, 1.08–2.41), but no significant interactions were detected (Table S4).
Sensitivity Analysis
We conducted the following sensitivity analyses. First, after further adjusted FIB-4, the relationship between MAFLD and PAD remains robust (Tables 4 and S7). Secondly, using the group of non-MAFLD or MAFLD without metabolic dysregulation as reference, this risk of PAD was increasing with the number of metabolic dysregulations in individuals with MAFLD (Tables S8 and S9). In the sensitive subgroup analysis, compared with the group with non-MAFLD or MAFLD without metabolic dysregulation, the MAFLD with variety metabolic dysregulation had higher risk of PAD in the T2DM, non-T2DM and obesity subgroup (Tables S10 and S11). However, whether in the cross-sectional study or cohort study, there was no significant association between MAFLD with variety metabolic dysregulation and PAD in the lean/normal weight subgroup (Tables S10 and S11). Finally, after excluding the participants with other liver disease, MAFLD was still associated with a significantly elevated risk of PAD (Tables S12 and S13).
 |
Table 4 Sensitivity Test I for PAD in Cross-Section Study After Further Adjusting FIB-4 |
Discussion
To our knowledge, we are the first to investigate the association between MAFLD and PAD in the Chinese population. We found that the risk of PAD was significantly higher in patients with MAFLD than in participants without MAFLD. Moreover, the risk of the presence and incidence of PAD increased with the number of metabolic comorbidities in individuals with MAFLD. Therefore, screening for subclinical atherosclerosis is of great significance in clinical practice for MAFLD patients.
PAD was commonly due to atherosclerosis and associated with a significant risk of cardiovascular disease. A national study estimated that the prevalence of PAD was 4.3% in the participants aged ≥40 years in the United States.26 However, most previous disease burden estimates for PAD have largely originated from studies of people who were older or combined with diabetes, which was likely to be higher than the prevalence in the general population. According to a small-scale cross-section study, the prevalence of PAD was 11.3% in the subjects ≥60 years in Beijing, China.27 In this study, we enrolled the participants aged ≥18 years under the health examination from the North and South area in China. And the prevalence of PAD was 2.5% in the cross-section study, which was lower than some previous epidemiological studies in the Chinese population.28,29 It may be explained by the population difference between the studies. Our population was based on the individuals with annual health examinations, which represents a younger population with better economic status compared to the general population.
Large studies reported that NAFLD was associated independently with atherosclerosis and cardiovascular disease.30,31 For example, a previous cross-sectional study accessed the association between NAFLD and PAD in diabetes patients ≥40 years, which showed that participants with NAFLD had a higher risk of PAD.14 However, with the MAFLD definition established, evidence for the association with PAD is still limited. Our study demonstrated that the MAFLD was a risk of both the presence and development of PAD in adults even after adjusting traditional risk factors for CVD.32 Previous studies have shown that insulin resistance (IR) and high-sensitive C-reactive protein (hs-CRP) were the risks of PAD.33 However, without IR scores and hs-CRP as the condition of MAFLD definition, we still found a significant association between MAFLD and PAD. However, a prospective study reported that NAFLD was not significantly associated with ABI.34 It is essential to assess the association between PAD, measured by repeated ABI, and MAFLD through conducting clinical trials or other analyses in participants with larger scale and variety ethnic. In addition, we further divided people with MAFLD to variety groups according to the variety of metabolic abnormalities in both the cross-section study and cohort study. The results all indicated that the people have the increased risk of PAD with a rising variety of metabolic abnormalities in MAFLD. This finding is consistent with previous findings in NAFLD.34
The etiology of PAD is multifactorial and several risk factors, including obesity, diabetes, high cholesterol level, and hypertension, are actively participated in the development of PAD.9 We further analyzed the association between MAFLD and PAD in individuals with or without these comorbidities. The association between MAFLD and PAD was non-significant in individuals with BMI <23, and more evident in those with BMI ≥23. This may be because people with a lower BMI had a lighter metabolic burden, and thus a longer time of follow-up may be needed to obtain a sufficient number of PAD events. In participants with diabetes or hypertension, the association between MAFLD and PAD was non-significant and less evident. Both diabetes and hypertension are strong risk factors for PAD. A meta-analysis demonstrated that the risk of PAD was increased with the severity of diabetes: for per 1% increase in hemoglobin level, the risk of PAD increased about 0.26 times.35 Hypertension has been reported as importantly related to the risk of PAD, especially in systolic blood pressure (SBP). A study reported that the participants with SBP (during 120–139 mmHg) had a 1.6 folds risk of PAD, compared to the SBP <120 mmHg group.36 Thus, in the presence of diabetes and hypertension, the association between MAFLD and PAD may be weakened due to the existence of multiple confounding factors. For the participants with normal lipid levels, the positive effect between MAFLD and PAD was existent in the cross-section study, but not in the cohort study. It is possible that dyslipidemia is usually via the inflammation to further impact the PAD, and the association between PAD and each component of dyslipidemia was inconsistent.37 Therefore, it takes a longer time to develop atherosclerotic disease in the MAFLD patients with normal lipid levels.
The physiological mechanisms between MAFLD and PAD progression are not fully understood. NAFLD may increase the risk of subclinical atherosclerosis via common and separate mechanisms.38,39 Oxidative stress, IR and systematical inflammation are played a crucial pathophysiological role in PAD.40–42 A recent review about the pathophysiology of PAD in DM reported that increased oxidative stress, inflammatory factors and dyslipidemia may indirectly or directly worsen PAD.43 In addition, the central pathogenesis of NAFLD is IR and increased oxidative stress, and IR. According to the two recent meaningful reviews, IR not only play the important role in the development of NAFLD but also the impact of NAFLD on the IR.44,45 Some mechanistic studies have reported that NAFLD may initiate and accelerate vascular injury through oxidative stress, low-grade inflammation, IR and lipid metabolism.46–48 Therefore, the MAFLD associated with PAD may be due to the oxidative stress, IR and systematic inflammation. Moreover, liver inflammation may directly contribute to the development of some extrahepatic diseases, such as CVD or DM.49 We further adjusted FIB-4 levels in the sensitive study. The results have shown that MAFLD was still associated with PAD.
Based on our finding, it seems that MD plays an important role for the MAFLD and PAD. A cohort study, based on the participants aged above 60 years old and with T2DM, reported that metabolic syndrome was closely associated with PAD.50 As well as, the NAFLD and metabolic syndrome share some common clinical and pathological features, with IR as the most relevant.45 According to the clinical trial, acarbose may be effective in the treatment of the process of non-alcoholic liver cirrhosis.51 Furthermore, a recent systematic review investigated the potential targets and emerging pharmacotherapeutics for NAFLD, which target several aspects of metabolic disruption, oxidative stress and inflammation.52 These drugs may have beneficial effects on PAD by alleviating MAFLD.
In this study, we enrolled large subjects from multicenter to conduct the study, increasing the generalizability of our findings. Moreover, we conduct cross-sectional and longitudinal analysis to examine the association between MAFLD and PAD, which allowed us to obtain robust and reliable results. Compared with the previous study, our study evaluated the effect of MAFLD on the risks of PAD, which fills a gap in PAD and provides evidence for early interventions of MAFLD patients to prevent clinical atherosclerosis. There were several limitations in this study. First, this study was conducted in China, and our results may not be generalizable to other countries and populations. Second, the study subjects were based on health examinations in the city hospital but not random sampling and cannot represent the rural populations in China. Moreover, the variety of smoking and exercise with too much missing data to that the adjusted factors not included these in our study. And our study did not involve medication information. In addition, the specific device that measures the ABI is unable to determine the type due to the multicenter study. Third, due to limited measurement of insulin resistance and high-sensitive C-reactive protein in the health check-up, the diagnosis of MAFLD based on these two indicators was not sufficient. Finally, our study was designed as a cross-section study and prospective cohort study. It is necessary to conduct a long-term cohort study and clinical trials to explore whether treating MAFLD is beneficial to atherosclerosis in the future.
Conclusion
MAFLD was significantly associated with PAD, especially in participants combined with various metabolic abnormalities. Our study provides important evidence on the association between MAFLD and PAD and provided an important early intervention or treatment target of MAFLD for atherosclerosis cardiovascular disease.
Abbreviations
NAFLD, non-alcoholic fatty liver disease; MAFLD, metabolic dysfunction-associated fatty liver disease; MD, metabolic disorder; CVD, cardiovascular diseases; PAD, peripheral arterial diseases; CHD, coronary heart disease; HF, heart failure; ABI, ankle-brachial index; AF, atrial fibrillation; LVH, left ventricular hypertrophy; VHD, valvular heart disease; RHD, rheumatic heart disease; WC, waist circumference; BMI, body-mass index; FBG, fasting blood glucose; TC, total cholesterol; TG, triglyceride; HDL-c, high-density lipoprotein cholesterol; LDL-c, low-density lipoprotein cholesterol; FIB-4, Fibrosis-4; eGFR, estimated glomerular filtration rate; T2DM, Diabetes mellitus type 2; OR, odds ratios; CI, confidence interval; HR, hazard ratio; SD, standard deviation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Science Foundation of China [82170436, 82170595] and the Medical Science Advancement Program of Wuhan University [TFJH2018006].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi:10.1038/nrgastro.2017.109
2. Younossi Z, Tacke F, Arrese M, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019;69(6):2672–2682. doi:10.1002/hep.30251
3. Eslam M, Sanyal AJ, George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999–2014.e1. doi:10.1053/j.gastro.2019.11.312
4. Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209. doi:10.1016/j.jhep.2020.03.039
5. Söderberg C, Stål P, Askling J, et al. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51(2):595–602. doi:10.1002/hep.23314
6. Forlano R, Mullish BH, Nathwani R, Dhar A, Thursz MR, Manousou P. Non-alcoholic fatty liver disease and vascular disease. Curr Vasc Pharmacol. 2021;19(3):269–279. doi:10.2174/1570161118666200318103001
7. Fargion S, Porzio M, Fracanzani AL. Nonalcoholic fatty liver disease and vascular disease: state-of-The-art. World J Gastroenterol. 2014;20(37):13306–13324. doi:10.3748/wjg.v20.i37.13306
8. Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilson PW. The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham Study. Arch Intern Med. 2003;163(16):1939–1942. doi:10.1001/archinte.163.16.1939
9. Morley RL, Sharma A, Horsch AD, Hinchliffe RJ. Peripheral artery disease. BMJ. 2018;360:j5842. doi:10.1136/bmj.j5842
10. Pande RL, Perlstein TS, Beckman JA, Creager MA. Secondary prevention and mortality in peripheral artery disease: national health and nutrition examination study, 1999 to 2004. Circulation. 2011;124(1):17–23. doi:10.1161/circulationaha.110.003954
11. Wang FM, Yang C, Ballew SH, et al. Ankle-brachial index and subsequent risk of incident and recurrent cardiovascular events in older adults: the Atherosclerosis Risk in Communities (ARIC) study. Atherosclerosis. 2021;336:39–47. doi:10.1016/j.atherosclerosis.2021.09.028
12. Huang Y, Bi Y, Xu M, et al. Nonalcoholic fatty liver disease is associated with atherosclerosis in middle-aged and elderly Chinese. Arterioscler Thromb Vasc Biol. 2012;32(9):2321–2326. doi:10.1161/atvbaha.112.252957
13. Ampuero J, Gallego-Durán R, Romero-Gómez M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: meta-analysis. Rev Esp Enferm Dig. 2015;107(1):10–6.
14. Zou Y, Li X, Wang C, et al. Association between non-alcoholic fatty liver disease and peripheral artery disease in patients with type 2 diabetes. Intern Med J. 2017;47(10):1147–1153. doi:10.1111/imj.13549
15. Liu S, Wang J, Wu S, et al. The progression and regression of metabolic dysfunction-associated fatty liver disease are associated with the development of subclinical atherosclerosis: a prospective analysis. Metabolism. 2021;120:154779. doi:10.1016/j.metabol.2021.154779
16. Angulo P, Bugianesi E, Bjornsson ES, et al. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2013;145(4):782–9.e4. doi:10.1053/j.gastro.2013.06.057
17. Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–2944. doi:10.1681/asn.2006040368
18. Chinese Diabetes Society. Clinical guidelines for prevention and treatment of type 2 diabetes mellitus in the elderly in China (2022 edition). Zhonghua nei ke za zhi. 2022;61(1):12–50. Chinese. doi:10.3760/cma.j.cn112138-20211027-00751
19. Liu LS, Wu ZS, Wang JG, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the Revision Committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16(3):182–241. doi:10.11909/j.issn.1671-5411.2019.03.014
20. Joint Committee for Developing Chinese guidelines on P. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua xin xue guan bing za zhi. 2007;35(5):390–419. Chinese.
21. Farrell GC, Chitturi S, Lau GK, Sollano JD. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22(6):775–777. doi:10.1111/j.1440-1746.2007.05002.x
22. Eslam M, Sarin SK, Wong VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14(6):889–919. doi:10.1007/s12072-020-10094-2
23. Alves-Cabratosa L, Elosua-Bayes M, García-Gil M, et al. Hypertension and high ankle brachial index: the overlooked combination. J Hypertens. 2019;37(1):92–98. doi:10.1097/hjh.0000000000001861
24. Newman AB, Siscovick DS, Manolio TA, et al. Ankle-arm index as a marker of atherosclerosis in the cardiovascular health study. Cardiovascular Heart Study (CHS) Collaborative Research Group. Circulation. 1993;88(3):837–845. doi:10.1161/01.cir.88.3.837
25. Aboyans V, Ricco JB, Bartelink MEL, et al. ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763–816. doi:10.1093/eurheartj/ehx095
26. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110(6):738–743. doi:10.1161/01.Cir.0000137913.26087.F0
27. He Y, Jiang Y, Wang J, Fan L, Li X, Hu FB. Prevalence of peripheral arterial disease and its association with smoking in a population-based study in Beijing, China. J Vasc Surg. 2006;44(2):333–338. doi:10.1016/j.jvs.2006.03.032
28. Chuang SY, Chen CH, Cheng CM, Chou P. Combined use of brachial-ankle pulse wave velocity and ankle-brachial index for fast assessment of arteriosclerosis and atherosclerosis in a community. Int J Cardiol. 2005;98(1):99–105. doi:10.1016/j.ijcard.2004.01.019
29. Wang Y, Li J, Xu YW, et al. Prevalence of peripheral arterial disease and correlative risk factors among natural population in China. Zhonghua xin xue guan bing za zhi. 2009;37(12):1127–1131. Chinese.
30. Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65(3):589–600. doi:10.1016/j.jhep.2016.05.013
31. Guleria A, Duseja A, Kalra N, et al. Patients with non-alcoholic fatty liver disease (NAFLD) have an increased risk of atherosclerosis and cardiovascular disease. Trop Gastroenterol. 2013;34(2):74–82. doi:10.7869/tg.2012.101
32. Liu Y, Liu C, Shi X, et al. Correlations of non-alcoholic fatty liver disease and serum uric acid with subclinical atherosclerosis in obese Chinese adults. J Diabetes. 2017;9(6):586–595. doi:10.1111/1753-0407.12441
33. Conte SM, Vale PR. Peripheral arterial disease. Heart Lung Circ. 2018;27(4):427–432. doi:10.1016/j.hlc.2017.10.014
34. Hong HC, Hwang SY, Ryu JY, et al. The synergistic impact of nonalcoholic fatty liver disease and metabolic syndrome on subclinical atherosclerosis. Clin Endocrinol. 2016;84(2):203–209. doi:10.1111/cen.12940
35. Selvin E, Marinopoulos S, Berkenblit G, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141(6):421–431. doi:10.7326/0003-4819-141-6-200409210-00007
36. Aday AW, Matsushita K. Epidemiology of peripheral artery disease and polyvascular disease. Circ Res. 2021;128(12):1818–1832. doi:10.1161/circresaha.121.318535
37. Golledge J, Ward NC, Watts GF. Lipid management in people with peripheral artery disease. Curr Opin Lipidol. 2019;30(6):470–476. doi:10.1097/mol.0000000000000638
38. Luo J, Xu L, Li J, Zhao S. Nonalcoholic fatty liver disease as a potential risk factor of cardiovascular disease. Eur J Gastroenterol Hepatol. 2015;27(3):193–199. doi:10.1097/meg.0000000000000254
39. Cai J, Xu M, Zhang X, Li H. Innate immune signaling in nonalcoholic fatty liver disease and cardiovascular diseases. Annu Rev Pathol. 2019;14:153–184. doi:10.1146/annurev-pathmechdis-012418-013003
40. Rocha-Singh KJ, Zeller T, Jaff MR. Peripheral arterial calcification: prevalence, mechanism, detection, and clinical implications. Catheter Cardiovasc Interv. 2014;83(6):E212–20. doi:10.1002/ccd.25387
41. Signorelli SS, Scuto S, Marino E, Xourafa A, Gaudio A. Oxidative stress in Peripheral Arterial Disease (PAD) mechanism and biomarkers. Antioxidants. 2019;8(9):367. doi:10.3390/antiox8090367
42. Britton KA, Mukamal KJ, Ix JH, et al. Insulin resistance and incident peripheral artery disease in the Cardiovascular Health Study. Vasc Med. 2012;17(2):85–93. doi:10.1177/1358863x11436195
43. Yang SL, Zhu LY, Han R, Sun LL, Li JX, Dou JT. Pathophysiology of peripheral arterial disease in diabetes mellitus. J Diabetes. 2017;9(2):133–140. doi:10.1111/1753-0407.12474
44. Caturano A, Acierno C, Nevola R, et al. Non-alcoholic fatty liver disease: from pathogenesis to clinical impact. Processes. 2021;9(1):135. doi:10.3390/pr9010135
45. Rinaldi L, Pafundi PC, Galiero R, et al. Mechanisms of non-alcoholic fatty liver disease in the metabolic syndrome. A narrative review. Antioxidants. 2021;10(2):270. doi:10.3390/antiox10020270
46. Li W, Liu J, Cai J, et al. NAFLD as a continuous driver in the whole spectrum of vascular disease. J Mol Cell Cardiol. 2022;163:118–132. doi:10.1016/j.yjmcc.2021.10.007
47. Tilg H, From EM. NAFLD to MAFLD: when pathophysiology succeeds. Nat Rev Gastroenterol Hepatol. 2020;17(7):387–388. doi:10.1038/s41575-020-0316-6
48. Lonardo A, Sookoian S, Pirola CJ, Targher G. Non-alcoholic fatty liver disease and risk of cardiovascular disease. Metabolism. 2016;65(8):1136–1150. doi:10.1016/j.metabol.2015.09.017
49. Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69(9):1691–1705. doi:10.1136/gutjnl-2020-320622
50. Gao L, Zhao W, Liu Q, Qin M. Association between metabolic syndrome and peripheral arterial disease in elderly patients with type 2 diabetes. Diabetes Metab Syndr Obes. 2021;14:4783–4789. doi:10.2147/dmso.S343441
51. Gentile S, Turco S, Guarino G, et al. Effect of treatment with acarbose and insulin in patients with non-insulin-dependent diabetes mellitus associated with non-alcoholic liver cirrhosis. Diabetes Obes Metab. 2001;3(1):33–40. doi:10.1046/j.1463-1326.2001.00103.x
52. Negi CK, Babica P, Bajard L, Bienertova-Vasku J, Tarantino G. Insights into the molecular targets and emerging pharmacotherapeutic interventions for nonalcoholic fatty liver disease. Metabolism. 2022;126:154925. doi:10.1016/j.metabol.2021.154925
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.