Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The ARISCAT Risk Index as a Predictor of Pulmonary Complications After Thoracic Surgeries, Almoosa Specialist Hospital, Saudi Arabia
Authors Eldaabossi S, Al-Ghoneimy Y , Ghoneim A, Awad A, Mahdi W, Farouk A, Soliman H, Kanany H, Antar A, Gaber Y, Shaarawy A , Nabawy O, Atef M, Nour SO , Kabil A
Received 23 January 2023
Accepted for publication 28 February 2023
Published 6 March 2023 Volume 2023:16 Pages 625—634
DOI https://doi.org/10.2147/JMDH.S404124
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Safwat Eldaabossi,1,2 Yasser Al-Ghoneimy,3 Ayman Ghoneim,3,4 Amgad Awad,5,6 Waheed Mahdi,2– 7 Abdallah Farouk,8,9 Hesham Soliman,10 Hatem Kanany,11 Ahmad Antar,12 Yasser Gaber,13,14 Ahmed Shaarawy,1 Osama Nabawy,1 Moaz Atef,1 Sameh O Nour,1 Ahmed Kabil1
1Department of Chest Diseases, Al-Azhar University, Cairo, Egypt; 2Pulmonology Department, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 3Cardiothoracic Surgery Department, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 4Department of Cardiothoracic Surgery, Al-Azhar University, Cairo, Egypt; 5Nephrology Department, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 6Department of Internal Medicine, Al-Azhar University, Cairo, Egypt; 7Department of Chest Diseases, Banha Faculty of Medicine, Banha, Egypt; 8Critical Care Consultant, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 9Department of Critical Care, Alexandria Faculty of Medicine, Alexandria, Egypt; 10Consultant and Chief of Anesthesia, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 11Department of Critical Care and Anesthesia, Al-Azhar University, Cairo, Egypt; 12Department of Internal Medicine, Hematology-Oncology Section, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 13Radiology Department, Almoosa Specialist Hospital, Al Ahsa, Saudi Arabia; 14Department of Radiology, Al-Azhar University, Cairo, Egypt
Correspondence: Ahmed Kabil, Department of Chest Diseases, Al-Azhar University, Cairo, Egypt, Tel +201006396601, Email [email protected]
Background: Pulmonary complications after thoracic surgery are common and are associated with prolonged hospital stay, higher costs, and increased mortality. This study aimed to evaluate the value of The Assess Respiratory risk in Surgical Patients in Catalonia (ARISCAT) risk index in predicting pulmonary complications after thoracic surgery.
Methods: This retrospective study was conducted at Almoosa Specialist Hospital, Saudi Arabia, from August 2016 to August 2019 and included 108 patients who underwent thoracic surgery during the study period. Demographic data, ARISCAT risk index score, length of hospital stay, time of chest tube removal, postoperative complications, and time of discharge were recorded.
Results: The study involved 108 patients who met the inclusion criteria. Their mean age was 42.5 ± 18.9 years, and most of them were men (67.6%). Comorbid diseases were present in 53.7%, including mainly type 2 diabetes mellitus and hypertension. FEV1% was measured in 58 patients, with a mean of 71.1 ± 7.3%. The mean ARISCAT score was 39.3 ± 12.4 and ranged from 24 to 76, with more than one-third (35.2%) having a high score grade. The most common surgical procedures were thoracotomy in 47.2%, video-assisted thoracoscopic surgery (VATS) in 28.7%, and mediastinoscopy in 17.6%. Postoperative pulmonary complications (PPCs) occurred in 22 patients (20.4%), mainly pneumonia and atelectasis (9.2%). PPCs occurred most frequently during thoracotomy (68.2%), followed by VATS (13.6%), and mediastinoscopy (9.1%). Multinomial logistic regression of significant risk factors showed that lower FEV1% (OR = 0.88 [0.79– 0.98]; p=0.017), longer ICU length of stay (OR = 1.53 [1.04– 2.25]; p=0.033), a higher ARISCAT score (OR = 1.22 [1.02– 1.47]; p=0.040), and a high ARISCAT grade (OR = 2.77 [1.06– 7.21]; p=0.037) were significant predictors of the occurrence of postoperative complications.
Conclusion: ARISCAT scoring system, lower FEV1% score, and longer ICU stay were significant predictors of postoperative complications. In addition, thoracotomy was also found to be associated with PPCs.
Keywords: thoracic surgery, postoperative complications, pulmonary complications, ARISCAT score, atelectasis, pneumonia
Introduction
Pulmonary complications after thoracic surgery are relatively common and are associated with increased costs, morbidity, and mortality. Thoracic surgery results in impaired postoperative respiratory function due to a decrease in lung volume and capacity, dysfunction of the diaphragm, impaired gas exchange, inefficient cough and mucociliary clearance, such that it may take up to six weeks for the respiratory system to return to its preoperative state. These changes are more pronounced in patients with chronic obstructive pulmonary disease (COPD), advanced age, heart disease, and smokers.1–3
The incidence of postoperative pulmonary complications (PPCs) after thoracic surgery has been reported to range from 5% to 80%. The incidence varies from hospital to hospital and depends on many factors: patient status, type of anesthesia, surgeon experience, details of thoracic surgery procedures, and quality of perioperative care.4 The most common PPCs after thoracic surgery are atelectasis, pneumonia, hemothorax, pulmonary edema, atrial fibrillation, wound infection, persistent air leak, and respiratory failure. Other less common complications include empyema, bronchopleural fistula, cardiac hernia, and others.5
Certain perioperative measures aimed at reducing PPCs, such as smoking cessation and pulmonary physiotherapy, optimization of cardiorespiratory comorbidities, correction of anemia, optimal anesthesia and surgical techniques (early awakening and effective pain management, pulmonary hygiene and physiotherapy, fluid and pain management, and pleural space management), must be taken.6,7
In recent years, several risk indices for preoperative assessment have been developed to predict PPCs, including the American Society of Anesthesiologists Physical Status Classification (ASA), the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT), and the Respiratory Failure Index (RFI).8–10 The ARISCAT score has shown promising results in identifying patients at higher risk for PPCs. The ARISCAT risk index is derived from numerous variables, including age, oxygen saturation, previous respiratory infections, anemia, abdominal or thoracic surgery, duration of surgery, and emergency surgery.9,10 The expected PPCs in these patients may differ from those in other surgical groups because thoracic surgery includes different patient populations with different diseases and different surgical procedures on the thoracic wall, mediastinum, or lung. The ARISCAT risk index is most commonly used for surgeries other than thoracic surgery and may not be appropriate for evaluating PPCs in thoracic surgery.10
This study aimed to evaluate the value of the ARISCAT risk index in predicting PPCs after thoracic surgeries.
Materials and Methods
Study Design and Setting
A retrospective study involving record analysis was conducted at Almoosa Specialist Hospital, one of the largest private hospitals in Al- Ahsa, the Eastern province of the Kingdom of Saudi Arabia with a capacity of 300 beds during the period from August 2016 to August 2019.
Inclusion Criteria
All patients who underwent various types of thoracic surgery (thoracotomy, thoracoscopy (medical and surgical), mediastinoscopy, mediastinotomy, or sternotomy) regardless of age or gender during the study period were included.
Exclusion Criteria
Patients who have not undergone thoracic surgery and patients who have undergone simple outpatient thoracic procedures involving only peripheral or local anesthesia.
Data
The following data were recorded during the preoperative examination: Sex, age, height, body weight, BMI, smoking history, complete blood count (leukocytes, hemoglobin, platelets), liver function tests (liver enzymes, albumin), renal function tests, preoperative oxygen saturation, history of previous surgery, and concomitant diseases (type 2 diabetes, hypertension, pulmonary and cardiac diseases).
The following data were also collected: History and physical examination findings, chest radiographs, computed tomographic examinations of the chest (CT), electrocardiography (ECG) and echocardiography (if required), pulmonary function test results (forced expiratory volume (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio), and arterial blood gases. In patients with lung cancer, the type and stage of malignancy were determined, and flexible bronchoscopy was performed.
During the intraoperative process, the type of endotracheal tube, the duration of anesthesia and surgery, the surgical procedure (VATS, thoracotomy, mediastinoscopy, and others) performed, and complications that required intraoperative treatment were also noted.
PPCs have been defined as complications that occur in the postoperative period and cause clinical conditions.
Score
The ARISCAT risk index is used to predict the following: respiratory failure, bronchospasm, respiratory infections, atelectasis, pneumothorax, pleural effusion, and aspiration pneumonitis.9,10 Atelectasis, pneumonia, or pleural effusion were diagnosed by routine clinical examination, chest radiography (chest x-ray or CT), and other relevant investigations. The risk score was classified as: Low risk: < 26, intermediate risk: 26–44, and High risk: ≥45 (Table 1).
 |
Table 1 Parameters of the ARISCAT Score and Risk Classification |
Other PPCs have also been reported, such as phrenic dysfunction due to phrenic nerve injury, hoarseness due to recurrent laryngeal nerve injury, difficult extubation, wound infection, and other complications. The management of complications, duration of chest drainage, length of ICU and hospital stay, and patient outcomes (discharge or in-hospital mortality) were also recorded.
Ethical Considerations
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from Almoosa Specialized Hospital Review Board (IRB log number: ARC-22.01.02) and exempted from informed consent because it was a retrospective study. All data were collected anonymously. Data protection, privacy, and confidentiality were maintained throughout the study process.
Statistical Analysis
It was performed with the SPSS computer package version 25.0 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp., USA). The data were normally distributed according to the Shapiro–Wilk test. For descriptive statistics, mean ± standard deviation (SD) was used for quantitative variables, and frequency and percentage were used for qualitative variables. Chi-square or Fisher’s exact tests were used to assess differences in the frequency of qualitative variables, whereas the independent-samples t-test was used to assess differences in the means of quantitative variables. Significant variables associated with postoperative complications in the univariate analysis were included in multivariate logistic regression to determine the independent predictors of the development of postoperative complications. The significance level was set at p < 0.05.
Results
The study involved 108 patients who met the inclusion criteria. Their mean age was 42.5 ± 18.9 years and ranged from 3 to 80 years, with approximately two-thirds of them being men (67.6%). Comorbid diseases were present in 58 patients (53.7%), including mainly diabetes mellitus and hypertension. FEV1% was measured in 58 patients with a mean of 71.1 ± 7.3 and a range of 50% to 80%. The mean ARISCAT score was 39.3 ± 12.4 and ranged from 24 to 76, with more than one-third (35.2%) having a high score grade (Table 2).
 |
Table 2 General and Clinical Characteristics of the Studied Patients |
Patients were diagnosed with mediastinal lesions (36 patients), pleural disease (34 patients), pulmonary neoplasms (13 patients), diffuse parenchymal lung disease (8 patients), diaphragmatic problems (three patients), and other lesions in 14 patients. Details of all lesions and procedures are listed in Supplementary Table 1.
Thoracotomy was performed in 51 patients (47.2%), VATS in 31 patients (28.7%), mediastinoscopy in 19 patients (17.6%), and mediastinotomy in two patients (1.9%). Other types of surgery are listed in Table 3, and the site of surgery is shown in Figure 1.
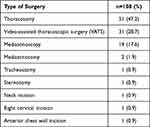 |
Table 3 Type of Surgery for the Studied Patients |
 |
Figure 1 Site of surgery for the study patients. |
The average length of ICU stay was 1.76 ± 1.07 days in 95 patients and ranged from 1 to 7 days. However, three patients received long-term ventilation in the ICU and were not included in the analysis. The mean length of stay in the ward was 3.16 ± 2.1 days and ranged from 1 to 15 days, and the mean length of stay until chest tube removal was 3.78 ± 2.63 days and ranged from 1 to 16 days, including patients treated by thoracotomy and VATS.
Postoperative complications occurred in 22 patients (20.4%), mainly pneumonia and atelectasis (five patients each), phrenic/laryngeal nerve injury (four patients), wound infection and difficult extubation (two patients each), and bronchopleural fistula, hemothorax, surgical emphysema, and acute exacerbation of interstitial lung disease (ILD) (one patient each). Regarding treatment, six patients required systemic antibiotic therapy, four patients required wound care, three patients required supportive care, two patients required systemic steroids, and one patient required noninvasive ventilation. No mortality was recorded (Table 4).
 |
Table 4 Outcomes of Surgery Among the Studied Patients |
Postoperative complications occurred more frequently in patients who had undergone thoracotomy (in 15 patients), followed by VATS (in three patients), mediastinoscopy, and other types of incisions (two patients each). Regarding risk factors for postoperative complications, no significant association was found between the development of postoperative complications and age, gender, presence of comorbidities, days elapsed until chest tube removal, low and intermediate ARISCAT grade, site of surgery, and/or other types of surgery other than thoracotomy. A low FEV1% score (mean 65.4 ± 8.6), longer length of stay in the ICU and in the hospital ward, higher ARISCAT score, high ARISCAT grade, and surgery by thoracotomy were found to be significant risk factors for the occurrence of postoperative complications. Further multinomial logistic regression of the significant risk factors revealed that a lower FEV1% score (OR = 0.88 [0.79–0.98]; p=0.017), a longer ICU length of stay (OR = 1.53 [1.04–2.25]; p=0.033), a higher ARISCAT score (OR = 1.22 [1.02–1.47]; p=0.040), and a high ARISCAT grade (OR = 2.77 [1.06–7.21]; p=0.037) were significant predictors of the occurrence of postoperative complications (Table 5).
 |
Table 5 Association of Different Study Variables as Risk Factors for Post-Operative Complications |
Discussion
PPCs have significant clinical and economic implications that depend on the type of thoracic surgery, type of anesthesia, preoperative health status, concomitant diseases, baseline pulmonary function, and quality of postoperative hospital care.3,5
The incidence of PPCs observed in this study was 20.4%, mainly pneumonia and atelectasis (9.2%), with no mortality reported. This incidence lies within the previously reported PPC rate of 5% to 55% in the literature.1,3,4,11–17 Similar incidence was reported by Bevilacqua et al who found 20% of cases developed PPCs after thoracotomy lung resection with a mortality rate of 5%, and pneumonia was the most common complication.11 However, our incidence was higher than the results reported by Pipanmekaporn et al who included a total of 1488 patients over a 7-year period, of whom 15.8% developed respiratory complications.12 In the study by Lugg et al, the occurrence of PPCs was observed in 13%.13 On the other hand, higher incidence was reported by Baar et al where the overall incidence of PPCs was 27% in a multicenter registry analysis of PPCs after thoracotomy for resection of primary lung cancer.14 The incidence of PPCs after thoracic surgery varies from study to study, mainly because thoracic surgery is heterogeneous and involves many parts of the thorax. There is no standard; it depends on the type of complications included, the definition of pulmonary complications, and the type of procedure.13
In this study, multinomial logistic regression of significant risk factors revealed that a high ARISCAT grade (OR = 2.77 [1.06–7.21]; p=0.037) was a significant predictor of the occurrence of postoperative complications. Ulger et al analyzed data from 120 patients and reported that PPCs developed in 21.7% and the 3-month mortality was 3.3%. The development of PPCs was statistically significant in patients with high ARISCAT scores. A small positive correlation was found between ARISCAT score and the timing of chest tube removal (P <0.001).18 Canet et al reported that the highest rate of PPCs was after cardiac surgery (39.6%), followed by thoracic (31.4%), abdominal (7.2%), and vascular procedures (5.8%), and that ARISCAT grade was statistically significantly higher (P = 0.009) in patients who developed PPCs.9 Gupta et al reported that the incidence of PPCs was 59 out of 1170 patients (5%). Multivariate analysis showed that patients with intermediate and high ARISCAT scoring had a higher risk of developing PPCs.19 Shaik et al studied the ARISCAT risk index to predict PPCs in patients undergoing elective or emergency surgical procedures, at a single center in India and reported that 55.6% of patients developed PPCs after intrathoracic procedures. The incidence of PPCs was higher in the high-risk group (45.7%) than in the intermediate- risk (17.6%) and low-risk (2.5%) groups.20 This was consistent with the study by Mazo et al which showed that the incidence of PPCs was higher in the high-risk group (38.01%) than in the intermediate- risk group (12.98%) and the low-risk group (3.39%) and found that it performed differently in different European geographic areas; it performed well in a Western European subsample.10
Other PPCs such as phrenic nerve injury, recurrent laryngeal nerve injury, hemothorax, and persistent air leak were not assessed with the ARICAST score. Thoracic surgery may result in injury to the phrenic nerve and recurrent laryngeal nerve, which may be temporary or permanent.21 In this study, four patients (3.7%) sustained injuries to the phrenic and laryngeal nerves. One of the most common problems after thoracic surgery is persistent postoperative air leak (28% to 60%), with most leaks resolving spontaneously by the fourth postoperative day.22 In this study, one patient (0.9%) experienced a persistent postoperative air leak which was treated by intrapleural injection of 100 mL of autologous blood through the intercostal chest drain. Bleeding after thoracic surgery is rare, occurring in less than 2% of VATS and in approximately 01% to 3% of open procedures.23 In this study, one patient (0.9%) had hemothorax after VATS bullectomy and pleurodesis for pneumothorax and was treated conservatively with blood transfusion.
In this study, PPCs occurred most frequently during thoracotomy (in 47.2%), followed by VATS (28.7%), and mediastinoscopy (17.6%). This is consistent with results from the literature and studies. VATS approach can reduce the incidence of PPCs.24–27 Thoracotomy was associated with a 10-fold higher risk of postoperative complications compared with VATS and was an independent risk factor for surgical complications.28–32
Multinomial logistic regression in our study showed that a low FEV1% score (OR = 0.88 [0.79–0.98]; p=0.017) was a significant predictor of the occurrence of postoperative complications. FEV1% may be useful to categorize the severity of underlying lung disease. Functional status has also been shown to influence outcomes.33 Berry et al showed that FEV1% is an independent predictor of PPCs,29 which is consistent with our findings. However, FEV1% is often less reliable in patients with airway obstruction.34 Studies have shown that older age is an important factor in the development of PPCs.5,35–37 In addition, male gender has been shown to be a risk factor for the development of PPCs.38 This is in contradiction with our results where both age and gender showed no significant association with the development of postoperative complications.
Limitations of the Study
The study has some limitations including the retrospective records review design, a single center study with a heterogeneous patient population, a small sample size, and possible selection bias. In addition, variables predicting postoperative complications may be modifiable and even a strong statistical association does not necessarily indicate a cause-effect relationship. Also, possible confounding effect caused by unmeasured covariates may occur as some independent risk factors were not investigated that may pose an increased risk for PPCs such as obesity, smoking, anemia, etc. Also, we did not include some of the other surgical risk scores as Respiratory Failure Risk score in the current study for more future studies covering this issue. Finally, we did not evaluate the risk factors for PPCs independently for each type of surgery and we are not sure about the long-term survival as we reviewed only in-hospital mortality.
Conclusions
ARISCAT scoring system, lower FEV1% score, and longer ICU stay were significant predictors of postoperative complications. Multicenter prospective studies in more specific patient populations are needed to more accurately determine the parameters that are successful in estimating PPCs and to enable future management plans of those at higher risk of postoperative and even preoperative complications.
Acknowledgment
The authors would like to acknowledge all of the members at Almoosa Specialized Hospital for their help and support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax. 2010;65:815–818. doi:10.1136/thx.2009.123083
2. Alnassar S. thoracic surgery: opportunities and challenges in Saudi Arabia. Ann Pak Inst Med Sci. 2018;14(4):252–255. doi:10.48036/apims.v14i4.191
3. Iyer A, Yadav S. Postoperative Care and Complications After Thoracic Surgery. In: Firstenberg MS. Principles and Practice of Cardiothoracic Surgery. London: IntechOpen; 2013.
4. Sengupta S. Post-operative pulmonary complications after thoracotomy. Indian J Anaesth. 2015;59:618–626. doi:10.4103/0019-5049.165852
5. Miskovic A, Lumb B. Postoperative pulmonary complications. Br J Anaesth. 2017;118:317–334. doi:10.1093/bja/aex002
6. Myles PS. Complications of thoracic surgery. In: Alston RP, Myles PS, Ranucci M editors. Oxford Textbook of Cardiothoracic Anaesthesia, Oxford Textbook in Anaesthesia, Oxford Academic. Oxford University Press;2015. doi:10.1093/med/9780199653478.003.0037
7. Demmy TL, Nwogu C. Is video-assisted thoracic surgery lobectomy better? Quality of life considerations. Ann Thorac Surg. 2008;85(2):S719–S28. doi:10.1016/j.athoracsur.2007.09.056
8. Doyle DJ, Hendrix JM, Garmon EH. American Society of Anesthesiologists Classification. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
9. Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–1350. doi:10.1097/ALN.0b013e3181fc6e0a
10. Mazo V, Sabaté S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121(2):219–231. doi:10.1097/ALN.0000000000000334
11. Bevilacqua Filho CT, Schmidt AP, Felix EA, Bianchi F, Guerra FM, Andrade CF. Risk factors for postoperative pulmonary complications and prolonged hospital stay in pulmonary resection patients: a retrospective study. Braz J Anesthesiol. 2021;71(4):333–338. doi:10.1016/j.bjane.2021.02.003
12. Pipanmekaporn T, Bunchungmongkol N, Punjasawadwong Y, Lapisatepun W, Tantraworasin A, Saokaew S. A risk score for predicting respiratory complications after thoracic surgery. Asian Cardiovas Thorac Ann. 2019;27:278–287. doi:10.1177/0218492319835994
13. Lugg ST, Agostini PJ, Tikka T, et al. Long-term impact of developing a postoperative pulmonary complication after lung surgery. Thorax. 2016;71:171–176. doi:10.1136/thoraxjnl-2015-207697
14. Baar W, Semmelmann A, Knoerlein J, et al. Risk factors for postoperative pulmonary complications leading to increase in-hospital mortality in patients undergoing thoracotomy for primary lung cancer resection: a multicentre retrospective cohort study of the German thorax registry. J Clin Med. 2022;11:5774. doi:10.3390/jcm11195774
15. Agostini P, Naidu B, Cieslik H, et al. Comparison of recognition tools for postoperative pulmonary complications following thoracotomy. Physiotherapy. 2011;97(4):278–283. doi:10.1016/j.physio.2010.11.007
16. Arslantas MK, Kara HV, Tuncer BB, et al. Effect of the amount of intraoperative fluid administration on postoperative pulmonary complications following anatomic lung resections. J Thorac Cardiovasc Surg. 2015;149(1):314–321. doi:10.1016/j.jtcvs.2014.08.071
17. Ellenberger C, Garofano N, Reynaud T, et al. Patient and procedural features predicting early and mid-term outcome after radical surgery for non-small cell lung cancer. J Thorac Dis. 2018;10(11):6020–6029. doi:10.21037/jtd.2018.10.36
18. Ülger G, Sazak H, Baldemir R, et al. The effectiveness of ARISCAT Risk Index, other scoring systems, and parameters in predicting pulmonary complications after thoracic surgery. Medicine. 2022;101(30):e29723. doi:10.1097/MD.0000000000029723
19. Gupta S, Fernandes RJ, Rao JS, Dhanpal R. Perioperative risk factors for pulmonary complications after non-cardiac surgery. J Anaesthesiol Clin Pharmacol. 2020;36(1):88–93. doi:10.4103/joacp.JOACP_54_19
20. Shaik VT, Ilangho RP, Bhaskaran K. Utility of ARICAST (Assess respiratory risk in surgical patients in Catalonia) score in predicting postoperative pulmonary complications in patients undergoing elective/emergency surgery in a tertiary care Hospital in India. J Assoc Pulmonologist Tamilnadu. 2021;4(3):94–103. doi:10.4103/japt.japt_38_21
21. Haithcock BE, Feins RH. Complications of Pulmonary Resection: injury to the phrenic nerve. In: Shields TW, LoCicero J, Reed CE, Feins RH, editors. General Thoracic Surgery.
22. Zhao K, Mei J, Xia C, et al. Prolonged air leak after video-assisted thoracic surgery lung cancer resection: risk factors and its effect on postoperative clinical recovery. J Thorac Dis. 2017;9(5):1219–1225. doi:10.21037/jtd.2017.04.31
23. Kuroda H, Dejima H, Mizumo T, Sakakura N, Sakao Y. A new Liga-Sure technique for the formation of segmental plane by intravenous indocyanine green fluorescence during thoracoscopic anatomical segmentectomy. J Thorac Dis. 2016;8(6):1210–1216. doi:10.21037/jtd.2016.04.61
24. Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg. 2009;138(2):419–425. doi:10.1016/j.jtcvs.2009.04.026
25. Agostini P, Lugg ST, Adams K, et al. Postoperative pulmonary complications and rehabilitation requirements following lobectomy: a propensity score matched study of patients undergoing video-assisted thoracoscopic surgery versus thoracotomy. Interact Cardiovasc Thorac Surg. 2017;24(6):931–937. doi:10.1093/icvts/ivx002
26. Cao C, Manganas C, Ang SC, Peeceeyen S, Yan TD. Video-assisted thoracic surgery versus open thoracotomy for non-small cell lung cancer: a meta-analysis of propensity score-matched patients. Interact Cardiovasc Thorac Surg. 2013;16(3):244–249. doi:10.1093/icvts/ivs472
27. Laursen LO, Petersen RH, Hansen HJ, Jensen TK, Ravn J, Konge L. Video-assisted thoracoscopic surgery lobectomy for lung cancer is associated with a lower 30-day morbidity compared with lobectomy by thoracotomy. Eur J Cardiothorac Surg. 2016;49(3):870–875. doi:10.1093/ejcts/ezv205
28. Galata C, Karampinis I, Roessner ED, Stamenovic D. Risk factors for surgical complications after anatomic lung resections in the era of VATS and ERAS. Thorac Cancer. 2021;12(23):3255–3262. doi:10.1111/1759-7714.14197
29. Berry MF, Villamizar-Ortiz NR, Tong BC, et al. Pulmonary function tests do not predict pulmonary complications after thoracoscopic lobectomy. Ann Thorac Surg. 2010;89(4):1044–1052. doi:10.1016/j.athoracsur.2009.12.065
30. Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg. 2010;139(4):976–983. doi:10.1016/j.jtcvs.2009.11.059
31. Wang Z, Zhang J, Cheng Z, et al. Factors affecting major morbidity after video-assisted thoracic surgery for lung cancer. J Surg Res. 2014;192(2):628–634. doi:10.1016/j.jss.2014.07.051
32. Yang J, Xia Y, Yang Y, et al. Risk factors for major adverse events of video-assisted thoracic surgery lobectomy for lung cancer. Int J Med Sci. 2014;11(9):863–869. doi:10.7150/ijms.8912
33. Zhang R, Lee SM, Wigfield C, Vigneswaran WT, Ferguson MK. Lung function predicts pulmonary complications regardless of the surgical approach. Ann Thorac Surg. 2015;99(5):1761–1767. doi:10.1016/j.athoracsur.2015.01.030
34. Brunelli A, Al Refai M, Monteverde M, Sabbatini A, Xiume F, Fianchini A. Predictors of early morbidity after major lung resection in patients with and without airflow limitation. Ann Thorac Surg. 2002;74(4):999–1003. doi:10.1016/s0003-4975(02)03852-3
35. Jammer I, Wickboldt N, Sander M, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32(2):88–105. doi:10.1097/EJA.0000000000000118
36. Tilak KM, Litake MM, Shingada KV. Study of risk, incidence and mortality associated with postoperative pulmonary complications using assess respiratory risk in surgical patients in Catalonia score. Int Surg J. 2019;6(9):3215–3222. doi:10.18203/2349-2902.isj20194054
37. Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(4):544–550. doi:10.1016/j.amjsurg.2013.03.012
38. Ramachandran SK, Nafiu OO, Ghaferi A, Tremper KK, Shanks A, Kheterpal S. Independent predictors and outcomes of unanticipated early postoperative tracheal intubation after nonemergent, noncardiac surgery. Anesthesiology. 2011;115(1):44–53. doi:10.1097/ALN.0b013e31821cf6de
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
