Back to Journals » Clinical Ophthalmology » Volume 16
The Application of Artificial Intelligence in the Analysis of Biomarkers for Diagnosis and Management of Uveitis and Uveal Melanoma: A Systematic Review
Authors Bassi A , Krance SH, Pucchio A , Pur DR, Miranda RN , Felfeli T
Received 13 June 2022
Accepted for publication 16 August 2022
Published 30 August 2022 Volume 2022:16 Pages 2895—2908
DOI https://doi.org/10.2147/OPTH.S377358
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Arshpreet Bassi,1 Saffire H Krance,1 Aidan Pucchio,2 Daiana R Pur,1 Rafael N Miranda,3,4 Tina Felfeli3– 5
1Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada; 2School of Medicine, Queen’s University, Kingston, Ontario, Canada; 3Toronto Health Economics and Technology Assessment Collaborative, Toronto, Ontario, Canada; 4The Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, Ontario, Canada; 5Department of Ophthalmology and Visual Sciences, University of Toronto, Toronto, Ontario, Canada
Correspondence: Tina Felfeli, Department of Ophthalmology and Visual Sciences, University of Toronto, 340 College Street, Suite 400, Toronto, ON M5T 3A9, Canada, Fax +416-978-4590, Email [email protected]
Purpose: This study aims to identify the available literature describing the utilization of artificial intelligence (AI) as a clinical tool in uveal diseases.
Methods: A comprehensive literature search was conducted in 5 electronic databases, finding studies relating to AI and uveal diseases.
Results: After screening 10,258 studies,18 studies met the inclusion criteria. Uveal melanoma (44%) and uveitis (56%) were the two uveal diseases examined. Ten studies (56%) used complex AI, while 13 studies (72%) used regression methods. Lactate dehydrogenase (LDH), found in 50% of studies concerning uveal melanoma, was the only biomarker that overlapped in multiple studies. However, 94% of studies highlighted that the biomarkers of interest were significant.
Conclusion: This study highlights the value of using complex and simple AI tools as a clinical tool in uveal diseases. Particularly, complex AI methods can be used to weigh the merit of significant biomarkers, such as LDH, in order to create staging tools and predict treatment outcomes.
Keywords: uveal melanoma, uveitis, artificial intelligence, biomarkers
Introduction
The uvea of the eye is a highly vascular structure including the anterior uvea and the posterior uvea or choroid,1 which are susceptible to breakdown of the blood-aqueous barrier and inflammatory response in cases of various diseases. Uveitis is a common sight-threatening disease that leads to 5–10% of vision impairment worldwide.2 It has been suggested that there are several markers that can predict the prognosis of the disease, pathogenesis and treatment outcome.3,4 Sauer et al found that elevated levels of interleukin (IL)-1β, IL-2, IL-6, interferon (IFN)-γ and tissue necrosis factor (TNF)-α may be implicated in uveitis.5 Additionally, elevated intraocular levels of IL-6 has been associated with idiopathic uveitis and uveitis in Behçet’s disease, sarcoidosis and ankylosing spondylitis.5 For uveal diseases such as uveal melanoma, the most common primary intraocular malignancy in adults,6 limited information is known on the characteristics that predict survivability for patients.8 Ericsson et al established that Human Leukocyte Antigen (HLA)-I expression is upregulated in metastatic disease resulting in a poor prognosis.9
As artificial intelligence (AI) methods are rapidly progressing, breakthrough technologies are changing the landscape of healthcare research with powerful diagnostic and prognostic value.10 Machine learning methods (also referred to as complex AI), supervised and unsupervised, are employed by AI systems to account for complex interaction either by collecting input data including biofluid and tissue to predict output values based on new input samples or by finding underlying patterns in an unlabelled data set to identify sub-cluster and outliers in the data.10
Although AI methods are well described in other healthcare fields, there is limited information on the value of using AI methods in understanding the complex nature of uveal diseases. Machine learning has allowed for more robust discovery of biomarkers that have been approved by the Food and Drug Administration (FDA) to guide treatment which can be valuable in diseases such as uveitis and uveal melanoma.10 Additionally, the biomarkers act as powerful clinical predictors that can individualize treatment options for patients for more desired outcomes.10
Herein, we aim to systematically review the available literature describing the application of AI methods in uveal diseases, highlighting the important biomarkers identified by AI methods for treatment, prognosis, and disease profile. We also characterize the type of AI methods utilized in uveal disease including sample selection and preferred analysis method, goals of the AI, and guide future research in this ever-evolving field.
Methods
This systematic review adhered to the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines and the protocol was registered in PROSPERO (reg. CRD42020196749).11
Search Strategy
The search strategy was developed with the aid of an expert librarian and was conducted across five electronic databases (EMBASE, Medline, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Web of Science). The search was initially conducted from inception to August 11, 2020, and updated on August 1, 2021. Terms related to the concepts of “ophthalmology” and “AI/bioinformatics” and “proteomics, metabolomics, lipidomics” were used in the formal search to capture all relevant articles (Supplemental File 1). Additionally, backward and forward citation tracking was conducted for completeness. Gray literature indexes were included via EMBASE.
Study Selection Criteria
The inclusion and exclusion criteria were determined prior to screening. The inclusion criteria were as follows: (1) original peer-reviewed studies that analyzed biomarker concentrations to predict or modify patient therapy or outcome/diagnosis in intraocular ophthalmic conditions; (2) studies that analyzed biomarker using any type of AI and/or bioinformatics approaches; (3) articles that studied biomarker samples from vitreous fluid, aqueous fluid, tear fluid, plasma, serum, or ophthalmic biopsies and analyzed a protein, lipid, or metabolite; (4) studies that combined biofluid biomarkers with other types of biomarkers (eg imaging) in their statistical models; and (5) simple regression studies that were longitudinal. The exclusion criteria included (1) articles studying ophthalmic diseases that only affect pediatric patients (eg retinopathy of prematurity), (2) studies on non-human subjects (animal or cell studies), (3) studies utilizing post-mortem samples from eyes, (4) non-English studies, (5) abstracts, or reviews, systemic reviews and meta-analyses. This study is part of a series of review papers focused on use of AI and biofluids, and for this particular study a subset of all studies concerning uveal diseases (uveal melanoma and uveitis) were included.
Study Selection and Data Extraction
All studies identified by the databases were imported into Covidence (Covidence, Veritas Health Innovation, Melbourne, Australia) for screening. Upon automatic removal of duplicate articles, the remaining articles underwent two levels of screening: title and abstract and full text by two independent reviewers. Disagreements were resolved at a follow-up consensus meeting mediated by a third reviewer after each level of screening.
A standardized data collection form developed prior to the commencement of data extraction was used to ensure a comprehensive and consistent extraction. Data was extracted by one reviewer followed by a quality check where 10% of the extractions were verified by a second independent reviewer to ensure consistency of extracted data. Key parameters extracted from each article included study population demographics, biofluid biomarker characterization and significance, and the AI/bioinformatics tool used in the analysis.
Synthesis of Evidence
Data were synthesized for each study including details regarding the biofluid sample, type of analysis conducted, significant biomarkers, and demographic information of mean age and sex. Furthermore, data concerning the type of AI and/or bioinformatic analysis of the biomarkers used in uveal diseases was categorized based on the study objective and utility including disease progression, disease prognosis, disease profile, disease treatment and differentiating between differential diagnosis. Due to the heterogeneity of the study designs and AI methods employed by researchers, a meta-analysis was not undertaken.
Risk of Bias Assessment
The Joanna Briggs Institute Critical Appraisal Tool was used for critical appraisal of the included studies.12 Risk of bias assessment was completed by one independent reviewer, and a quality check of 10% of the articles was completed by a second reviewer to ensure consistency between the data extractors. High ROB was applied to studies that reached up to 49% of questions as “yes”, moderate ROB was classified as 50–69%, and low ROB was classified as greater than 70%.28
Results
The search strategy yielded 27,702 articles from all the databases. After the duplicates were removed, 10,258 studies were screened and a total of 18 studies met the criteria for inclusion in the systematic review. A PRISMA flow-chart summarizing the results of the literature can be found in Figure 1.
 |
Figure 1 PRISMA flow diagram of search strategy. Abbreviation: AI, artificial intelligence. |
Study and Patient Characteristics
The two diseases of interest were uveal melanoma (44%) and uveitis (56%) (Table 1). With regard to study design, 9 studies were cohort studies (50%), 8 are cross-sectional studies (44%) and 1 is a case report (6%). Fifteen studies were conducted retrospectively (83%) and 3 were completed prospectively (17%). The studies were conducted in 9 different countries, with the majority from China (7,39%). The total number of subjects in each study ranged from 18 to 10,453, while the median age of the patients ranged from 30 to 63 years (Table 1).
 |
Table 1 Summary of Study and Patient Characteristics |
Samples and Biomarkers
The most common type of bio-sample taken from the uveal melanoma patients was tissue (63% studies) from of enucleated eyes and aqueous humor in the uveitis patients (50%, Table 2). Other types of biofluid samples were serum, plasma, undifferentiated blood and vitreous humor. The biomarker sample types collected varied across all studies, as 6 studies included cytokines, 6 metabolites, 5 proteins, 2 serum products, 2 at chemokines, 2 at cellular infiltrates, 2 at immune cells, 1 at lipids, 1 at electrolytes, and 1 at stromal cells. Furthermore, the number of individual biomarkers analyzed varied from 1 to 4386 per study with most studies researching less than 10 (50%). Although all except one study found significant biomarkers for their respective study objective, there is little to no overlap in the specific biomarkers found to be significant. The only overlap was that of lactate dehydrogenase (LDH) in 50% of the uveal melanoma studies.8,17–19
 |  |  |  |
Table 2 Summary of Biofluid Samples, Biomarkers and Artificial Intelligence Applications in the Included Studies |
Algorithm/Bioinformatic Applications
Ten (56%) studies used machine learning methods, and 13 (72%) studies used regression methods to interpret the data. Of the 10 studies that used machine learning methods, 2 used unsupervised methods, 3 used supervised methods and 5 used a combination of both methods. The studies that used regression analysis all employed supervised methods. The most common complex AI method used was principal component analysis (33%), whereas logistic regression (38%) analysis was the most common regression tool. Other types of complex AI methods used were artificial neuronal network (6%), hierarchal neural network (6%), decision tree analysis (6%), random forest (6%), partial least square-discriminant analysis (25%), and orthogonal projection to latent structure discriminant analysis (6%). In addition to AI methods, there were 8 studies that conducted analysis using bioinformatics. Bioinformatics was used for either pathway analysis (5 out of 8 bioinformatics studies) or cluster analysis (3 out of 8 bioinformatics studies). Most commonly, the studies that utilized bioinformatics in their methodology did so in order to differentiate between disease diagnosis (4 out of 8 bioinformatics studies) and understand disease profile (4 out of 8 bioinformatics studies). Overall the study objectives included disease progression (6%), disease prognosis (50%), disease treatment (28%), disease profile (22%), and differentiating between differential diagnosis (22%).
Applications of AI in Uveitis
Of the 10 studies focused on uveitis, 4 focused on disease differentiation in which 3 of the 4 studies used machine learning methods. Curnow et al studied cytokine levels of uveitis-presenting diseases such as Behcet's disease, herpes-induced, Fuchs’ heterochromic cyclitis and idiopathic uveitis and used cluster analysis and random forest analysis for disease differentiation and specifically found TH 1 cytokines, IL-6, IL-8, CCL2 and IFNy are elevated in idiopathic uveitis.3 Verhagen et al used PCA and PLS-DA to determine that ketoleucine is upregulated in Human-Leukocyte antigen-B27 (HLA-B27) positive acute anterior uveitis, which can be used to differentiate it from HLA-B27 negative acute anterior uveitis.4 Partial least square discriminant analysis (PLS-DA) was also used by Young et al to differentiate between lens-induced uveitis and chronic uveitis, with a sensitivity of 78% and specificity of 85%.13 Additionally, 3 studies used machine learning methods to examine disease profile.14–16 Guo et al used PLS-DA to identify 33 potential biomarkers and 10 metabolic pathways related to acute anterior uveitis after conducting metabolic analysis.14 Similarly, Xu et al also used PLS-DA to determine specific amino acids and fatty acids to differentiate between controls and uveitis induced by Vogt-Koyanagi-Harada and Behcet’s disease.15 Wang et al used PCA to determine the profile of disease for Posner-Schlossman syndrome-induced uveitis and found 14 significant pathways.16 The remaining studies used regression methods to determine treatment outcomes and prognosis.21,24,26,27
Applications of AI in Uveal Melanoma
Three studies determined factors predictive of treatment outcome; Indini et al used machine learning, whereas Heppt et al, and Nicholas et al used regression methods.17–19 Indini et al used unsupervised artificial neural network analysis (ANN) to determine the importance of baseline factors in predicting response to anti-PD1 treatment in a retrospective cohort patient.17 The specific biomarkers found in blood that showed significance in increasing overall survival and response to treatment value were neutrophil-to-lymphocyte ratio (NLR) and baseline lactate dehydrogenase (LDH).17 Similarly, Heppt et al and Nicholas et al found LDH levels as a significant prognostic factor.18,19 Lastly, all studies for UM found biomarkers significant in determining disease prognosis. While most studies employed regression modeling, 3 studies employed complex AI technology. However, each study used a different algorithm modality; Indini et al, as previously stated, used unsupervised ANN analysis, Sun et al used unsupervised hierarchical neural network and Ehlers et al used supervised principal component analysis.7,17,20 Specifically, Sun et al used hierarchical neural network for recognition of BAP1 expression in tissue samples for prognostic utility.21 Additionally, principal component analysis was conducted by Ehlers et al to analyze microarray expression results to determine that Nbs1 is a highly significant prognostic factor that can stand alone.20 There was one study that used bioinformatics to conduct pathway analysis for disease prognosis.21 CTLA-4 was assessed in 33 types of cancers to determine its expression and pathway via KEGG and GO databases by Zhang et al.22
Quality of Evidence
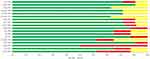
Most of the studies included in this review were of high quality (94%) and 1 was of moderate quality (6%), as highlighted in Figure 2. Of the cohort studies, 56% were unclear in identifying confounding factors and 78% of the studies were unclear or failed to identify strategies to account for the confounding variables. Similarly, 75% of the cohort studies did not describe their strategies for addressing confounding variables. Additionally, all 8 cohort studies (100%) did not clearly define the inclusion criteria for sample selection.
Discussion
To our knowledge, this is the first systematic review that summarises the current advancements of AI for analysis of biomarkers involved in uveal diseases, specifically uveitis and uveal melanoma. Almost all studies found significant biomarkers related to their disease of interest through either regression or machine learning methods, emphasizing the value of AI. However, due to the heterogeneous nature of the biomarkers chosen in each study, no significant biomarkers have been identified consistently across all studies for uveal conditions.
We provided a wide overview of both complex AI methods and regressions models, highlighting their utility. Principal component analysis was used most commonly, in 33% of studies and was found to be a powerful tool to determine significant biomarkers in uveal diseases. Although there is a large variation in types of complex AI used, many showed strong predictive ability. For instance, the value of a random forest analysis was demonstrated by Curnow et al, where with 100% accuracy elevated cytokines were identified in idiopathic uveitis, specifically TH 1 cytokines, IL-6, IL-8, CCL2 and IFNy.3 The results from this study indicate the value of a random forest analysis and its future application in differentiating disease profile of uveitis in Behcet's disease, herpes-induced, and Fuchs’ heterochromic cyclitis with larger sample sizes.3
Considering that uveal melanoma is one of the most common ocular malignancies with a high risk of developing metastatic cancer, it would be beneficial to determine biomarkers that may predict disease progression, prognosis and treatment outcomes.18 Although the number and type of significant biomarker varied from study to study, there was one biomarker that was found significant across multiple studies. Lactate dehydrogenase (LDH) was found to be an important biomarker for disease prognosis and disease treatment outcome by Indini et al, Lorenzo et al, Heppt et al and Nicholas et al.8,17–19 Indini et al determined that elevated baseline serum LDH was negatively correlated with anti-PD1 treatment outcome, whereas Lorenzo et al, Heppt et al and Nicholas et al observed high LDH levels with decreased prognosis.8,17–19 LDH has been previously established as an important prognostic biomarker and is incorporated in staging procedures, such as the Padova-Mayo model and AJCC model.19 The ability to use LDH as a validated prognostic marker supports the idea of biomarkers as valuable prognostic tools.29 However, as highlighted by Indini et al, ANN is able to characterize the importance of such biomarkers in reference to treatment outcomes.17 Identification of important biomarkers involved in uveal diseases may enable better diagnostics and guide treatment decisions.19 In the current review, AI methods are used to confirm previous findings and weigh the significance of LDH against other prognostic variables with respect to treatment outcomes.19 Although the number of studies in this review offers a large amount of information regarding significant biomarkers, with a limited number of studies focusing on each biomarker, it is difficult to recognize definitive biomarkers for diagnostic and prognostic application.
Despite the large amount of data provided by the studies in this review, there are limitations that affect the ability to apply this information in a clinical setting. As assessed by the risk of bias, there were no studies that clearly defined the inclusion criteria for the sample, affecting the generalizability of findings and replicability for future studies. Additionally, there was no mention of the reliability of the biomarker sample collection process, which further affects the bias presented in the studies. This could potentially create confounding variables that were failed to be identified. Additionally, limited information is provided on the specificity and sensitivity of the analytic methods used, making it difficult to assess the precise utility of AI methods.
Conclusion
In the current study, we reviewed the literature on the use of AI or bioinformatics to determine significant biomarkers in disease progression, prognosis, differentiation, profile and treatment outcome of uveitis and uveal melanoma. Particularly, using complex AI methods can be used to weigh the merit of significant biomarkers, such as LDH, in order to create staging tools and predict treatment outcome. Identification of these important biomarkers may guide clinicians in clinical decision-making and optimizing management strategies. Although the information presently available has a large degree of heterogeneity, future studies have the potential of creating impactful AI models that can result in clinical tool development and implementation.
Presentations
The contents of this manuscript may be presented at the International Conference of Ophthalmology (September 9 to September 12, 2022) pending acceptance.
Funding
This research was in-part funded by Fighting Blindness Canada.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Van der Woerdt A. Management of intraocular inflammatory disease. Clin Tech Small Anim Pract. 2001;16(1):58–61. doi:10.1053/svms.2001.22807
2. Tsirouki T, Dastiridou A, Symeonidis C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16. doi:10.1080/09273948.2016.1196713
3. Curnow SJ, Falciani F, Durrani OM, et al. Multiplex bead immunoassay analysis of aqueous humor reveals distinct cytokine profiles in uveitis. Invest Ophthalmol Vis Sci. 2005;46(11):4251. doi:10.1167/iovs.05-0444
4. Verhagen FH, Stigter ECA, Pras-Raves ML, Radstake TRDJ, de Boer JH, Kuiper JJW. Aqueous humor analysis identifies higher branched chain amino acid metabolism as a marker for human leukocyte Antigen-B27 acute anterior uveitis and disease activity. Am J Ophthalmol. 2019;198:97–110. doi:10.1016/j.ajo.2018.10.004
5. Sauer A, Villard O, Creuzot-Garcher C, et al. Intraocular levels of interleukin 17A (IL-17A) and IL-10 as respective determinant markers of toxoplasmosis and viral uveitis. Clin Vaccine Immunol. 2014;22(1):72–78. doi:10.1128/cvi.00423-14
6. Krantz BA, Dave N, Komatsubara KM, Marr BP, Carvajal RD. Uveal melanoma: epidemiology, etiology, and treatment of primary disease. Clin Ophthalmol. 2017;11:279–289. doi:10.2147/opth.s89591
7. Sun M, Zhou W, Qi X, et al. Prediction of BAP1 expression in uveal melanoma using densely-connected deep classification networks. Cancers. 2019;11(10):1579. doi:10.3390/cancers11101579
8. Lorenzo D, Ochoa M, Piulats JM, et al. Prognostic factors and decision tree for long-term survival in metastatic uveal melanoma. Cancer Res Treatment. 2018;50(4):1130–1139. doi:10.4143/crt.2017.171
9. Ericsson C, Seregard S, Bartolazzi A, et al. Association of HLA Class I and Class II Antigen expression and mortality in uveal melanoma. Invest Ophthalmol Vis Sci. 2001;42(10):2153–2156.
10. Yu K-H, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng. 2018;2(10):719–731. doi:10.1038/s41551-018-0305-z
11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097
12. JBI. Critical-appraisal-tools - Critical Appraisal Tools. Joanna Briggs Institute. Jbi.global; 2021. Available from: https://jbi.global/critical-appraisal-tools.
13. Young SP, Nessim M, Falciani F, et al. Metabolomic analysis of human vitreous humor differentiates ocular inflammatory disease; 2009. Available from: Www.molvis.org.http://www.molvis.org/molvis/v15/a129/#sec-discussion.
14. Guo J, Yan T, Bi H, et al. Plasma metabonomics study of the patients with acute anterior uveitis based on ultra-performance liquid chromatography–mass spectrometry. Graefes Arch Clin Exp Ophthalmol. 2014;252(6):925–934. doi:10.1007/s00417-014-2619-1
15. Xu J, Su G, Huang X, et al. Metabolomic analysis of aqueous humor identifies aberrant amino acid and fatty acid metabolism in Vogt-Koyanagi-Harada and Behcet’s disease. Front Immunol. 2021;12. doi:10.3389/fimmu.2021.587393
16. Wang H, Zhai R, Sun Q, et al. Metabolomic profile of Posner–Schlossman syndrome: a gas chromatography time-of-flight mass spectrometry-based approach using aqueous humor. Front Pharmacol. 2019;10. doi:10.3389/fphar.2019.01322
17. Indini A, Di Guardo L, Cimminiello C, De Braud F, Del Vecchio M. Artificial intelligence estimates the importance of baseline factors in predicting response to Anti-PD1 in metastatic melanoma. Am J Clin Oncol. 2019;42(8):643–648. doi:10.1097/coc.0000000000000566
18. Heppt MV, Heinzerling L, Kähler KC, et al. Prognostic factors and outcomes in metastatic uveal melanoma treated with programmed cell death-1 or combined PD-1/cytotoxic T-lymphocyte antigen-4 inhibition. Eur J Cancer. 2017;82:56–65. doi:10.1016/j.ejca.2017.05.038
19. Nicholas MN, Khoja L, Atenafu EG, et al. Prognostic factors for first-line therapy and overall survival of metastatic uveal melanoma: the Princess Margaret Cancer Centre experience. Melanoma Res. 2018;28(6):571–577. doi:10.1097/cmr.0000000000000468
20. Ehlers JP, Harbour JW. NBS1 expression as a prognostic marker in uveal melanoma. Clin Cancer Res. 2005;11(5):1849–1853. doi:10.1158/1078-0432.ccr-04-2054
21. Sun L, Wu R, Xue Q, Wang F, Lu P. Risk factors of uveitis in ankylosing spondylitis. Medicine. 2016;95(28):e4233. doi:10.1097/MD.0000000000004233
22. Zhang C, Chen J, Song Q, et al. Comprehensive analysis of CTLA-4 in the tumor immune microenvironment of 33 cancer types. Int Immunopharmacol. 2020;85:106633. doi:10.1016/j.intimp.2020.106633
23. Armstrong GW, Lorch AC. A(eye): a Review of Current Applications of Artificial Intelligence and Machine Learning in Ophthalmology. Int Ophthalmol Clin. 2020;60(1):57–71. doi:10.1097/iio.0000000000000298
24. Bonacini M, Soriano A, Cimino L, et al. Cytokine profiling in aqueous humor samples from patients with non-infectious uveitis associated with systemic inflammatory diseases. Front Immunol. 2020;11. doi:10.3389/fimmu.2020.00358
25. Johansson CC, Mougiakakos D, Trocme E, et al. Expression and prognostic significance of iNOS in uveal melanoma. Int J Cancer. 2010:NA–NA. doi:10.1002/ijc.24984
26. Cai J, Qi L, Chen Y, et al. Evaluation of factors for predicting risk of uveitis recurrence in Behcet’s disease patients. Braz J Med Biol Res. 2020;53(6). doi:10.1590/1414-431x20209118
27. Fabiani C, Vitale A, Rigante D, et al. Predictors of sustained clinical response in patients with Behçet’s disease-related uveitis treated with infliximab and Adalimumab. Clin Rheumatol. 2018;37(6):1715–1720. doi:10.1007/s10067-018-4092-4
28. Valesan LF, Da-Cas CD, Réus JC, et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig. 2021;25(2):441–453. doi:10.1007/s00784-020-03710-w
29. Palmer SR, Erickson LA, Ichetovkin I, Knauer DJ, Markovic SN. Circulating serologic and molecular biomarkers in malignant melanoma. Mayo Clin Proc. 2011;86(10):981–990. doi:10.4065/mcp.2011.0287
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.