Back to Journals » International Journal of General Medicine » Volume 14
Temporary Ligation of the Bilateral Uterine Arteries During Laparoscopy Combined with Hysteroscopy in the Treatment of Caesarean Scar Pregnancy: Experience at a Chinese Teaching Hospital
Authors Chen R, An J , Guo Q, Lin Q, Yang L, Wang Y
Received 17 February 2021
Accepted for publication 27 April 2021
Published 26 May 2021 Volume 2021:14 Pages 2087—2094
DOI https://doi.org/10.2147/IJGM.S306462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Temporary ligation of the bilateral uterine arteries" [ID 306462].
Views: 442
Ruixin Chen,* Jian An,* Qingfeng Guo, Qingping Lin, Lingling Yang, Yanlong Wang
Department of Gynecology, Women and Children’s Hospital, School of Medicine, Xiamen University, Xiamen, 361000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanlong Wang
Department of Gynecology, Women and Children’s Hospital, School of Medicine, Xiamen University, Xiamen, 361000, People’s Republic of China
Email [email protected]
Purpose: This study aimed to investigate the clinical efficacy of temporary ligation of the bilateral uterine arteries during laparoscopy combined with hysteroscopy in the treatment of caesarean scar pregnancy (CSP).
Patients and Methods: This study was a retrospective analysis of 83 patients who had initially undergone laparoscopy combined with hysteroscopy for CSP between 2012 and 2018 at Xiamen Women and Children’s Hospital. Patients were assigned to the ligation group or the no ligation group according to whether they underwent temporary ligation of the bilateral uterine arteries. Factors extracted from the database included general preoperative information, surgical indicators (intraoperative blood loss, operation time, and blood transfusion), postoperative recovery indicators (β-hCG on day 3 after surgery, time to β-hCG normalization), and postoperative complications (decrease in menstrual bleeding, alteration in the menstrual cycle) and were compared between the two groups.
Results: The intraoperative blood loss of patients in the ligation group was significantly less than that of patients in the no ligation group (P=0.027), especially in patients with higher serum β-hCG level (P=0.030). No significant differences in the operation time, blood transfusion, decline ratio of hCG on day 3 after surgery, reduction in haemoglobin and haematocrit value, decrease in menstrual bleeding, or alteration in the menstrual cycle were observed between the two groups (P> 0.05).
Conclusion: For CSP patients, temporary ligation of the bilateral uterine arteries during laparoscopy combined with hysteroscopy achieved better clinical outcomes than laparoscopy combined with hysteroscopy without ligation with respect to intraoperative blood loss. This approach offers effective and safe surgical management for CSP in clinical practice.
Keywords: artery ligation, hysteroscopy, laparoscopy, intraoperative blood loss
Introduction
The incidence of caesarean scar pregnancy (CSP) has been increasing in recent years.1,2 The underlying reason for this increase may be explained by improvements in ultrasonographic and diagnostic methods,3 improvements in the suturing technique (two layer was changed to one layer),4 and adjustments to a family planning policy in China.5 CSP is no longer a rare long-term complication after caesarean delivery but rather a disease that is often encountered in clinical practice and may cause serious consequences. However, the optimal treatment remains uncertain even though a wide range of management options have been reported.6
Management options, including medicine, embolization, surgery, or combinations of those, should be individually chosen based on the type of CSP, the related factors of patients (eg, gestational week, bleeding quality, and uterine rupture), the appropriate facilities, and physicians’ skills.7 Methotrexate administered locally or systemically is the most common medical management that has been utilized to treat CSP.8 However, this noninvasive regimen does not always work and can be undertaken only in specific situations and selected candidates. On the other hand, surgical treatment, including the resection of CSP tissues by laparotomy, laparoscopy, or transvaginal surgery, is more effective but increases the risk of massive blood loss and is usually followed by fertility-harmed uterine artery embolization in many institutes.9
Hence, after exploring the best treatment strategy for CSP, in the present study, we report our experience with laparoscopy combined with hysteroscopy with temporary ligation of the bilateral uterine arteries in the treatment of CSP and the clinical efficacy of this technique.
Patients and Methods
Study Population
This comparative study was approved by Xiamen Women and Children’s Hospital Institutional Research Ethics Committee, which waived the requirement for informed consent due to the retrospective nature of the study (No: KY-2020-101). We reviewed the medical records of patients with CSP diagnosed and treated at our hospital between January 2012 and May 2018. To maintain data confidentiality, we deidentified through anonymity, and this study was performed in compliance with the Declaration of Helsinki.
A diagnosis of CSP was made based on the Expert Opinion of Diagnosis and Treatment of Cesarean Scar Pregnancy published in the Chinese Journal of Obstetrics and Gynecology.10 CSP is classified as types I, II, and III based on the relationship between the gestational sac and uterine incision scar by ultrasound. Type I: The muscular thickness at the scar in the anterior uterine wall is >3mm without exogenous gestational sac. Type II: The muscular thickness at the scar in the anterior uterine wall is ≤3mm without exogenous gestational sac. Type III: The muscular thickness at the scar in the anterior uterine wall is ≤3mm with exogenous gestational sac. The inclusion criteria were as follows: (1) type II and III CSP: muscular thickness at the scar in the anterior uterine wall ≤3 mm; (2) initial surgical treatments were performed by video laparoscopy combined with hysteroscopy; and (3) uterine artery embolization was not performed before surgery.
Since there is no vascular and interventional radiology department in our hospital, preoperative uterine artery embolization was not carried out in patients with CSP who were initially admitted and treated surgically in our hospital. Based on our experience with laparoscopy and hysteroscopy in a certain number of patients with CSP, we gradually explored a procedure involving temporary ligation of the bilateral uterine arteries to reduce intraoperative and postoperative haemorrhage. Since 2016, this technique has been performed in all patients treated with laparoscopy and hysteroscopy in our department. The no ligation group comprised 45 patients who underwent laparoscopy combined with hysteroscopy without temporary ligation of the bilateral uterine arteries for CSP before 2016. The ligation group comprised 38 patients who underwent laparoscopy combined with hysteroscopy with temporary ligation of the bilateral uterine arteries after 2016.
Surgical Methods
Under general anaesthesia and in the Trendelenburg lithotomy position, the surgery was performed as follows (See Video) and no complications occurred in all patients.
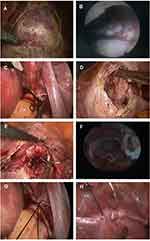
- Laparoscopic and hysteroscopic exploration: Laparoscopy and hysteroscopy were performed to confirm the location of scar pregnancy and its relationship with the caesarean scar. (Figure 1A and B)
- Adhesiolysis and exposure of the lower uterine segment: Adhesiolysis was performed when necessary. After application of a uterine manipulator (with a cup), the serosa of the uterovesical flexion was incised, and the bladder was pushed caudally to achieve sufficient exposure of the lower uterine segment. (Figure 1A)
- Temporary and reversible uterine artery ligation: First, we explored the course of the ureter, and found the location of “water under the bridge” (Uterine artery crosses the ureter above it and at right-angles to it). Then, open the posterior peritoneum, the pulsatile uterine artery can be seen above the ureter. And the uterine artery was dissected and dissociated. Ligature with a removable knot was applied to the bilateral uterine arteries. (Figure 1C) Cyanosis of the uterus is a sign of successful ligation.
- Evacuation of pregnancy tissue: Vacuum aspiration under laparoscopic monitoring.
- Removal of the caesarean scar and residual pregnancy tissues: A transverse incision was made under the guidance of hysteroscopy, and then caesarean scar tissue and residual pregnancy tissues were excised. (Figure 1D)
- Repair of caesarean scar dehiscence: Two layers of continuous sutures were applied to repair scar dehiscence. (Figure 1E)
- Untie ligation and hysteroscopic exploration: The ligation was removed to restore uterine blood supply. Then, hysteroscopic exploration was performed again to assess sutures and to confirm no diverticulum or remnants.(Figure 1F–H)
Clinical Outcome and Follow-Up
Intra-operative blood loss was estimated by weighing swabs and measuring blood volume in the suction devices. The total volume of wash used was subtracted from the total amount of fluid in the suction container so as to get the total blood loss as accurate as possible. During the postoperative recovery period, the following parameters were assessed: serum β-hCG on day 3 after surgery, time at which the serum β-hCG level returned to normal, reduction in haemoglobin (HB) and haematocrit (HCT) values, postoperative residual lesion, decrease in menstrual bleeding (menstrual flow was halved or worse), and alteration in the menstrual cycle (alteration for more than 7 days). The patient’s serum β-hCG level was determined weekly after discharge until it returned to normal. Ultrasound was performed biweekly to observe the residual lesion until it had been completely absorbed.
Statistical Analysis
SPSS 24.0 software (IBM, USA) was used for data analysis. Continuous data that conformed to normal distribution are presented as the means±standard deviations(SD) and were compared using the independent Student’s t-test. Continuous data that did not conform to normal distribution are presented as the median and interquartile range (IQR) and were compared using Mann–Whitney U-tests. Categorical data are presented as the n (%) and were compared using the chi-square test and Fisher exact test. A p value <0.05 was considered statistically significant.
Results
General Data of the Patients
The patients’ baseline characteristics are provided in Table 1. There were no significant differences between the two groups in age, BMI, number of caesarean sections, time from the last caesarean section, time from last menstruation, average diameter of the gestational sac, embryonic length, muscular thickness at the scar, CSP type, HB and HCT before surgery, or MTX treatment (all P>0.05, Table 1). The proportions of patients with ultrasound-confirmed foetal cardiac activity and whose serum β-hCG level normalized before surgery were significantly higher in the ligation group than in the no ligation group (both P<0.05).
 |
Table 1 Comparison of General Data from the Two Groups of Patients |
Clinical Efficacy of Temporary Ligation of the Bilateral Uterine Arteries in Surgery
For all 83 patients, the surgery we conducted was successful, and none of the patients required re-treatment. The difference in the operation time and blood transfusion rate between the two groups was not statistically significant (P>0.05), but intraoperative blood loss was lower in the ligation group (P=0.027) (Table 2). We also performed stratification analysis according to the levels of β-hcg and foetal cardiac activity. And only in patients whose serum β-hCG level>40,000 mIU/mL, intraoperative blood loss was significantly lower in the ligation group (P=0.030) (Tables 3 and 4).
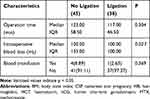 |
Table 2 Comparison of Different Surgical Indicators in the Two Groups of Patients |
 |
Table 3 Stratification Analysis for Surgical Indicators in the Two Groups of Patients According to the Levels of β-Hcg |
 |
Table 4 Stratification Analysis for Surgical Indicators in the Two Groups of Patients According to Foetal Cardiac Activity |
In the follow-up, even though all patients’ serum β-hCG levels in our study eventually returned to normal, the serum β-hCG level on day 3 after surgery was higher in the ligation group, and the time to β-hCG normalization seemed longer in the ligation group (both P<0.05). However, the serum β-hCG level before surgery was significantly higher in the ligation group. We calculated the ratio of β-hCG on day 3 after surgery to β-hCG before surgery and included it in the analysis and found no difference between the two groups. Furthermore, significant differences in decreased menstrual bleeding, reduction in HB and HCT value, or alteration in the menstrual cycle were not observed between the two groups (P>0.05) (Table 5).
 |
Table 5 Comparison of Postoperative Indicators in the Two Groups of Patients |
Discussion
Scar removal and uterine repair have been reported to be some of the best options for CSP11 since the first successful CSP treatment via pregnancy lesion tissue removal was reported in 1978.12 However, uterine rupture, massive haemorrhage and other severe complications are still major concerns in surgery for CSP. Therefore, preoperative uterine artery embolism is widely used in clinical practice to reduce intraoperative and postoperative blood loss. The paradox is that the embolization technique requires specific facilities and may result in postembolization syndrome, pelvic infection, intrauterine adhesions, and fertility impairment in patients.13–15 With this consideration in mind, we explored this procedure involving temporary and reversible ligation of the uterine artery to simultaneously reduce blood loss and preserve fertility when treating patients with CSP.
Our results showed that the procedure involving temporary ligation of the bilateral uterine arteries did not lengthen the operation time but reduced intraoperative blood loss. There are some studies on the application of temporary uterine blood blockage in CSP, and no failed treatment cases or severe complications have been reported. As early as 2009, Persson J reported a successful case of robot-assisted laparoscopic surgery with temporary occlusion of the uterine blood supply in treating CSP.16 With the progress of endoscopic technology, there have been more attempts to improve surgical treatment for CSP. Xu et al17 reviewed a series of CSP cases treated by laparoscopy combined with hysteroscopy with temporary occlusion of the bilateral internal iliac arteries, and all 5 patients had a favourable prognosis. Additionally, a retrospective comparative study of 173 patients with type II and III CSP demonstrated that hysteroscopy and laparoscopy surgery and reversible ligation of the uterine artery achieved better clinical outcomes than other surgical management methods.18 Interestingly, the efficacy in the ligation group seemed inferior to that in the no ligation group because the serum β-hCG level on day 3 after surgery was higher in the ligation group, and the time to β-hCG normalization seemed longer in the ligation group. However, it is worth noting that the serum β-hCG level before surgery was significantly higher than that in the no ligation group. Furthermore, intraoperative blood loss was significantly lower in the ligation group especially in patients with higher serum β-hCG level. A higher level of serum β-hCG usually suggests a higher risk of massive haemorrhage during surgery. Thus, the clinical efficacy of our procedure involving temporary and reversible ligation of the uterine artery was validated to a certain degree since it reduced blood loss in patients at high risks.
Our procedure involving temporary ligation of the bilateral uterine arteries during laparoscopy combined with hysteroscopy achieved better clinical outcomes than no ligation with respect to intraoperative blood loss. Furthermore, it was superior to other management practices in some regards. First, curettage and excision of scar tissue under direct vision with laparoscopy can ensure the complete removal of CSP lesions. Second, temporary and reversible ligation can minimize the negative effect on the blood supply of the uterus and ovary. This procedure may be suitable for patients with CSP who wish to preserve fertility. However, this study had an unavoidable limitation of its retrospective design. Some variables (postoperative thickness of the uterine scar, postoperative fertility outcome, and postoperative ovarian reserve) could not be included, and therefore, the clinical efficacy of our procedure was not evaluated in all respects. This procedure was carried out only in a small number of patients from only a single centre. The external validity of our results was limited, and further prospective studies with larger sample sizes in a broader context are needed.
Conclusion
In summary, temporary ligation of the bilateral uterine arteries during laparoscopy combined with hysteroscopy seems to be a good strategy to reduce the risk of haemorrhage in CSPs. As a treatment option for CSP, it can be applied in clinical practice to reduce intraoperative bleeding and may benefit patients who wish to preserve fertility. To explore the best management for CSP, research confirming the validity and security of this procedure is encouraged.
Funding
This study received the support from Young talent Spark Program of Women and Children’s hospital, School of Medicine, Xiamen University ([2018]26 to Chen RX).
Disclosure
The authors declare no conflicts of interest.
References
1. Drever N, Bertolone J, Shawki M, Janssens S. Caesarean scar ectopic pregnancy: experience from an Australian tertiary centre. Aust N Z J Obstet Gynaecol. 2020;60(3):330–335. doi:10.1111/ajo.13119
2. Uysal F, Uysal A, Adam G. Cesarean scar pregnancy: diagnosis, management, and follow-up. J Ultrasound Med. 2013;32(7):1295–1300. doi:10.7863/ultra.32.7.1295
3. Zanaboni A, Magee M, Gibbons RC, Costantino TG. Point-of-care ultrasound diagnosis of cesarean scar ectopic pregnancy: a case series. J Emerg Med. 2020;undefined. doi:10.1016/j.jemermed.2020.09.035
4. Enkin MW, Wilkinson C. Single versus two layer suturing for closing the uterine incision at caesarean section. Cochrane Database Syst Rev. 2000;2(2):CD000192.
5. Wang L, Xu X, Baker P, et al. Patterns and associated factors of caesarean delivery intention among expectant mothers in China: implications from the implementation of China’s new national twochild policy. Int J Environ Res Public Health. 2016;13(7):undefined.
6. Petersen KB, Hoffmann E, Larsen CR, Nielsen HS. Cesarean scar pregnancy: a systematic review of treatment studies. Fertil Steril. 2016;105(4):958–967. doi:10.1016/j.fertnstert.2015.12.130
7. Wang HY, Zhang J, Li YN, et al. Laparoscopic management or laparoscopy combined with transvaginal management of type II cesarean scar pregnancy. JSLS. 2013;17(2):263–272. doi:10.4293/108680813X13654754535197
8. Levin G, Shai D, Dior UP, et al. Single- versus multiple-dose methotrexate in cesarean scar pregnancies management: treatment and reproductive outcomes. Arch Gynecol Obstet. 2021;undefined. doi:10.1007/s00404-020-05914-7
9. Maheux-Lacroix S, Li F, Bujold E, et al. Cesarean scar pregnancies: a systematic review of treatment options. J Minim Invasive Gynecol. 2017;24(6):915–925. doi:10.1016/j.jmig.2017.05.019
10. Family Planning Subgroup, Chinese Society of Obstetrics and Gynocology, Chinese Medical Association. Expert opinion of diagnosis and treatment of cesarean scar pregnancy. Zhonghua Fu Chan Ke Za Zhi. 2016;51(8):568–572. doi:10.3760/cma.j.issn.0529-567X.2016.08.003
11. Roche C, McDonnell R, Tucker P, et al. Caesarean scar ectopic pregnancy: evolution from medical to surgical management. Aust N Z J Obstet Gynaecol. 2020;60(6):852–857. doi:10.1111/ajo.13241
12. Litwicka K, Greco E. Caesarean scar pregnancy: a review of management options. Curr Opin Obstet Gynecol. 2013;25(6):456–461. doi:10.1097/GCO.0000000000000023
13. Keung JJ, Spies JB, Caridi TM. Uterine artery embolization: a review of current concepts. Best Pract Res Clin Obstet Gynaecol. 2018;46:66–73. doi:10.1016/j.bpobgyn.2017.09.003
14. Arthur R, Kachura J, Liu G, Chan C, Shapiro H. Laparoscopic myomectomy versus uterine artery embolization: long-term impact on markers of ovarian reserve. J Obstet Gynaecol Can. 2014;36(3):240–247. doi:10.1016/S1701-2163(15)30632-0
15. Qi F, Zhou W, Wang MF, Chai ZY, Zheng LZ. Uterine artery embolization with and without local methotrexate infusion for the treatment of cesarean scar pregnancy. Taiwan J Obstet Gynecol. 2015;54(4):376–380. doi:10.1016/j.tjog.2015.01.003
16. Persson J, Gunnarson G, Lindahl B. Robot-assisted laparoscopic surgery of a 12 week scar pregnancy with temporary occlusion of the uterine blood supply. J Robotic Surg. 2009;3(1):53–55. doi:10.1007/s11701-009-0135-9
17. Xu W, Wang M, Li J, Lin X, Wu W, Yang J. Laparoscopic combined hysteroscopic management of cesarean scar pregnancy with temporary occlusion of bilateral internal iliac arteries: a retrospective cohort study. Medicine (Baltimore). 2019;98(37):e17161. doi:10.1097/MD.0000000000017161
18. Huang L, Zhao L, Shi H. Clinical efficacy of combined hysteroscopic and laparoscopic surgery and reversible ligation of the uterine artery for excision and repair of uterine scar in patients with type II and III cesarean scar pregnancy. Med Sci Monit. 2020;26:e924076. doi:10.12659/MSM.924076
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.