Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Tawazon- An Intensive Lifestyle Diabetes Prevention Program: The Saudi Arabian Pilot
Authors Mushcab H , Alsharif F, Nazeer A, Mollah A, Matroud A, Qahtani S, Ghamdi M
Received 4 August 2021
Accepted for publication 3 September 2021
Published 1 October 2021 Volume 2021:14 Pages 2767—2775
DOI https://doi.org/10.2147/JMDH.S331776
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hayat Mushcab, Fawaz Alsharif, Asghar Nazeer, Ali Mollah, Ashwaq Matroud, Saeed Qahtani, Mohammed Ghamdi
Johns Hopkins Aramco Healthcare, Dhahran, Saudi Arabia
Correspondence: Hayat Mushcab
Johns Hopkins Aramco Healthcare, Room 2, Building 1188, Dhahran, Saudi Arabia
Tel +966 556373411
Email [email protected]
Background: Lifestyle modification interventions help prevent or postpone Type 2 Diabetes and its complications with diet modification and increasing physical activity. This is translational research of Tawazon-DPP in which we evaluate the efficacy of the intensive lifestyle modification program.
Methods: Tawazon was piloted in 2 phases over 6 and 9 months at a Tertiary Hospital. Phase I was conducted in 2017 in one district facility with 47 participants while Phase II was conducted in 2018 in 4 district facilities with 247 participants. Data are collected retrospectively in a before-and-after study design. The program included adults with 25 kg/m 2 BMI and HbA1c ranging between 5.7 and 6.4 mmol/L, while excluding participants with comorbidities, such as cardiovascular conditions, musculoskeletal injuries, and pregnancy.
Results: We used descriptive analysis as well as Wilcoxon rank sign test and McNemar-Bowker for before and after data comparisons. Phase I exhibited a mean age of 43± 7 years and statistically significant improvement in HbA1c (0.3 mmol/L), weight (3.3 kg), BMI (1 kg/m 2), triglyceride (30.4 mg/dL) and LDL (14.67 mg/dL). Phase II exhibited a mean age of 45± 9 years with 70% above 40 years old. Significant improvement was also found in HbA1c (0.2 mmol/L), weight (5.1 kg), and BMI (1.8 kg/m 2); the lipid profile in the second phase showed better results with significant improvement in total cholesterol (7.4 mg/dL), triglyceride (20.9 mg/dL), LDL (8.8 mg/dL), and (0.9 mg/dL) increase in HDL.
Conclusion: This pilot has taken lifestyle interventions to real-life and it led to the favored and desired outcome. It showed that long-term guided support can help patients make the needed changes in their diet, habits, and physical activity, thus, prevent or delay the onset of Type 2 diabetes.
Keywords: diabetes, type 2, HbA1c, lifestyle, prevention
Corrigendum for this paper has been published
Introduction
Diabetes is considered one of the leading threats to health worldwide. It is estimated that 9.3% of the global adult population live with diabetes, making it a total of 463 million people between the ages of 20 to 79 years are diagnosed with either type 1 or type 2 diabetes.1,2 It is projected that the number will rise from 300 million in 2010 by 1% in 2030 and 2.6% in 2045 leading to total estimated numbers of 568 million and 700 million respectively.1 These estimates and projections mark Diabetes as an epidemic and a global burden on healthcare.3
Diabetes is a chronic condition characterized by high glucose levels in the blood due to either shortage in the body’s production of insulin or its inability to sufficiently use it (sometimes both).2,4 Daily insulin therapy is essential for people with type 1 diabetes (T1D) which constitutes 5–10% of all people with diabetes.4 However, the vast majority of people with diabetes are diagnosed with the more common type 2 diabetes (T2D) which is characterized by insulin resistance. Patients with T2D can manage their condition with less invasive treatment such as lifestyle change, diet modification, and physical activity.2
Today, diabetes prevails amongst more than 4 million people (18.3%) of the Saudi Arabian adult population imposing a large economic burden on the individuals and the kingdom in general.5,6 People with T2D are at risk for cardiovascular diseases, renal failure, lower limb amputation, blindness, and overall decreased quality of life.7 Research suggests that living a healthy lifestyle, adding physical activity to one’s routine, and making better choices for one’s diet does not just prevent T2D but can also reverse its progress.8 Long-term improvement in insulin sensitivity in people with T2D is called “reversal of diabetes –or remission from diabetes-.9,10 Diabetes remission is achieved when people with T2D are able to reduce their HbA1c to below (6%) without taking diabetes medication,9 however, remission is rarely recorded.10
The Centers for Disease Control and Prevention (CDC) has developed a National Diabetes Prevention Program (DPP) that can help individuals change their lifestyles and build new habits that will last a lifetime.11 In 2016, The Institute for Clinical and Economic Review (ICER) published an Evidence report entitled, “Diabetes Prevention Programs: Effectiveness and Value.” The report concluded that the 10 U.S.-based CDC-recognized DPP provided “an incremental or better” net health benefit versus standard care.12
Our tertiary hospital has adopted the CDC’s diabetes prevention program for pre-diabetic adults at a high risk of progressing to T2D. The program is called “Tawazon”, the Arabic word for “Balance”. In Tawazon, our hospital adopted the DPP and modified it in a way that would accommodate some cultural differences to encourage a drastic conversion to a healthy lifestyle.
While RCTs have shown that primary prevention is possible, population-level approaches are needed for widespread and targeted population benefit. Therefore, translation research is needed to disseminate such interventions to a wider target and this includes utilizing the cultural adaptation process.13 Tawazon-DPP was piloted in 2 phases to tailor the program and optimize it to our Saudi Arabian culture successfully. This is a translational research paper of Tawazon-DPP in which we evaluate the efficacy of the intensive lifestyle modification program to a target audience by including the cultural adaptation process. We assess the efficacy of diet and physical activities on the reduction of A1c levels with patients at risk of developing T2D.
Methods
Study Design
This program was piloted in 2 phases over 6 then 9 months at a tertiary hospital, which is a multi-centered healthcare institution serving the Saudi Aramco community in several districts. This is a retrospective study and data were collected between May 2017 and May 2019 in a before-and-after study design to investigate the effectiveness of the DPP Tawazon intervention program. The program was piloted in 2 phases in order for the program team to involve all the facilities (districts) within our organization and include a larger sample size in a longer period of study in the second phase before embarking on the actual program population-wide. The manuscript is written following the STROBE Statement checklist for observational cohort studies.
Population
The program included participants with Body Mass Index (BMI) of 25 kg/m2 and above, adult participants of 25 years and older, and Hemoglobin A1c (HbA1c) ranging between 5.7 and 6.4 mmol/L. Participants meeting the inclusion criteria but with cardiovascular conditions, musculoskeletal injuries, terminal illnesses, and pregnancy at the time of recruitment were excluded from the program.
Program Description
Tawazon is an intensive lifestyle intervention program, adopted from the CDC’s National Diabetes Prevention Program (DPP). Our hospital is in the process of obtaining the CDC’s approval to be an official partner. National DPP is an evidence-based and cost-effective program that was created a decade ago as a collaboration between public and private organizations in the United States to offer individuals who are at risk for T2D interventions to help prevent diabetes and improve their overall health.14
The DPP aims to deliver lifestyle change programs nationwide while ensuring the quality and adherence to proven standards. This can be achieved by training community organizations that can effectively run a lifestyle change program while increasing coverage by all employers and insurers.15 Organizations aiming to implement the National DPP program take the responsibility for ensuring an adequate workforce that is well-trained to the program’s curriculum is available to deliver such an intensive program.15
The lifestyle change program consists of several sessions that provide the participants with information, outside-of-class activities, and feedback regarding diet modification and their daily physical activity. These sessions are given in stages to gradually optimize behavioral change and make it permanent. The material presented in the lifestyle change program is vital for behavioral and motivational content with mainly one goal in mind which is preventing T2D and the need to make these lifestyle changes long-lasting.15
Sixteen sessions must be conducted in the first 6 months (weeks 1–26) of the DPP lifestyle change program covering the topics presented in Table 1 in Appendix (A). Any of these modules can be repeated after delivering the 16 required core sessions based on the organization’s preference and participants’ needs. In the second half of the program (weeks 27–52) of the program, life coaches will deliver at least one session each month (for a minimum of 6 sessions). Organizations are encouraged to deliver more sessions if the participants ought to need more support.15 All the topics that can be covered in this half of the program are presented in Table 2 in Appendix (A).
The National DPP program is a year-long program, however, Tawazon-DPP was piloted for 6 months for the first phase with one district facility involved in participant recruitment. Then piloted for the second phase after extending the population to include 4 district facilities of the hospital to be able to recruit more participants.
Tawazon-DPP has adopted the National-DPP with cultural adaptation to make it better appealing and acceptable to the population. The adaptation process included the following: 1) material was translated to the Arabic language to accommodate non-English speakers, 2) simplifying the curriculum material to make it easy for all participants to read and understand, 3) recreated the visual material to reflect the Saudi Arabian culture, 4) gender and spoken languages of the trainers and life-coaches were considered with each participant, 5) educational material on food type and nutrition was created based on locally available foods, 6) used social media (WhatsApp) to constantly remind the participants for their sessions rather than using the conventional reminders (emails) alone, 7) healthcare professionals were part of the program delivery system as they are conveyed as the most trusting source of information, 8) Islamic metaphors and examples were utilized to highly motivate participants to be more active (eg, going to a further mosque to perform their prayers and add more steps to their step-count), 9) Food nutrition sessions and recipes were adjusted to accommodate the religious and traditional habits of the holy month of Ramadan, and finally 10) educating the participants on how to deal with social occasion pressure without affecting their diet and physical progress.
Outcome Measures
The primary outcome of the program was the changes in weight and HbA1c from baseline to program completion (6 months for the first phase of the pilot and 9 months for the second phase). Secondary outcome measures included the achievement of the weight loss goal, HbA1c, total cholesterol, HDL, LDL, triglycerides, and change in BMI. In addition to that, patient satisfaction was also a secondary outcome to the program post Phase II.
Data Collection
The program-trained staff collected all variables at baseline and after the completion of the Tawazon program. Data extracted from the participant’s Electronic Health Record (EHR). All participants weigh in at the beginning of every session. Data collection for the pilot was in one district clinic of the hospital’s multiple centers (AB) and it started in May to December 2017. Phase II of the pilot started in September 2018 to May 2019. Finally, an online survey was sent to all participants via SMS upon completion of phase II of the program from the 1st until the 31st of July 2020.
Risk of Bias
All recruited patients were approached by their primary care physician. Any patient who met the criteria was asked to join the program without any selection bias.
Sample Size
The first phase of the pilot study was conducted in 2017 in one of the hospital’s district clinics (AB) with 47 participants. Whereas, 247 participants were enrolled in the second phase of the pilot from all 4 district facilities (DHA, AH, AB, and RT).
Statistical Analysis
Data were entered and analyzed using IBM SPSS Statistics for Windows, Version 24.0 Armonk, NY: IBM Corp. Categorical data were presented as frequencies and percentages while numerical data were presented as mean and standard deviation. Wilcoxon rank sign test was used to compare numerical data before and after the intervention. McNemar-Bowker Test was used to compare categorical data before and after the intervention. The level of significance was set at α=0.05.
Results
Pilot (Phase I)
The pilot was conducted in one district facility (AB) for 6 months from May to December 2017. A total of 47 individuals were initially enrolled in the program and only 27 (57%) completed the program. The mean age of the participants was 43±7 years old and the vast majority of the participants were male 38 (80.8%) and 9(19.2%) were female.
Pre-post changes from baseline to 6 months of the piloted intensive lifestyle change program intervention in all participants are shown in (Table 1). The mean reduction of HbA1c [5.8±0.3 vs 5.5±0.3 mmol/L, P<0.001, effect size= 1.19], mean weight loss measured at [94.5±9.9 vs 91.2±10.9 Kg, P=0.007, effect size= 1.04], leading to a reduced BMI [31.6±3.4 vs 30.6±3.4 kg/m2, P=0.024, effect size=0.024]. The lipid profile showed significant improvement in 2 out of 4 lipid measurements. The total cholesterol and HDL levels showed no significant improvements [197.9±33.9 vs 183.8±39.7 mg/dL, P=0.085, effect size=0.38] and [45±11.3 vs 42.3±10.4 mg/dL, P=0.209, ES= 0.28], respectively. While Triglyceride and LDL showed significant improvements at [150.8±63.9 vs 120.4±43.5 mg/dL, P=0.005, effect size= 0.66], and [134.2±27.9 vs 119.6±37.6 mg/dL, P=0.04, effect size= 0.46], respectively (Table 1).
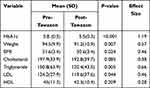 |
Table 1 Comparison of the Outcome Pre-Post Tawazon-DPP Intervention in the First Phase of the Pilot |
After completing 6 months of the program, a total of 8(34.8%) of the participants have changed their HbA1c from pre-diabetic to normal which was found to be a significant change with P=0.008 (Table 2).
 |
Table 2 McNemar Test Was Performed to Determine the Number of Participants Who Changed Their Pre-Diabetic State to Normal in Phase I of the Study |
Pilot (Phase II)
A total of 247 individuals were enrolled in the program that met the inclusion criteria; 171 (69%) participants completed the program. The height mean is 164.5±9.7 cm and the age mean is 45±9 years, however, the vast majority of participants are 40 years of age or older 121 (70.6%). Participants’ age groups were divided as younger than 40, between 40 and 49 years, and 50 years old or older, and that results are 50 (29.4%), 60 (35%), and 61 (35.6%) respectively (Table 3). Of those 84 (49.1%) were males and 87 (50.9%) were females and no significant differences were found in any baseline variable between males and females. The majority of the participants were from AB facility 52 (30.4%), followed by DHA 48 (28.1%), AH 47 (27.5%), and finally RT 24 (14.0%).
 |
Table 3 Baseline Demographic Characteristics of the Participants |
Pre-post changes from baseline to 9 months of the intensive lifestyle change program intervention in all participants are shown in (Table 4). The mean reduction in HbA1c was [6.0±0.4 vs 5.8±0.3 mmol/L, P<0.001], mean weight loss measured at [87.4±17.2 vs 82.3±17.5 kg, P<0.001], leading to a mean reduction in Body Mass Index (BMI) of [32.3±6.0 vs 30.5±6.2 kg/m2, P<0.001] (Table 5). Moreover, the lipid profile showed significant improvement as well at all levels. Total cholesterol showed a mean reduction of [190.3±40.1 vs 182.9±38 mg/dL, P<0.001], Triglyceride [128.7±58.7 vs 107.8±49.4 mg/dL, P<0.001], and LDL [129.0±37.9 vs 120.2±33.0 mg/dL, P=0.002], and finally significant increase in HDL [47.6±13.8 vs 48.5±12.5 mg/dL, P=0.006].
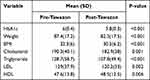 |
Table 4 Comparison of the Outcome Pre-Post Tawazon-DPP Intervention in the Second Phase of the Pilot |
 |
Table 5 McNemar Test Was Performed to Determine the Number of Participants Who Changed Their Pre-Diabetic State to Normal in Phase II of the Study |
After completing 9 months in the program, significant changes were found in the levels of HbA1c and BMI. A total of [41 (24.8%), P<0.001] have changed their HbA1c level from pre-diabetic to the normal level. Furthermore, 24 (14.1%) participants have reduced their BMI from Obese level to overweight and normal levels, 47 (27.7%) reduced their BMI from overweight to normal with P<0.001, and 2 (1.2%) have moved from normal BMI level to underweight.
Participant Satisfaction
A patient satisfaction survey was administered via SMS between the 1st and 31st of July 2020, in both English and Arabic languages. The survey was sent to all 171 participants who completed the program and only 20 (11.6%) responded and completed it. Both access to the program and the coaches received the highest satisfaction rates of 90.6% and 90.3%, respectively. Moreover, material, program structure, and program impact on lifestyle scored 82.2%, 82.5%, and 84.2%, respectively. Overall, the program received a rate of 86.1% satisfaction and 90.3% likelihood for recommending the program to others.
Discussion
In 2019, approximately 463 million adults were living with diabetes and associated with 4.2 million deaths and 20 million live births worldwide.16 Moreover, there are another 374 million people who are pre-diabetic or at-risk of developing T2D.16 These people are considered to be the at risk population due to several risk factors, such as unhealthy diet, weight increase, family history of diabetes, physical inactivity, aging, high blood pressure, ethnicity, impaired glucose tolerance (IGT), history of gestational diabetes, and malnutrition during pregnancy.17
It is evident that most of these risk factors are lifestyle behavioral and they are associated with the modern lifestyle which is generally characterized by long sedentary periods and physical inactivity.18 Since T1D is not preventable as the environmental triggers that are considered to destruct the body’s insulin-producing cells are still under investigation, lifestyle changes and community-based interventions mainly target people who are at risk for T2D to help them prevent the development of the condition and who are previously diagnosed with T2D to prevent its complications.18
Many evidence-based studies around the globe aim to prevent the development of T2D in those high-risk people. The most well-known studies with overwhelming evidence were conducted in the USA, Finland, India, China, and Japan.18 The Chinese study that was published in 1997 was probably the first to conduct a lifestyle intervention study with a 6 years follow-up duration.19 The study concluded that the interventional groups (diet arm, exercise arm, and diet-plus-exercise arm) showed significant reductions in the risk of developing diabetes with (31%) reduction of BMI, (46%) reduction of fasting glucose, and (42%) committing to a healthy diet.19
Following that, in 2002, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) in the USA funded the Diabetes Prevention Program in 25 centers nationwide.20 The NIDDK-DPP study was a landmark randomized clinical trial (RCT) that investigated how lifestyle changes can effectively delay or prevent diabetes in a high-risk overweight and obese population compared to the control group who were administered metformin (medication for T2D treatment).20 The goal of the study was to achieve (7%) weight loss and at least 150 minutes of physical activity per week.21 The mean age for the NIDDK-DPP participants was 50.6±10.7 years, 94.2±20.3 kg in weight, and 34.0±6.7 kg/m2 in their BMI, compared to 45±9 year, 94.5±9.9 kg, and 31.6±3.4 kg/m2 in Tawazon-DPP participants, respectively. Moreover, the goal of weight loss of 7% or more in the lifestyle change group in the NIDDK-DPP was achieved by (50%) of the participants at 24 weeks (6 months), while Tawazon showed a total of (41.8%) changes in BMI levels, thus weight loss in 9 months. This could be due to the COVID-19 Pandemic towards the end of the program as it was initially intended to be a full year (12 months) program but with all the safety measures and precautions taken in Saudi Arabia, curfews were put in place, all participants were housebound and their physical activities were very limited. However, (41.8%) was still a statistically and clinically significant improvement for Tawazon-DPP.
A year after, in 2003, the Finnish Diabetes Prevention Study (DPS) was published with 3-year result of a lifestyle intervention on diet and physical activity.22 Despite that the Finnish DPS is an RCT, only minor differences were found compared to Tawazon’s study population. The Finnish DPS targeted older adults (age 4–64 years) while Tawazon’s criteria included younger adults of 18 years and older (youngest participant was 25 years old) but similar BMI levels and all participants were pre-diabetic. The Finnish DPS was prematurely terminated as the lifestyle intervention group showed a statistically significantly low number of diabetes incidents compared to the control group. The program had a dietary intervention and exercise intervention with modules methods spread throughout the first year with individualized discussions and guidance to increase their overall level of physical activity.22
Another 4 arms RCT was conducted in India between 2001 and 2005 and published in 2006.23 The program’s duration was 30 months with mean age and HbA1c level for the Lifestyle intervention arm were very close to Tawazon’s participants with 46.1±5.7 years and 6.1±0.5 mmol/L, respectively. However, the BMI level was considerably less in the Indian Diabetes Prevention Program (INDPP) 25.7±3.3 km/m2.
Four years later, in 2010, Congress authorized the CDC to establish the National Diabetes Prevention Program (National DPP) based on the NIDDK-DPP RCT results. The CDC started building the infrastructure of the National DPP to move the program from research to implementation in communities across the USA.12 A final evidence report was published by The Institute for Clinical and Economic Review (ICER) in 2016 concluding that the National DPP provided an incremental or better net health benefit.12 Since then, the CDC’s National DPP has been adopted by many organizations internationally. Most of these organizations have received CDC’s approval and recognition as a partner in the program. The hospital has initiated the partnership with the CDC to be a recognized partner, however, currently, the process is pending until the situation with COVID-19 Pandemic clears out.
The goal of the National DPP is to achieve 5–7% weight loss of baseline body weight, hence, BMI and HbA1c levels. Such goals can be achieved by focusing on self-monitoring of diet and physical activity, having a solid self-efficacy and social support system for maintaining all the necessary lifestyle changes, and strategize the problem-solving methods to overcome challenges to sustaining weight loss.24 Tawazon-DPP emphasized these strategies and focused on giving the participants the support needed to continue their weight loss journey and sustain it. With such promising results of the pilot (phase I and Phase II) of Tawazon-DPP, the hospital has patented the name and intends to resume the program and initiate a full year of Tawazon-DPP within the Saudi Aramco community.
A review published in 2019 summarizes the available data available in the literature on the prevalence of T2D and prediabetes, ways to manage the disease, the risk factors for T2D, and complications associated with T2D in the Middle East, Africa, and Russia.25 The support from governments and healthcare authorities in these regions was limited with the deemed high cost of lifestyle change intensive programs. This leads to a lack of centralized resources to provide community-delivered lifestyle changes that are used in DPP interventions such as the 16-week curriculum that covers the basic knowledge on diet, exercise, and behavior modification, and the individualized sessions.25
Most recently, an RCT conducted in Saudi Arabia implementing an 18-months lifestyle changes intervention following the American Diabetes Association (ADA) criteria with similar age and BMI, in addition to the glucose levels 43.4±7.8, 31.3±6.4, and 6.1±0.4, respectively.26 The study also showed similar results to Tawazon-DPP’s outcomes with a significant reduction in body weight, BMI, and glucose/HbA1c.26 However, the published study team struggled with sustaining the interest of the individuals to implement the needed lifestyle changes. And despite this major limitation of poor compliance from the participants, the study added to the literature clinical value given the ethnic and cultural variations in response to DPPs.
With Tawazon proving its efficacy in achieving the desired weight loss and decreasing the HbA1c level to normalcy, a population-wide intervention is an option that is being considered. Moreover, the Tawazon-DPP can also be implemented across Saudi Arabia in the foreseeable future. The program has exhibited outstanding clinical outcomes, however, the cost-effectiveness of the program is yet to be investigated. Cost-effectiveness remains a concern as related data can be a limitation as Cost-related data does not reflect associated requisite activities such as gym memberships and diabetes risk-assessment process which can overwhelm the primary care physicians. Another limitation of this study was the low participants’ satisfaction response which can which can be due to limited communication during the beginning of the pandemic.
Conclusion
Diabetes Prevention Programs have been implemented to prevent or postpone the development of T2D for over 2 decades. However, most of the studies published are overwhelmingly from RCTs, where the setting of these interventions is controlled and the outcomes are probably expected. This paper provides real data from the actual care plan that was put in place to prospectively help our patients. Tawazon-DPP has achieved the desired goals even though it was terminated prematurely due to the COVID-19 pandemic. But that showed what a strong approach to life and patient care that the hospital can provide to its patients. Furthermore, this intensive lifestyle changing program has proven its significant potential and it could benefit the whole nation hoping to tackle T2D and its burden on the healthcare system.
Recommendations
- Maintenance sessions need to be delivered following the core sessions, as the CDC recommends these to foster sustainability of positive program outcomes such as weight loss and to collect further data.
- Online or electronic media-assisted versions of the program can be introduced to widen the choices and are effective in selected individuals comparable to levels achieved by health professionals.
- Programs based on coordinated public health and clinical approaches in healthcare, workplace, and community settings have a synergistic effect in maximizing gains in diabetes prevention.
Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki and has received our Institution Review Board’s approval number (20-05) in January 1st 2020. Informed consent form was waivered as data was collected retrospectively and anonymously from patients’ electronic medical records.
Acknowledgments
The authors would like to thank the Tawazon team for their dedication to the program from beginning to end. Ms. Ahlam Sarhan, Dr Ghassan Saleh, Dr Abdulwahed Khalefa, Abdulrahman Almishal, Hanouf Al Ghamdi, Shadia Ismail, Malakah Dawood, Manal Mahrouq, Maria Hammad, Rana Ibrahim, Zainab Sadah, Fatma Mohammed; Najat Al Achkar, Dr Daniele Rigamonti.
Funding
Tawazon is one of the institution's health promotion program and a budget is allocated for this program as part of the population health strategic plan.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Saeedi P, Petersohn I, Salpea P, et al.; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
2. Mushcab H, Kernohan WG, Wallace J, Martin S. Web-based remote monitoring systems for self-managing type 2 diabetes: a systematic review. Diabetes Technol Ther. 2015;17(7):498–509. doi:10.1089/dia.2014.0296
3. Mushcab H, Kernohan WG, Wallace J, Harper R, Martin S. Self-management of diabetes mellitus with remote monitoring: a retrospective review of 214 cases. Int J E-Health Med Commun. 2017;8(1):52–61.
4. Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Fard HH, Ghojazadeh M. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promot Perspect. 2020;10(2):98–115. doi:10.34172/hpp.2020.18
5. Naeem Z. Burden of diabetes mellitus in Saudi Arabia. Int J Health Sci. 2015;9(3):V–VI.
6. International Diabetes Federation. Middle East and North Africa. International Diabetes Federation; 2020. Available from: https://www.idf.org/our-network/regions-members/middle-east-and-north-africa/members/46-saudi-arabia.html.
7. Uusitupa M, Khan TA, Viguiliouk E, et al. Prevention of type 2 diabetes by lifestyle changes: a systematic review and meta-analysis. Nutrients. 2019;11(11):2611. doi:10.3390/nu11112611
8. Tello M. Healthy lifestyle can prevent diabetes (and even reverse it). Harvard Health Publishin - Harvard Medical School; 2018. Available from: https://www.health.harvard.edu/blog/healthy-lifestyle-can-prevent-diabetes-and-even-reverse-it-2018090514698.
9. Diabetes.co.uk. Type 2 diabetes-reversing type 2 diabetes. Diabetes.co.uk; 2019. Available from: https://www.diabetes.co.uk/reversing-diabetes.html.
10. BMJ. Losing weight can reverse type 2 diabetes, but is rarely achieved or recorded. BMJ; 2021. Available from: https://www.bmj.com/company/newsroom/losing-weight-can-reverse-type-2-diabetes-but-is-rarely-achieved-or-recorded/.
11. Centers for Disease Control and Prevention. Lifestyle change program details. CDC; 2020. Available from: https://www.cdc.gov/diabetes/prevention/lcp-details.html.
12. Centers for Disease Control and Prevention. Key National DPP milestones. Centers for Disease Control and Prevention; 2018. Available from: https://www.cdc.gov/diabetes/prevention/milestones.htm.
13. Tabak R, Sniclair K, Baumann A, et al. A review of diabetes prevention program translations: use of cultural adaptation and implementation research. Behav Med Pract Policy Res. 2015;5(4):401–414. doi:10.1007/s13142-015-0341-0
14. Centers for Disease Control and Prevention. About the National DPP. Centers for Disease Control and Prevention; 2018. Available from: https://www.cdc.gov/diabetes/prevention/about.htm.
15. Centers for Disease Control and Prevention. Centers for disease control and prevention diabetes prevention recognition program: standards and operating procedures. Centers for Disease Control and Prevention; 2018.
16. International Diabetes Federation. Diabetes facts & figures. International Diabetes Federation; 2020. Available from: https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html#:~:text=Approximately%20463%20million%20adults%20(20,low%2D%20and%20middle%2Dincome%20countries.
17. International Diabetes Federation. Type 2 diabetes. International Diabetes Federation; 2020. Available from: https://www.idf.org/aboutdiabetes/type-2-diabetes.html.
18. International Diabetes Federation. Diabetes prevention. International Diabetes Federation; 2019. Available from: https://www.idf.org/aboutdiabetes/prevention.html.
19. Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–544. doi:10.2337/diacare.20.4.537
20. Diabetes Prevention Program Outcomes Study. Welcome. Diabetes Prevention Program Outcomes Study. Available from: https://dppos.bsc.gwu.edu/.
21. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi:10.1056/NEJMoa012512
22. Lindström J, Louheranta A, Mannelin M, et al. The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003;26(12):3230–3236. doi:10.2337/diacare.26.12.3230
23. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V; IDPP. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–297. doi:10.1007/s00125-005-0097-z
24. DPP Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi:10.2337/diacare.25.12.2165
25. Khalil S, Abdelaziz S, Al Shammary A, et al. Prediabetes management in the Middle East, Africa and Russia: current status and call for action. Diab Vasc Dis Res. 2019;16(3):213–226. doi:10.1177/1479164118819665
26. Amer O, Sabico S, Alfawaz H, et al. Reversal of prediabetes in Saudi Adults: results from an 18 month lifestyle intervention. Nutrients. 2020;12:804. doi:10.3390/nu12030804
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
