Back to Journals » Journal of Inflammation Research » Volume 16
Systemic Inflammation Response Index as a Predictor of Stroke Risk in Elderly Patients with Hypertension: A Cohort Study
Authors Cai X , Song S , Hu J, Wang L, Shen D , Zhu Q, Yang W, Luo Q, Hong J, Li N
Received 23 August 2023
Accepted for publication 10 October 2023
Published 24 October 2023 Volume 2023:16 Pages 4821—4832
DOI https://doi.org/10.2147/JIR.S433190
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Xintian Cai,1,* Shuaiwei Song,1,* Junli Hu,2 Lei Wang,2 Di Shen,1 Qing Zhu,2 Wenbo Yang,2 Qin Luo,2 Jing Hong,2 Nanfang Li2
1Graduate School, Xinjiang Medical University, Urumqi, Xinjiang, People’s Republic of China; 2Hypertension Center of People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang Hypertension Institute, NHC Key Laboratory of Hypertension Clinical Research, Key Laboratory of Xinjiang Uygur Autonomous Region, Hypertension Research Laboratory, Xinjiang Clinical Medical Research Center for Hypertension (Cardio-Cerebrovascular) Diseases, Urumqi, Xinjiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Nanfang Li, Hypertension Center of People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang Hypertension Institute, NHC Key Laboratory of Hypertension Clinical Research, Key Laboratory of Xinjiang Uygur Autonomous Region, Hypertension Research Laboratory, Xinjiang Clinical Medical Research Center for Hypertension (Cardio-Cerebrovascular) Diseases, No. 91 Tianchi Road, Urumqi, Xinjiang, 830001, People’s Republic of China, Tel +86 8564818, Email [email protected]
Objective: This study aimed to evaluate the relationship between the systemic inflammation response index (SIRI) and the risk of stroke and its subtypes in elderly patients with hypertension and to explore its predictive accuracy and any potential effect modifiers.
Methods: The study included 4749 participants with no history of stroke at baseline. Cox regression was used to estimate adjusted hazard ratios (HR) and 95% confidence intervals (CIs). Interaction tests and subgroup analyses were conducted. The predictive performance of various inflammatory indicators for stroke was compared using the area under the curve (AUC), continuous net reclassification improvement (NRI), and integrated discrimination improvement (IDI).
Results: During a median follow-up period of 3.2 years, 640 strokes were recorded, of which 526 were ischemic and the remainder hemorrhagic. After adjustment for confounders, compared to the reference group, the HRs (95% CI) of stroke were 1.28 (95% CI, 1.01– 1.64) and 1.46 (95% CI, 1.14– 1.88) for participants in the second and third tertiles, respectively. We observed interactions between SIRI and homocysteine levels (< 15 vs. ≥ 15 μmol/L) (p for interaction = 0.014) on ischemic stroke risk. Furthermore, the AUC, NRI, and IDI analyses demonstrated that SIRI exhibited better predictive value for stroke risk when compared to other indicators. Similar results were observed for both ischemic and hemorrhagic strokes.
Conclusion: Elevated SIRI levels were significantly associated with the risk of stroke and its subtypes in elderly patients with hypertension, suggesting its potential as a promising indicator for stroke risk in this population. However, larger prospective studies are needed to confirm these findings.
Keywords: systemic inflammation response index, stroke, elderly, hypertension, inflammation, cohort study
Introduction
Stroke is one of the leading causes of death in China and the second leading cause of death globally.1–4 It exhibits significant morbidity, mortality, and disability, imposing a substantial burden on society and families.1,5 With a rapidly aging population, the incidence of hypertension has increased annually. Several large-scale epidemiological surveys in China have shown that about 23.2–27.8% of adults suffer from hypertension, and even more than 50% of people over 60 years of age are affected.6–9 Hypertension, especially in the elderly, is a high-risk factor for stroke.10 Therefore, identifying the residual risk of stroke and early risk stratification in elderly patients with hypertension is critical to the more effective formulation of risk reduction strategies.
Inflammation is associated with a poor clinical prognosis in patients with various diseases.11 In recent decades, accumulating evidence has confirmed that inflammation is an integral part of the development and maintenance of hypertension, the formation of atherosclerosis, and the rupture of arterial plaques, suggesting a key role in the emergence of cardiovascular diseases (CVD).12–14 Various markers reflecting inflammation include peripheral platelets, neutrophils, lymphocytes, and monocytes, as well as indicators of inflammation constructed based on these markers, such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR).15–17 Recently, two novel inflammatory indices, the systemic immune inflammation index (SII) and the systemic inflammation response index (SIRI), composed of platelets and three subtypes of white blood cells, have emerged as significant correlates of CVD.18–21 In particular, SIRI is regarded as a superior indicator of chronic inflammation and has a good prognostic predictive value for patients with acute strokes and tumors.22–24 However, little research has investigated the relationship between SIRI and stroke, especially in elderly hypertensive patients.
The aim of this study was to evaluate the relationship between SIRI and the risk of stroke and its subtypes in the elderly hypertensive population and to explore its predictive superiority and any potential effect modifiers.
Materials and Methods
Study Population
This study was a retrospective cohort study. Hypertensive patients with ≥2 visits registered at the Hypertension Center of Xinjiang Uygur Autonomous Region People’s Hospital from January 1, 2010, to December 31, 2021, were enrolled. Participants in the retrospective study were selected, as previously mentioned.25,26 There were a total of 8031 elderly hypertensive patients greater than or equal to 60 years of age. Exclusion criteria can be found in Figure S1. Ultimately, 4749 participants were included in the final analysis. The Ethics Board of the People’s Hospital of the Xinjiang Uygur Autonomous Region (KY2021031901) approved this retrospective study. Due to the retrospective design and the use of de-identified data, an exemption status for individual informed consent was provided. The Declaration of Helsinki guidelines were followed during the whole study. All data collected was kept strictly confidential and de-identified prior to analysis. Each patient’s data has an anonymous numeric code that prevents the patient from being identified in order to protect the patient’s privacy. The study adhered to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) when presenting its findings.
Data Collection and Definitions
Data for this study was obtained from the patient’s electronic medical records. Alcohol use and smoking status were categorized as binary variables: never/former or current. Standardized procedures were used to record blood pressure, height, and weight. The body mass index (BMI) was calculated in kilograms per square meter. All baseline blood samples were collected after an overnight fast. Fasting plasma glucose (FPG), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), high-density lipoprotein (HDL-C), homocysteine (Hcy), and uric acid (UA) were measured by the automatic biochemical analyzer. Hcy level ≥ 15 mmol/L was defined as hyperhomocysteinemia. The estimated glomerular filtration rate (eGFR) was calculated by the CKD-EPI equation. Routine blood tests, including white blood cell, neutrophil, monocyte, lymphocyte, and platelet counts, were determined by a full blood count analyzer. The following inflammatory indicators were calculated: LMR = lymphocyte count/monocyte count; PLR = platelet count/lymphocyte count; NLR = neutrophil count/lymphocyte count; SII = platelet count * neutrophil count/lymphocyte count; SIRI = neutrophil count * monocyte count/lymphocyte count. Medical history was identified by the ICD-10 codes. The medical history included coronary heart disease (CHD) (I24 and I25), atrial fibrillation (AF) (I48), diabetes (E10–E14), and dyslipidemia (E78). The Charlson comorbidity index (CCI) provided a summary of the overall burden of comorbidities. Table S1 lists the drugs involved in this study.
Outcomes and Follow-Up
The primary outcome was the first stroke, whether ischemic or hemorrhagic. The supplemental materials and methods describe methods for determining an incident stroke. Medical records, interviews, contacts with regional sickness and death registries, or access to the database of basic medical insurance were all used to establish the study’s outcomes. Patients were monitored from the time of enrollment until the end of the period, which was defined as the date of the final follow-up appointment, the date the first study outcome appeared, the date of death, or the conclusion of the investigation (December 31, 2021).
Statistical Analysis
The missForest procedure based on R was employed to impute the missing covariates.27 Continuous variables are presented as means ± standard deviation (SD) or medians (interquartile range) as appropriate, and categorical variables as proportions. Kaplan-Meier analysis was carried out with a log rank test. The proportional hazard assumption was verified using Schoenfeld residuals (Figure S2). Collinearity was assessed using variance inflation factors (Table S2). Cox proportional hazards models were utilized to calculate hazard ratios (HRs) and 95% confidence intervals (CI) for stroke events, with adjustment for age, sex, heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), smoking status, drinking status, uric acid (UA), eGFR, triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), fasting plasma glucose (FPG), homocysteine (Hcy), platelet count, hypertension duration, CHD, diabetes, dyslipidemia, AF, and the CCI. Restricted cubic splines were used to graphically assess the dose-response correlations between SIRI and stroke risk. We tested for interactions and performed subgroup analyses. To test the robustness of the findings, several additional sensitivity analyses were conducted. Prediction performance was measured by the receiver operating characteristics curve (ROC) and area under the ROC curve (AUC). A comparison of prediction performance was assessed using the reclassification method, expressed as continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI). Further details on the statistical analysis can be found in the supplemental materials and methods. R version 4.1.1 was used for all statistical analyses. The threshold for statistical significance (p = 0.05) was applied to all two-sided p values.
Results
Baseline Characteristics
As shown in the flow chart (Figure S1), a total of 4749 participants were included in the study. The study participants had an average age of 66.39 (SD, 4.67) years, and their average SIRI was 1.04 (SD, 0.50). Table 1 presents the baseline characteristics of the study participants categorized into SIRI tertiles. Participants with higher SIRI levels tended to have higher BMI, UA, DBP, TG, HLD-C, blood cell counts, and higher rates of diabetes compared with participants in the lowest tertile group. Similarly, they were more likely to receive antiplatelet, lipid-lowering, and glucose-lowering treatments. For SBP, TC, LDL-C, and Hcy, no discernible trend was observed.
 |
Table 1 Baseline Characteristics of Participants |
Association Between SIRI and Total Stroke and Its Subtypes
The mean duration of follow-up time was 3.67 years, with a median duration of 3.20 years. During this period, 640 strokes were identified, of which 526 were ischemic strokes (IS) and the remainder were hemorrhagic strokes (HS). The Kaplan–Meier curves showed the participants in the highest tertile of SIRI had a higher cumulative incidence of total stroke, IS, and HS compared to those in other groups over the follow-up period (Log rank test, all p < 0.05; Figure 1). Table 2 presents the relationships between SIRI and the risk of stroke and its subtypes. Overall, there were significant positive correlations between SIRI and the risk of total stroke (per SD increment; HR, 1.26, 95% CI: 1.15–1.38); IS (per SD increment; HR, 1.19, 95% CI: 1.07–1.32); and HS (per SD increment; HR, 1.51, 95% CI: 1.25–1.81) (Figure 2). After multivariable adjustment, compared to the reference group (the first tertile), the HRs of total stroke were 1.28 (95% CI, 1.01–1.64) in the second tertile and 1.46 (95% CI, 1.14–1.88) in the highest tertile. SIRI showed a positive and dose-dependent association with total stroke risk in Model 3 (p for trend = 0.003). The same patterns were observed for the risks of IS and HS.
 |
Table 2 Hazard Ratios (95% Confidence Intervals) of Incident Stroke According to the SIRI |
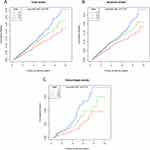 |
Figure 1 Kaplan-Meier survival curves for total stroke and individual outcomes based on SIRI tertiles. (A) Total stroke, (B) ischemic stroke, and (C) hemorrhagic stroke. |
 |
Figure 2 Dose-response association between SIRI and risk of stroke events. (A) Total stroke, (B) ischemic stroke, and (C) hemorrhagic stroke. |
Subgroup and Sensitivity Analysis
The results of subgroup analyses are shown in Figure 3. There was a significant interaction for patients with compared with patients without hyperhomocysteinemia (p for interaction = 0.014; Figure 3B) when looking at IS as an outcome. For total stroke and HS, there were no interactions for any of the subgroups (all p for interactions > 0.05; Figure 3A and C). In the sensitivity analyses, we excluded participants with less than 1 year of follow-up, and the results remained consistent (Table S3). Additionally, participants with AF at baseline were excluded, and the results still showed a strong correlation (Table S4). Furthermore, we adjusted for multiple drugs used based on Model 3, and the results remained consistent (Table S5). The analysis using competing-risks models yielded similar results (Table S6). We also excluded participants with missing values, and the results remained stable (Table S7). Ultimately, the E-value indicated that unmeasured confounding was unlikely to account for the results (Table S8).
 |
Figure 3 Subgroup analyses of the relationship between SIRI and risk of stroke events. (A) Total stroke, (B) ischemic stroke, and (C) hemorrhagic stroke. |
Comparative Analysis of Five Inflammatory Indicators in Predicting Stroke
ROC curve analysis was performed to determine the value of LMR, PLR, NLP, SII, and SIRI for predicting total stroke and its subtypes (Figure S3). Among all inflammatory parameters, the SIRI consistently exhibited the highest AUC value for total stroke and its subtypes. Furthermore, the cNRI and IDI for total stroke and its subtypes were significantly improved by the addition of SIRI to the basic model (Table S9). Nevertheless, adding other inflammatory parameters (LMR, PLR, NLR, and SII) did not significantly enhance the prediction.
Discussion
Currently, most studies investigating the relationship between inflammation and cerebrovascular disease primarily focus on the cellular level. These studies indicate that multiple cellular inflammatory factors are crucial to stroke occurrence and prognosis. However, our study aims to fill this research gap by investigating the association between inflammation, specifically SIRI, and the risk of total stroke and its subtypes in hypertensive elderly patients. We found that elevated levels of SIRI substantially increase the risk of stroke, even after adjusting for multiple confounders. The dose-response curve analysis further supports a significant positive correlation. Furthermore, in comparisons of various inflammatory indicators, we observed that SIRI consistently showed significant and stable results in assessing stroke risk.
Traditional indicators, such as LMR, PLR, and NLR, have been widely used to quantify the inflammatory state.28–33 In contrast, two novel indicators, SII and SIRI, integrate information from three immune pathways, including the sustained inflammatory response of monocytes and neutrophils as well as immune regulation by lymphocytes.34,35 These novel indicators offer a more comprehensive assessment of the inflammatory state.36 Previous studies have demonstrated the validity of SII and SIRI in assessing the level of inflammation and its association with metabolic disorders, CVD, cancer, and acute stroke prognosis, particularly SIRI.23,37–39
In this cohort study, we investigated the association between SIRI and stroke risk in elderly patients with hypertension. Our findings revealed that increasing SIRI levels were associated with an elevated risk of stroke. Consistent with our results, several previous studies have shown that chronic inflammation increases the risk of CVD and stroke.21,22,40–42 There is growing evidence linking inflammation to the pathogenesis of ischemic stroke and acute stage secondary brain injury.42–44 In a study of SIRI and SII dynamic status and the risk of CVD, subjects with a significantly higher risk of CVD were found to have higher levels of SIRI, and in particular, SIRI levels significantly increased the risk of stroke.21 Huang et al found that SIRI could predict the severity and functional outcome of stroke patients. The higher SIRI was correlated with a greater risk of stroke severity, and it may be a predictor of the early functional outcome of stroke.22 Additionally, SIRI has been identified as an independent risk factor for stroke prognosis and outcomes in patients with acute ischemic stroke.41
A substantial body of evidence indicates that inflammation plays a significant role in cerebrovascular disease and is a key mechanism contributing to the risk of stroke.45–47 To date, no randomized controlled trials have been completed on the use of anti-inflammatory drugs for stroke prevention.48 However, there have been a number of heart disease-related randomized controlled trials reported.49–54 Indirectly, these studies offer significant proof-of-concept data for the contribution of inflammation to stroke etiology and support the need for randomized controlled studies of anti-inflammatory medicines in the prevention of stroke. In conclusion, our findings may, in part, help with risk stratification and better clinical identification of elderly patients with hypertension who need primary prevention or personalized medicine approaches to management, such as anti-inflammatory therapy for high-risk patients who need to start primary prevention.
Meanwhile, subgroup analyses showed that the SIRI increased the risk of incident IS, especially in patients with hyperhomocysteinemia. The exact mechanisms linking inflammation, hyperhomocysteinemia, and IS remain to be determined. Several studies have shown a significant correlation between HCy levels and the severity of inflammation.55,56 A previous study suggested that inflammatory monocytes could be a potential target for treating inflammation and cardiovascular complications in hyperhomocysteinemia patients.57 Youssef et al hve also suggested the involvement of inflammation-related mechanisms in the association between Hcy and CVD risk.58 However, further investigations are needed to fully understand the underlying mechanisms.
Strong evidence exists that inflammatory processes in hypertension are dominated by innate and adaptive immune responses, and this relationship is particularly evident in elderly patients with hypertension.59,60 Through the excessive release of cytokines and chemokines, activated immune cells can infiltrate target tissues, resulting in the promotion of end-organ injuries.61,62 Furthermore, an increasing number of studies have demonstrated the relevance of inflammation in the pathogenesis of stroke. Firstly, inflammation of the cerebrovascular system triggers an oxidative stress response, leading to the occlusion of blood vessels. This triggers an immediate immune response in the ischemic brain, promoting the chemotaxis of inflammatory cells into brain tissue, resulting in brain tissue damage.63–65 Additionally, proinflammatory signals from immune mediators also promptly activate permanent cells and affect the infiltration of inflammatory cells into the ischemic zone, exacerbating the brain injury.66 Secondly, cerebral ischemia not only activates both innate immunity and adaptive immunity but also releases a large amount of indiscriminate humoral and cellular inflammation factors to damage brain cells and tissues, thus forming a vicious cycle.66,67 Thirdly, high inflammatory stimulation can lead to the activation of the complement system, causing a large number of active complement components produced in the blood vessels to enter the brain parenchyma and damage the brain tissue.68,69 Meanwhile, the activation of complement also promotes the phagocytosis of microglia on stressed neurons, leading to impairment of the corresponding nerve function.70,71 Finally, inflammation is also involved in all stages of atherosclerotic plaque, leading to thrombotic events.46,72,73
To our knowledge, this study represents the first exploration of the association between SIRI levels and the risk of stroke and its subtypes in elderly hypertensive patients. This study has several strengths worth noting. Firstly, it boasts a relatively large sample size and a prolonged follow-up duration. Secondly, the confidence interval for continuous NRI and IDI was generated through 1000 repeated samplings to minimize the impact of sampling error. Other advantages include multiple sensitivity analyses to confirm the robustness of the findings. Nevertheless, certain limitations should be acknowledged. Firstly, SIRI measurements were only obtained at baseline and did not account for dynamic changes during the follow-up period. Secondly, while multivariable adjustment and multiple sensitivity analyses were performed, unmeasured confounding remains. Thirdly, being an observational study, it can only report on associations but cannot attribute causality. Lastly, given that this study was conducted solely on a Chinese population, the external generalizability of the findings remains uncertain. Thus, further validation of these results in future studies is warranted.
Conclusion
Elevated SIRI levels were significantly associated with the risk of stroke and its subtypes in elderly patients with hypertension. Furthermore, SIRI may be a promising predictor of stroke risk in this population. Consequently, larger-scale, multicenter cohort studies are warranted to validate these initial findings.
Funding
Financial support was provided by the Major Science and Technology Special Projects in Xinjiang Uygur Autonomous Region (No. 2022A03012-1).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jing M, Bao L, Seet R. Estimated incidence and mortality of stroke in China. JAMA Netw Open. 2023;6(3):e231468. doi:10.1001/jamanetworkopen.2023.1468
2. Ding Q, Liu S, Yao Y, Liu H, Cai T, Han L. Global, regional, and national burden of ischemic stroke, 1990–2019. Neurology. 2022;98(3):e279–e290. doi:10.1212/WNL.0000000000013115
3. Tian DS, Liu CC, Wang CL, et al. Prevalence and risk factors of stroke in China: a national serial cross-sectional study from 2003 to 2018. Stroke Vasc Neurol. 2023;8(3):238–248. doi:10.1136/svn-2022-001598
4. Tu WJ, Zhao Z, Yin P, et al. Estimated burden of stroke in China in 2020. JAMA Netw Open. 2023;6(3):e231455. doi:10.1001/jamanetworkopen.2023.1455
5. Yao M, Ren Y, Jia Y, et al. Projected burden of stroke in China through 2050. Chin Med J. 2023;136(13):1598–1605. doi:10.1097/CM9.0000000000002060
6. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi:10.1161/CIRCULATIONAHA.117.032380
7. Li Y, Yang L, Wang L, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–523. doi:10.1016/j.ijcard.2016.10.110
8. Liu X, Gu W, Li Z, Lei H, Li G, Huang W. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: an update. J Hypertens. 2017;35(3):637–644. doi:10.1097/HJH.0000000000001203
9. China T, Hu SS. Report on cardiovascular health and diseases in China 2021: an updated summary. J Geriatr Cardiol. 2023;20(6):399–430. doi:10.26599/1671-5411.2023.06.001
10. Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313(13):1325–1335. doi:10.1001/jama.2015.2274
11. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133(11):1104–1114. doi:10.1161/CIRCULATIONAHA.115.020406
12. Ganjali S, Gotto AM, Ruscica M, et al. Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol. 2018;233(12):9237–9246. doi:10.1002/jcp.27028
13. Frostegård J. Immunity, atherosclerosis and cardiovascular disease. BMC Med. 2013;11(1):117. doi:10.1186/1741-7015-11-117
14. Dinh QN, Drummond GR, Sobey CG, Chrissobolis S. Roles of inflammation, oxidative stress, and vascular dysfunction in hypertension. Biomed Res Int. 2014;2014:406960. doi:10.1155/2014/406960
15. Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy. 2021;122(7):474–488. doi:10.4149/BLL_2021_078
16. Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med. 2019;39(4):345–357. doi:10.3343/alm.2019.39.4.345
17. Bg S, Gosavi S, Ananda Rao A, et al. Neutrophil-to-lymphocyte, lymphocyte-to-monocyte, and platelet-to-lymphocyte ratios: prognostic significance in COVID-19. Cureus. 2021;13(1):e12622. doi:10.7759/cureus.12622
18. Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
19. Xiao S, Wang Z, Zuo R, et al. Association of systemic immune inflammation index with all-cause, cardiovascular disease, and cancer-related mortality in patients with cardiovascular disease: a cross-sectional study. J Inflamm Res. 2023;16:941–961. doi:10.2147/JIR.S402227
20. Xia Y, Xia C, Wu L, Li Z, Li H, Zhang J. Systemic Immune Inflammation Index (SII), System Inflammation Response Index (SIRI) and risk of all-cause mortality and cardiovascular mortality: a 20-year follow-up cohort study of 42,875 US adults. J Clin Med. 2023;12(3):1128. doi:10.3390/jcm12031128
21. Li J, He D, Yu J, et al. Dynamic status of SII and SIRI alters the risk of cardiovascular diseases: evidence from kailuan cohort study. J Inflamm Res. 2022;15:5945–5957. doi:10.2147/JIR.S378309
22. Huang L. Increased systemic immune-inflammation index predicts disease severity and functional outcome in acute ischemic stroke patients. Neurologist. 2023;28(1):32–38. doi:10.1097/NRL.0000000000000464
23. Zhou Y, Zhang Y, Cui M, Zhang Y, Shang X. Prognostic value of the systemic inflammation response index in patients with acute ischemic stroke. Brain Behav. 2022;12(6):e2619. doi:10.1002/brb3.2619
24. Qi Q, Zhuang L, Shen Y, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 2016;122(14):2158–2167. doi:10.1002/cncr.30057
25. Cai X, Hu J, Wen W, et al. Association between the geriatric nutritional risk index and the risk of stroke in elderly patients with hypertension: a longitudinal and cohort study. Front Nutr. 2022;9:1048206. doi:10.3389/fnut.2022.1048206
26. Cai X, Hu J, Wang M, et al. Association between the sarcopenia index and the risk of stroke in elderly patients with hypertension: a cohort study. Aging. 2023;15(6):2005–2032. doi:10.18632/aging.204587
27. Stekhoven DJ, Bühlmann P. MissForest--non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–118. doi:10.1093/bioinformatics/btr597
28. Zhang YX, Shen ZY, Jia YC, et al. The Association of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and systemic inflammation response index with short-term functional outcome in patients with acute ischemic stroke. J Inflamm Res. 2023;16:3619–3630. doi:10.2147/JIR.S418106
29. Zhao Y, Xia J, He H, Liang S, Zhang H, Gan W. Diagnostic performance of novel inflammatory biomarkers based on ratios of laboratory indicators for nonalcoholic fatty liver disease. Front Endocrinol. 2022;13:981196. doi:10.3389/fendo.2022.981196
30. Bai YY, Xi Y, Yin BB, Zhang JH, Chen F, Zhu B. Reference intervals of systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and platelet-to-lymphocyte ratio during normal pregnancy in China. Eur Rev Med Pharmacol Sci. 2023;27(3):1033–1044. doi:10.26355/eurrev_202302_31199
31. Kosidło JW, Wolszczak-Biedrzycka B, Matowicka-Karna J, Dymicka-Piekarska V, Dorf J. Clinical significance and diagnostic utility of NLR, LMR, PLR and SII in the course of COVID-19: a literature review. J Inflamm Res. 2023;16:539–562. doi:10.2147/JIR.S395331
32. Li P, Li H, Ding S, Zhou J. NLR, PLR, LMR and MWR as diagnostic and prognostic markers for laryngeal carcinoma. Am J Transl Res. 2022;14(5):3017–3027.
33. Misiewicz A, Dymicka-Piekarska V. Fashionable, but what is their real clinical usefulness? NLR, LMR, and PLR as a promising indicator in colorectal cancer prognosis: a systematic review. J Inflamm Res. 2023;16:69–81. doi:10.2147/JIR.S391932
34. Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):298–306. doi:10.1038/nrc3245
35. Zhang M, Wang K, Zheng H, Zhao X, Xie S, Liu C. Monocyte lymphocyte ratio predicts the new-onset of chronic kidney disease: a cohort study. Clin Chim Acta. 2020;503:181–189. doi:10.1016/j.cca.2019.11.021
36. Jin Z, Wu Q, Chen S, et al. The Associations of Two Novel Inflammation Indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
37. Chu M, Luo Y, Wang D, et al. Systemic inflammation response index predicts 3-month outcome in patients with mild acute ischemic stroke receiving intravenous thrombolysis. Front Neurol. 2023;14:1095668. doi:10.3389/fneur.2023.1095668
38. Wang P, Guo X, Zhou Y, et al. Monocyte-to-high-density lipoprotein ratio and systemic inflammation response index are associated with the risk of metabolic disorders and cardiovascular diseases in general rural population. Front Endocrinol. 2022;13:944991. doi:10.3389/fendo.2022.944991
39. Chen JH, Zhai ET, Yuan YJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–6272. doi:10.3748/wjg.v23.i34.6261
40. Xiao S, Wang X, Zhang G, et al. Association of systemic immune inflammation index with estimated pulse wave velocity, atherogenic index of plasma, triglyceride-glucose index, and cardiovascular disease: a large cross-sectional study. Mediators Inflamm. 2023;2023:1966680. doi:10.1155/2023/1966680
41. Dang H, Mao W, Wang S, et al. Systemic inflammation response index as a prognostic predictor in patients with acute ischemic stroke: a propensity score matching analysis. Front Neurol. 2022;13:1049241. doi:10.3389/fneur.2022.1049241
42. Anrather J, Iadecola C. Inflammation and Stroke: an Overview. Neurotherapeutics. 2016;13(4):661–670. doi:10.1007/s13311-016-0483-x
43. Xia W, Han J, Huang G, Ying W. Inflammation in ischaemic brain injury: current advances and future perspectives. Clin Exp Pharmacol Physiol. 2010;37(2):253–258. doi:10.1111/j.1440-1681.2009.05279.x
44. Jin R, Liu L, Zhang S, Nanda A, Li G. Role of inflammation and its mediators in acute ischemic stroke. J Cardiovasc Transl Res. 2013;6(5):834–851. doi:10.1007/s12265-013-9508-6
45. McCabe JJ, Kelly PJ. Inflammation, cholesterol, and stroke risk: building evidence for a dual target strategy for secondary prevention. Stroke. 2021;52(9):2837–2838. doi:10.1161/STROKEAHA.121.035676
46. Kelly PJ, Lemmens R, Tsivgoulis G. Inflammation and stroke risk: a new target for prevention. Stroke. 2021;52(8):2697–2706. doi:10.1161/STROKEAHA.121.034388
47. Li J, Lin J, Pan Y, et al. Interleukin-6 and YKL-40 predicted recurrent stroke after ischemic stroke or TIA: analysis of 6 inflammation biomarkers in a prospective cohort study. J Neuroinflammation. 2022;19(1):131. doi:10.1186/s12974-022-02467-1
48. Coveney S, McCabe JJ, Murphy S, O’Donnell M, Kelly PJ. Anti-inflammatory therapy for preventing stroke and other vascular events after ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev. 2020;5(5):CD012825. doi:10.1002/14651858.CD012825.pub2
49. Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–1131. doi:10.1056/NEJMoa1707914
50. Ridker PM, Everett BM, Pradhan A, et al. Low-dose methotrexate for the prevention of atherosclerotic events. N Engl J Med. 2019;380(8):752–762. doi:10.1056/NEJMoa1809798
51. Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. 2013;61(4):404–410. doi:10.1016/j.jacc.2012.10.027
52. Tardif JC, Kouz S, Waters DD, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. 2019;381(26):2497–2505. doi:10.1056/NEJMoa1912388
53. Tong DC, Quinn S, Nasis A, et al. Colchicine in patients with acute coronary syndrome: the Australian COPS randomized clinical trial. Circulation. 2020;142(20):1890–1900. doi:10.1161/CIRCULATIONAHA.120.050771
54. Nidorf SM, Fiolet A, Mosterd A, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020;383(19):1838–1847. doi:10.1056/NEJMoa2021372
55. Pusceddu I, Herrmann W, Kleber ME, et al. Subclinical inflammation, telomere shortening, homocysteine, vitamin B6, and mortality: the Ludwigshafen Risk and Cardiovascular Health Study. Eur J Nutr. 2020;59(4):1399–1411. doi:10.1007/s00394-019-01993-8
56. Schroecksnadel K, Grammer TB, Boehm BO, März W, Fuchs D. Total homocysteine in patients with angiographic coronary artery disease correlates with inflammation markers. Thromb Haemost. 2010;103(05):926–935. doi:10.1160/TH09-07-0422
57. Fang P, Li X, Shan H, et al. Ly6C + inflammatory monocyte differentiation partially mediates hyperhomocysteinemia-induced vascular dysfunction in type 2 diabetic db/db mice. Arterioscler Thromb Vasc Biol. 2019;39(10):2097–2119. doi:10.1161/ATVBAHA.119.313138
58. Youssef MY, Mojiminiyi OA, Abdella NA. Plasma concentrations of C-reactive protein and total homocysteine in relation to the severity and risk factors for cerebrovascular disease. Transl Res. 2007;150(3):158–163. doi:10.1016/j.trsl.2007.02.006
59. McMaster WG, Kirabo A, Madhur MS, Harrison DG. Inflammation, immunity, and hypertensive end-organ damage. Circ Res. 2015;116(6):1022–1033. doi:10.1161/CIRCRESAHA.116.303697
60. Liu Q, Han L, Du Q, Zhang M, Zhou S, Shen X. The association between oxidative stress, activator protein-1, inflammatory, total antioxidant status and artery stiffness and the efficacy of olmesartan in elderly patients with mild-to-moderate essential hypertension. Clin Exp Hypertens. 2016;38(4):365–369. doi:10.3109/10641963.2015.1131285
61. Schiffrin EL. Immune mechanisms in hypertension and vascular injury. Clin Sci. 2014;126(4):267–274. doi:10.1042/CS20130407
62. Barrows IR, Ramezani A, Raj DS. Inflammation, immunity, and oxidative stress in hypertension-partners in crime. Adv Chronic Kidney Dis. 2019;26(2):122–130. doi:10.1053/j.ackd.2019.03.001
63. Tuttolomondo A. Ischemic stroke pathogenesis: genetics, epigenetics and inflammation. Curr Pharm Des. 2020;26(34):4207–4208. doi:10.2174/138161282634200831110542
64. Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron. 2010;67(2):181–198. doi:10.1016/j.neuron.2010.07.002
65. Gauberti M, De Lizarrondo SM, Vivien D. The “inflammatory penumbra” in ischemic stroke: from clinical data to experimental evidence. Eur Stroke J. 2016;1(1):20–27. doi:10.1177/2396987316630249
66. Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA. Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation. 2019;16(1):142. doi:10.1186/s12974-019-1516-2
67. Iadecola C, Buckwalter MS, Anrather J. Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest. 2020;130(6):2777–2788. doi:10.1172/JCI135530
68. Schäfer MK, Schwaeble WJ, Post C, et al. Complement C1q is dramatically up-regulated in brain microglia in response to transient global cerebral ischemia. J Immunol. 2000;164(10):5446–5452. doi:10.4049/jimmunol.164.10.5446
69. Mocco J, Mack WJ, Ducruet AF, et al. Complement component C3 mediates inflammatory injury following focal cerebral ischemia. Circ Res. 2006;99(2):209–217. doi:10.1161/01.RES.0000232544.90675.42
70. Kanazawa M, Ninomiya I, Hatakeyama M, Takahashi T, Shimohata T. Microglia and monocytes/macrophages polarization reveal novel therapeutic mechanism against stroke. Int J Mol Sci. 2017;18(10):2135. doi:10.3390/ijms18102135
71. Alawieh A, Langley EF, Tomlinson S. Targeted complement inhibition salvages stressed neurons and inhibits neuroinflammation after stroke in mice. Sci Transl Med. 2018;10(441):eaao6459. doi:10.1126/scitranslmed.aao6459
72. Soehnlein O, Libby P. Targeting inflammation in atherosclerosis - from experimental insights to the clinic. Nat Rev Drug Discov. 2021;20(8):589–610. doi:10.1038/s41573-021-00198-1
73. Bäck M, Yurdagul A, Tabas I, Öörni K, Kovanen PT. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nat Rev Cardiol. 2019;16(7):389–406. doi:10.1038/s41569-019-0169-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
