Back to Journals » Journal of Inflammation Research » Volume 15
Systemic Inflammation is Associated with Cardiometabolic Risk Factors and Clinical Outcomes
Authors Tejada B, Joehanes R, Hwang SJ, Huan T, Yao C, Ho JE, Levy D
Received 30 July 2022
Accepted for publication 18 November 2022
Published 29 December 2022 Volume 2022:15 Pages 6891—6903
DOI https://doi.org/10.2147/JIR.S382620
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Brandon Tejada,1,2 Roby Joehanes,1,2 Shih-Jen Hwang,1,2 Tianxiao Huan,1– 3 Chen Yao,1,2 Jennifer E Ho,4 Daniel Levy1,2,5
1Framingham Heart Study, Framingham, MA, USA; 2Population Sciences Branch, National Heart, Lung, and Blood Institute, Bethesda, MD, USA; 3Ophthalmology and Visual Sciences, University of Massachusetts Medical School, Worcester, MA, USA; 4CardioVascular Institute and Division of Cardiology, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, MA, Unites States; 5Boston University School of Medicine, Boston, MA, USA
Correspondence: Daniel Levy, Framingham Heart Study, 73 Mt. Wayte Avenue, Suite 2, Framingham, MA, 01702, USA, Email [email protected]
Purpose: Assessing an individual’s systemic inflammatory state is vital to understand inflammation’s role in cardiometabolic diseases and identify those at the greatest risk of disease. We generated global inflammation scores and investigated their associations with cardiometabolic risk factors and adverse outcomes.
Patients and Methods: Aggregate Inflammation Scores (AIS) and Principal Component Analysis (PCA) scores were generated for 7287 Framingham Heart Study participants using up to 26 inflammation-related proteins, with higher scores reflecting a pro-inflammatory milieu. Multivariable regression and proportional hazards analyses were conducted to investigate the associations of inflammation with cardiometabolic risk factors and outcomes. The primary outcomes for cross-sectional analyses included age, cigarette smoking, fasting lipid and glucose levels, blood pressure, body mass index (BMI), and hypertension, diabetes, and obesity. For prospective analyses, new-onset hypertension, diabetes, obesity, cardiovascular disease and all-cause mortality were investigated.
Results: Higher inflammation scores were associated with smoking and older age, higher BMI, systolic blood pressure, lipids, and glucose levels, and with greater odds of hypertension and diabetes after adjusting for age, sex, cohort, and BMI (all p < 0.001). Higher baseline scores were associated with greater odds of new-onset hypertension after adjusting for traditional risk factors (OR [95% CI] per one standard deviation [1-SD] increase, AIS: 1.33 [1.21– 1.47], PCA score: 1.26 [1.12– 1.42], p < 0.001). The AIS also was associated with new-onset diabetes (1.32 [1.14– 1.52], p < 0.001). Proportional hazards analyses revealed greater risk of new-onset cardiovascular disease events and all-cause mortality (HR [95% CI] per 1-SD, AIS: 1.25 [1.14– 1.37] and 1.32 [1.23– 1.42], PCA score: 1.22 [1.13– 1.33] and 1.40 [1.31– 1.49], p < 0.001).
Conclusion: Global inflammation scores encompassing an array of pro- and anti-inflammatory proteins and pathways may enhance risk assessment for cardiometabolic diseases. The AIS and PCA scores provide further opportunities to investigate the mechanisms of inflammation-related risk of disease.
Keywords: inflammation scores, cardiovascular disease, heart failure, pathways
Introduction
Inflammation pathways play a critical role in health and disease. Through acute inflammatory processes including vasoconstriction, leukocyte chemotaxis and extravasation, and the acute phase response, the innate immune system, and to some extent the adaptive immune system, protects the body against foreign pathogens, tissue damage, and oxidative stress. Excessive and protracted inflammation, however, can culminate in chronic inflammation that is a feature of atherosclerosis, a key contributor to cardiovascular disease (CVD).1–3 In addition to its role in CVD, chronic inflammation is a critical contributor to kidney,4–6 lung,7 and autoimmune diseases.8 It is thought that the association of inflammation with CVD is mediated in part by dysregulated inflammation. The ability to better assess the inflammatory milieu may thus aid in understanding an individual’s risk of CVD and other inflammation-linked diseases.
Previous studies have explored the adverse consequences of excessive inflammation and its relations to long-term health and predisposition to disease.9 Associations of protein biomarkers of systemic and acute inflammation with risk of myocardial infarction, type 2 diabetes, and chronic obstructive pulmonary disease have been reported in both cross-sectional and prospective studies.10–12 More recently, several studies have generated multi-marker inflammation scores to explore how systemic inflammation is linked to a variety of adverse clinical outcomes. Many of these studies relied on circulating levels of a small number of proteins, most notably pro-inflammatory C-reactive protein, to generate inflammation scores linked to adverse outcomes.13–15 Several recent studies have employed principal component analysis (PCA), a technique that reduces large datasets into smaller factors that capture patterns within a dataset.16,17 In a recent study, PCA was used to characterize inflammation in patients with heart failure with a preserved ejection fraction.17
The limitation of using single or a few biomarkers to characterize inflammation is that there is an abundance of inflammation-related proteins and inflammation is regulated by multiple pathways with redundancy and checks and balances. Moreover, the interplay between pro- and anti-inflammatory proteins adds to the complexity of inflammation. While many inflammatory scores focus solely on pro-inflammatory proteins, some inflammatory scores also consider anti-inflammatory proteins to counterbalance the directional effects of their pro-inflammatory counterparts.18 Most scores, however, are limited to a handful of inflammation-related proteins as proxies of the intricate innate and adaptive immune system responses. Thus, many scores may not capture the breadth of the complex inflammation network that can be used in analyses of inflammation-related diseases.
In this study, we leveraged multiple inflammation-related proteins measured as part of the Systems Approach to Biomarker Research (SABRe) in Cardiovascular Disease initiative19 to construct two inflammatory scores in over 7000 participants in the Framingham Heart Study (FHS). The first score, an aggregate inflammatory score (AIS), sums the levels of 24 inflammatory biomarkers after accounting for their pro- or anti-inflammatory properties. The second score uses a PCA approach to group inflammation-related biomarkers and constructs an inflammatory score. These inflammatory summary scores were then investigated for (1) their cross-sectional associations with cardiometabolic risk factors, (2) their prospective associations with new-onset hypertension, diabetes, and obesity, and (3) their relations to new-onset CVD and death during follow-up.
Methods
Study Sample
The FHS has recruited three generations of participants in whom it has conducted repeated examinations and obtained biosamples to generate multi-omics data resources. As part of the FHS SABRe CVD Initiative, 71 CVD-related circulating proteins were measured, spanning multiple biological processes, with selection of candidate proteins based on literature review, genome wide association studies, and proteomic and transcriptomic studies of CVD and its risk factors.19 The plasma proteins were measured in 3254 FHS Offspring cohort participants (exam 7; 1998–2001) and 4033 FHS Third Generation cohort participants (exam 1, 2002–2005).19,20 This study was approved by the Boston Medical Center Institutional Review Board, and written informed consent was obtained from all FHS participants in the study, adhering to the principles of the Declaration of Helsinki.
Protein Measurement
Blood plasma samples were obtained from FHS study participants and stored at −80°C. From these samples, the circulating levels of 85 proteins were measured: 14 proteins were identified as having high proportion of samples falling below the lower limits of detection and were excluded, leaving a total of 71 proteins for the current study. Protein measurements were carried out using a modified Enzyme-Linked Immunosorbent Assay (ELISA) sandwich protocol and multiplexed on a Luminex xMAP platform (Sigma-Aldrich, St. Louis, MO) as previously described.19 Briefly, singleton assays were developed to measure each protein biomarker before creating the multiplexed panel assays for compatible biomarker targets. For protein measurement calibration, a seven-point calibration curve was used in triplicate. Intra- and inter-assay coefficients of variation were determined using quality control samples: high and low spikes (Supplementary Table 1).
Separate high sensitivity C-reactive protein (hsCRP) plasma measurements were previously obtained using a Dade Behring CardioPhase hsCRP enzyme immunoassay. The assay consists of polystyrene particles with an antibody coating of monoclonal antibodies specific to C-reactive protein as detailed in prior studies.21 The protein levels were then quantified using nephelometry.
Internal Validation
The total study sample was split 50:50 by pedigree to produce discovery (n = 3645) and validation (n = 3642) sets that were relatively free of relatedness. These sets were utilized in a secondary analysis to investigate the internal replicability and robustness of the cross-sectional association results.
Data Processing
Protein measurements were scaled using a transformation based on the floor value in the protein dataset (1/10log10(floor)) to resolve the large differences in the magnitudes of observed plasma levels across all proteins. This transform guarantees the output to be between 0 and 10. Protein measurements were missing in a small number of participants (maximum number of missing values was observed for the protein leptin [n = 105; 7%]); missing protein values were imputed via the multivariate chain imputation (MICE) method.22 This scaled and imputed dataset was used to generate the PCA scores. In order to obtain a normally distributed protein dataset for the AIS, protein values in the scaled imputed dataset were then rank normalized (inverse normal transformation).
Identification and Characterization of Inflammatory Proteins
To identify inflammatory functions, the ontologies of the 71 SABRe proteins were classified using Gene Ontology (AmiGO 2, v. 2.5.13).23–25 The Gene Ontology annotations for each protein were investigated using the “gene and gene products” search (organism: Homo sapiens). A protein was considered inflammatory if it was identified as having the broad Gene Ontology annotation “inflammatory response” (GO:0006954). The categorization was further verified via the use of a second annotation tool, QIAGEN Ingenuity Pathway Analysis (QIAGEN Inc., https://www.qiagenbioinformatics.com/products/ingenuity-pathway-analysis), yielding 26 proteins with inflammation annotations (Supplementary Table 2). Data for all 26 inflammatory proteins were used to generate the PCA score.
The inflammatory proteins were categorized as pro-inflammatory or anti-inflammatory to develop an aggregate score that accounted for each protein’s inflammatory properties. This characterization utilized two steps. The first step entailed a literature review to identify which proteins were pro-inflammatory and anti-inflammatory based on consensus within the literature. This identified two hallmark pro-inflammatory proteins (C-reactive protein and monocyte chemotactic molecule 1) and two hallmark anti-inflammatory proteins (soluble receptor for advanced glycosylation endproducts and insulin-like growth factor 1). In the second step, the remaining proteins were categorized based on each protein’s correlations with the four literature defined pro-inflammatory and anti-inflammatory proteins. Using the scaled, unimputed dataset, a matrix of pairwise Pearson coefficients of correlation was produced for all 26 inflammatory proteins based on all available values in the study sample. The proteins were assessed for their correlations with the four literature defined pro-/anti-inflammatory proteins. A protein was defined pro- or anti-inflammatory if it had statistically significant (Bonferroni corrected threshold p < 0.05/(26*25/2) = 1.54 × 10−4) and directionally consistent correlations with at least two of the four flagship pro-inflammatory and anti-inflammatory markers. For example, a protein was defined as pro-inflammatory if it had positive correlations with both of the hallmark pro-inflammatory proteins or a negative correlation with a hallmark anti-inflammatory protein and a positive association with one of the hallmark pro-inflammatory proteins. Two proteins (clusterin and kallikrein) presented conflicting correlations and could not be categorized into either of the two categories (Supplementary Table 3). These two proteins were excluded from the AIS but were retained for the PCA approach.
Construction of Inflammatory Scores
To create the AIS, the directionality and levels of the 21 pro-inflammatory and three anti-inflammatory proteins were considered jointly and summed up as described below. In constructing the AIS score, rank normalized values for anti-inflammatory proteins were multiplied by −1, while observed values of pro-inflammatory proteins were retained. This approach allowed the summation of inflammatory properties: a net positive value was considered to reflect pro-inflammatory influences and a net negative value to reflect an anti-inflammatory milieu (Supplementary Table 4).
For the PCA inflammatory score, PCA was conducted on the scaled, imputed dataset. The individual loadings for each protein in the first principal component captured 89.7% of protein variance and were utilized in the PCA score (Supplementary Table 5). An individual’s score was calculated by summing the weighted protein measurements (loading factor * scaled protein measurement) for all 26 SABRe inflammatory proteins.
Statistical Analyses
The PCA and AIS scores were investigated for cross-sectional associations with cardiometabolic risk factors at baseline. In this analysis, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting lipids (triglycerides, total cholesterol, and HDL-cholesterol), fasting glucose, and body mass index (BMI; weight in kilograms divided by the square of height in meters) were individually tested for associations with the scores in linear regression models. Due to the effects of lipid-lowering, glucose-lowering, and blood pressure-lowering medications on the corresponding risk factors, lipid levels, blood pressure, and fasting glucose levels were imputed using a previously described technique to account for medication effects.26 In brief, fasting triglyceride and total cholesterol levels were raised by 20% and 33%, respectively, while HDL levels were lowered by 10% for individuals using lipid-lowering medications; systolic and diastolic blood pressures were raised by 15 and 10 mmHg, respectively, for participants using blood pressure lowering medications; fasting glucose was raised to the larger of a 10% increase or 126 mg/dL for individuals using diabetes medication. Each specific score was used as the predictor in the linear models. Separate sensitivity analyses were conducted in which participants using medications that are used for the risk factor of interest were excluded from the analyses. In a separate model, age, smoking status (current smoker [yes/no]), and sex were individually investigated as predictors in the regression model to determine their association with an individual’s inflammatory score, after adjusting for study cohort and the established inflammation covariates (age and sex) where relevant. Additionally, logistic regression was used to study the individual cross-sectional associations of the scores with prevalent diabetes (fasting glucose ≥126 mg/dL or use of diabetes medication), obesity (BMI ≥30 kg/m2), and hypertension status (SBP ≥130 or DBP ≥80 mmHg or use of antihypertensive medication).
Logistic regression was used in prospective analyses to investigate the associations of the inflammatory scores with new-onset hypertension, diabetes, and obesity between the baseline and follow-up examinations (mean interval = 6.36 years, standard deviation = 0.701). After excluding individuals who did not attend the follow-up exam, 6132 individuals were available for prospective analyses. Model 1 adjusted for age, sex, and cohort, while Model 2 additionally adjusted for the relevant cardiometabolic risk factor at baseline (SBP and DBP in new-onset hypertension analyses; fasting glucose in new-onset diabetes analyses; BMI in new-onset obesity analyses). Additional models further adjusted for baseline BMI or baseline hsCRP protein levels.
Cox regression models were used to investigate the association between the inflammatory scores and the prospective outcomes of new-onset CVD and all-cause mortality. The primary CVD outcome was a composite of new-onset coronary heart disease (including myocardial infarction, coronary insufficiency, and coronary revascularization procedures), heart failure, atherothrombotic stroke, and CVD death. Definitions of these outcomes are provided elsewhere. Of the 7287 participants with biomarker data, those without qualifying event data and relevant clinical covariates (age, sex, cohort, blood pressure, hypertension medication use, total cholesterol/HDL-cholesterol ratio, diabetes status, and smoking status) were excluded. Participants 50 years of age or younger were also excluded from CVD event and all-cause mortality analyses due to the rarity of such events among younger participants (n = 3799 individuals excluded based on all exclusion criteria). The final study sample for all-cause mortality analyses included 3488 participants. In the analysis of new-onset CVD, participants with a prior diagnosis of CVD were excluded (n = 387), leaving a study sample of 3101 participants. Cox regression models were adjusted for baseline age (10-year groupings), sex, cohort, smoking status, baseline systolic blood pressure and hypertension medication use, total cholesterol/HDL-cholesterol ratio, and diabetes status with each score investigated separately as a predictor. In secondary analyses, the associations of the scores with the individual components of the composite CVD outcome were assessed separately using the same covariate adjustments. The associations of hsCRP levels at baseline with new-onset CVD, all-cause mortality, and individual CVD endpoints were additionally investigated in secondary analyses.
Pathway-Specific Inflammatory Scores
To gain detailed insight into the associations of specific inflammation-related pathways with outcomes, pathway-specific AIS scores were generated. The Gene Set Enrichment Analysis (GSEA) webtool was used to identify the top ten canonical pathways that were significantly enriched (FDR < 0.05) in the set of 26 inflammatory proteins using all available canonical pathway gene sets: KEGG, Reactome, BioCarta, PID, and Wikipathways.27,28 The AIS method was then utilized to construct pathway-specific inflammatory scores. These pathway-specific AIS scores were then investigated for their associations in cross-sectional and prospective analyses as detailed above.
Results
Clinical Characteristics
The clinical characteristics of the study sample at baseline are presented in Table 1. In the combined cohort dataset, the average participant age was 49 years and 53% of the study population were women. The pairwise Pearson coefficients of correlation for the proteins are summarized in Supplementary Table 3. Approximately 71% of protein pairwise correlations were negligible or small (|r| ≤ 0.2) and only 3% of unique pairs had an absolute correlation greater than 0.4. The largest correlation was observed between pro-platelet basic protein (PPBP) and LDL receptor (r = 0.66).
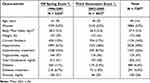 |
Table 1 Baseline Characteristics of the Study Sample |
Cross-Sectional Associations with Cardiometabolic Risk Factors
Aggregate Inflammatory Score
Regression analyses revealed that the AIS was higher with increasing age, higher in men than in women and higher in current smokers than in never or former smokers (p < 2.70 × 10−22; Table 2, (A); Supplementary Figure 1). Additionally, a higher AIS was associated with higher blood pressures (systolic and diastolic), BMI, and fasting glucose levels (all p < 2.40 × 10−55; Table 2 (B)). Additionally, a higher AIS was associated with higher fasting triglyceride and total cholesterol levels (all p < 3.59 × 10−18), and with lower HDL cholesterol (p = 1.30 × 10−171; Table 2 (B)). In secondary analyses (Model 2), associations of AIS with cardiometabolic risk factor associations remained statistically significant after additional adjustment for BMI (Table 2 (A and B), Model 2). A higher AIS was also found to associate with a greater odds of obesity (odds ratio [OR] per 1 standard deviation [1-SD] increment in the AIS, 2.70; [95% CI], 2.52–2.90), hypertension (OR 1.67; [95% CI] 1.57–1.76), and diabetes (OR 2.38; [95% CI] 2.13–2.66; Table 2 (C), Model 1). After adjusting for corresponding cardiometabolic risk factors (model 1 + risk factor adjustment), the association of AIS with hypertension remained significant (Table 2 (C), Model 1 + risk factor adjustments). Following the exclusion of participants using lipid-lowering, blood pressure-lowering, or glucose-lowering medication in sensitivity analyses, all associations with cardiometabolic risk factors remained significant, except for systolic blood pressure (Supplementary Table 6). When the overall sample was split by pedigrees into separate discovery and internal validation sets, all significant associations from the primary analyses of the overall dataset remained significant in both split datasets (Supplementary Table 7, replication defined as p < 3.33 × 10−3 = 0.05/15 traits), reflecting the robustness of the associations.
 |
Table 2 Aggregate Inflammatory Score: Cross-Sectional Associations with Cardiometabolic Risk Factors |
Principal Component Analysis Score
The PCA score also demonstrated statistically significant associations with older age, cigarette smoking, and cardiometabolic risk factors (all p < 2.42 × 10−7; Table 3, (A and B); Supplementary Figure 2). In Model 1, no significant associations were found between PCA scores and sex or total cholesterol (p > 1.25 × 10−1; Table 3, (A and B)). In secondary analyses (Model 2), all significant risk factor associations, except the association with diastolic blood pressure, remained statistically significant following additional adjustment for BMI (Table 3 (A and B), Model 2). At baseline, a 1-SD increase in the PCA score was also found to associate with a greater odds of obesity (OR per 1-SD increment in the PCA score, 1.70; [95% CI], 1.59–1.81), hypertension (OR 1.41; [95% CI] 1.32–1.50), and diabetes (OR 1.62; [95% CI] 1.48–1.78; Table 3 ©, Model 1). After adjusting for relevant cardiometabolic risk factors (Model 1 + risk factor adjustment), the PCA score remained significantly associated with hypertension (Table 3 (C), Model 1 + risk factor adjustment). In sensitivity analyses, after exclusion of participants using risk-factor lowering medications, the PCA score only remained significantly associated with triglycerides, total cholesterol, HDL levels, and systolic blood pressure (Supplementary Table 6). In the separate analysis of split samples by pedigree, all significant associations from the primary analyses of the overall dataset remained significant in both split datasets except for the association of diastolic blood pressure with the PCA score (Supplementary Table 8, replication defined as p < 3.33 × 10−3 = 0.05/15 traits).
 |
Table 3 Principal Component Analysis Score: Cross-Sectional Associations with Cardiometabolic Risk Factors |
Prospective Analyses
Aggregate Inflammatory Score
Multivariable adjusted analyses demonstrated positive associations between the baseline AIS and multiple prospective outcomes at the follow-up exam. A one SD increase in the AIS was significantly associated with 45% greater odds of hypertension, 78% greater odds of diabetes, and 60% greater odds of obesity ([95% CI] 1.32–1.60, 1.57–2.03, 1.43–1.79, respectively; Table 4 (A)) at follow-up in Model 1. After additionally adjusting for the relevant cardiometabolic risk factor for each outcome in Model 2 (baseline systolic and diastolic blood pressure and plasma glucose levels), the AIS was significant associated with 33% and 32% greater odds of hypertension and diabetes ([95% CI] 1.21–1.47 and 1.14–1.52; Table 4 (A), Model 1). After additional adjustment for baseline BMI, the association of the AIS with new-onset obesity was no longer significant. As measures of odds of occurrence, the results of these odds ratios should not be interpreted as definitive measures of risk.
 |
Table 4 Logistic Regression: Prospective Associations of PCA and AIS Scores with New-Onset Hypertension, Diabetes, and Obesity |
Principal Component Analysis Score
Similarly, a 1-SD increase in the PCA score was significantly associated with 31% greater odds of new-onset hypertension, 29% greater odds of new-onset diabetes, and 27% greater odds of new-onset diabetes at follow-up ([95% CI] 1.17–1.46, 1.12–1.47, 1.12–1.43, respectively; Table 4 (B), Model 1) after adjusting for baseline age, sex, cohort, and the time between the baseline and follow-up exams. After further adjustments for the relevant cardiometabolic risk factor at baseline for each outcome (Model 2), a one SD increase in the PCA score associated with a 26% greater odds of new-onset hypertension after additionally adjusting for baseline systolic and diastolic blood pressure ([95% CI] 1.12–1.42; Table 4 (B), Model 2). The associations of the PCA score with new onset diabetes and obesity were not statistically significant after additionally adjusting for baseline glucose and BMI, respectively.
In sensitivity analyses that additionally adjusted for baseline BMI (Model 3), 1-SD increases in either the AIS or PCA score remained significantly associated with greater odds of new-onset of hypertension (Supplementary Table 9). Additional adjustment of Model 2 with high-sensitivity C-reactive protein values at baseline to explore the informativeness of the inflammatory scores beyond the influence of an established inflammatory biomarker revealed that the AIS and PCA scores remained statistically significantly associated with new-onset hypertension at follow-up (Supplementary Figures 3–4 and Supplementary Tables 10–11). Neither of the inflammatory scores remained significantly associated with new-onset diabetes after adjusting for baseline high-sensitivity C-reactive protein level.
New-Onset CVD and All-Cause Mortality Analyses
During a mean follow-up of 15.2 ± 5.2 years, 627 new-onset CVD events occurred in 3101 eligible participants. During a mean follow-up of 15.9 ± 4.5 years, 1070 deaths occurred in 3488 eligible participants. In addition, there were 288 new-onset coronary heart disease events, 332 revascularization procedures, 319 new-onset heart failure events, 109 new-onset atherothrombotic stroke events, and 249 CVD-related deaths.
Both the AIS and the PCA inflammatory scores were associated with new-onset CVD and all-cause mortality. A one SD increase in the AIS was associated with a 25% greater risk of new onset CVD ([95% CI] 1.14–1.37; p = 1.21 × 10−6, Table 5) and a one SD increase in the PCA score was associated with a 22% greater risk of new onset CVD ([95% CI] 1.13–1.33; p = 8.81 × 10−7). In all-cause mortality analyses, a one SD increase in the AIS was associated with a 32% greater risk of death ([95% CI] 1.23–1.42; p = 1.20 × 10−14, Table 5), while a one SD increase in the PCA score was associated with a 40% greater risk of death ([95% CI] 1.31–1.49; p < 1.00 × 10−20). In separate secondary analyses for each inflammatory score, the AIS and PCA scores were significantly associated with greater odds of new-onset heart failure, revascularization procedures, and CVD death, but not with new-onset coronary heart disease (Table 5). Of note, a one SD increase in the PCA score was associated with a 52% greater risk of new-onset heart failure ([95% CI] 1.37–1.69; p = 2.30 × 10−15, Table 5) and the AIS was associated with a 54% greater risk ([95% CI] 1.36–1.74; p = 1.83 × 10−11, Table 5). Additionally, the PCA score was significantly associated with a greater risk of new-onset atherothrombotic stroke, but the AIS was not (Table 5).
 |
Table 5 Proportional Hazards Regression: Associations of AIS and PCA Scores with New-Onset All-Cause Mortality and Cardiovascular Disease |
Given the associations of CRP as a marker of inflammation and a risk factor for cardiovascular outcomes, a supplementary analysis was conducted to assess whether the inclusion of CRP in the inflammatory scores drove the associations with new-onset CVD and all-cause mortality. This analysis demonstrated that a one-standard deviation increase in CRP was significantly associated with greater risk of all-cause mortality, new-onset CVD, and each component of the CVD composite except atherothrombotic stroke (Supplementary Table 12). Comparatively, the AIS and PCA scores were associated with modestly greater risk for the primary outcomes of new-onset CVD and all-cause mortality (roughly 20% and 30–40% greater risk, respectively) than CRP does as a sole marker of inflammation (12% and 6% greater risk, respectively). Of note, both the AIS and PCA scores were associated with a roughly 50% greater risk of heart failure per-1-standard deviation increase, while a one-standard-deviation increase in CRP was associated with a 9% greater risk. Additionally, the multi-marker inflammatory scores were associated with 40–60% greater risk of CVD death, whereas CRP was associated with 9% greater risk. Thus, the associations of the AIS and PCA scores with all-cause mortality and-onset CVD, and notably with heart failure, depict greater inflammation associated risk.
Pathway Specific Inflammation Scores
To provide insight into the biological processes linked to inflammation, pathway-specific inflammation scores were generated to highlight the potential use of the AIS approach in investigations of the molecular mechanisms of inflammation linked to key outcomes. The inflammatory protein dataset was found to be enriched in pathways relating to the complement system; vitamin B12, selenium, and folate metabolism; the innate immune system; platelet activation, signaling, and aggregation; response to elevated platelet cytosolic calcium; platelet-mediated interactions with vascular and circulating cells; hemostasis; and Interleukin-1 and megakaryocytes involved in obesity (all FDR < 1 × 10−6). Of note, the complement system-specific AIS was more highly associated with lower HDL-cholesterol (p = 1.22 × 10−163, Supplementary Table 13) and cigarette smoking (p < 9.22 × 10−48, Supplementary Table 13) than was the overall AIS score. A 1-SD increase in the complement-specific AIS was also more highly associated with new-onset diabetes (OR 1.35; [95% CI] 1.17–1.55; Supplementary Table 13) than the overall AIS score. The proteins linked to the complement system AIS included adrenomedullin (ADM), apolipoprotein A-1 (APOA1), C-reactive protein (CRP), P-selectin (GMP140), and soluble intercellular adhesion molecule-1 (sICAM1), while plasma kallikrein (KLKB1), though involved in the complement system, was excluded from the score since it could not be clearly categorized as pro- or anti-inflammatory.
Discussion
By incorporating values of over 20 circulating inflammatory proteins, we generated two sets of scores that reflect multiple inflammatory pathways and better capture the global inflammatory milieu. Drawing from an approach that was developed to study heart failure with a preserved ejection fraction, the AIS utilizes an inductive approach by assigning pro- or anti-inflammatory status based on the pro- or anti-inflammatory properties of multiple proteins.17 We also utilized a deductive PCA approach that leverages inflammation-related proteins and identifies key patterns within the complex inflammatory dataset.9 In cross-sectional analyses, both the AIS and PCA scores were significantly associated with age, smoking status, and multiple cardiometabolic risk factors including lipid levels, blood pressure, body mass index, and fasting glucose levels, while the AIS was additionally associated with sex. In prospective analyses, both scores were also significantly associated with greater odds of new-onset hypertension after adjusting for baseline blood pressure, while the AIS was additionally associated with new-onset diabetes after adjusting for baseline fasting glucose. In proportional hazards analyses, both inflammatory scores were significantly associated with risk of new-onset CVD and all-cause mortality over an approximate 15-year follow-up period after adjusting for clinical covariates and relevant cardiometabolic risk factors. These prospective CVD analyses were driven in part by strong associations of the inflammatory scores with risk of heart failure. We hypothesize that inflammation summary techniques that combine the informativeness of multiple pro- and anti-inflammatory biomarkers better capture inflammation-induced risk and can identify biological pathways contributing to specific inflammation-related outcomes.
In previous studies, selected biomarkers have been used to study the association of inflammation with risks of various diseases. C-reactive protein has been extensively investigated in the context of inflammation and has been demonstrated to be associated with risk for CVD, chronic obstructive pulmonary disease, chronic kidney disease, and other acute and chronic inflammatory conditions.29–31 C-reactive protein is a component of both the AIS and PCA scores and was correlated with both scores (pairwise Spearman correlations 0.45 and 0.27, respectively; Supplementary Figures 3 and 4). Additionally, both sets of inflammatory scores were significantly associated with new-onset hypertension after additionally adjusting for high sensitivity C-reactive protein levels in Model 2. This suggests that the multi-marker inductive and deductive inflammatory scores we developed capture a greater degree of the inflammatory environment than single inflammatory markers such as C-reactive protein. As such, our inflammatory scores may prove useful for summarizing global systemic inflammation. Moreover, the application of this approach to inflammation-related pathways and their proteins may yield greater insight into the molecular mechanisms involved in inflammation-linked health outcomes.
The practicality and informativeness of these inflammatory scores lie in their potential to relate inflammatory pathways to disease risk via a diverse set of weakly-to-modestly correlated individual proteins. We found that our composite new-onset CVD outcome findings were largely driven by the associations of inflammation with risk for heart failure; a 1-SD increase in either of the inflammatory scores was associated with more than a 50% increase in risk of new-onset heart failure, greater than that predicted by CRP as a sole marker of inflammation. This finding may result from the heterogeneity of heart failure32 and the more comprehensive nature of the inflammatory scores. Numerous phenotypes of heart failure are detailed in the literature, each with differing factors such as left ventricular function, response to interventions and therapeutics, risk factors,33 and, most pertinently, proteomic signatures. Prior studies have demonstrated varying, and conflicting, inflammatory proteome characteristics among subtypes of heart failure: significant associations of CRP with heart failure with reduced ejection fraction (HFrEF), but not with and heart failure with preserved ejection fraction (HFpEF);34 inflammatory pathways (particularly involving GMP140/SELP) uniquely enriched in cases of heart failure with preserved and a mid-range ejection fraction (HFpEF and HFmrEF) and not in those with HFrEF;35 and significant associations of interleukin-6 and CRP with HFpEF but not with HFrEF or HFmrEF.36 While it is understood that inflammation plays a critical role in heart failure, the diversity of these proteomic findings suggests a complex relationship between inflammation and heart failure in which different phenotypes of the syndrome are shaped by specific inflammatory pathways. Therefore, single markers of inflammation, such as CRP, may not adequately capture these varying pathways as well as multi-marker inflammatory metrics, such as the AIS and PCA scores. As such, we note differences in the magnitudes of risk of heart failure observed between the multi-marker inflammatory scores (i.e., the AIS and PCA scores) and CRP as a solitary inflammatory marker. Future studies investigating differences in the inflammatory signatures of heart failure phenotypes are needed to identify the inflammatory mechanisms that are pertinent to disease progression and develop phenotype-specific therapeutics for heart failure.
This study has several strengths including a large sample size of approximately 7000 participants with available phenotype and proteomic data used to generate and investigate two sets of inflammatory scores. The availability of long-term and follow-up clinical data further added to the strengths of this study by allowing for both cross-sectional and prospective analyses. In cross-sectional analyses, the associations of these scores with risk factors were investigated in separate discovery and replication sets, demonstrating the robustness of our findings. The analyses of new-onset CVD and all-cause mortality were strengthened by the sizeable number of these events in the FHS.
Several limitations of this study are also noteworthy. Although a set of 26 inflammatory proteins was used to summarize inflammation, this set only partially represents the entirety of the inflammation proteome. The score generation methods employed in the current study can be applied in future investigations using larger proteomic datasets. Additionally, the study population consists largely of participants of European ancestry, limiting the generalizability of the current findings. Therefore, similar investigations in more racially and ethnically diverse cohorts are needed. Although separate discovery and replication sets were investigated in cross-sectional analyses, there was no independent external replication of the results. While these limitations may limit the clinical utility of these scores, the inflammatory scores may be of greater use in future investigations to aid in unveiling the inflammatory mechanisms that predispose one to greater risk of disease.
In this study, we demonstrated methodologies to generate two distinct systemic inflammation scores based on 24–26 inflammatory proteins from various inflammatory pathways. After adjusting for numerous clinical traits, the multi-marker AIS and PCA inflammatory scores were associated with an array of cardiometabolic traits, all-cause mortality, and new-onset CVD, particularly driven by strong associations with heart failure. Sensitivity analyses adjusting for CRP or comparing the strength of associations with those of CRP highlight the importance of diverse, multi-marker metrics of systemic inflammation in analyses of inflammatory mechanisms of disease. Future studies with larger cohorts and more comprehensive inflammatory biomarker datasets may allow for detailed profiles of inflammatory pathologies and elucidate the unique inflammatory mechanisms that differentiate phenotypes of heterogeneous conditions such as heart failure.
Funding
The Framingham Heart Study laboratory work for this project was funded by National Institutes of Health (NIH; contract N01-HC-25195). The analytical component of this project was funded by the Division of Intramural Research, National Heart, Lung, and Blood Institute (NHLBI), NIH (D. Levy, principal investigator). The views and opinions expressed in this report are those of the authors and do not necessarily represent the views of the NHLBI, the NIH, or the US Department of Health and Human Services.
Disclosure
Potential conflict of interest: The co-author C. Yao aided in the completion of this project, while an employee of the National Heart, Lung, and Blood Institute; Dr Yao is currently an employee of Bristol Myers Squibb. Jennifer E Ho reports grants from NIH, grants from Bayer, AG, outside the submitted work. The authors declare that they have no other conflicts of interest.
References
1. Frostegard J. Immunity, atherosclerosis and cardiovascular disease. BMC Med. 2013;11(117). doi:10.1186/1741-7015-11-117
2. Ruparelia N, Chai JT, Fisher EA, Choudhury RP. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat Rev Cardiol. 2017;14. doi:10.1038/nrcardio.2016.185
3. Li J, Lee DH, Hu J, et al. Dietary inflammatory potential and risk of cardiovascular disease among men and women in the U.S. J Am Coll Cardiol. 2020;76:2181–2193. doi:10.1016/j.jacc.2020.09.535
4. Stenvinkel P, Chertow GM, Devarajan P, et al. Chronic inflammation in chronic kidney disease progression: role of Nrf2. Kidney Int Rep. 2021;6:1775–1787. doi:10.1016/j.ekir.2021.04.023
5. Huang Y, Zeng M, Zhang L, et al. Dietary inflammatory potential is associated with sarcopenia among chronic kidney disease population. Front Nutr. 2022;9(856726). doi:10.3389/fnut.2022.856726
6. Martini S, Nair V, Keller BJ, et al. Integrative biology identifies shared transcriptional networks in CKD. J Am Soc Nephrol. 2014;25:2559–2572. doi:10.1681/ASN.2013080906
7. Zhang J, Xu Q, Sun W, et al. New insights into the role of NLRP3 inflammasome in pathogenesis and treatment of chronic obstructive pulmonary disease. J Inflamm Res. 2021;14:4155–4168. doi:10.2147/JIR.S324323
8. Lubberts E, van den Berg WB. Cytokines in the pathogenesis of rheumatoid arthritis and collagen-induced arthritis. Adv Exp Med Biol. 2003;520:194–202. doi:10.1007/978-1-4615-0171-8_11
9. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, sii and siri with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 Individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
10. Arroyo-Espliguero R, Avanzas P, Quiles J, Kaski JC. Predictive value of coronary artery stenoses and C-reactive protein levels in patients with stable coronary artery disease. Atherosclerosis. 2009;204:239–243. doi:10.1016/j.atherosclerosis.2008.08.009
11. Su B, Liu T, Chen F, et al. Inflammatory markers and the risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. PLoS One. 2016;11(e0150586). doi:10.1371/journal.pone.0150586
12. Wang X, Bao W, Liu J, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013;36:166–175. doi:10.2337/dc12-0702
13. Nozoe T, Matono R, Ijichi H, Ohga T, Ezaki T. Glasgow Prognostic Score (GPS) can be a useful indicator to determine prognosis of patients with colorectal carcinoma. Int Surg. 2014;99:512–517. doi:10.9738/INTSURG-D-13-00118.1
14. Bonaccio M, Di Castelnuovo A, Pounis G, et al. A score of low-grade inflammation and risk of mortality: prospective findings from the Moli-sani study. Haematologica. 2016;101:1434–1441. doi:10.3324/haematol.2016.144055
15. Conen D, Ridker PM, Everett BM, et al. A multimarker approach to assess the influence of inflammation on the incidence of atrial fibrillation in women. Eur Heart J. 2010;31:1730–1736. doi:10.1093/eurheartj/ehq146
16. Crouch SH, Botha-Le Roux S, Delles C, Graham LA, Schutte AE. Inflammation and hypertension development: a longitudinal analysis of the African-PREDICT study. Int J Cardiol Hypertens. 2020;7:100067. doi:10.1016/j.ijchy.2020.100067
17. Sanders-van Wijk S, Tromp J, Beussink-Nelson L, et al. Proteomic evaluation of the comorbidity-inflammation paradigm in heart failure with preserved ejection fraction: results from the PROMIS-HFpEF Study. Circulation. 2020;142:2029–2044. doi:10.1161/CIRCULATIONAHA.120.045810
18. Faria AP, Ritter AMV, Gasparetti CS, et al. A proposed inflammatory score of circulating cytokines/adipokines associated with resistant hypertension, but dependent on obesity parameters. Arq Bras Cardiol. 2019;112. doi:10.5935/abc.20190032
19. Ho JE, Lyass A, Courchesne P, et al. Protein biomarkers of cardiovascular disease and mortality in the community. J Am Heart Assoc. 2018;7. doi:10.1161/JAHA.117.008108
20. Yao C, Chen G, Song C, et al. Genome-wide mapping of plasma protein QTLs identifies putatively causal genes and pathways for cardiovascular disease. Nat Commun. 2018;9(3268). doi:10.1038/s41467-018-05512-x
21. Rost NS, Wolf PA, Kase CS, et al. Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke. 2001;32:2575–2579. doi:10.1161/hs1101.098151
22. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–49. doi:10.1002/mpr.329
23. Ashburner M, Ball CA, Blake JA, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25:25–29. doi:10.1038/75556
24. Carbon S, Ireland A, Mungall CJ, et al. AmiGO: online access to ontology and annotation data. Bioinformatics. 2009;25:288–289. doi:10.1093/bioinformatics/btn615
25. Gene Ontology C, Douglass E, Good BM. The Gene Ontology resource: enriching a GOld mine. Nucleic Acids Res. 2021;49:D325–D334. doi:10.1093/nar/gkaa1113
26. Yin X, Subramanian S, Willinger CM, et al. Metabolite signatures of metabolic risk factors and their longitudinal changes. J Clin Endocrinol Metab. 2016;101:1779–1789. doi:10.1210/jc.2015-2555
27. Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci U S A. 2005;102:15545–15550. doi:10.1073/pnas.0506580102
28. Mootha VK, Lindgren CM, Eriksson K-F, et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet. 2003;34:267–273. doi:10.1038/ng1180
29. Olafsdottir IS, Gíslason T, Thjódleifsson B, et al. Gender differences in the association between C-reactive protein, lung function impairment, and COPD. Int J Chron Obstruct Pulmon Dis. 2007;2:635–642.
30. Danesh J, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350:1387–1397. doi:10.1056/NEJMoa032804
31. Yeo ES, Hwang J-Y, Park JE, et al. Tumor necrosis factor (TNF-alpha) and C-reactive protein (CRP) are positively associated with the risk of chronic kidney disease in patients with type 2 diabetes. Yonsei Med J. 2010;51:519. doi:10.3349/ymj.2010.51.4.519
32. Ahmad T, Pencina MJ, Schulte PJ, et al. Clinical implications of chronic heart failure phenotypes defined by cluster analysis. J Am Coll Cardiol. 2014;64:1765–1774. doi:10.1016/j.jacc.2014.07.979
33. Ho JE, Lyass A, Lee DS, et al. Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circ Heart Fail. 2013;6:279–286. doi:10.1161/CIRCHEARTFAILURE.112.972828
34. de Boer RA, Nayor M, deFilippi CR, et al. Association of cardiovascular biomarkers with incident heart failure with preserved and reduced ejection fraction. JAMA Cardiol. 2018;3:215. doi:10.1001/jamacardio.2017.4987
35. Tromp J, Westenbrink BD, Ouwerkerk W, et al. Identifying pathophysiological mechanisms in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2018;72:1081–1090. doi:10.1016/j.jacc.2018.06.050
36. Albar Z, Albakri M, Hajjari J, et al. Inflammatory markers and risk of heart failure with reduced to preserved ejection fraction. Am J Cardiol. 2022;167:68–75. doi:10.1016/j.amjcard.2021.11.045
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
