Back to Journals » Cancer Management and Research » Volume 11
Systemic immune-inflammation index and ultrasonographic classification of breast imaging-reporting and data system predict outcomes of triple-negative breast cancer
Authors Wang P , Yue W, Li W, Luo Y, Li Z, Shao Y , He Z
Received 30 August 2018
Accepted for publication 13 November 2018
Published 17 January 2019 Volume 2019:11 Pages 813—819
DOI https://doi.org/10.2147/CMAR.S185890
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kenan Onel
Ping Wang,1 Wensheng Yue,1 Wenyan Li,1 Yuqun Luo,1 Zukun Li,1 Yi Shao,2 Zhizhong He3
1Department of Ultrasound, The Affiliated Hospital of North Sichuan Medical College, Nanchong, Sichuan 637000, China; 2Department of Ophthalmology, The First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi 330006, China; 3Department of Ultrasound, Dongguan People’s Hospital, Dongguan, Guangdong 523000, China
Introduction: This research was conducted to explore the relationship between the systemic immune-inflammation index (SII) and breast imaging-reporting and data system (BI-RADS) classification using ultrasonography and the survival of patients with triple-negative breast cancer (TNBC) in a cohort of Chinese.
Methods: A total of 215 TNBC patients treated at our hospital between November 2008 and March 2016 were enrolled in this study. We used the log-rank test and Kaplan–Meier curves to assess the overall survival (OS) and disease-free survival (DFS) differences between groups. The prognostic role of SII and other clinicopathological characteristics in TNBC patients were identified using the Cox regression model.
Results: Patients with low and high SII had median OS of 60.9 and 40.3 months, respectively, (HR=3.78, 95% CI: 2.16–4.15, P<0.001); while the median DFS was 22.4 months and 14.4 months for TNBC patients with low and high SII, respectively (HR =3.16, 95% CI: 1.82–4.02, P<0.001). For patients with grade 5 ultrasonographic BI-RADS classification, the median DFS and OS were 41.2 and 16.5 months, respectively, whereas, it was 57.7 and 21.3 months, respectively, for those with BI-RADS grades 3–4 (P<0.01). According to multivariable analyses, increased SII was a risk factor that independently predicted poor OS (HR =2.96, 95% CI: 2.18–3.98, P<0.001) and DFS (HR = 2.85, 95% CI: 1.62–3.81, P=0.005). In addition, tumor stage, BI-RADS, and histological grade also independently predicted poor OS (P=0.002, <0.001, 0.004).
Conclusion: Pretreatment SII and BI-RADS 5 were independent indicators for prognosis in TNBC patients. It is imperative to conduct prospective studies to evaluate the potential role of SII in patient selection, treatment guidance, and design of clinical trials.
Keywords: TNBC, SII, inflammation, prognosis, immunity
Introduction
Currently, breast cancer is the most common cancer in women, with a yearly increasing incidence in China.1 Although the mortality rates of breast cancer have decreased in recent years due to advances in tumor therapy, the disease is still one of the most common causes of cancer mortality among women.2 The prognosis of breast cancer is affected by several factors, including molecular, biological characteristics (such as human epidermal growth factor receptor 2 [HER2], hormonal receptors, and molecular subtypes) and clinicopathological parameters (such as the age of patient, lymph node status, tumor size, etc).3–5
Triple-negative breast cancer (TNBC) accounts for ~10%–20% of any newly diagnosed breast cancer. It is defined as the negative expression of HER2 and hormonal receptors.6 Progression and relapse are commonly observed in TNBC women. The peak of recurrence takes place within the first 3–5 years after diagnosis.7 TNBC has a characteristic of an intrinsic, aggressive tumor pathology, including histological grade, high levels of proliferation, frequency of TP53 mutations, and mitotic index, which lead to large tumor sizes, as well as poor clinical outcomes.8,9 Therefore, it is particularly important to explore factors for the prognosis of TNBC in patients.
In recent years, many researchers have paid attention to inflammation and found that cancer-related inflammation played an essential role in cancer development and prognosis.10–13 Systemic immune-inflammation index (SII) is an indicator that is based on peripheral neutrophil, lymphocyte, and platelet counts, and defined as (platelet × neutrophil)/lymphocyte, a potential indicator capable of establishing balance between inflammatory and immune status in the host.14 SII has been investigated in various cancers, including nasopharyngeal carcinoma, prostate cancer, colorectal cancer, pancreatic cancer, gastric cancer, and hepatocellular carcinoma.14–21 However, the role of SII in breast cancer patients has not been well understood. Therefore, this research was focused on exploring the clinical significance of SII in TNBC patients.
Materials and methods
Patient enrollment
The present study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of The Affiliated Hospital of North Sichuan Medical College. Written forms of informed consent were not required for individual patients because the study was retrospective, and all the data in the analysis were anonymous.
A total of 215 patients diagnosed with TNBC from November 2008 to March 2016 at our hospital were retrospectively included. We enrolled patients with histological confirmation of TNBC and they underwent surgery with neoadjuvant chemotherapy and adjuvant chemotherapy. We excluded patients with inflammatory diseases, immune diseases, coronary artery diseases, and hematological diseases; suffering from an infectious disease within 2 weeks of enrollment; using anti-inflammatory or immunosuppressive drugs prior to enrollment; with metastatic or inflammatory breast cancer. Data for differential blood counts were collected prior to anticancer treatment.
Collection of clinicopathological parameters
Negative estrogen receptor and progesterone receptor were defined as 1% of invasive tumor nuclei observed in the immunohistochemistry test. Negative HER2 status implies that the immunohistochemistry result was 0; positive HER2 means that the result was 3+ or positivity for 1+ and 2+ patients was confirmed by fluorescence in situ hybridization. All patients underwent radical mastectomy or breast-conserving surgery. The treatment methods for patients included chemotherapy (neoadjuvant and adjuvant chemotherapy), adjuvant radiotherapy, and surgery (mastectomy or breast-conserving surgery). Chemotherapy strategies included anthracyclines + cyclophosphamide + paclitaxel (AC-T) for 163 (76%) patients and docetaxel + carboplatin (TP) for 52 (24%) patients. Data for platelet count, neutrophil count, and lymphocyte count, as well as age, tumor size, breast imaging-reporting and data system (BI-RADS), lymph node metastasis, lympho-vascular invasion, histological grade, and antitumor treatment were collected. The SII was defined by the formula: (neutrophil × platelet)/lymphocyte.
Follow-up
Patient follow-up was regularly conducted; every three months within the first 2 years after surgery, and then every 6 months from that point until death or lost follow-up from the study. Ultrasound imaging, positron emission computed tomography, magnetic resonance imaging, and computed tomography were used to assess disease status. The contents of follow-up included the extent of disease progression, loss of follow-up, and death. The deadline for follow-up was December 2017. Disease-free survival (DFS) time refers to the period from surgery to the first recurrence of disease, while overall survival (OS) was defined as the period from pathological diagnosis to death.
Statistical analyses
The Kaplan–Meier analysis was applied to evaluate the DFS and OS. Comparison of the differences in survival between patients from the two groups was performed using the log-rank test. We used the Cox regression model for multivariable analysis to clarify independent factors for prognosticating TNBC in patients with breast cancer. Patients were divided into high or low SII groups according to the median index value. Chi-squared tests and Fisher’s exact tests were used to evaluate the correlation between clinicopathological parameters and SII. P<0.05 was considered statistically significant. The SPSS 21.0 software (IBM Corporation, Armonk, NY, USA ) was used for data analysis.
Results
Patient information
Table 1 summarizes the characteristics of the 215 TNBC patients at baseline in this study. One hundred eighty-one patients underwent radical mastectomy, while 34 patients received breast-conserving surgery. One hundred sixty-eight patients had ductal carcinoma, while 47 patients had lobular carcinoma. There were 138 and 77 patients with histopathological grades I, II, and III, respectively. Based on the American Joint Committee on Cancer staging system, 30, 114, and 71 patients were at stages I, II, and III of the disease, respectively. The median (range) value of SII was 624 (138–1,682), which was used to divide high and low SII. One hundred twenty-five and 90 patients were identified as BI-RADS 5 (high BI-RADS) and BI-RADS 3–4 (low BI-RADS), respectively. The median time for follow-up was 49.2 months (4–105 months). At the end of follow-up, 71 (33%) patients were still alive, 5 (2%) patients lost follow-up, and 139 (65%) patients had died. One hundred seventy-one patients had recurrent or metastatic cancer, of whom 136 died. Three patients died without any recurrence or metastasis.
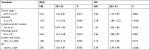
  | Table 1 Baseline characteristics of 215 TNBC patients Abbreviations: AJCC, American Joint Committee on Cancer; TNBC, triple-negative breast cancer. |
Relationship between clinicopathological parameters and SII
The association between SII and clinicopathological parameters is shown in Table 2. Histologic grade, lymph node status, and tumor stage positively correlated with SII (P<0.001, P=0.002, P=0.004, respectively). We did not find a statistically significant correlation between other clinicopathological parameters and SII in our study (P>0.05, Table 2).
  | Table 2 Association between SII and clinicopathological parameters Abbreviations: AJCC, American Joint Committee on Cancer; SII, systemic immune-inflammation index. |
Kaplan–Meier and univariable analysis
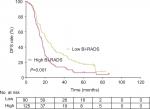
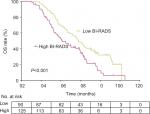
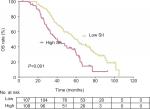
The median DFS for patients with TNBC who had low and high SII was 22.4 months and 14.4 months, respectively, (HR=3.16, 95% CI: 1.82–4.02, P<0.001; Table 3, Figure 1), while the median OS was 60.9 and 40.3 months for patients who had low and high SII, respectively (HR =3.78, 95% CI: 2.16–4.15, P<0.001; Table 3, Figure 2). The median DFS for patients with BI-RADS 5 was 16.5 months, while it was 21.3 months for those with BI-RADS 3–4 (HR =1.74, 95% CI: 1.23–2.45, P=0.001; Table 3, Figure 3). The median OS was 41.2 and 57.7 months for patients with BI-RADS 5 and 3–4, respectively (HR =2.35, 95% CI: 1.61–3.42; P<0.001; Figure 4, Table 3).
  | Figure 1 DFS rates for 215 patients with TNBC as indicated by SII (P<0.001). Abbreviations: DFS, disease-free survival; SII, systemic immune-inflammation index; TNBC, triple-negative breast cancer. |
  | Figure 2 OS rates for 215 patients with TNBC as indicated by SII (P<0.001). Abbreviations: OS, overall survival; SII, systemic immune-inflammation index; TNBC, triple-negative breast cancer. |
Multivariable analysis
Multivariable analysis showed that elevated SII was an independent risk factor for poor DFS (HR =2.85, 95% CI: 1.62–3.81, P=0.005; Table 4) and for poor OS (HR =2.96, 95% CI: 2.18–3.98, P<0.001; Table 4). Moreover, tumor stage, BI-RADS, and histological grade independently associated with poor OS for patients with TNBC (P=0.002, P<0.001, P<0.004, Table 4).
Discussion
Several studies have demonstrated the association between the inflammatory system and tumors. The number of peripheral inflammatory cells before treatment, including lymphocytes, monocytes, and neutrophils, have shown the strong link between the prognosis of different kinds of cancer and the inflammatory system.22–32 Neutrophils, reportedly, is an indicator of inflammatory and immune response; their involvement in the proliferation and metastasis of tumor by releasing inflammatory factors, such as neutrophil elastase, matrix metalloproteinase-9, and interleukin-8 has been elucidated.33 In addition, platelets have been shown to play a role in promoting angiogenesis and metastases of tumors, as well as shielding tumor cells to protect them from antitumor immune responses.34 In contrast, tumor-infiltrating lymphocytes are involved in the prevention of tumor growth and spread, by initiating antitumor immune response, and correlate with better survival in cancer patients.35,36
Until now, the values of SII in prognosis have been reported in nasopharyngeal carcinoma, prostate cancer, colorectal cancer, pancreatic cancer, gastric cancer, and hepatocellular carcinoma.14–17,19–21,37,38 Hu et al14 reported, for the first time, the role of SII in hepatocellular carcinoma as a novel and independent prognostic indicator. Compared with the patients who had lower SII, patients with higher SII before treatment had shorter survival time and increased recurrence rates. Jiang et al21 also showed SII as an independent predictor for survival in patients with nasopharyngeal carcinoma, while Huang et al39 reported that high SII values correlated with poor clinicopathological features and could be used to identify poor prognosis.
In this study, we have shown that increased SII independently correlates with poor OS and DFS in TNBC patients, which is consistent with previously reported findings. Tong et al20 proved SII’s independent prognostic value when investigating the association between SII and OS and treatment response in patients with non-small-cell lung cancer at stage III. Furthermore, we found that tumor stage, BI-RADS, and histological grade also independently predicted poor DFS, while the same factors, alongside lympho-vascular invasion and lymph node status were independently associated with poor OS for patients with TNBC.
To the best of our knowledge, this study is the first research to explore the clinical significance of SII in Chinese TNBC patients. Nevertheless, there are some limitations in our study. Firstly, even though we ruled out patients with diseases that may influence the SII, some of the patients who took part in our study might have had these diseases but were not registered in the medical records. Secondly, the sample size for our study was small. Finally, this retrospective, single-center study inevitably had selection bias and lacked external validation.
Conclusion
This study indicates that SII may be associated with OS and DFS in TNBC patients and could be conveniently introduced in clinical practice for identifying TNBC patients with poor prognosis. It, however, still requires prospective studies to evaluate the possible role of SII in selecting patients, guiding treatments, and designing clinical trials.
Disclosure
The authors report no conflicts of interest in this work.
References
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. | ||
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. | ||
Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L. Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol. 2016;13(11):674–690. | ||
Brewster AM, Chavez-Macgregor M, Brown P. Epidemiology, biology, and treatment of triple-negative breast cancer in women of African ancestry. Lancet Oncol. 2014;15(13):e625–e634. | ||
van Roozendaal LM, Smit LHM, Duijsens G, et al. Risk of regional recurrence in triple-negative breast cancer patients: a Dutch cohort study. Breast Cancer Res Treat. 2016;156(3):465–472. | ||
Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363(20):1938–1948. | ||
Yang J, Peng L, Sahin AA. Biology and management of patients with triple-negative breast cancer. Breast Cancer Res Treat. 2016;21(9):1050–1062. | ||
Criscitiello C, Azim HA, Schouten PC, Linn SC, Sotiriou C. Understanding the biology of triple-negative breast cancer. Ann Oncol. 2012;23(6):vi13–vi18. | ||
Bosch A, Eroles P, Zaragoza R, Viña JR, Lluch A. Triple-negative breast cancer: molecular features, pathogenesis, treatment and current lines of research. Cancer Treat Rev. 2010;36(3):206–215. | ||
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. | ||
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. | ||
Wang K, Shen T, Siegal GP, Wei S. The CD4/CD8 ratio of tumor-infiltrating lymphocytes at the tumor–host interface has prognostic value in triple-negative breast cancer. Hum Pathol. 2017;69:110–117. | ||
Liu C, Sun B, Xu B, et al. A panel containing PD-1, IL-2Rα, IL-10, and CA15-3 as a biomarker to discriminate breast cancer from benign breast disease. Cancer Manag Res. 2018;10:1749–1761. | ||
Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. | ||
Yang J, Guo X, Wang M, Ma X, Ye X, Lin P. Pre-treatment inflammatory indexes as predictors of survival and cetuximab efficacy in metastatic colorectal cancer patients with wild-type RAS. Sci Rep. 2017;7(1):17166. | ||
Aziz MH, Sideras K, Aziz NA, et al. The systemic-immune-inflammation index independently predicts survival and recurrence in resectable pancreatic cancer and its prognostic value depends on bilirubin levels: a retrospective multicenter cohort study. Ann Surg. 2018;1:1. | ||
Chen L, Yan Y, Zhu L, et al. Systemic immune-inflammation index as a useful prognostic indicator predicts survival in patients with advanced gastric cancer treated with neoadjuvant chemotherapy. Cancer Manag Res. 2017;9:849–867. | ||
Lolli C, Basso U, Derosa L, et al. Systemic immune-inflammation index predicts the clinical outcome in patients with metastatic renal cell cancer treated with sunitinib. Oncotarget. 2016;7(34):54564–54571. | ||
Fan L, Wang R, Chi C, et al. Systemic immune-inflammation index predicts the combined clinical outcome after sequential therapy with abiraterone and docetaxel for metastatic castration-resistant prostate cancer patients. Prostate. 2018;78(4):250–256. | ||
Tong YS, Tan J, Zhou XL, Song YQ, Song YJ. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J Transl Med. 2017;15(1):221. | ||
Jiang W, Chen Y, Huang J, et al. Systemic immune-inflammation index predicts the clinical outcome in patients with nasopharyngeal carcinoma: a propensity score-matched analysis. Oncotarget. 2017;8(39):66075–66086. | ||
Chen Y, Chen K, Xiao X, et al. Pretreatment neutrophil-to-lymphocyte ratio is correlated with response to neoadjuvant chemotherapy as an independent prognostic indicator in breast cancer patients: a retrospective study. BMC Cancer. 2016;16:320. | ||
Yao M, Liu Y, Jin H, et al. Prognostic value of preoperative inflammatory markers in Chinese patients with breast cancer. Onco Targets Ther. 2014;7:1743–1752. | ||
Pistelli M, de Lisa M, Ballatore Z, et al. Pre-treatment neutrophil to lymphocyte ratio may be a useful tool in predicting survival in early triple negative breast cancer patients. BMC Cancer. 2015;15:195. | ||
Liu C, Huang Z, Wang Q, et al. Usefulness of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in hormone-receptor-negative breast cancer. Onco Targets Ther. 2016;9:4653–4660. | ||
Yamagishi T, Fujimoto N, Nishi H, et al. Prognostic significance of the lymphocyte-to-monocyte ratio in patients with malignant pleural mesothelioma. Lung Cancer. 2015;90(1):111–117. | ||
Templeton AJ, Mcnamara MG, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. | ||
Kao SC, Pavlakis N, Harvie R, et al. High blood neutrophil-to-lymphocyte ratio is an indicator of poor prognosis in malignant mesothelioma patients undergoing systemic therapy. Clin Cancer Res. 2010;16(23):5805–5813. | ||
Cannon NA, Meyer J, Iyengar P, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol. 2015;10(2):280–285. | ||
Song S, Li C, Li S, Gao H, Lan X, Xue Y. Derived neutrophil to lymphocyte ratio and monocyte to lymphocyte ratio may be better biomarkers for predicting overall survival of patients with advanced gastric cancer. Onco Targets Ther. 2017;10:3145–3154. | ||
Grenader T, Nash S, Plotkin Y, et al. Derived neutrophil lymphocyte ratio may predict benefit from cisplatin in the advanced biliary cancer: the ABC-02 and BT-22 studies. Ann Oncol. 2015;26(9):1910–1916. | ||
Liu C, Wu S, Meng X, et al. Predictive value of peripheral regulatory T cells in non-small cell lung cancer patients undergoing radiotherapy. Oncotarget. 2017;8(26):43427–43438. | ||
Houghton AM, Rzymkiewicz DM, Ji H, et al. Neutrophil elastase-mediated degradation of IRS-1 accelerates lung tumor growth. Nat Med. 2010;16(2):219–223. | ||
Franco AT, Corken A, Ware J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood. 2015;126(5):582–588. | ||
Ali HR, Provenzano E, Dawson SJ, et al. Association between CD8+ T-cell infiltration and breast cancer survival in 12,439 patients. Ann Oncol. 2014;25(8):1536–1543. | ||
Mohammed ZM, Going JJ, Edwards J, McMillan DC. The role of the tumour inflammatory cell infiltrate in predicting recurrence and survival in patients with primary operable breast cancer. Cancer Treat Rev. 2012;38(8):943–955. | ||
Geng Y, Shao Y, Zhu D, et al. Systemic immune-inflammation index predicts prognosis of patients with esophageal squamous cell carcinoma: a propensity score-matched analysis. Sci Rep. 2016;6:39482. | ||
Fukuda H, Takagi T, Kondo T, Shimizu S, Tanabe K. Predictive value of inflammation-based prognostic scores in patients with metastatic renal cell carcinoma treated with cytoreductive nephrectomy. Oncotarget. 2018;9(18):14296–14305. | ||
Huang L, Liu S, Lei Y, et al. Systemic immune-inflammation index, thymidine phosphorylase and survival of localized gastric cancer patients after curative resection. Oncotarget. 2016;7(28):44185–44193. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.