Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Suvorexant: a promising, novel treatment for insomnia
Authors Lee-Iannotti J, Parish J
Received 1 July 2015
Accepted for publication 19 August 2015
Published 25 February 2016 Volume 2016:12 Pages 491—495
DOI https://doi.org/10.2147/NDT.S31495
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Joyce K Lee-Iannotti,1 James M Parish2
1Division of Neurology, Sleep Disorders Center, Banner University Medical Center, Phoenix, AZ, USA; 2Division of Pulmonary Medicine, Center for Sleep Medicine, Mayo Clinic, Phoenix, AZ, USA
Abstract: Suvorexant a novel, orexin receptor antagonist was recently approved by the US Food and Drug Administration for the treatment of sleep onset and sleep maintenance insomnia in August 2014. Multiple animal and human studies support the efficacy, safety, and tolerability of suvorexant for patients of various profiles. Current recommendations advocate for a starting dose of 10 mg and a maximum dose of 20 mg, with cautious use in women, obese patients, and patients taking other CYP3A4 inhibitors. More head-to-head studies comparing suvorexant to other sedative-hypnotic therapies are needed to further delineate which patients will benefit the most from this medication over others.
Keywords: insomnia, orexin-receptor antagonist, CYP3A4, benzodiazepan receptor antagonist, MK-4305
Background
Insomnia is a disorder in which people experience difficulty falling asleep or maintaining sleep.1 Lack of consolidated sleep may lead to daytime sleepiness, lack of focus and attention, worsening depression or anxiety, and decreased energy.2 Insomnia can affect quality of life, work performance, and functioning on a daily basis.
There are two types of insomnia: primary and secondary insomnia. Secondary insomnia is the most common disorder, estimated to affect eight out of ten people with insomnia. It is usually related to other comorbidities (eg, heart or lung diseases, mood disorders, and other sleep conditions such as restless legs syndrome or sleep apnea) or side effects from toxins or medications (eg, stimulant therapy, caffeine, tobacco, alcohol).2 In contrast, primary insomnia is not attributable to underlying medical, psychiatric, or environmental causes. It is an isolated disorder of poor sleep quality (difficulty falling asleep, multiple nocturnal awakenings with inability to resume sleep with each arousal). When insomnia persists for more than 3 nights per week for more than 3 months, it is defined as chronic or persistent insomnia. If it occurs for less than 1 week, then it is considered acute; if it occurs between 1 week and 3 months, then it is subacute.3,4
Insomnia remains a significant undertreated and underrecognized medical condition. It is estimated that approximately 30%–50% of adults experience insomnia at some point in their lifetime, with chronic insomnia occurring in 9%–12% of adults.5,6 Those at risk for insomnia include the elderly (estimated as high as 20% of the elderly population), women, patients with mental and chronic medical disorders, shift workers, frequent travelers who cross multiple time zones, and persons with constant stressors.5
Several pharmacological therapies for insomnia have been formulated, including benzodiazepine receptor antagonists (BzRAs) (eg, benzodiazepines and nonbenzodiazepine sedative-hypnotics, such as zolpidem, zaleplon, and eszopiclone), melatonin, melatonin-receptor agonists, and various antidepressant medications including quetiapine, amitriptyline, mirtazapine, and trazodone. Some are approved for use by the US Food and Drug Administration (FDA), while others are used off-label.1 The most novel treatment is suvorexant (MK-4305), a potent and selective orexin receptor antagonist, which has shown promise in animals and human studies.7,8
Pharmacology
Suvorexant acts by blocking the orexin system, therefore reducing arousals and improving sleep consolidation. The orexin system is located in the lateral hypothalamus and plays a crucial role in the arousal system.9 In normal animal models, there is a diurnal variation of orexin activity, with increased activity during wakefulness and reduced activity during sleep.10,11 A well-established connection between orexin mutations and narcolepsy has been shown in the literature, both in humans and animals.12 Suvorexant acts by blocking the orexin-mediated wakefulness and inducing sleep. Unlike the BzRAs, which act diffusely on the gamma-aminobutyric acid (GABA) receptors and cause side effects such as visual hallucinations, memory problems, dependence, and next-day “hangover effect”, suvorexant is thought to act more centrally and selectively on the orexin system, thereby reducing adverse effects and abuse potential.13
Suvorexant exhibits linear pharmacokinetics, with a mean half-life of approximately 12 hours, reaching a steady state by 3 days.14 It is extensively bound to plasma proteins with an estimated bioavailability of 82% for the 10 mg dosage. Interestingly, absorption is inversely proportional to dosage, with a dose of 80 mg showing much less bioavailability than the 10 mg dose. It is advised that it be taken on an empty stomach with a time-to-peak concentration (Tmax) of 2 hours. Food intake delays the Tmax by up to 90 minutes. See Table 1 for comparison of pharmacokinetics of various available sedative-hypnotics.
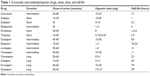  | Table 1 Commonly used sedating/hypnotic drugs, onset, dose, and half-life |
It is metabolized by the CYP3A4 (major) and CYP2C19 (minor) systems, resulting in an inactive hydroxyl-suvorexant metabolite and is eliminated mainly through the feces (~66%) and the urine (23%). The pharmacokinetics of suvorexant are affected by body mass index and sex. In obese patients, the area under the curve or maximum concentration (Cmax) is increased by approximately 31%. In women, the area under the curve is increased by 17%, and Cmax is 9% in women and 5% in men. Obese women are additively at higher risk of overdosing. Thus, lower starting dosages and more gradual titrations are recommended for both women and obese patients.14
Clinical trials
In animal studies involving rodents, dogs, and rhesus monkeys, suvorexant was shown to reduce active wake time and increase rapid eye movement (REM) sleep and slow wave activity.7,8 The long-term effects of these findings and clinical relevance are unclear but hypothesized to be beneficial.
In humans, until now, there are three randomized, double blind, placebo-controlled trials showing suvorexant to be effective and safe for the treatment of insomnia. The first trial was led by Herring et al15 in 2012, which incorporated a crossover design in adult patients (age 18–64 years) receiving one of four suvorexant dosages for 4 weeks (62 patients on 10 mg, 61 on 20 mg, 59 on 40 mg, and 61 on 80 mg) and placebo for the other 4 weeks. The treatment order was randomized with a week-long washout period in between. Efficacy was assessed objectively by a polysomnogram (PSG) on night 1 and at the end of week 4 (day 28). The primary end point was sleep efficiency (calculated as total sleep time [TST] divided by time in bed in minutes). Secondary end points included wake after sleep onset (WASO) and latency to persistent sleep (LPS). The results showed significant dose-related improvement in both the primary and secondary end points in the treatment versus the placebo group (P<0.001). Adverse effects were dose-dependent, but overall, minor. The most common side effect was somnolence, reported in 1.6% of the 10 mg dosage group versus 11.5% in the 80 mg group. There was one patient who reported excessive next-day sedation, which was noted in the high dose group (80 mg).
In the second trial in 2013, Sun et al16 published a study showing favorable outcomes in healthy, young men (age 18–45 years) taking suvorexant implementing sleep parameters obtained in a sleep laboratory setting. Similar to Herring’s study, this study incorporated a crossover design with a 4-period crossover PSG and an additional 5th week to assess the pharmacokinetics of the drug. Each patient underwent two PSG-monitored nights: one for habituation off of medication, followed by a second night with medication. Suvorexant dosages of 10, 50, 100 mg or placebo were used in a randomized fashion. Results showed that all doses of suvorexant effectively promoted sleep compared to placebo, with no significant effects on PSG sleep parameters including sleep stages, slow wave sleep, or delta activity. The greatest decrease on sleep parameters (decreased LPS and WASO; increased sleep efficiency and TST) was observed in the higher 50 and 100 mg doses, but the 10 mg dose also showed favorable decreased WASO. No serious adverse effects were reported but reports of next-day residual effects of sedation were noted to be dose-dependent (20.5% with 100 mg dose versus 4.5% with 10 mg dose).
The third trial was performed by Michelson et al in 2014.17 Subjects younger than 65 years received 40 mg of suvorexant, while those older than 65 years received a lower dose of 35 mg. Both groups took the medication for up to 1 year, followed by a 2-month randomized washout phase to assess the potential for withdrawal effects and rebound with abrupt discontinuation. Results showed no significant safety or withdrawal/rebound effects. Subjective reports of TST were improved in the treatment group versus placebo (38.7 versus 16 minutes; 95% CI =16.4–29.0, P<0.0001). Similarly, time-to-sleep onset improved with the treatment group showing −18 versus −8.4 minutes in the placebo group (95% CI =−14.6 to −4.5, P=0.0002). Furthermore, those subjects that continued therapy beyond 1 year reported continued benefit.
It is imperative to recognize that although they were notable clinical trials, there were several limitations. None of the studies assessed the value of combination therapy with suvorexant plus behavioral interventions (eg, cognitive behavioral therapy [CBT], sleep hygiene therapy, etc). Additionally, no head-to-head comparisons with nonpharmacological therapies or even competing pharmacological therapies were performed to assess superiority/inferiority (eg, zolpidem versus suvorexant, suvorexant versus CBT). Patients with prior history of drug abuse or addiction (illicit drugs, narcotics, alcohol) were excluded, limiting the ability to comment on the risk of abuse potential of suvorexant in known addicts. Finally, longitudinal studies are needed over a longer period of time to assess safety and efficacy over time. Although sedative-hypnotic therapy for insomnia is intended to be short-term, many insomniacs tend to use medications for much longer, particularly with chronic, secondary insomnia.
Current FDA recommendations
In August 2014, the FDA approved four strengths of suvorexant, ie, 5, 10, 15, and 20 mg.18 Higher dosages were not approved due to concern for dose-related side effects, particularly drowsy driving. The current recommendation is to start with a dose of 10 mg, which is to be taken within 30 minutes prior to bedtime. The maximum dose is 20 mg. However, the FDA cautions prescribers on the use of higher doses in females, obese patients, and patients taking competing CYP3A4 inhibitors. No adjustment is needed for renal or hepatic impairment at this time.
Due to concerns for abuse or addiction potential, suvorexant was classified as a Schedule IV controlled substance.19
Adverse effects and contraindications
Based on the clinical trials (see the section “Clinical trials”), the most common adverse effects of suvorexant included somnolence, fatigue, and headache. Other side effects included dry mouth, cough, and increased incidence of respiratory tract infections. The risk of adverse effects was dose-dependent and seemed to occur more frequently in women than men. There was no reported difference in younger versus elderly patients (>65 years).
Suvorexant is contraindicated in patients with narcolepsy or suspected narcolepsy, based on the mechanism of action and potential to accentuate daytime sleepiness in these already sleepy individuals.
For patients on potent CYP3A4 inhibitors (eg, ketoconazole, clarithromycin, ritonavir), the recommended maximum dose is 10 mg (starting dose of 5 mg). For patients on CYP3A4 inducers (eg, rifampin and antiepileptics such as phenytoin and carbamazepine), higher doses may be required for efficacy. As with all other sedative-hypnotics, concomitant use of other sedating medications should be strictly avoided.
Currently, suvorexant is considered Pregnancy Category C (not been sufficiently studied in pregnant women). Use of suvorexant is discouraged in breast-feeding mothers, although it is unknown if it is secreted in breast milk.14
Therapeutic indications and patient selection
The American Academy of Sleep Medicine (AASM) emphasizes the value of nonpharmacological therapies (treating comorbid conditions, discontinuing medications that may perpetuate insomnia, CBTs, and relaxation exercises) prior to initiation of medications. However, if pharmacological therapy is indicated, the current AASM guidelines recommend nonbenzodiazepine hypnotics (ie, zolpidem, zaleplon, eszopiclone) or melatonin MT1 and MT2 receptor agonists (ie, ramelteon) as first-line agents, followed by sedating antidepressants and benzodiazepines for patients failing first-line therapies. Over-the-counter regimens, although frequently used by patients, have no standard AASM recommendations due to lack of evidence and efficacy data. Because suvorexant is fairly new, the AASM has not made official recommendations regarding its use.
As shown before, clinical trials have demonstrated that suvorexant is safe, efficacious, and well-tolerated overall. Significant improvements in sleep quality and sleep latency compared to placebo are apparent. Based on the current available data and our pharmacological understanding of suvorexant, there may be several advantages of orexin antagonists over other sedative-hypnotics. To begin with, because it is more centrally acting and targets the specific orexin receptors, it is less likely to cause major side effects (residual next-day sleepiness, drowsy driving, and undesired behaviors in sleep). Along the same lines, the potential for abuse and withdrawal effects with abrupt discontinuation may be much less than BzRAs, which act diffusely on the GABA-nergic system. Surprisingly, studies have shown good tolerability in the elderly, unlike BzRAs or benzodiazepines, both of which can cause gait imbalance with higher risk of falls, memory impairment, and psychomotor slowing. Superiority of suvorexant over other competing sedative-hypnotics, however, is difficult to gauge due to the lack of head-to-head trials comparing pharmacological options for insomnia. This is where future clinical trials will play a major role.
Of relevance, however, Ma et al20 compared the electroencephalographic (EEG) power spectral density profile of suvorexant with placebo, along with comparisons to gaboxadol 15 mg, zolpidem 10 mg, and trazodone 150 mg during REM and non-REM sleep. They found that suvorexant had limited effects on the power spectral density compared with placebo and other insomnia treatments, suggesting that suvorexant may improve sleep without deleterious neurophysiological changes illustrated by EEG.
The biggest foreseeable barrier to the widespread use of suvorexant is availability and cost. The estimated cost of suvorexant is between $200 and $300 per month (manufactured by Merck & Co, Inc., Whitehouse Station, NJ, USA), compared to generic BzRAs and benzodiazepines that can cost as low as $5–$10 per month. Due to its relatively new FDA approval, obtaining suvorexant is also challenging, particularly in rural parts of the USA.
Summary
Suvorexant, the first orexin receptor antagonist approved for the treatment of sleep onset and sleep maintenance insomnia holds promise for patients suffering from insomnia. Although more head-to-head studies are required, landmark clinical trials have shown that suvorexant is safe, well-tolerated, and efficacious. Ongoing trials will help further delineate optimal dosing, ideal length of treatment, and suitable candidates for suvorexant use.
Disclosure
The authors have no conflicts of interest or financial involvement with this paper.
References
Merrigan JM, Buysse DJ, Bird JC, et al. Insomnia. JAMA. 2013;309:733. | ||
American Sleep Association. About Insomnia. Available from: https://www.sleepassociation.org/patients-general-public/insomnia/insomnia/. Accessed June 1, 2015. | ||
American Academy of Sleep Medicine. International Classification of Sleep Disorders, Revised: Diagnostic and Coding Manual. Chicago, IL: American Academy of Sleep Medicine; 2001. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. | ||
Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. | ||
Dopp JM, Phillips BG. Sleep disorders. In: DiPiro JT, Talbert RL, Yee GC, et al. editors. Pharmacotherapy: A Pathophysiological Approach. 9th ed. New York, NY: McGraw-Hill; 2014. | ||
Cox CD, Breslin MJ, Whitman DB, et al. Discovery of the dual orexin receptor antagonist methanone (MK-4305) for the treatment of insomnia. J Med Chem. 2010;53:5320–5332. | ||
Winrow CJ, Gotter AL, Cox CD, et al. Promotion of sleep by MK-4305 – a novel dual orexin receptor antagonist. J Neurogenet. 2011;25:52–61. | ||
Peyron C, Tighe DK, van den Pol AN, et al. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci. 1998;18:9996–10015. | ||
Taheri S, Sunter D, Dakin C, et al. Diurnal variation in orexin A immunoreactivity and prepro-orexin mRNA in the rate central nervous system. Neurosci Lett. 2000;279:109–112. | ||
Zeitzer JM, Buckmaster CL, Parker KJ, et al. Circadian and homeostatic regulation of hypocretin in a primate model: implications for the consolidation of wakefulness. J Neurosci. 2003;23:3555–3560. | ||
Zeitzer JM, Nishino S, Mignot E. The neurobiology of hypocretins (orexins), narcolepsy and related therapeutic interventions. Trends Pharmacol Sci. 2006;27:368–374. | ||
Citrome L. Suvorexant for insomnia: a systematic review of the efficacy and safety profile for the newly approved hypnotic – what is the number needed to treat, number needed to harm, and likelihood to be helped or harmed? Int J Clin Pract. 2014;68:1429–1441. | ||
Belsomra® (survorexant) [package insert]. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2014. | ||
Herring JW, Snyder E, Budd K, et al. Orexin receptor antagonism for treatment of insomnia: a randomized clinical trial of suvorexant. Neurology. 2012;79:2265–2274. | ||
Sun H, Kennedy WP, Darren W, et al. Effects of survorexant, an orexin receptor antagonist, on sleep parameters as measured by polysomnography in healthy men. Sleep. 2013;36:259–267. | ||
Michelson D, Snyder E, Pardis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double blind, placebo-controlled trial. Lancet Neurol. 2014;13:461–471. | ||
US Food and Drug Administration. FDA approves new type of sleep drug, Belsomra. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm409950.htm. Accessed June 2, 2015. | ||
Department of Justice. Drug Enforcement Administration. Schedules of controlled substances: placement of suvorexant into Schedule IV. Final rule. Fed Regist. 2014;79:51243–51247. | ||
Ma AJ, Svetnik V, Snyder E, et al. Electroencephalographic prower spectral density profile of the orexin receptor antagonist surorexant in patients with primary insomnia and healthy subjects. SLEEP. 2014;37(10):1609–1619. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
