Back to Journals » International Journal of General Medicine » Volume 15
Susceptibility to Rubella Infection and Incidence of Congenital Rubella Infection: 6 Years Retrospective Study
Authors Al Dossary RA , Althuwaiqeb S , Alkharsah KR , Wanni NHO, Hunasemaranda BC, Obeid OE, Siddiqui ZI, El-Badry AA, Al Qahtani NH
Received 20 December 2021
Accepted for publication 14 March 2022
Published 2 April 2022 Volume 2022:15 Pages 3605—3611
DOI https://doi.org/10.2147/IJGM.S353867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Reem A Al Dossary,1 Sarah Althuwaiqeb,2 Khaled R Alkharsah,1 Nahid HO Wanni,1 Basavaraja C Hunasemaranda,1 Obeid E Obeid,1 Zaheenul Islam Siddiqui,1 Ayman A El-Badry,1 Nourah Hasan Al Qahtani3
1Department of Microbiology, College of Medicine, Imam Abdulrahman bin Faisal University, Dammam, Saudi Arabia; 2Imam Abdulrahman bin Faisal University, Dammam, Saudi Arabia; 3Department of Obstetrics and Gynecology, College of Medicine, Imam Abdulrahman bin Faisal University, Dammam, Saudi Arabia
Correspondence: Reem A Al Dossary, Email [email protected]
Introduction: Rubella is considered one of the most serious and most common congenital infections. Despite global efforts for elimination, rubella cases are still being reported in many parts of the world. The purpose of this study is to determine the level of immunity to rubella in the community and most importantly among women at childbearing age in the eastern province of Saudi Arabia and compare it with the target set by the World Health Organization (WHO) along with the incidence of acute rubella infection and the associated congenital rubella infection and congenital rubella syndrome.
Methods: This is a retrospective cross-sectional study over the six years period (Jan 2014–Jun 2020) on all individuals tested for rubella IgM and IgG in a university teaching hospital.
Results: Nighty one percent (15,894/17,469) of the population tested showed evidence of rubella immunity with 8.8% (1546/17,469) being susceptible. Among women at childbearing age, susceptibility to rubella was higher with 9.2% (1220/13,278) of women showing no evidence of immunity. In addition, acute rubella infection was reported for 0.17% (29/17,469) of the population tested and 0.15% (20/13,278) in women at childbearing age. No cases of congenital rubella infection were reported in the study period.
Discussion: The level of Rubella immunity in the population is 91% and is less than the WHO target for rubella control therefore, risk of resurge of cases is present, indicating the need for continued national surveillance and more efforts to improve vaccination coverage in the kingdom.
Keywords: rubella, immunity, susceptibility, congenital
Introduction
Rubella was initially considered a mild childhood exanthematous disease characterized by fever, faint maculopapular rash and lymphadenopathies which resolve in few days with no major sequels.1 But with the observation of an Australian ophthalmologist, Sir Norman McAlister Gregg in 1941 of a cluster of1 infants born with cataract and cardiac defect which was associated with maternal history of rubella infection in early pregnancy, rubella was then identified as a major cause of congenital defects.2
Rubella, which is also known as German measles, is caused by Rubella virus, a member of the Togaviridae, genus Rubivirus. Rubella infection or vaccination commonly leads to lifelong immunity, as the virus has only one serotype.3 Rubella virus targets almost all organs of the body leading to a wide range of clinical manifestations. It utilizes myelin oligodendrocyte glycoprotein (MOG) as its receptor along with other yet to be discovered receptors.1 Following primary infection of non-immune pregnant women, rubella virus spreads to the placenta, and from there to the developing fetus causing systemic inflammation and interference with organ development. Rubella virus is believed to cause congenital defects via multiple mechanisms, including necrosis of chorionic epithelium and endothelial cells, inhibition of cell division, and development and induction of immunopathological events.4
Infants born with congenital rubella infection display a variety of manifestations including fetal death, ocular complications (cataract, glaucoma, pigmentary retinopathy, microphthalmia and chorioretinitis), auditory complications (sensorineural hearing loss) and cardiac complications (patent ductus arteriosus, ventricular septal defect and pulmonary artery stenosis).5 Infants born with laboratory evidence of rubella infection in addition to clinical manifestations are referred to as suffering from congenital rubella syndrome (CRS). In addition, infants who survive intrauterine rubella infection, can suffer from developmental and endocrinal problems including autism and insulin dependent diabetes mellitus.6
With the recognition of rubella virus as a major teratogen, vaccination became a primary mode for the control and prevention of this disease. The World Health Organization (WHO) has recommended very-high vaccination coverage of >95% in order to interrupt rubella transmission and prevent congenital rubella infections.7 A live attenuated vaccine for rubella is available in 168 countries as per WHO 2018 statistics8 and is included in the Centers for Disease Control and Prevention (CDC) recommended childhood vaccination schedule.9 Since this vaccine is used primarily to prevent congenital rubella infection, vaccination is recommended for children and is also given to adults at high risk of transmission, like health care workers, travelers, and university freshers.10 This pattern of selective catch-up vaccination of non-immune adults, in addition to the current anti-vaccine propaganda in many parts of the world, might be responsible for the rubella epidemic in Japan in 2012, in which 17,000 rubella cases were reported along with 45 cases of congenital rubella syndrome.11 This epidemic was reported to be caused by non-immune men who represented more than two third of the cases.12 The observed antivaccine behaviors, which has been linked to religious issues, financial problems in the provision of the vaccine and lack of healthcare education, has led to suboptimal global vaccination coverage of around 69%.13 This can lead to unpredicted rubella outbreaks similar to those already reported in Japan,11 Canada,14 China,15 Romania,16 and Ethiopia.17
Understanding the direct relationship between increased maternal susceptibility to rubella and increased congenital rubella cases, along with the current trend of anti-vaccine behaviors in many societies, highlights the need to determine the immune status of childbearing women to rubella before conception in order to predict the likelihood of rubella outbreaks and CRS cases. In line with the WHO Global measles and rubella strategic plan 2012–2020, this study aims to determine the seroprevalence of rubella susceptibility and incidence of acute rubella infections among women of childbearing age, and the associated incidence of congenital rubella infections and congenital rubella syndrome at King Fahad Hospital of the University (KFHU) over the past 6 years.
Method
This is a 6-years retrospective study on all individuals tested for rubella virus infection between Jan 2014 and Jun 2020 at KFHU in the Eastern Province of Saudi Arabia. The study population included newborn babies and infants below one year of age tested for suspected congenital rubella infection. In addition, all women at childbearing age (14–49 years) tested for rubella immunity or suspected acute rubella infection at antenatal clinics were included. Clinical and laboratory data for all patients tested were obtained retrospectively from computerized patient’s data system.
To determine the overall seroprevalence of rubella susceptibility in the population, and define the mean age of acute rubella infection, all individuals tested for suspected rubella infections including children, females and males were included in the study.
Testing for rubella immunoglobulin G (IgG) and IgM was done using the Liaison® rubella IgG and IgM assays (Dia sorin, Italy) according to manufacturer’s instructions. Rubella IgG and IgM assays were quantitative assays which were interpreted based on the antibody titer (positive IgG ≥10 IU/mL, negative IgG < 10 IU/mL, positive IgM >25 AU/mL, negative IgM < 20 AU/mL, and equivocal IgM 20–25 AU/mL). The Records for rubella IgG and IgM were collected from computerized patient’s data system.
For patients with positive serological tests (positive IgM) indicating acute infection, further clinical data were obtained from patients’ files. The results were interpreted as follows:
Newborn babies and infants of age below 1 year were diagnosed as having congenital rubella infection based on a positive rubella IgM test, regardless of IgG status due to confounding maternal IgG. Diagnosis of congenital infections was difficult after the first year of life using antibody testing due to vaccination and should be done using virus isolation from the affected body site. On the other hand, diagnosis of CRS, requires in addition to laboratory evidence of infection, a positive clinical finding suggestive of rubella which includes ophthalmic changes (cataracts or congenital glaucoma), congenital heart disease, hearing defect, and pigmentary retinopathy, according to CDC definition.18 Detection of rubella infection using Polymerase chain reaction (PCR) was not available in the hospital and was not done to confirm the infection.
Children more than one year of age and adults were considered immune to rubella if they test positive for rubella IgG and susceptible if they are negative for rubella IgG. Acute infection is defined as a positive test result for rubella IgM in the presence or absence of clinical findings.
Results
Overall Seroprevalence of Rubella in the Community and Median Age of Acute Rubella Infection
Since rubella vaccine is given with routine childhood vaccines at 12 and 18 months of age, all individuals aged 2 years and above, that were tested for rubella antibodies, were included in the study. Out of 17,469 individuals tested for rubella antibodies, 8.8% (1546/17,469) were found susceptible, and 91% (15,894/17,469) were immune (Table 1). In addition, the odds ratio for rubella susceptibility increases for individual older than 39, 44 and 49 years of age (OR=1.15, 1.045, and 2.103 respectively (p-value < 0.001)).
 |
Table 1 The Overall Seroprevalence of Rubella Among the Population Stratified by Age Groups |
On the other hand, evidence of acute rubella infection was seen in 0.17% (29/17,469) (Table 2) and the median age of acute rubella infection was found to be 29.1 years. A significant increase in the incidence of acute rubella infection was seen in age group 2–14 years old (p value =0.006). On the contrary, a significant reduction in acute rubella infection was seen in age group 19–24 years old (p value =0.002).
 |
Table 2 The Incidence of Acute Rubella Infection According to Age Groups as Indicated by IgM Detection |
Rubella Susceptibility and Incidence of Acute Rubella Infection in Women at Childbearing Age
During the 6 years period of the study, 13,278 females at childbearing age (14–49) were tested for rubella for which 13,894 rubella IgG and 1478 rubella IgM tests were done. Out of all women tested, 9.2% (1220/13,258) were found susceptible to rubella, 90.8% (12,038/13,258) were immune, and 0.15% (20/13,258) had serological profiles suggestive of primary acute rubella infection, demonstrated by positive IgM immunoglobulin (Table 3), with median age of 29.5 years. More than one third of the cases (35%) of acute rubella infections occur for women between 29 and 34 years of age and 25% of the cases were among women at 24–29 years of age (Table 3). A significant association was found between rubella susceptibility and increasing age (p value <0.001)
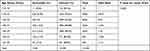 |
Table 3 Frequency of Rubella Seroprevalence Among Women at Childbearing Age in Different Age Groups |
Fifteen women with serological evidence of acute rubella infection were completely asymptomatic, of which 8 were non pregnant ladies. Two women presented with rash and one reported miscarriage with birth defects and two with birth defects. None of the cases reported fever, sore throat, or joint pain.
Congenital Rubella Infections and Congenital Rubella Syndrome (CRS)
During the study period, 212 infants below the age of one year were tested for rubella. None of the tested infants were positive for rubella IgM, indicating no probable acute rubella infection. Yet, for women tested positive for rubella IgM during pregnancy, there is one report of miscarriage and three reports of birth defect with no reported results of rubella IgM for the newborn babies.
Discussion
Prior to introduction of rubella vaccine in Saudi Arabia in routine childhood vaccination in 1991,19 various studies has shown that the level of rubella seropositivity, due to natural infection, among women at childbearing age ranges between 90–95%.20,21 Being one of the most common and serious congenital infections associated with fetal loss and teratogenicity, the WHO suggested a vaccination coverage of 95% is required to prevent congenital rubella infections. But recently, with antivaccination behaviors observed in many countries due to safety concern, cases of rubella continued to be seen.22 In 2020, one study in western part of Saudi Arabia showed that 88.9% of women are immune to rubella and another study showed that rubella susceptibility in women was as high as 24%.23,24 Furthermore, WHO report 62 rubella cases in Saudi Arabia in 2019 along with 4 cases of congenital rubella syndrome in the period 2017–2018.22 Therefore this study was done to determine the seroprevalence of rubella in the eastern province of Saudi Arabia and report cases of acute rubella infections to guide and assess national vaccination programs.
This six-year retrospective study showed that 8.8% of the general population is susceptible to rubella infection and that 91% of the population is immune. Acute rubella infection, defined as positive rubella IgM, occurred in 17/10,000 which is considerably higher than the goal set by the WHO to eliminate congenital rubella infections.
More importantly, among women at childbearing age, rubella seronegativity was detected in 9.2%. This rate is comparable to the global estimates of 9.4% seronegativity, using pooled meta-analysis data,25 but is higher that the WHO target of 5%. Reports from different parts of the world showed variable rubella seronegativity rates among pregnant women and women at child bearing age ranging between zero % in Turkey to 53% in Nigeria.25 This variation is directly linked to national vaccination programs and is affected by the study design. Rubella susceptibility rates of 9.2% among women at childbearing age in our study is warning and indicates a possible risk for resurgence of rubella cases and subsequently congenital rubella infections. In particular, many expatriate from countries like Africa and south east Asia, where vaccination coverage is low are visiting the kingdom and this also increase the chance of outbreaks of rubella.13
In addition, evidence for primary acute rubella infection was present in 0.15% of the women at childbearing age. Although this rate is similar to rates reported from developing countries like Tanzania (0.3%), it is very high as compared to countries like UK, where the rate is 0.23 per 100,000.26 Furthermore, the median age of acute rubella infection in our study is 29.1 years, which is expected to be seen in countries with high childhood vaccination coverage, where the infection is mostly seen in adults due to the waning immune response. But surprisingly, the level of rubella susceptibility in children below 14 years is also higher, reaching 10.96%, indicating a possible impact of inadequate vaccination coverage which will eventually lead to a higher level of susceptibility among women at childbearing age. This group of susceptible women are at risk of developing the infection that may lead to a possible outbreak of CRS. Attention to this problem is extremely important to prevent the outbreak. Recently, the Ministry of Health has issued a mandate for all hospitals in public and private sectors to give rubella vaccine to all post-partum women immediately after delivery in the hospital. It is also repeated after 4 weeks in the primary care clinic. This effort will have a great impact on reducing the possible outbreak of CRS among multiparous women. However, women in their first pregnancy will still be at risk. Our recommendation is to include the testing for rubella as a part of the pre-marital mandatory testing performed in Saudi Arabia since 2004.27 Those who are susceptible should be vaccinated when coming to pick up their results along with folic acid. To eliminate rubella and congenital rubella infections, high coverage using a two-dose childhood vaccination program must be implemented. The United Kingdom (UK) has achieved the WHO rubella elimination status in 2016 by committing to rubella vaccination for the past 35 years. Rare cases are reported in UK in mothers who are born outside of UK.28,29
One of the limitations of this study is that we were unable to get the data of the newborn babies or about the pregnancies. The outcomes of those 20 pregnancies are unknown. It could have ended in abortion, CRS, or no effect.
Conclusion
In the era of wide availability of rubella vaccination in the kingdom of Saudi Arabia and inclusion of rubella in national vaccination programs for almost 20 years, rubella is not eliminated and the level of immunity within the study population is 91% and among women at childbearing age is almost 90.8%. This indicate that efforts need to be continued to improve vaccination coverage to 95% in order to control rubella and subsequently, prevent all cases of severe congenital rubella syndrome within the kingdom.
Abbreviations
MOG, myelin oligodendrocyte glycoprotein; CRS, congenital rubella syndrome; WHO, World Health Organization; CDC, Centers for Disease Control and Prevention; Ig, Immunoglobulin.
Data Sharing Statement
All data used and discussed in this study is available from the corresponding author upon request.
Ethics Approval and Consent to Participate
The protocol of the study was evaluated and reviewed by the Standing Committee on Research Ethics on Living Creatures (SCRELC) at Imam Abdulrahman Bin Faisal University and Ethical approval for this study was obtained (IRB-2018‐01‐ 157). Patient consent was not requested due to the retrospective nature of the study and the large number of participants. Patient datasets were obtained from the hospital information technology department upon IRB approval. All data presented did not include any identifiable data and were managed in accordance with Helsinki declarations were patients’ rights and confidentiality were maintained throughout the study. In addition, the study did not represent any additional risk to the participant and did not interfere with patient management in the hospital.
Acknowledgments
The project team is thankful to the Deanship of Scientific Research at Imam Abdulrahman Bin Faisal University (IAU), Dammam, Saudi Arabia, for their support and to the information technology department at King Fahd hospital of the University for their tremendous efforts in providing data.
Funding
The project is a non-funded project.
Disclosure
All authors declare no conflict of interest.
References
1. Lambert N, Strebel P, Orenstein W, Icenogle J, Poland GA. Rubella. Lancet. 2015;385(9984):2297–2307. doi:10.1016/S0140-6736(14)60539-0
2. Hertzberg R. Congenital cataract following German measles in the mother. Abstracts from the publications of the late Sir Norman McAlister Gregg. Aust NZ J Ophthalmol. 1985;13(3):303–309. doi:10.1111/j.1442-9071.1985.tb00439.x
3. Best JM, Thomson A, Nores JR, O’Shea S, Banatvala JE. Rubella virus strains show no major antigenic differences. Intervirology. 1992;34(3):164–168. doi:10.1159/000150277
4. Bouthry E, Picone O, Hamdi G, Grangeot-Keros L, Ayoubi JM, Vauloup-Fellous C. Rubella and pregnancy: diagnosis, management and outcomes. Prenat Diagn. 2014;34(13):1246–1253. doi:10.1002/pd.4467
5. Leung AKC, Hon KL, Leong KF. Rubella (German measles) revisited. Hong Kong Med J. 2019;25(2):134–141. doi:10.12809/hkmj187785
6. Yazigi A, De Pecoulas AE, Vauloup-Fellous C, Grangeot-Keros L, Ayoubi JM, Picone O. Fetal and neonatal abnormalities due to congenital rubella syndrome: a review of literature. J Matern Fetal Neonatal Med. 2017;30(3):274–278. doi:10.3109/14767058.2016.1169526
7. World Health Organization. Strategic Plan for Measles and Congenital Rubella Infection in the European Region of WHO. Copenhagen: WHO Regional Office for Europe; 2003.
8. Grant GB, Desai S, Dumolard L, Kretsinger K, Reef SE. Progress toward rubella and congenital rubella syndrome control and elimination - worldwide, 2000–2018. MMWR Morb Mortal Wkly Rep. 2019;68(39):855–859. doi:10.15585/mmwr.mm6839a5
9. McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR–04):1–34.
10. Center for Disease Control and Prevention. Routine measles, mumps, and rubella vaccination; 2021. Available from: https://www.cdc.gov/vaccines/vpd/mmr/hcp/recommendations.html.
11. Sugishita Y, Takahashi T, Hori N, Abo M. Ongoing rubella outbreak among adults in Tokyo, Japan, June 2012 to April 2013. Western Pac Surveill Response J. 2013;4(3):37–41. doi:10.5365/wpsar.2013.4.2.011
12. Minakami H, Kubo T, Unno N. Causes of a nationwide rubella outbreak in Japan, 2012–2013. J Infect. 2014;68(1):99–101. doi:10.1016/j.jinf.2013.09.002
13. World Health Organization. Rubella; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/rubella.
14. Macey JF, Tam T, Lipskie T, Tipples G, Eisbrenner T. Rubella elimination, the Canadian experience. J Infect Dis. 2011;204(Suppl 2):S585–92. doi:10.1093/infdis/jir406
15. Chang C, Ma H, Liang W, et al. Rubella outbreak and outbreak management in a school setting, China, 2014. Hum Vaccin Immunother. 2017;13(4):772–775. doi:10.1080/21645515.2016.1252494
16. Lazar M, Abernathy E, Chen MH, et al. Epidemiological and molecular investigation of a rubella outbreak, Romania, 2011 to 2012. Euro Surveill. 2016;21(38). doi:10.2807/1560-7917.ES.2016.21.38.30345
17. Dinede G, Wondimagegnehu A, Enquselassie F. Rubella outbreak in the school children, Addis Ababa, Ethiopia: February-April 2018. BMC Infect Dis. 2019;19(1):267. doi:10.1186/s12879-019-3873-y
18. Tatiana Lanzieri MS, Joseph Icenogle MS. Congenital rubella syndrome: national center for immunization and respiratory diseases; 2020. Available from: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt15-crs.html.
19. Abdullah MA, Jamjoom G, Karrar ZA, Badreldine A, Jishi NA, Taha SA. Seroepidemiology of rubella in Saudi Arabia: an adapted vaccination policy. J Epidemiol Community Health. 1984;38(3):236–239. doi:10.1136/jech.38.3.236
20. Hossain A. Seroepidemiology of rubella in Saudi Arabia. J Trop Pediatr. 1989;35(4):169–170. doi:10.1093/tropej/35.4.169
21. Alsibiani SA. Rubella immunity among pregnant women in Jeddah, Western Region of Saudi Arabia. Obstet Gynecol Int. 2014;2014:659838. doi:10.1155/2014/659838
22. World Health Organization. WHO vaccine-preventable diseases: monitoring system 2020 global summary; 2020. Available from: https://apps.who.int/immunization_monitoring/globalsummary/timeseries/tsincidencecrs.html.
23. Al-Hakami AM, Paul E, Al-Abed F, et al. Prevalence of toxoplasmosis, rubella, cytomegalovirus, and herpes (TORCH) infections among women attending the antenatal care clinic, maternity hospital in Abha, Southwestern Saudi Arabia. Saudi Med J. 2020;41(7):757–762. doi:10.15537/smj.2020.7.25121
24. AlShamlan NA, AlOmar RS, AlOtaibi AS, et al. Seroprevalence of rubella virus among pregnant women: a 4-year registered-based study from family medicine and obstetric clinics in Saudi Arabia. Int J Clin Pract. 2021;75(6):e14156. doi:10.1111/ijcp.14156
25. Pandolfi E, Gesualdo F, Rizzo C, et al. Global seroprevalence of rubella among pregnant and childbearing age women: a meta-analysis. Eur J Public Health. 2017;27(3):530–537. doi:10.1093/eurpub/ckw259
26. Bukasa A, Campbell H, Brown K, et al. Rubella infection in pregnancy and congenital rubella in United Kingdom, 2003 to 2016. Euro Surveill. 2018;23(19). doi:10.2807/1560-7917.ES.2018.23.19.17-00381
27. Gosadi IM. National screening programs in Saudi Arabia: overview, outcomes, and effectiveness. J Infect Public Health. 2019;12(5):608–614. doi:10.1016/j.jiph.2019.06.001
28. Guidance UK measles and rubella elimination indicators and status: public health England; 2019. Available from: https://www.gov.uk/government/publications/measles-and-rubella-elimination-uk/uk-measles-and-rubella-elimination.
29. Research and analysis confirmed cases of measles, mumps and rubella in England and Wales: 1996 to 2020: public health England; 2021. Available from: https://www.gov.uk/government/publications/measles-confirmed-cases/confirmed-cases-of-measles-mumps-and-rubella-in-england-and-wales-2012-to-2013.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
