Back to Journals » Vascular Health and Risk Management » Volume 19
Survival status and predictors of mortality among adult Stroke patients admitted to Jimma University Medical Center, South west Ethiopia: A retrospective Cohort study
Authors Mosisa W, Gezehagn Y, Kune G, Chego M , Yigezu HF, Getnet M
Received 17 May 2023
Accepted for publication 8 August 2023
Published 25 August 2023 Volume 2023:19 Pages 527—541
DOI https://doi.org/10.2147/VHRM.S399815
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Daniel Duprez
Wakgari Mosisa,1 Yenealem Gezehagn,2 Guta Kune,2 Melese Chego,3 Hamba Fida Yigezu,1 Masrie Getnet2
1Department of Public Health, Institute of Health Sciences, Dambi Dollo University, Dambi Dollo, Ethiopia; 2Department of Epidemiology, College of Public Health, Jimma University, Jimma, Ethiopia; 3Department of Public Health, Wollega University, Nekemte, Ethiopia
Correspondence: Guta Kune, Email [email protected]
Background: Stroke is the leading cause of cardiovascular disease death in sub-Saharan Africa and the second leading cause of mortality worldwide. In 2016, 6.23% of all fatalities in Ethiopia were stroke-related.
Objective: To assess survival status and predictors of mortality among adult stroke patients admitted to Jimma University Medical Center from April 1/2017 to March 31/2022.
Methods: A retrospective cohort study was conducted on 480 adult stroke patients selected by simple random sampling from patients admitted to the Jimma University Medical Center Stroke Unit from April 1, 2017 to March 31, 2022. Data were extracted from May to June 2022 and entered Epi-data v.3.1 and analyzed by R v.4.2. The Kaplan-Meier curve with Log rank test was used to estimate survival time and to compare survival experience between categories of explanatory variables. The Cox regression model was computed to identify predictors of survival status in stroke patients. Then the 95% CI of the hazard ratio was set with corresponding p-value < 0.05 to declare statistical significance.
Results: During 4350 person-days of follow-up; 88 (18.33%) patients died; resulting in an incidence mortality of 20.23 per 1000 person-days, with a median survival time of 38 days. Glasgow coma score < 8 on admission (AHR = 7.71; 95% CI: 3.78, 15.69), dyslipidemia (AHR = 3.96; 95% CI: 2.04, 7.69), aspiration pneumonia (AHR 2.30; 95% CI: 1.23– 4.26), and increased intracranial pressure (AHR = 4.27; 95% CI: 2.33, 7.81), were the independent predictors of the time until death.
Conclusion: The incidence of stroke mortality was higher at the seven and fourteen days. Glasgow Coma Scale, increased intracranial pressure, dyslipidemia, and aspiration pneumonia were independent predictors of mortality.
Keywords: stroke, survival time, predictors, retrospective cohort, JUMC, Southwest Ethiopia
Introduction
The World Health Organization describes stroke as a clinical syndrome with rapidly growing clinical indicators of focal or global impairment of brain function in the case of coma, with symptoms lasting more than 24 hours or culminating in death, with no other obvious cause other than vascular origin.1 Ischemic and hemorrhagic strokes are the two major categories of strokes.1,2 The subtypes of ischemic infarct with the highest in-hospital mortality are cardio-embolic stroke and atherothrombotic stroke. Compared to other ischemic stroke subtypes, individuals with cardio-embolic stroke and atherothrombotic stroke have poor short-term prognoses.3
According to estimates, cardiovascular diseases (CVDs) are the largest cause of mortality in the world, accounting for around 32% of all fatalities in 2019. Deaths from heart attacks and strokes made up 85% of total mortality, with low- and middle-income nations accounting for more than three-quarters of these deaths (LMICs).4 The global epidemiology of stroke is changing rapidly.5 Stroke is the second most common cause of mortality for adults over 60 in the globe, after heart disease,6,7 and the fifth leading cause of death for people aged 15 to 59; account for 11.8% of all deaths.6
Every year, almost six million people worldwide die from a stroke. One in six people will suffer a stroke in their lifetime.7 Stroke patients under the age of 50 account for 5–10% of all strokes worldwide.8 In fact, it is the leading cause of acquired disabilities and the third leading cause of death in women worldwide.9 An estimated 17 million people worldwide have had a first-time stroke; one every two seconds and 62 million stroke survivors.10,11
The 2019 global burden of disease data showed that in 2010 in sub-Saharan Africa and LMICs, stroke was the leading cause of death and disability from cardiovascular disease.7,12–14 According to the 2018 WHO report covering all ages and genders, in Ethiopia, 39% of the total number of deaths were due to NCDs, and among these NCDs, cardiovascular diseases accounted for more than a third of the mortality.15 There is growing evidence for an increasing trend in the incidence of stroke in young adults.
Younger to middle-aged people were affected by stroke16,17 Ischemic, intracerebral hemorrhage, subarachnoid hemorrhage, and undetermined are the major risk factors for one-year mortality, with male gender, previous stroke, subarachnoid hemorrhage from atrial fibrillation, and in-hospital complications being associated with increased fatality at any time.17
Stroke prevalence in Africa is still relatively high, although little is known about the dynamics of stroke epidemiology among Africans.18 For instance, mortality following stroke by its main types in Ghana was 49.7%, 62.9%, and 73.7%, at 1, 5 and 8 years respectively. The Crude Death Rate (CDR) following intracranial hemorrhage was lower than the CDR following an ischemic stroke. Long-term determinants of death following a stroke in Ghana were increasing age, level of education, and stroke severity.19
Low-middle-income countries account for 87% of stroke-related disability and 70% of stroke-related deaths. Compared to Western Europe and the USA, stroke incidence and prevalence are 2–3 times higher in Africa. Over 80% more cases of fatalities in three years.20
Stroke in young adults is of particular concern in developing countries as it affects the most economically productive group in society,21 and even it is associated with higher mortality in this age group.22 In Ethiopia, cerebrovascular disease ranked first among the top ten causes of death from NCDs in both men and women, and ranked fifth in the total number of deaths in 2007. In 2017, it rose 8.35% to the top spot.23 Overall, stroke is one of the top devastating NCDs globally and the majority of the burden is targeted in developing countries.
About 8–12% of ischemic strokes are fatal compared to 37–38% of hemorrhagic strokes. It depends on the severity of the stroke, advanced age, comorbidities and the effectiveness of treating complications.24 In-hospital stroke mortality is 3–11% in developed countries compared to 7–15% in low- and middle-income countries.25 But in sub-Saharan Africa it is much more significant, three to four times higher than in developed countries, where it ranges from 11 to 43.4%.26
In Ethiopia, stroke prevalence was 19.3%; with ischemic stroke accounting for 51.2% of all cases and having a ratio of 1.36 to hemorrhagic stroke.27 The burden of stroke is increasing, accounting for 7.5% to 19.3% of hospital admissions and about 11% to 42.8% of deaths between 2014 and 2019.28 The stroke fatality rate in Ethiopia is 6.23% of all deaths and the age-adjusted stroke mortality rate in the country is 89.82 per 100,000 people.29 In the absence of a significant global public health response, the number of strokes is projected to increase to 23 million new cases and 7.8 million deaths per year by the end of 2030.30 Established risk factors include arterial hypertension, diabetes mellitus, cigarette smoking, hyperlipidemia, atrial fibrillation, micro-vascular rupture, male gender, age, obesity, excessive alcohol consumption, family history, drug use, ethnicity, and observed comorbidities such as sickle cell anemia, hypercoagulability, human immune viral infections, and cerebral malaria increasingly common in the tropics.29,31 Cerebrovascular stroke trends increase with age, and men are more affected than women. Hypertension is the most common risk factor and ischemic stroke is the most common type of stroke.32
Stroke is disabling for a long time if not treated promptly, and these patients usually require more extensive investigations to find the underlying cause of the condition. It is one of the most important life-threatening and serious medical emergencies that requires timely medical evaluation, diagnosis and treatment.33 And it is an emerging public health problem that is under-addressed. In the past, stroke was a disease affecting only wealthy countries, but it is now becoming a public health problem in developing countries as well. There is even evidence that the incidence and prevalence of stroke in Africa today may be up to two to three times higher compared to Western Europe and the United States of America.20 This has serious consequences for lost productivity, premature death and long-term disability.34
In Ethiopia, stroke is becoming an increasingly serious public health problem and there is limited data hindering the formulation of appropriate interventions to minimize the impact of stroke. Although the study was conducted five years ago on burden, clinical outcomes, and predictors of stroke in this study area, there is no more recent study on long-term survival and its predictors in adult stroke patients enrolled at Jimma University Medical Center. Therefore, the purpose of this study is to determine survival status and its predictors in adult stroke patients admitted to Jimma University Medical Center.
Methods
Study Setting, Design and Population
The study was conducted from May-June 2022 at the Jimma University Medical Center (JUMC) Stroke Unit. A retrospective follow-up study was conducted on selected adult stroke patients (age > 18 years) admitted to the stroke unit for a case of stroke by clinical imaging or brain imaging as per WHO diagnosis from April 1, 2017 to March 31, 2022.
Sample Size Determination and Sampling Techniques
The sample size was determined using significant variables from the different studies using STATA v.14.0, considering; 95% CI, Zα/2 = 1.96 and 80% power, probability of death 15%, AHR= 2, Variability of covariates of interest= 50%.28 We assumed that no subjects will be anticipated to withdraw from the follow-up. Finally, by adding 10% of contingency the minimum sample size for the study was 480. A sampling frame was prepared from the available medical record number of patients and simple random sampling by using computer-generated random numbers was used to select 480 adult stroke patients (Figure 1).
 |
Figure 1 Flow diagram of sampling procedure. |
Data Collection, Quality Control
The tools were adapted from the WHO guideline “Stepwise” and related studies,35,36 which included information on socio-demographic characteristics, patient baseline data, pre-existing risk factors for stroke, neurological factors, comorbidities, and discharge status data from patient medical records extract. Four BSc. Nurse with data registration experience and a second-year MPH student were assigned to data collection and the principal investigator as supervisor checked and guided the data collection process on a daily basis and missed data. Prior to data collection, data collectors were trained for two days on the content of the data abstraction checklist and the extraction of data from patient records. A week prior to the study, a pretest was performed on 5%24 patients of the sample size at JUMC in a similar study area to ensure availability of important variables and to make partial or full changes to questions affecting data consistency.
Operational Definitions
Survival status: Discharge status of adults’ stroke patients on discharge summary which can be either of “death” (1) or’ censored’ (0) Event: Adult stroke patient who died during treatment. Censored: An adult stroke patient whose discharge status is either alive at the end of the follow-up, lost to follow-up, withdrawn, or transferred to other health institutions without knowing the outcome status. Survival time: Calculated in completed days using the time between dates of admission and the date of the event (death) or date of censoring. Time to death: Time in days from the first date of admission to a stroke unit to the time of death of an adult stroke patient.
Atrial fibrillation: Had atrial fibrillation on ECG before stroke (records seen) or during hospitalization.36 Diabetes Mellitus: Defined as when the patient was taking any anti-diabetic medication or when a random blood sugar level of ≥ 200 mg/dl or two consecutive fasting venous plasma glucose levels of ≥ 126 mg/dl persists beyond the acute phase of stroke.37 Dyslipidemia: Defined as when the patient was taking lipid-lowering medications or a total cholesterol level ≥ 240 mg/dl.38,39 First-ever stroke: A stroke that occurred in persons who never had a stroke before.36 Recurrent stroke: is defined as a history of a previous stroke event at some time in the past that meets the WHO definition or a history of a new stroke event occurring more than 28 days after the onset of a stroke event already registered.36
Data Processing and Analysis
After collection, the data was checked for completeness and consistency and then entered into Epi-data v.3.1 and exported to STATA v.14.2 for data cleansing and exported to R v.14.2 for analysis. 4.2. The event of interest was coded as one (1) and censored as zero (0). The Kaplan-Meier curve is used to estimate survival time and to compare vulnerability rates between variables. Variables with p-value < 0.25 in the bivariable Cox proportional analysis were selected for the multivariable Cox proportional hazards analysis model to identify factors associated with outcome. In addition, the graphical evaluations were also carried out using Schoenfeld residual diagram and log-minus-log diagram. The overall goodness of fit of the model was assessed using the Cox-Snell residual plot. Finally, 95% CI of the hazard ratio with a corresponding p-value < 0.05 was established to indicate statistical significance.
Ethical Consideration
Ethical clearance reference number IHRPGD/855/22 was obtained from the Jimma University Institute of Health Ethical Review Board. A letter of approval to continue the study was obtained from the Chairman and Medical Director of Jimma University Medical Center and the Stroke Unit Coordinator. The data recorded from the patient file will be treated confidentially. Data extraction tools are coded in a way that excludes the display of names and other personal information. No reference is made in oral or written reports that could associate the participants with the study. The study was conducted in accordance with the principles set out in the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of Study Participants
There were 480 patients involved in the study. The mean age of the patients was 55.43±14.56 years. The mean age of patients who died was 55.11 ±15.36 years, and 55.51±14.40 years among those censored. The incidence of stroke was maximum, 224 (46.67%) in the age group of 45–65. Male comprised 299 (62.29%) with a male-to-female ratio of 1.65:1 (Table 1).
 |
Table 1 Socio-demographic and other related Characteristics of study participants |
Antecedent risk factors
In the study, 349 (72.71%) of the participants had a history of hypertension, while 94 (26.93%) were diagnosed with hypertension after admission for stroke. The mean duration of hypertension before stroke was 3 (IQR: 1–5) years. Of the 255 (73.07%) hypertensive patients with pre-existing hypertension, 98 (38.58%) were taking antihypertensive medication upon arrival at the hospital. In addition, 42 (8.75%) had diabetes (Table 2).
 |
Table 2 Antecedent risk factors of study participants |
Neurological Factors
In this study, 262 (54.58%) of the participants suffered an ischemic stroke. In addition, 244 (50.83) patients had a GCS score of 13–15. In addition, the median time between stroke onset and hospital arrival was 24 (IQR 11–48) hours. Four hundred sixty-three (96.46%) of the strokes were sudden. On the other hand, 423 (88.13%) had the first stroke episode and the remaining 57 (11.88%) had the underlying condition of a previous/recurrent stroke (Table 3).
 |
Table 3 Neurological Factors of Adult Stroke Patients Admitted to JUMC |
Stroke Event Factors
On admission, 319 (66.46%) of the stroke patients had a systolic blood pressure of 140 mmHg, while 299 (62.29%) of them had a diastolic blood pressure of 90 mmHg. In addition, 289 (66.90) had a serum creatinine of 0.6 to 1.2 with a mean serum creatinine of 0.86 (IQR = 0.69–1.08) (Table 4).
 |
Table 4 Stroke event factors among study participants |
Hospital Complications of a Stroke
Two hundred forty-two (50.40%) people had a stroke complication in the hospital. Among these complications, the most common were increased intracranial pressure, aspiration pneumonia, and urinary tract infection, which were diagnosed in 135 (28.13%), 127 (26.46%), and 46 (9.58%), respectively (Table 5).
 |
Table 5 Hospital Complications Among Adult Stroke Patients Admitted to JUMC |
Treatment Outcome
In the present study, 88 patients died on discharge from the hospital, representing an in-hospital mortality rate of 18.3%. The remainder were alive at discharge, with 319 (66.46%) being discharged on improvement and 9 (1.88%) going against medical advice at the request of the patient and/or the patient’s family (Figure 2).
 |
Figure 2 Treatment outcome of adult stroke patients admitted to JUMC. |
Kaplan Meier survival curve indicating survival time in days among admitted patients (Figure 3).
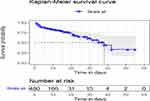 |
Figure 3 Overall survival probability of adult stroke patients admitted to JUMC. |
Kaplan Meier cumulative hazard curve indicating number of days at risk among admitted patients in JUMC (Figure 4).
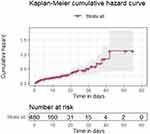 |
Figure 4 Cumulative Hazard of adult stroke patients admitted to JUMC. |
Predictors of Stroke
In the bi-variable Cox proportional hazards regression analysis, 14 variables (Glasgow coma scale at admission, aspiration pneumonia, type of stroke, atrial fibrillation, increased ICP, diabetes, vomiting, dyslipidemia, rheumatic valvular heart disease, seizure, the pulse rate and the respiration rate at hospital arrival, the presence of stroke complication, and patient’s age) were significant at p<0.25 and selected for multivariable cox proportional hazard model. In multivariable cox regression, only four variables were identified as the predictors of mortality: Glasgow coma scale≤8 (AHR=7.71), aspiration pneumonia (AHR=2.30), history of dyslipidemia (AHR=3.96) and increased ICP (AHR=4.27) (Table 6).
 |
Table 6 Bi-Variable and Multi-Variable Cox Proportional Hazard Model of Adult Stroke Patients Admitted to JUMC, from April 2017 to March 31/ 2022 |
Discussion
The incidence of stroke mortality is 20.23per 1000 person-days in this study. The median survival time was 38 days. GCS score ≤ 8, dyslipidemia, aspiration pneumonia, and increased intracranial pressure were predictors of mortality. The mean age at which stroke occurs were 55.43±14.56 years, which was comparable to study done in different parts of Ethiopia,35,40–43 which indicates that, stroke is the most common disease affecting elder population. After adjusting for potential confounders, stroke patients aged >65 years old had an 18% higher hazard of death compared to those aged less than 45 years, even though there was no statistically significant difference in overall survival time between the age groups. However, study carried out in Northwest Ethiopia found that age over 65years was independent predictor of death from stroke.28,41
In our study, hemorrhagic stroke accounted for 45.42% of stroke patients, which is in line with study done at Tikur Anbessa specialized Hospital,27 Dessie referral hospital,44 and Mekele Ayder referral hospital.35 However, it is less than study conducted in Addis Ababa and Nigeria.40,45 The sample size difference may be the reason for the discrepancy. However, the findings were higher than study conducted in Iran.46 The possible explanation could be due to the high magnitude of hypertension in Africa, and the majority of patients in our study (72.4%) were not adherent to their prescribed anti-hypertensive drugs, all of which contribute to the high incidence of hemorrhagic stroke. According to research done in Mekele, the cardio-embolic subtype for ischemic stroke was the most frequently detected,38 which is in line with our finding.
The present study revealed, 18.33% of patients died from stroke which is comparable to the proportion reported in other parts of Ethiopia;27,47 however, it is higher than study done at Debre Markos referral hospital and Ambo University referral hospital, 8.6%,16.2% respectively.48,49 However, it is lower when compared to study conducted in Felege Hiwot referral hospital (15.2%),28 Ayder hospital (12%)35 and Tikur Anbessa specialized hospital.40 Deviations in the sample size, the characteristics of the study population, the composition of the study population, the study design and the study areas can be the reason for deviations in the mortality proportions. On the other hand, it is lower than the study conducted in Democratic Republic of Congo and Uganda which were 31.7% and 31% respectively.50,51 The study in Congo was conducted at a multicenter, while the lower unit health facility may not have standard laboratory testing. This disparity in treatment facilities may be the possible cause of the discrepancy. On the other hand, the difference in study design, sample size and inclusion criteria could be the possible reason for being lower than the study conducted in Uganda. Furthermore, we found that the median survival time was 38 days, lower compared to the study conducted in northern Ethiopia which was 48 days.38 According to this study, the probability of survival at 7 days, 14 days, 30 days and 42 days was 85.2%, 79.5%, 60.8% and 32.7%, respectively. However, the 30-day survival probability is slightly lower than in previous studies.38,43 A study in southern Nigeria reported that the case fatality rate at 7 days, 14 days, and 30 days was 22.2%, 25.5%, and 30.8%; which is higher for 7 days and 14 days and lower for 30 days.45
In this study, we found no significant difference in survival time between male and female, which is in line with previous studies conducted in Ethiopia.28,38 Furthermore, we found that there was no significant difference in survival time between hemorrhagic and ischemic types of stroke and this finding is in line with previous studies done in Ethiopia.38
At a given instant of time during the follow-up period, stroke patients who had a GCS score of ≤ 8 were 7.71 times more likely to die as compared to those with a GCS score of 13–15, adjusting for other variables. This finding is consistent with study conducted in other parts of Ethiopia,28,38 Nigeria,52 Sierra Leone53 and Uganda.50 Patients with poor GCS scores are more likely to die, typically because of complications such as aspiration pneumonia and intracranial pressure. This might imply that, patients with poor GCS scores require more immediate care and managing of underlying complications.
At any particular point in time during the follow-up period, the hazard of death among adult stroke patients who had aspiration pneumonia complications was 2.3 times higher than those who had no it. Which is in line with a study on tertiary referral in the east of England and Sierra Leon.50,54 Stroke patients with aspiration pneumonia are usually at increased risk of respiratory infection. This might imply that stroke patients with a history of dysphagia need close follow-up.
Moreover, it was identified that an adult stroke patient with a history of dyslipidemia died at hazard ratio of 3.96 times at all follow-up periods as compared to those who did not have, which is consistent with the study conducted in Mekele,38 which shows there is a significant difference in survival time of patients who had borderline cholesterol had four times higher risk of death compared to with normal cholesterol level.
At any particular time during the follow-up period, the hazard of death among patients having the complication of raised intracranial pressure was 4.27 times higher than those who did not. Increased intracranial pressure increases the hazard of death of stroke patients mainly since it results in lower cerebral perfusion pressure, cerebral ischemia, herniation of brain stem, and other important structures. Therefore, stoke patients with elevated ICP must be recognized as soon as possible to monitor it and should begin therapies early.
In our study, there is no statistically significant difference in survival time among types of stroke. However, the hazard of death among hemorrhagic stroke patients is 15% lower than patients who had an ischemic stroke, which agree with study done in Ethiopia,38 Kazakhstan.55
Limitations of the Study
It is a referral hospital-based study rather than a population-based study, thus selection (referral bias) may occur because severe cases may have died before reaching the hospital or mild cases may have not reported to the hospital, it focused on all ischemic and intra cerebral hemorrhage but there may be difference between lacunar and non-lacunar stroke, because the pathophysiology, prognosis and clinical features of lacunar strokes are different from other acute cerebrovascular diseases.56
Conclusion and Recommendations
The mortality rate in adult stroke patients enrolled in JUMC was higher in the first and second weeks than in the previous studies. A GCS score ≤8, increased intracranial pressure, history of dyslipidemia, and aspiration pneumonia were independent predictors of stroke mortality. Therefore, careful follow-up and early detection of stroke complications is recommended in unconscious patients. In addition, policymakers and affected bodies should develop appropriate strategies to counteract the changeable risk factors. We recommend that, prospective cohort study by taking in to consideration other classification of stroke for future researchers.
Abbreviations
AHR, Adjusted Hazard Ratio; BSc, Bachelor of Science; CVDs, Cardio-Vascular Disease; ECG, Electrocardiography; GCS, Glasgow Coma Scale; LMICs, Low and Middle-Income Countries; NCDs, Non-Communicable Diseases.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author on a reasonable request.
Acknowledgments
We are grateful to Jimma Medical Health Center, Medical ward coordinator and data collectors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare there is no conflict of interest in this work.
References
1. The National Collaborating Centre for Chronic Conditions. Stroke: National Clinical Guideline for Diagnosis and Initial Treatment of Acute Stroke and Transient Ischaemic (TIA). Royal College of Physicians; 2008.
2. Public Health England. Technical Document: First Incidence of Stroke Estimates for England 2007 to 2016 About Public Health England; 2016.
3. Arboix A, Oliveres M, Massons J, Pujades R, Garcia-Eroles L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: a multivariate analysis. Eur J Neurol [Internet]. 1999;6(6):677–83. doi:10.1046/j.1468-1331.1999.660677.x
4. Cardiovascular diseases (CVDs); 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
5. Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology. 2015;45(3):161–176. doi:10.1159/000441085
6. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation. 2016;133:38–48.
7. Patne S, Chintale K. Study of clinical profile of stroke patients in rural tertiary health care centre. Int J Adv Med. 2016;3(3):666–670. doi:10.18203/2349-3933.ijam20162514
8. Tan KS, Navarro JC, Wong KS, et al. Clinical profile, risk factors and aetiology of young ischaemic stroke patients in Asia: a prospective, multicentre, observational, hospital-based study in eight cities. Neurol Asia. 2014;19(2):117–127.
9. Manorenj S, Inturi S, Jyotsna B, Savya V, Areli D, Reddy B. Prevalence, pattern, risk factors and outcome of stroke in women: a clinical study of 100 cases from a tertiary care center in South India. Int J Res Med Sci. 2016;4(6):2388–2393. doi:10.18203/2320-6012.ijrms20161819
10. Rutten-Jacobs LCA, Arntz RM, Maaijwee NAM, et al. Long-term mortality after stroke among adults aged 18 to 50 years. JAMA. 2013;309(11):1136–1144. doi:10.1001/jama.2013.842
11. Seymour M. State of the nation state, Stroke statistics. Stroke Associaton. 2016;1–441. Available from: stroke.org.uk.
12. Alemayehu CM. Assessment of stroke patients: occurrence of unusually high number of haemorrhagic stroke cases in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Clin Med Res. 2013;2(5):94. doi:10.11648/j.cmr.20130205.11
13. Yamasaki, NIH Public Access. Bone; 2014. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf.
14. Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222.
15. Damasceno A. Noncommunicable Disease. Heart of Africa: Clinical Profile of an Evolving Burden of Heart Disease in Africa. John Wiley & Sons; 2016.
16. Sarfo FS, Ovbiagele B. Key determinants of long-term post-stroke mortality in Ghana. J Neurol Sci. 2022;2022:434.
17. Youkee D, Deen G, Baldeh M, et al. Stroke in Sierra Leone: case fatality rate and functional outcome after stroke in Freetown. Int J Stroke. 2023;18(6):174749302311648. doi:10.1177/17474930231164892
18. Okekunle AP, Jones S, Adeniji O, et al. Stroke in Africa: a systematic review and meta-analysis of the incidence and case-fatality rates. Int J Stroke. 2023;18:634–644. doi:10.1177/17474930221147164
19. Sarfo FS, Akassi J, Ofori E, Ovbiagele B. Long-term determinants of death after stroke in Ghana: analysis by stroke types & subtypes. J Stroke Cerebrovasc Dis. 2022;31(9):106639. doi:10.1016/j.jstrokecerebrovasdis.2022.106639
20. Akinyemi RO, Ovbiagele B, Adeniji OA, et al. Stroke in Africa: profile, progress, prospects and priorities. Nat Rev Neurol. 2021;17(10):634–656. doi:10.1038/s41582-021-00542-4
21. Pandit A, Dash D, Bhashin A, et al. Risk factors and etiologies of ischemic strokes in young patients: a tertiary hospital study in North India. J Stroke. 2014;16(3):173. doi:10.5853/jos.2014.16.3.173
22. Thrift AG, Cadilhac DA, Thayabaranathan T, et al. Global stroke statistics. Int J Stroke. 2014;9(1):6–18. doi:10.1111/ijs.12245
23. Fenta EH, Sisay BG, Gebreyesus SH, Endris BS. Trends and causes of adult mortality from 2007 to 2017 using verbal autopsy method, Addis Ababa, Ethiopia. BMJ Open. 2021;11(11):1–8. doi:10.1136/bmjopen-2020-047095
24. Balami JS, Chen RL, Grunwald IQ, Buchan AM. Neurological complications of acute ischaemic stroke. Lancet Neurol. 2011;10(4):357–371. doi:10.1016/S1474-4422(10)70313-6
25. Koennecke HC, Belz W, Berfelde D, et al. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology. 2011;77(10):965–972. doi:10.1212/WNL.0b013e31822dc795
26. Getachew Erkabu S, Agedie Y, Mihretu DD, Semere A, Alemu YM. Ischemic and hemorrhagic stroke in Bahir Dar, Ethiopia: a retrospective hospital-based study. J Stroke Cerebrovasc Dis. 2018;27(6):1533–1538. doi:10.1016/j.jstrokecerebrovasdis.2017.12.050
27. Kassaw Asres A, Cherie A, Bedada T, Gebrekidan H. Frequency, nursing managements and stroke patients’ outcomes among patients admitted to Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia a retrospective, institution based cross-sectional study. Int J Africa Nurs Sci. 2020;13(October 2019):100228.
28. Walelgn N, Abyu GY, Seyoum Y, Habtegiorgis SD, Birhanu MY. The survival status and predictors of mortality among stroke patients at north west Ethiopia. Risk Manag Healthc Policy. 2021;14:2983–2994. doi:10.2147/RMHP.S322001
29. Abate TW, Zeleke B, Genanew A, Abate BW. The burden of stroke and modifiable risk factors in Ethiopia: a systemic review and meta-analysis. PLoS One. 2021;16(November):1–19. doi:10.1371/journal.pone.0259244
30. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–187. doi:10.1016/S1474-4422(07)70031-5
31. Kuriakose C, Naseem Shifafiya M, Tharakan NS, Sattanathan K, Sambath Kumar R. A prospective study of clinical profile of stroke in a tertiary care hospital. Asian J Pharm Clin Res. 2016;9:178–181. doi:10.22159/ajpcr.2016.v9s3.13622
32. Umakanth M. Clinical profile of stroke-study conducted in the Batticaloa teaching hospital, Sri Lanka. J Biosci Med. 2018;6(6):1–6.
33. Green TL, McNair ND, Hinkle JL, et al. Care of the patient with acute ischemic stroke (Posthyperacute and prehospital discharge): update to 2009 comprehensive nursing care scientific statement: a scientific statement from the American Heart Association. Stroke. 2021;52:E179–97. doi:10.1161/STR.0000000000000357
34. Kalkonde YV, Alladi S, Kaul S, Hachinski V. Europe PMC funders group stroke prevention strategies in the developing world. Stroke. 2018;49(12):3092–3097. doi:10.1161/STROKEAHA.118.017384
35. Gebremariam SA, Yang HS. Types, risk profiles, and outcomes of stroke patients in a tertiary teaching hospital in northern Ethiopia. eNeurologicalSci. 2016;3:41–47. doi:10.1016/j.ensci.2016.02.010
36. World Health Organization. The WHO STEPwise approach to stroke surveillance. World Health Organization; 2006. Available from: http://www.who.int/chp/steps/Stroke/en/.
37. Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. doi:10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
38. Gufue ZH, Gizaw NF, Ayele W, et al. Survival of stroke patients according to hypertension status in Northern Ethiopia: seven years retrospective cohort study. Vasc Health Risk Manag. 2020;16:389–401. doi:10.2147/VHRM.S247667
39. Cocho D, Yarleque S, Boltes A, et al. Clinical outcome of ischemic stroke in old patients versus oldest-old. J Stroke Cerebrovasc Dis. 2018;27(12):3657–3661. doi:10.1016/j.jstrokecerebrovasdis.2018.08.041
40. Gedefa B, Menna T, Berhe T, Abera H. Assessment of risk factors and treatment outcome of stroke admissions at St. Paul’s teaching hospital, Addis Ababa, Ethiopia. J Neurol Neurophysiol. 2017;08(3):6–11. doi:10.4172/2155-9562.1000431
41. Kassie A, Ayalew S, Abere M. Survival time of adult ischemic stroke patients and associated risk factors: a retrospective cohort study at felege hiwot referral hospital. Asian J Med Res. 2019;8(4):ME29–35. doi:10.21276/ajmr.2019.8.4.ME5
42. Kefale B, Ewunetei A, Molla M, Tegegne GT, Degu A. Clinical pattern and predictors of stroke treatment outcome among hospitalised patients who had a stroke at Felege Hiwot comprehensive specialised hospital, northwest Ethiopia: a retrospective cross-sectional study. BMJ Open. 2020;10(12):1–10. doi:10.1136/bmjopen-2020-040238
43. Fekadu G, Chelkeba L, Kebede A. Burden, clinical outcomes and predictors of time to in hospital mortality among adult patients admitted to stroke unit of Jimma University medical center: a prospective cohort study. BMC Neurol. 2019;19(1):1–10. doi:10.1186/s12883-018-1232-z
44. Abdu H, Tadese F, Seyoum G. Comparison of ischemic and hemorrhagic stroke in the medical ward of Dessie referral hospital, Northeast Ethiopia: a retrospective study. Neurol Res Int. 2021;2021. doi:10.1155/2021/9996958
45. Kayode-Iyasere E, Odiase FE. A seven-year retrospective review of stroke admissions in Benin-City, Southern Nigeria. Ann Heal Res. 2019;5(1):11–19. doi:10.30442/ahr.0501-2-32
46. Habibi-Koolaee M, Shahmoradi L, Niakan Kalhori SR, Ghannadan H, Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in Gorgan: a retrospective hospital-based study – 2015–2016. Neurol Res Int. 2018;2018. doi:10.1155/2018/2709654
47. Alene M, Assemie MA, Yismaw L, Ketema DB. Magnitude of risk factors and in-hospital mortality of stroke in Ethiopia: a systematic review and meta-analysis. BMC Neurol. 2020;20(1):1–10. doi:10.1186/s12883-020-01870-6
48. Mulugeta H, Yehuala A, Haile D, et al. Magnitude, risk factors and outcomes of stroke at Debre Markos referral hospital, Northwest Ethiopia: a retrospective observational study. Egypt J Neurol Psychiatry Neurosurg. 2020;56(1). doi:10.1186/s41983-020-00173-4
49. Gadisa DA, Busawa GB, Gebremariam ET, et al. Clinical characteristics, treatment outcomes, and its predictors among hospitalized stroke patients in Ambo University Referral Hospital, West Ethiopia: a retrospective hospital-based study. Vasc Health Risk Manag. 2020;16:591–604. doi:10.2147/VHRM.S287465
50. Namale G, Kamacooko O, Makhoba A, et al. Predictors of 30-day and 90-day mortality among hemorrhagic and ischemic stroke patients in urban Uganda: a prospective hospital-based cohort study. BMC Cardiovasc Disord. 2020;20(1):1–11. doi:10.1186/s12872-020-01724-6
51. Kamabu L, Lekuya HM, Muhindo Kasusula B, et al. Risk factors of mortality among patients with stroke in eastern region of the Democratic Republic of Congo: a retrospective series study. Pamj-Cm. 2020;4(123):1–11.
52. Oyemomi A, Muftau O, Anthony T, Olowoyo P. African journal of emergency medicine five-year analysis of clinical presentations and predictors of stroke mortality in rural Southwestern Nigeria: a retrospective observational study. African J Emerg Med. 2022;12(1):12–18. doi:10.1016/j.afjem.2021.10.005
53. Russell JBWW, Charles E, Conteh V, Lisk DR. Risk factors, clinical outcomes and predictors of stroke mortality in Sierra Leoneans: a retrospective hospital cohort study. Ann Med Surg. 2020;60(November):293–300. doi:10.1016/j.amsu.2020.10.060
54. Teh WH, Smith CJ, Barlas RS, et al. Impact of stroke-associated pneumonia on mortality, length of hospitalization, and functional outcome. Acta Neurol Scand. 2018;138(4):293–300. doi:10.1111/ane.12956
55. Viderman D, Issanov A, Temirov T, Goligher E, la Fleur P. Outcome predictors of stroke mortality in the neurocritical care unit. Front Neurol. 2020;11(December):1–7. doi:10.3389/fneur.2020.579733
56. Rudilosso S, Rodríguez-Vázquez A, Urra X, Arboix A. The potential impact of neuroimaging and translational research on the clinical management of lacunar stroke. Int J Mol Sci. 2022;23(3):1497. doi:10.3390/ijms23031497
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
