Back to Journals » Clinical Epidemiology » Volume 12
Survival, Prevalence, Progression and Repair of Abdominal Aortic Aneurysms: Results from Three Randomised Controlled Screening Trials Over Three Decades
Authors Lindholt JS , Diederichsen AC , Rasmussen LM, Frost L , Steffensen FH, Lambrechtsen J, Urbonaviciene G, Busk M, Egstrup K, Kristensen KL , Behr Andersen C, Søgaard R
Received 13 November 2019
Accepted for publication 10 January 2020
Published 23 January 2020 Volume 2020:12 Pages 95—103
DOI https://doi.org/10.2147/CLEP.S238502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eyal Cohen
Jes S Lindholt, 1–3 Axel C Diederichsen, 2, 4 Lars M Rasmussen, 2, 5 Lars Frost, 6, 7 Flemming H Steffensen, 8 Jess Lambrechtsen, 8 Grazina Urbonaviciene, 6, 7 Martin Busk, 9 Kenneth Egstrup, 8 Katrine L Kristensen, 1–3 Carsten Behr Andersen, 3 Rikke Søgaard 10
1Department of Cardiothoracic and Vascular Surgery, Odense University Hospital, Odense, Denmark; 2Elitary Centre for Individualized Medicine in Arterial Diseases (CIMA), Odense, Denmark; 3Department of Vascular Surgery, Viborg Hospital, Viborg, Denmark; 4Department of Cardiology, Odense University Hospital, Odense, Denmark; 5Department of Clinical Biochemistry and Pharmacology, Odense University Hospital, Odense, Denmark; 6Department of Cardiology, Diagnostic Centre, Regional Hospital Silkeborg, Silkeborg, Denmark; 7Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 8Department of Cardiology, Vejle Hospital, Vejle, Denmark; 9Department of Cardiology, University Hospital Odense Svendborg, Svendborg, Denmark; 10Department of Public Health and Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Correspondence: Jes S Lindholt
Department of Cardiothoracic and Vascular Surgery, Odense University Hospital, J.B. Winsløv Vej 4, Odense 5000, Denmark
Tel +45 2464 1214
Email [email protected]
Aim: The prevalence and mortality of abdominal aortic aneurysms (AAA) has been reported to decline. The aim of this study is to compare survival, prevalence, and repair rate of AAA in Denmark in the 1990s, the 2000s and the 2010s – and to examine any change in factors known to influence the prevalence.
Methods: Baseline status and up to 5-year outcomes of 34,079 general population men aged 65– 74 were obtained from three RCTs; the Viborg study (1994– 1998, n=4,860), the Viborg Vascular (VIVA) trial (2008– 2011, n=18,748), and the Danish Cardiovascular (DANCAVAS) trial (2015– 2018, n=10,471). After the millennium (VIVA and DANCAVAS) men with AAA were further offered low dose aspirin and statins. Follow-up data were not available for the DANCAVAS trial yet.
Results: Across the three decades, the AAA prevalence was 3.8% (Reference), 3.3% (p< 0.001) and 4.2% (p=0.882), the proportion of smokers were 62%, 42% and 34% (p< 0.001) amongst men with AAA, but AAA risk associations with smoking increased during the decades suggesting increased tobacco consumption of smokers. In addition, the proportions of attenders with ischemic heart disease or stroke increased significantly. The aneurysmal progression rate in the 1990s was 2.90 vs 2.98 mm/year in the 2000s (p=0.91). The need for preventive AAA repair increased insignificantly in the 2000s (Age adj. HR= 1.29, 95% C.I.: 0.95; 1.71, p=0.10), and mortality of men with screen-detected AAA was lower in the 2000s compared to the 1990s (Age-adj. HR= 0.28, 95% C.I.: 0.22; 0.36, p< 0.001).
Conclusion: The Danish prevalence of AAA today compares to the nineties. Unchanged aneurysmal progression rates combined with improved survival of men at risk of AAA leave them in longer time to develop an AAA, be diagnosed and to need later aneurysmal repair or experience rupture.
Clinical Trial Registrations: Viborg study: No possibility of registration in the nineties. VIVA: NCT00662480, URL: https://clinicaltrials.gov/show/NCT00662480, DANCAVAS: ISRCTN12157806, URL: http://www.isrctn.com/ISRCTN12157806.
Keywords: abdominal aortic aneurysms, screening, prevalence, survival, progression, smoking
Introduction
After an epidemic rise in mortality of abdominal aortic aneurysm (AAA) during the 1980s and early 1990s, reports from Sweden, UK and the US reported declining prevalence and AAA-specific mortality after the millennium.1–3 Actually, the decline was reported shortly after the first implementations of general population screening programs for men in Sweden, UK and US, while other countries now halt back a decision about general population screening, because the continued decrease in prevalence of AAA may tip the balance between harm and benefit.4,5 However, at the same time, evidence on the value of screening to citizens emerge and show that informed individuals are able to reflect on the participation decision if given a choice. When asked to weigh the potential health benefit against potential harms of overtreatment and later regret of the participation decision, individuals valued the benefit >10 times higher than the harm.6
The cause of the decrease in AAA prevalence has mainly been explained as monofactorial - a simple and logic consequence of reduced smoking in the Western World.7 Epidemiological trends are, however, very seldom monofactorially driven. Although reduced smoking could be a partly explaining factor, the developed societies, health care systems and technologies have changed; the prehospital emergency services have been greatly improved with increasingly faster and better supported transfer of emergencies to hospitals, where modern, sophisticated, high-tech imaging secures fast and valid diagnoses followed by much better outcomes of emergency procedures. Furthermore, focus on AAA combined with easier access to detection has caused a much higher incidental detection of AAA. A modern Danish model on screening for AAA estimated that the annual probability of a large AAA being incidentally detected is around 15% compared to only 3% in the 1990s.8 This combined with the introduction of endovascular aneurysm repair (EVAR) and much better outcomes of preventive repair has caused a constant increase in preventive, elective procedures.9 Altogether, these factors suggest that the observed decrease in AAA-specific mortality is hardly attributable to lower prevalence and reduced smoking alone.
In Denmark, three randomised controlled trials on the efficacy of screening for AAA have been conducted by the same principal investigator since 1994 using high-quality equipment and uniform standardized screening and surveillance methods allowing for comparison of risk factors and outcomes across three decades. Consequently, the aim of this study is to compare the survival, prevalence, and repair rate of AAA across three decades – the 1990s, the 2000s and the 2010s – and to explain any change by trends in factors known to influence the prevalence of AAA: smoking, predisposing comorbidity, aneurysmal growth, need for aneurysm repair, and survival of men with AAA.9
Materials and Methods
Attenders to three randomised screening trials for AAA of men aged 65–74; the Viborg study from the 1990s (n=4,816), The VIVA trial from the 2000s (n=18,710) and the DANCAVAS trial from the 2010s (n=10,471)
In the Viborg and VIVA trials, all men aged 65–74 years, and living in the county of Viborg during 1994–98 or in the Central Denmark Region during 2008–2011, were randomised 1:1 without exclusion criteria to be invited to screening for AAA by abdominal aortic ultrasound (US) scanning at the nearest hospital by special trained mobile screening teams consisting of nurses.10,11
Maximal infrarenal anterior-posterior aortic were measured in the peak of the systole at the widest diameter in case of a dilatation, and if not, just above the bifurcation. This method for assessing has proven to be very reproducible with high observer agreement.12,13
Men with an AAA above 50 mm were referred for vascular evaluation, while those below 50 mm were followed by annual control scans to check for progression to operation-recommendable sizes. The annual growth rates were calculated by individual linear regression analysis of the observed AP diameters during observation time.
In the DANCAVAS trial, 65–74-year-old men living in on the island of Funen or in the municipalities of Kolding, Fredericia, Vejle, Silkeborg and Ikast-Brande were randomised 2:1 as controls or for invitation to ECG gated truncal non-contrast CT scanning for quantification of coronary calcification and screening for aneurysms causing the infrarenal aorta examined in the end diastole performed and measured by specially trained radiographers. This method has been validated and found in agreement with the above mentioned US-based method, probably due to measurement in the end-diastolic phase.14,15
In all three trials, non-responders were reinvited once. In the VIVA and DANCAVAS trials, the additional screening offers were performed at the same time as the AAA screening.
In the Viborg study and the DANCAVAS trial, transverse aortic diameters ≥30 mm were also considered as AAA, while in VIVA it was only AP diameters, so this paper only deals with those having an AP diameter ≥30 mm. A maximal infrarenal anterior-posterior aortic diameter ≥30 mm was used to define an AAA in all three trials. In the Viborg and VIVA trials, people with an aortic diameter between 30–49 mm were offered annual surveillance while people with an aortic diameter ≥50 mm were referred to CT scan and assessment of indication for elective surgery. In the DANCAVAS trial, similar regimes were offered but the threshold for referral to vascular surgeons for assessment of indication for elective surgery was increased to 55 mm.
No further preventive actions were offered in the Viborg study, while positive findings in the VIVA and DANCAVAS trials were prescribed with statins and low dose aspirin, if not already initiated or contraindicated. In addition, active smokers with positive findings in the VIVA trial were offered assistance to quit smoking.10,11,14
All attenders to the VIVA and DANCAVAS trials fulfilled a similar health questionnaire including smoking habits, while this was only the case for positive findings in the Viborg trial. The used proportion of smokers among attenders was based upon a study of age and sex-stratified proportions of smokers in Denmark in the 1990s.16
Hypertension was self-reported in all trials, and comorbidities were register-based regarding the Viborg Study and VIVA as any hospital admission during the last ten years prior to randomisation, while comorbidities were self-reported in DANCAVAS. Outcome data concerning aneurysmal repair and overall mortality after five years were obtained from national health registers, and only available for the Viborg Study and VIVA trial.
Written informed consent was collected at entrance to the studies, which were conducted in agreement with the Helsinki Declaration, and approved by the relevant ethical committees: The Viborg Study (The Scientific Ethical Committee of the Counties of Northern Jutland and Viborg, 2-16-41-2-90), the VIVA trial (The Scientific Ethical Committee of the Mid Region of Denmark, M20080028), and DANCAVAS (The Scientific Ethical Committee of Southern Denmark, S20140069), and data protection authorities.
Statistical Analysis
Baseline characteristics are reported as frequencies (%) with 95% confidence intervals (CI) and means with standard deviations (SD), and compared by chi square test for categorical variables, and ANOVA for continuous variables.
Comparisons among the trials were adjusted for age as the selection to the Viborg Study differed slightly from the two other trials as 74-year-old men were not invited. To test for differences in prevalences in AAA, logistic regression was used using the trial from 90s as the reference with adjustment for age. A subgroup analysis regarding 65-year-old men was performed, as this group is the potential target for screening.
Odds ratios for having an AAA in all three decades were calculated regarding ever vs never-smokers, current smokers vs never smokers, and ex-smokers vs never smokers.
To test for differences in the growth rate over the decades, individual linear regression was used to estimate the individual growth rate and thus taking into account that different numbers of observations and different intervals between observations were present.
Differences in growth rate over the decades were examined univariately by unpaired t-test.
Cox regression analysis adjusted for age was used to compare the need for aneurysmal repair and overall survival of AAA detected men over the decades as well. In addition, cox regression analyses adjusted for age were performed to compare mortality of AAA detected men with attending men without AAA across the decades.
As sensitivity analysis, we estimated subhazard ratios with 95% CI using competing risk regression regarding repair rate as death is an obvious competing risk. This method was chosen to account for informative censoring during the long follow-up of this study. Time was measured from baseline screening until a participant underwent surgery, died or end of follow-up, whichever came first. We adjusted for age as in the main analysis.
Corresponding author had full access to all the data in the study and takes responsibility for its integrity and the data analyses.
Results
In all, 110,117 were randomised of which 48,179 were invited to screening and 34,079 (71%) attended. Attendance rates varied from 4,860 out of 6333 (77%) in the 1990s, 18,710 out of 25,076 (74%) in the 2000s and 10,471 out of 16,768 (62%) in the 2010s. The mean ages were 67.3, 69.0 and 69.0, respectively (p<0.001).
Trends in Demographic Characteristics and Risk Factors
The prevalence of acute myocardial infarction (AMI) remained unchanged through the three decades, but the proportion of angina pectoris or stroke at baseline increased significantly. In all, the proportion having had some manifestation of occlusive cardiovascular disease increased (Table 1).
 |
Table 1 Risk Factors and Comorbidities in Screened General Population Men Across Decades: Prevalence in All Attenders and Attenders with a Positive Test for Abdominal Aortic Aneurysm |
Height, body mass index (BMI) and lowest measured ankle-brachial blood pressure index (ABI) increased significantly, while systolic and diastolic blood pressure decreased significantly in accordance with significantly more using antihypertensive therapy in the last trial. Use of low dose aspirin decreased, while use of statins was unchanged in general and among those having an AAA diagnosed (Table 1).
We do not have population-based trial data regarding smoking habits from the 1990s, but assumable 41% were active smokers,15 in the 2000s were 21% of the attenders active smokers, and 15% in the 2010s (p<0.001). Regarding those with a positive AAA finding, 62%, 42% and 34% were active smokers in 1990s, 2000s and 2010s (p<0.001), respectively.
Odds ratios for having an AAA in all three decades regarding ever vs never-smokers, current smokers vs never smokers, and ex-smokers vs never smokers were all significant, and increased during the decades (Table 2).
 |
Table 2 Association Between Smoking Status (%) and AAA |
Prevalence of Abdominal Aortic Aneurysms
The AAA prevalence stratified by age and decade of study is shown in Table 3 and illustrated in Figure 1. The prevalence of AAA was 3.8%, 3.3% and 4.2%, respectively. Adjusted for age at randomisation and using the 1990s as reference, 2000s had significantly lower risk of AAA (age adj. OR= 0.76, 95% CI: 0.64; 0.90, p<0.001), while the 2010s had equal risk of AAA compared to the 90s (age adj. OR=0.99, 95% CI: 0.82; 1.19, p=0.882) (Table 3).
 |
Table 3 Age-Stratified Prevalence of Abdominal Aortic Aneurysms (n and %) and Overall Time Trends Across Decades (Odds Ratios with 95% Confidence Intervals) |
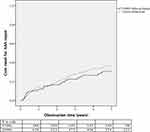 |
Figure 1 Five-year cumulative aneurysmal repair for men with screen-detected abdominal aortic aneurysm in the 1990s versus the 2000s (Age adj. HR = 1.29, 95% C.I.: 0.95; 1.71, p=0.10). |
Regarding the subgroup of men aged 65, the prevalence of AAA was 3.4% in the 1990s, 2.6% in the 2000s and 2.9% in the 2010s, respectively (p=0.334).
Aneurysmal Growth Rate and Need for Surgical Repair
This change in smoking habits and the intention to motivate current smokers to stop smoking in the VIVA trial from the 2000s together with other general cardiovascular preventive actions as statin and low dose aspirin medication and antihypertensive treatment ought to influence aneurysmal growth, but the mean annual aneurysmal growth rate appeared to be unchanged from 2.90 ± 2.57 mm/year in the 1990s to 2.98 ±2.57 mm/year in the 2000s (p=0.91).
The need for aneurysmal repair increased insignificantly by almost 30% in the 2000s compared to the 1990s regardless of the indication threshold having been increased from 5.0 cm to 5.5 cm (HR= 1.29, 95% C.I.: 0.95; 1.71, p=0.10), Figure 1. When competing risk analysis was performed, the insignificant increased risk of needing aneurysmal repair in the 2000s compared to the 1990s was sustained (age-adj SHR: 1.30, 95% CI: 0.94; 1.80, p=0.115).
Overall Survival
In the 1990s, the age-adjusted five-year mortality hazard among subjects screened positive for AAA was almost twice as high compared to the other attenders (Age adj. HR=1.88, 95% CI: 1.57; 2.24, p<0.001). In the 2000s, this risk was almost 2.5-fold increased (Age adj. HR=2.40, 95% CI: 2.02; 2.86, p<0.001). However, comparing survival of those detected with an AAA in the 1990s and the 2000s, the age-adjusted five-year mortality hazard was 72% lower in the 2000s (Age-adj. HR= 0.277, 95% C.I.: 0.215; 0.356, p<0.001) (Figure 2).
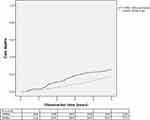 |
Figure 2 Five-year mortality of men detected with abdominal aortic aneurysm in the 1990s versus the 2000s regarding overall mortality (Age-adjusted HR= 0.277, 95% C.I.: 0.215; 0.356, p<0.001). |
Discussion
This comparison of the three Danish RCTs including AAA screening through three decades demonstrated no decline in AAA prevalence – rather a paradoxical sustained prevalence after a small decline in the 2000s. Paradoxical as we all expected the prevalence to decline. However, prevalence is a function of incidence and living years, and substantially improved survival was observed and could be explained by the decreased smoking rates and modern pharmacological prophylaxis with statins and low dose aspirin. However, smoking cessation and modern cardiovascular pharmacological prevention did not inhibit aneurysmal growth rates. The unchanged aneurysmal progression rates and longer survival could explain the sustained prevalence of AAA and although insignificant, 30% increased need for elective repair, the latter combined with better outcomes of surgical repair allows patients with more comorbidity to be treated – particularly after the introduction of EVAR.17,18 The 1990s used a 50-mm threshold, as it took place before the UKSAT trial and ADAM study defined the current threshold at 55 mm. In the 2000s, they were referred for CT scanning and vascular evaluation when it was or became more than 50 mm. Some may have been offered repair before 55 mm; we don´t have data access to that, but still, the general lower threshold in the 1990s is a bias towards no change in repair rate. The opposite could be possible regarding no repair as EVAR has been introduced, and operative results improved. However, in the 1900s, 16.4% referred for surgery weren´t repaired, while it also was 15.2% in the 2000s regarding those above 55 mm.
Our observation of sustained AAA prevalence is in contrast to other reports.1–3 Synchronously with the reports on declining AAA-specific mortality, nationwide screening programmes of 65-year-old men have been implemented in Sweden, UK, and the USA all reporting a much lower prevalence than observed in the screening studies from the 90s.1–3 However, age is a very strong risk factor for AAA, and the screening studies from the 1990s enrolled men aged 65–74 years. Only in the Gloucestershire screening trial, the prevalence of AAA has been described solely for 65-year-old men since the 1990s and reported to be declining.19 Again, it can be questioned whether this could be partly explained by technology development. The B-mode imaging quality of ultrasound (US) scanners has taken a dramatic rise in quality since the first generations in the late eighties and early nineties – it was especially difficult to define the posterior aortic wall in absence of calcifications, which without doubt has triggered measurements on the longitudinal anterior ligament of the vertebra causing substantial overdiagnosing. Finally, the proportion being diagnosed incidentally has increased substantially, and it is likely that those with a known AAA would not attend a screening programme for something already detected as they would not gain any benefit of it. The VIVA and DANCAVAS trials offered additional screening offers, which could have attracted more men with an AAA to attend.
The present observations in this study are based upon studies conducted with several strengths; they are population-based with high attendance rates minimising the risk of selection bias, the Viborg and VIVA trial used exactly the same method for detection and surveillance of AAA minimising the risk of information bias between these two trials, and all three trials included the same gender and age-group minimising the risk of confounding. However, it also carries some limitations; the examined geographically areas were not exactly the same, and local differences may exist. In addition, the improvement of US scanners between the Viborg study and the VIVA study could have produced more reliable AAA diagnoses in the VIVA trial, and in the Viborg Study, the transverse aortic diameter was also measured, so the measurements were performed in the axial plane, which risks lack of right-angled measurements compared to VIVA, which only used the longitudinal plane. Such information bias would be towards the null hypothesis that the prevalence was declining, which was seen between the Viborg study and the VIVA trial.
Ultrasound- versus CT-Based Screening
The latter use of CT scanning in DANCAVAS ought to produce a bias towards a higher prevalence, because CT scanning, in general, is reported to overestimate the aortic diameter compared to the US.20 However, the screening methods of the two modalities were compared in 533 consecutive attenders in the DANCAVAS pilot study showing no difference.15 The explanation seems most obvious that while the US-based measurement in the two US-based trials were measured in the peak of the systole, the CT scans in DANCAVAS were produced in the end-diastole as a consequence of the ECG gating needed to estimate coronary calcification scores, and the infrarenal aortic diameter difference between the peak of the systole and the end of diastole was described in general to be 2 mm in the VIVA trial – similar to the differences usually described between US and CT.12,21
However, as a number of other measurement aspects than technology will impact agreement between these technologies, we strongly disbelieve that this explains our finding of a sustained prevalence. First, the DANCAVAS protocol was defined to match the Viborg and VIVA by specifying strict anterior-posterior measurements from plaque to plaque (inner to inner measurements). Second, the qualification and training of the staff will directly influence the systematic error of e.g. the rate of visualization, precision in the identification of the plaques, and agreement across repeated measurements. Third, both random and systematic errors are affected by scale and scope of setting where there is a notable difference between protocolised high-volume screening trials and ad hoc measurement studies without reported strict standards of measurement. The screening method used in DANCAVAS was validated with the US confirming CT measures AAA diameters higher than the US, but more than 95% are not aneurysmatic, and overall there was no disagreement between the two modalities regarding infrarenal anterior-posterior aortic diameters. Nevertheless, the prevalence of AAA was 18% higher by CT scanning than US scanning in the validation study which could be an artefact because of the change in screening modality. However, 60% of these AAA were either more than 5 mm larger by CT or aorta weren´t visualised at the US. We interpret this as a consequence of the ultrasound scans were performed by unexperienced medical students after basic supervised training. However, we can never prove the rest isn´t due to the difference in methods, but this would maximally cause a 10% higher AAA prevalence by CT scanning.
Sustained Prevalence of AAA in Denmark
A sustained prevalence of AAA in Denmark is supported by a constant incidence of preventive elective and emergency interventions in Denmark (www.karbase.dk). In fact, a VASCUNET presentation at the ESVS annual meeting in 2018 demonstrated a higher national incidence of elective AAA repairs in Denmark (43.2/100.000) compared to England (33.5/100.000) and Sweden (37.5/100.000), where nation-wide screening programmes are implemented. Furthermore, a worldwide WHO based report clearly showed a sustained and higher AAA-specific mortality in Denmark compared to Sweden, UK and the USA.3 Finally, in addition, the prevalence of AAA by the US in the pilot study of DANCAVAS was 4.5%, which still seems similar or even higher than observed in the 1990s but the numbers examined were relatively low leaving relatively wide confidence intervals (95% C.I.: 3.0; 6.6%).
Potential Explanations
Odds ratios for having an AAA in ever, current, and former smokers compared to never all confirmed that any history of smoking is associated with AAA, but more surprisingly, the risk association has increased during the decades indicating an increased tobacco consumption (so-called “hardening of smokers”) among smokers. This is only possible, if the tobacco use per smoker has increased. While the prevalence of smoking has declined substantially over recent decades, there is empirical support for the “hardening” hypothesis in that the daily consumption per smoker in Denmark has increased from 14 cigarettes in the 1990s, to 20 in the 2000s, and to 25 in the 2010s.20 So smokers have increased their use of tobacco, and they survive CVD better and live longer,22 which combined increases their cumulative smoking exposure and thus risk of AAA explaining the sustained prevalence of AAA.
What remains to be shown is whether Denmark is uniquely experiencing a paradox of sustained prevalence of AAA – perhaps through a unique hereditary disposition, which is suggested by a twin study demonstrating that 70% of all Danish AAA can be genetically explained23 - or whether this is the first sign of a general paradox in the prevalence of AAA in similar countries as a consequence of the increasing aging population of men in risk of developing an AAA. Although the improved survival observed in the 2000s has been sustained, or improved upon in the 2010s remains to be seen, the finding of a marked two-third reduction in overall mortality by introducing general cardiovascular preventive actions in cases with screen-detected AAA calls for adding such actions to existing screening programmes and be taken into consideration by decision-makers evaluating whether permanent screening should be offered in their area.
Acknowledgments
The numerous involved project, – administrative, – and clinical staff making these trials possible are truly acknowledged, as well as the GPs in the Central Region and the Southern Region of Denmark who took over the preventive actions.
Disclosure
Dr Lars Frost reports personal fees from Bayer, Boehringer Ingelheim, BMS, MSD, and Pfizer, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Svensjö S, Björck M, Gürtelschmid M, Djavani Gidlund K, Hellberg A, Wanhainen A. Low prevalence of abdominal aortic aneurysm among 65-year-old Swedish men indicates a change in the epidemiology of the disease. Circulation. 2011;124(10):1118–1123. doi:10.1161/CIRCULATIONAHA.111.030379
2. Anjum A, Powell JT. Is the incidence of abdominal aortic aneurysm declining in the 21st century? Mortality and hospital admissions for England & Wales and Scotland. Eur J Vasc Endovasc Surg. 2012;43(2):161–166. doi:10.1016/j.ejvs.2011.11.014
3. Sidloff D, Stather P, Dattani N, et al. Aneurysm global epidemiology study: public health measures can further reduce abdominal aortic aneurysm mortality. Circulation. 2014;129(7):747–753. doi:10.1161/CIRCULATIONAHA.113.005457
4. Wanhainen A, Svensjö S, Holst J, Björck M, Gottsäter A, Swedish Aneurysm Screening Study group and the Swedish Society for Vascular Surgery. Screening for abdominal aortic aneurysm. Lancet. 2019;393(10166):27–28. doi:10.1016/S0140-6736(18)32761-2
5. Johansson M, Zahl PH, Siersma V, Jørgensen KJ, Marklund B, Brodersen J. Screening for abdominal aortic aneurysm – authors’ reply. Lancet. 2019;393(10166):28. doi:10.1016/S0140-6736(18)32742-9
6. Hansen TB, Lindholt JS, Diederichsen ACP, et al. Individual preferences on the balancing of good and harm of cardiovascular disease screening. Heart. 2019. doi:10.1136/heartjnl-2018-314103
7. Johansson M, Hansson A, Brodersen J. Estimating overdiagnosis in screening for abdominal aortic aneurysm: could a change in smoking habits and lowered aortic diameter tip the balance of screening towards harm? BMJ. 2015;350:h825. doi:10.1136/bmj.h825
8. Søgaard R, Laustsen J, Lindholt JS. Cost effectiveness of abdominal aortic aneurysm screening and rescreening in men in a modern context: evaluation of a hypothetical cohort using a decision analytical model. BMJ. 2012;345:e4276. doi:10.1136/bmj.e4276
9. Lindholt JS. Abdominal aortic aneurysms. Dan Med Bull. 2010;57(12):B4219.
10. Grøndal N, Søgaard R, Lindholt JS. Baseline prevalence of abdominal aortic aneurysm, peripheral arterial disease and hypertension in men aged 65-74 years from a population screening study (VIVA trial). Br J Surg. 2015;102(8):902–906. doi:10.1002/bjs.9825
11. Lindholt JS, Juul S, Fasting H, Henneberg EW. Screening for abdominal aortic aneurysms: single centre randomised controlled trial. BMJ. 2005;330(7494):750. doi:10.1136/bmj.38369.620162.82
12. Grøndal N, Bramsen MB, Thomsen MD, Rasmussen CB, Lindholt JS. The cardiac cycle is a major contributor to variability in size measurements of abdominal aortic aneurysms by ultrasound. Eur J Vasc Endovasc Surg. 2012;43(1):30–33. doi:10.1016/j.ejvs.2011.09.025
13. Lindholt JS, Vammen S, Juul S, Henneberg EW, Fasting H. The validity of ultrasonographic scanning as screening method for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 1999;17(6):472–475. doi:10.1053/ejvs.1999.0835
14. Diederichsen AC, Rasmussen LM, Søgaard R, et al. The Danish Cardiovascular Screening Trial (DANCAVAS): study protocol for a randomized controlled trial. Trials. 2015;16:554. doi:10.1186/s13063-015-1082-6
15. Liisberg M, Diederichsen AC, Lindholt JS. Abdominal ultrasound-scanning versus non-contrast computed tomography as screening method for abdominal aortic aneurysm – a validation study from the randomized DANCAVAS study. BMC Med Imaging. 2017;17(1):14. doi:10.1186/s12880-017-0186-8
16. Osler M, Prescott E, Gottschau A, et al. Trends in smoking prevalence in Danish adults, 1964-1994. The influence of gender, age, and education. Scand J Soc Med. 1998;26(4):293–298. doi:10.1177/14034948980260041101
17. Adkar SS, Turner MC, Leraas HJ, et al. Low mortality rates after endovascular aortic repair expand use to high-risk patients. J Vasc Surg. 2018;67(2):424–432. doi:10.1016/j.jvs.2017.06.107
18. Wanhainen A, Verzini F, Van Herzeele I, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2019;57(1):8–93. doi:10.1016/j.ejvs.2018.09.020
19. Darwood R, Earnshaw JJ, Turton G, et al. Twenty-year review of abdominal aortic aneurysm screening in men in the county of Gloucestershire, United Kingdom. J Vasc Surg. 2012;56(1):8–13. doi:10.1016/j.jvs.2011.12.069
20. Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014;311(2):183–192. doi:10.1001/jama.2013.284692
21. Wanhainen A, Bergqvist D, Björck M. Measuring the abdominal aorta with ultrasonography and computed tomography – difference and variability. Eur J Vasc Endovasc Surg. 2002;24(5):428–434. doi:10.1053/ejvs.2002.1748
22. Hjerteforeningen (The Danish Heart Foundation). HjerteTal.dk [Internet]. 2018. Available from: https://hjerteforeningen.dk/alt-om-dit-hjerte/hjertetal/hjertetaldk/.
23. Joergensen TM, Christensen K, Lindholt JS, Larsen LA, Green A, Houlind K. Editor’s choice – high heritability of liability to abdominal aortic aneurysms: a population based twin study. Eur J Vasc Endovasc Surg. 2016;52(1):41–46. doi:10.1016/j.ejvs.2016.03.012
24. Osler M, Holstein B, Avlund K, Damsgaard MT, Rasmussen NK. Socioeconomic position and smoking behaviour in Danish adults. Scand J Public Health. 2001;29(1):32–39. doi:10.1177/14034948010290010801
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
