Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 14
Sunburn Prevalence is Underestimated in UK-Based People of African Ancestry
Authors Bello O, Sudhoff H, Goon P
Received 18 August 2021
Accepted for publication 30 September 2021
Published 24 November 2021 Volume 2021:14 Pages 1791—1797
DOI https://doi.org/10.2147/CCID.S334574
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Olayemi Bello,1 Holger Sudhoff,2 Peter Goon1,2
1Department of Dermatology, Peterborough City Hospital, North West Anglia NHS Foundation Trust, Peterborough, PE3 9GZ, Cambridgeshire, UK; 2Department of Otolaryngology, University of Bielefeld, Campus Klinikum Bielefeld, Bielefeld, 33604, Germany
Correspondence: Peter Goon
Department of Otolaryngology, University of Bielefeld, Campus Klinikum Bielefeld, Bielefeld, 33604, Germany
Email [email protected]
Background: Eumelanin, the primary pigment in human epidermis, has a well-established photo-protective role. It can confer a protection factor of up to approximately 13.4 in some individuals. However, the protection eumelanin affords is not absolute and, further, the susceptibility of human skin to the harmful effects of UV radiation is more complex than skin pigmentation alone.
Objective: Our survey explored the lifetime prevalence of sunburn in people of African Ancestry based in the UK (Black African or Black Caribbean).
Results: A significant number of respondents, 52.2% (n=222), reported a history of sunburn. Interestingly, there was a significant increase in frequency of sunburn in those with a lighter skin tone (self-classified from dark, medium and light – 47.3%, 53.5% and 71.4%, respectively). In total 69% reported that the episode of sunburn occurred when they were not using sunscreen, and another 10% could not recall whether sunscreen was used. A large proportion of respondents (59%) indicated that they had been sunburnt while away from the UK in hot/sunny climates, raising the question of whether intermittent sun exposure at high UV indices is a key factor in sunburn risk for those living in temperate climates.
Conclusion: Our findings do not support the hypothesis of a simplistic relationship between skin colour and sun sensitivity and encourage us to re-examine this relationship and its implications for public health promotion. It also adds to a body of evidence revealing the need for more up-to-date and appropriate systems to assess the risk UV radiation poses to diverse populations.
Keywords: sunburn, UV radiation, skin of colour
Plain Language Summary
- Sunburn does occur in skin of colour (Black African or Black Caribbean) although this is not common knowledge outside these communities.
- The reported annual prevalence ranges from 5.8% to 38.9% but most studies are from the US, and only 1 study from the UK.
- Sun protection knowledge and sunscreen use is limited in these communities
- We found that there was a higher lifetime prevalence of reported sunburn (52.2%) amongst UK-based people of African ancestry compared to a previous report
- There was a significant increase in sunburn episodes in skin tones from dark, medium to light
- 69% were not using sunscreen at the time of sunburn
- This study has shown the dearth of data on sunburn and sun protection measures amongst people of African ancestry
- More urgent research needed on UV protection from melanin, skin tone and skin cancer incidence in these communities
- There is a need to target sun protection advice and sunscreen usage to specific communities
Introduction
Skin colour is primarily determined by the quantity and distribution of melanin,1,2,3 but other chromophores such as carotenoids4 and oxy-/deoxyhaemoglobin5,6 can also influence its appearance to a lesser degree. Skin colour is the result of complex genetics and the interaction with environmental factors, predominantly UV exposure. Sunburn, however, indicates there has been inflammation and damage due to UV over-exposure, and that too much ionising UV radiation has been absorbed. Pain, redness, heat and swelling (4 cardinal signs of inflammation dolor, rubor, calor, tumor) indicate that the skin has received significant injury from ionising radiation that can cause mutations in genomic DNA. Furthermore, the darker skin tones in humans correlate with the fewest reported incidence rates of skin cancers of all types, and point strongly towards a relatively protective effect of melanin, the dominant pigment in human skin. Accordingly, the relationship between skin colour and sunburn risk is certainly more complex than was previously understood.
The figures for annual sunburn prevalence in Black populations7,8 range from 5.8%9 to as high as 38.9%.10 Most of this work has been carried out in relation to those based in the United States. We therefore conducted a pilot survey of sunburn in a UK-based cohort self-identifying as Black&/Mixed-Race (with Black heritage).
Methods
Power and sample size calculations were performed in order to detect differences from previously published data. These calculations were based on work by Diffey et al,11 who found that 62 of 94 (66%) UK-based individuals, who “identified as having black skin”, had never experienced sunburn. Assuming the maximum number of people who may have experienced sunburn to be 32 (34%), we expected to find at least this frequency in our own study but wanted to be able to detect a difference of at least 20%. Using a standard power of 80%, with a significance level of 0.05 (alpha), we found that n = 393 would detect a difference in mean of 20%. This survey recruited n = 425 responses, thus achieving this sample size easily. Our study sample is over 4x larger than the previous study.
Ethical approval review was not required as this was a completely anonymised study, with no way to contact or identify any study participants who filled in the survey form. This is as per national guidelines from the UK NHS Health Research Authority:
The establishment of a database for public health or clinical purposes does not require review by a REC and should be managed under clinical governance arrangements. This anonymous data may then be used for research without REC approval
A 10-question survey was made accessible via platforms, such as Facebook, Instagram, Snapchat and WhatsApp (see Supplementary Materials). Questions were asked about how people self-identified, country(ies) of heritage, perceived skin shade on a scale of dark/medium/light and lifetime sunburn frequency. Only responses from participants who indicated that they lived in the UK and those that self-identified as being Black&/Mixed Race (with Black heritage) were included in the analysis (Inclusion and exclusion criteria).
Informed consent was provided by all (by voluntarily participating after reading the website materials and anonymous questionnaire), and this study was conducted in accordance with the Declaration of Helsinki.
The survey was made available between 07/06/20 and 27/07/20 which was 52 days.
The formula for exponential growth/decay can be expressed as:
x(t) = x0(1 + r)t where x(t) is the value at time t
x0 is the initial value at time t = 0
r is the growth rate
t is the time in integer units, ie days/months/years, etc.
We have approximated the growth rate of the survey as being seen by internet traffic, and therefore with r = 0.04 (4%) to 0.06 (6%) we get between 553 and 6963 visualizations.
The lower limit is likely to be at this level as any lower and there would not be the number of responders that we obtained (n = 425). The upper limit is speculative, as exponential growth rates can accelerate very quickly (going “viral”) but a very2 large and accelerating increase in internet traffic was also unlikely, as the survey and website were monitored regularly and this type of increase was not noticed.
Statistical analyses (power calculations, Fischer’s exact tests and χ2 tests) were performed with GraphPad Prism 8, assuming normally distributed populations.
Results
Four hundred and twenty-five participant responses were included in the analyses. Of the respondents who specified their geographical heritage, 312 reported having heritage in 1 or more African countries and 115 reported heritage from one or more Caribbean islands/Caricom countries (See Figure 1). Ten respondents had heritage in both Africa and the Caribbean and at least 30 respondents reported heritage from countries outside Africa and the Caricom, including China, India and European countries. Two hundred and fifty respondents identified as female, 174 as male and one respondent did not specify their sex. Thirty-five respondents were excluded from the analyses due to: (i) not self-identifying as Black&/Mixed-Race or (ii) not having the UK as the main country of domicile. The mean age of respondents was 32 years (SD 11).
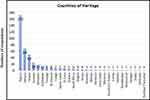 |
Figure 1 Countries of heritage as specified by respondents. |
52.2% (n = 222) of included participants had experienced sunburn at least once in their lifetime. This result is significantly higher than the value reported by Diffey et al (*p = 0.014, Fischer’s exact test). Of those that had experienced sunburn before, 37.4% (n = 83) had sunburnt only once, while 16.7% (n = 37) had sunburned over five times (see Figure 2).
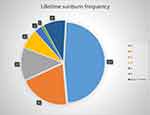 |
Figure 2 Lifetime frequency of sunburn. 0 (n=203), 1 (n=83), 2 (n=54), 3 (n=32), 4 (n=12), 5 (n=4), Over 5 times (n=37). |
The relationship between self-reported skin complexion and sunburn frequency was also assessed. 47.3% (n = 89) of those with a self-reported “dark” complexion had been sunburnt before, compared with 53.5% (n = 108) of those with a “medium” complexion and 71.4% (n = 25) of those with a “light” complexion. In regard to whether people had been sunburnt before or not, the respondents self-classifying as “light” were found to be more likely to have reported sunburn compared to the other skin tone groups (χ2, p = 0.00116*).
Furthermore, 37 participants reported that they had been sunburnt over 5 times; n = 17, 18 and 2 for the dark, medium and light complexion categories, respectively. [This seemingly counter-intuitive result could potentially be explained by people with darker skin having the misconception that they cannot be sunburnt, and thus not protecting themselves.] We classified this group as those with high sunburn episodes, and compared them to respondents who had a lower history of sunburn episodes (5 and less). No significant differences were found between the high and low sunburn groups within the 3 groups of dark, medium and light skin tone (χ2, p = 0.420678).
Other factors were explored, including age and sex. Participants aged 30 and above were more likely to have experienced sunburn before. A greater proportion of female respondents (63.2%) had been sunburnt as compared with 36.8% of males. Respondents were also asked about sunscreen use at the time of sunburn; 69% reported “no”, 21% “yes” and 10% were not able to recall (see Figure 3).
 |
Figure 3 Sunscreen use at time of sunburn. |
Respondents were given the opportunity to leave a comment regarding the circumstances surrounding their sunburn experience(s); indication of being away on holiday or “abroad” was mentioned 163 times whilst being in the UK was mentioned 40 times. Frequently, the comments made reference to hot climates, high temperatures, sunbathing and prolonged sun exposure.
Discussion
Estimates of sunburn prevalence in people of African Ancestry are as low as 5.8%9 when focusing on annual sunburn risk alone. However, when this question is expanded to investigate lifetime risk, as little as 34% of Black South Africans, in a survey by Diffey et al, reported never experiencing sunburn before.11 In the same survey, Diffey et al also found that 66% of their UK-based respondents reported never experiencing sunburn before. In our survey, 52.4% of included respondents had experienced sunburn over their lifetime compared to 47.6% who had not. These discrepancies highlight the fact that survey studies are more subjective, depend on the way the questions are phrased, and highly dependent on sample sizes plus target populations. The comparison between annual and lifetime risk highlights the way in which the question choice can influence the wider narrative on sunburn risk in some populations.
Another key influence on our understanding of sunburn risk has been the Fitzpatrick scale, the most extensively used skin typing classification. It started life as a 4-point scale designed to categorise white skin but was later extended to accommodate “brown” (type V) and “black” (type VI) skin.12 The concept of a direct relationship between skin colour and its response to UV radiation has become heavily associated with the scale such that modern variations assert that brown/type V skin rarely burns, while black/type VI skin “never burns”. This is further complicated by the commonplace conflation of skin colour and racialisation as well as the use of the Fitzpatrick scale as a proxy for race/ethnicity13 (in direct contrast to Fitzpatrick’s own 1988 understanding of race12). In our survey, there was an increasing proportion of respondents who reported sunburn, the lighter their self-perceived skin tone. This relationship, however, was non-linear. Our survey also demonstrated that people of varying ethnicities experienced sunburn, irrespective of their self-reported skin tone. This thereby illustrates that the relationship between skin complexion, ethnicity and sunburn risk is not so straightforward.
Moreover, while the photo-protective effects of eumelanin have been well documented,14 increased pigmentation/eumelanin content does not provide total immunity against UV radiation. Tadokoro et al15 demonstrated that while lighter skin types were more susceptible to UV-induced DNA damage than darker skin types, even low levels of UV exposure were able to induce significant DNA damage in all skin types. In addition, they did not find a relationship between skin pigmentation or racial/ethnic classification and efficiency of DNA damage removal.15 Furthermore, despite comparatively lower incidence rates of some skin cancers in people of African ancestry, skin cancers do occur nonetheless. However, the association between UV exposure in skin of colour and skin cancers is controversial, and deserves much more research to elucidate any mechanistic pathways of protection (if these exist).
Lopes et al carried out a meta-analysis that did not support an association between melanomas in skin of colour with UV exposure,16 although the authors were only able to include 13 studies of low-to-moderate quality. Two studies showed a small but significant association in Blacks and Hispanics but 11 studies did not demonstrate any association. There is therefore limited evidence to support the hypothesis that UV exposure is linked to melanoma in skin of colour. Conversely, there have been multiple reports of the occurrence of basal cell carcinomas at sun-exposed sites in people of African ancestry.17–19 The reason underlying the differential skin cancer incidence and survival rates between different populations is an area that requires ongoing research.
A large proportion of those that had experienced sunburn indicated that they had been outside the UK at the time, typically in hot/sunny climates. This raises the question of whether there is a relationship between sunburn tendency and intermittent sun exposure at high UV indices for people who normally live in temperate climates. Conversely, a smaller proportion of respondents indicated that they had been sunburnt, while they were in the UK. Thus, further research is required to explore the importance of intermittent sun exposure, holiday frequency and UV index in regard to sunburn risk in diverse populations.
Sixty-nine percent of respondents who had sunburnt before reported not using sunscreen at the time. Similarly, there have been reports of comparatively lower sunscreen usage in communities of people of African Ancestry.20,21 The reasons for this are likely to be multifactorial, as previous authors have demonstrated discrepancies in the understanding of: (i) what constitutes sunburn;22,23 (ii) the harmful effects of UV radiation;24 and (iii) benefits of sunscreen.24 Factors affecting the choice of sun protection modality may also provide useful insight,11,25 as well as acknowledging that sunscreens have additional uses beyond sunburn avoidance. The lack of visibility of people from ethnic minority backgrounds in Western sunscreen advertising is likely to play a role. Moreover, uncertainty exists within the medical community in regard to sun protection and skin cancer prevention advice for non-Caucasian populations. In one study, Black people were less likely to report having undergone a full-body skin examination by their physician compared to their White counterparts26 while another study found that Black people were less likely to be recommended sunscreen than their White counterparts.27 The shortage of research exploring sunburn and sun protection in diverse populations and the significance of these issues in the context of low intrinsic skin cancer risk is likely to contribute to this uncertainty.
As there is presently little published information on sunburn and sun protection amongst the UK’s ethnic minority groups, this preliminary survey offers some useful insight. The limitations of our work include the use of a self-selected sample and a subjective measure of skin complexion. Nonetheless, our work demonstrates that the relationship between sunburn and skin complexion is more complex and highlights the need for further research. Future works should explore additional factors that may impact sunburn prevalence, including frequency of holidays in hot/sunny climates, UV index, socioeconomic status, educational attainment and sociocultural factors, as well as knowledge of skin cancer and sun protection. A deeper understanding of the effects of sun exposure on those living in temperate climates as compared with those living in tropical climates is also required. Such work may one day allow us to be able to tailor sun protection advice to meet individual needs.
Abbreviation
The Caricom (ie Caribbean Community) is a group of twenty countries, which consists of fifteen Member States and five Associate Members.
Access to Data and Data Analyses
Dr Goon had had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
No funder or sponsor was involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure
Holger Sudhoff and Peter Goon are co-senior authors of this study. The authors declare that they have no known conflicts of interest.
References
1. Kaidbey KH, Agin PP, Sayre RM, et al. Photoprotection by melanin - a comparison of black and Caucasian skin. J Am Acad Dermatol. 1979;1(3):249–260. doi:10.1016/S0190-9622(79)70018-1
2. Thody AJ, Higgins EM, Wakamatsu K, et al. Pheomelanin as well as eumelanin is present in human epidermis. J Invest Dermatol. 1991;97(2):340–344. doi:10.1111/1523-1747.ep12480680
3. Wakamatsu K, Kavanagh R, Kadekaro AL, et al. Diversity of pigmentation in cultured human melanocytes is due to differences in the type as well as quantity of melanin. Pigment Cell Res. 2006;19(2):154–162. doi:10.1111/j.1600-0749.2006.00293.x
4. Alaluf S, Heinrich U, Stahl W, et al. Dietary carotenoids contribute to normal skin colour and UV photosensitivity. J Nutr. 2020;132(3):399–403. doi:10.1093/jn/132.3.399
5. Stamatas GN, Kollias N. Blood stasis contributions to the perception of skin pigmentation. J Biomed Opt. 2004;9(2):313–322. doi:10.1117/1.1647545
6. Takiwaki H, Miyaoka Y, Kohno H, Arase S. Graphic analysis of the relationship between skin colour change and variations in the amounts of melanin and haemoglobin. Skin Res Technol. 2020;8(2):78–83. doi:10.1034/j.1600-0846.2002.00333.x
7. Holman DM, Ding H, Guy GP
8. Holman DM, Ding H, Berkowitz Z, et al. Sunburn prevalence among US adults, National Health Interview Survey, 2005, 2010, and 2015. J Am Acad Dermatol. 2019;80(3):817–820. doi:10.1016/j.jaad.2018.10.044
9. CDC. Sunburn prevalence among adults — United States, 1999, 2003 and 2004. MMWR. 2007;56(21):524–528.
10. Chapman LW, Ochoa A, Tenconi F, Herman A. Dermatologic health literacy in underserved communities: a case report of south Los Angeles middle schools. Dermatol Online J. 2015;21(11). doi:10.5070/D32111029308
11. Diffey BL, Fajuyigbe D, Wright CY. Sunburn and sun protection in Black skin. Int J Dermatol. 2019;58(9):1053–1055. doi:10.1111/ijd.14402
12. Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124(6):869–871. doi:10.1001/archderm.1988.01670060015008
13. Ware OR, Dawson JE, Shinohara MM, Taylor SC. Racial limitations of Fitzpatrick skin type. Cutis. 2020;105(2):77–80.
14. Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochem Photobiol. 2008;84(3):539–549. doi:10.1111/j.1751-1097.2007.00226.x
15. Tadokoro T, Kobayashi N, Zmudzka BZ, et al. UV induced DNA damage and melanin content in human skin differing in racial/ethnic origin. FASEB J. 2003;17(9):1177–1179. doi:10.1096/fj.02-0865fje
16. Lopes FCPS, Sleiman MG, Sebastian K, et al. UV exposure and the risk of cutaneous melanoma in skin of color: a systematic review. JAMA Dermatol. 2021;157(2):213–219. doi:10.1001/jamadermatol.2020.4616
17. Matsuoka LY, Schauer PK, Sordillo PP, et al. Basal cell carcinoma in Black patients. J Am Acad Dermatol. 1981;4(6):670–672. doi:10.1016/S0190-9622(81)70067-7
18. Fleming ID, Barnawell JR, Burlison PE, Rankin JS. Skin cancer in Black patients. Cancer. 1975;35(3):600–605. doi:10.1002/1097-0142(197503)35:3<600::AID-CNCR2820350309>3.0.CO;2-3
19. da Silva DLF, Vasconcelos J, Silva RR, et al. Basal cell carcinoma in African-Americans; two case reports. J Clin Exp Dermatol Res S. 2013;3:2.
20. Caldéron TA, Bleakley A, Jordan AB, et al. Correlates of sun protection behaviors in racially and ethnically diverse U.S. adults. Prev Med Rep. 2019;13:346–353. doi:10.1016/j.pmedr.2018.12.006
21. Summers P, Bena J, Arrigan S, et al. Sunscreen use: non-Hispanic Black compared with other racial and/or ethnic groups. Arch Dermatol. 2011;147(7):863–864. doi:10.1001/archdermatol.2011.172
22. Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessing Fitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149(11):1289–1294. doi:10.1001/jamadermatol.2013.6101
23. Robinson JK, Joshi KM, Ortiz S, et al. Melanoma knowledge, perception, and awareness in ethnic minorities in Chicago: recommendations regarding education. Psychooncology. 2011;20(3):313–320. doi:10.1002/pon.1736
24. Dlova NC, Gathers R, Tsoka-Gwegweni J, Hift RJ. Skin cancer awareness and sunscreen use among outpatients of a South African hospital: need for vigorous public education. S Afr Fam Pract. 2018;60(4):132–136. doi:10.1080/20786190.2018.1426900
25. Wright CY, Reeder AI, Albers PN. Knowledge and practice of sun protection in schools in South Africa where no national sun protection programme exists. Health Educ Res. 2016;31(2):247–259. doi:10.1093/her/cyw005
26. Rodriguez GL, Ma F, Federman DG, et al. Predictors of skin cancer screening practice and attitudes in primary care. J Am Acad Dermatol. 2007;57(5):775–781. doi:10.1016/j.jaad.2007.04.023
27. Akamine KL, Gustafson CJ, Davis SA, et al. Trends in sunscreen recommendation among US physicians. JAMA Dermatol. 2014;150(1):51–55. doi:10.1001/jamadermatol.2013.4741
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
