Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Suicidality, self-stigma, social anxiety and personality traits in stabilized schizophrenia patients – a cross-sectional study
Authors Vrbova K, Prasko J , Ociskova M , Holubova M, Kantor K , Kolek A, Grambal A, Slepecky M
Received 9 January 2018
Accepted for publication 14 March 2018
Published 1 June 2018 Volume 2018:14 Pages 1415—1424
DOI https://doi.org/10.2147/NDT.S162070
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Roger Pinder
Kristyna Vrbova,1,2 Jan Prasko,1–3 Marie Ociskova,1,2 Michaela Holubova,4 Krystof Kantor,1,2 Antonin Kolek,1,2 Aleš Grambal,1,2 Milos Slepecky3
1Department of Psychiatry, University Hospital Olomouc, Olomouc, Czech Republic; 2Faculty of Medicine and Dentistry, Palacky University Olomouc, Olomouc, Czech Republic; 3Department of Psychology Sciences, Faculty of Social Science and Health Care, Constantine the Philosopher University in Nitra, Nitra, Slovak Republic; 4Department of Psychiatry, Hospital Liberec, Liberec, Czech Republic
Background and aim: Patients who have schizophrenia are more prone to suicidal behavior than the general population. This study aimed to find connections between suicidality and self-stigma, hope, and personality traits in patients with schizophrenia.
Methods: Forty-eight stabilized outpatients with schizophrenia attended this cross-sectional study. Patients were diagnosed by the Mini International Neuropsychiatric Interview (MINI) using the ICD-10 research diagnostic criteria. The assessments included Positive and Negative Syndrome Scale, objective and subjective Clinical Global Impression, Liebowitz Social Anxiety Scale, Beck Depression Inventory-second edition, Internalized Stigma of Mental Illness, the Temperament and Character Inventory, and Adult Dispositional Hope Scale.
Results: The individual rate of suicidality (suicidal index from MINI) strongly positively correlated with self-stigma, level of depression, social anxiety, and harm-avoidance, and negatively correlated with hope, self-directedness, and stigma resistance.
Conclusion: Individuals with additional symptoms of depression, social anxiety, trait-like anxiety, and self-stigma should be carefully monitored for suicidal ideation. On the opposite side, patients with sufficient hope, self-esteem, and goal-directed attitudes are less likely to have suicidal thoughts and may potentially be role models in group rehabilitation programs, motivating more distressed colleagues and showing them ways to cope.
Keywords: schizophrenia, suicidality, self-stigma, hope, positive and negative symptoms, personality traits, social anxiety
Introduction
Despite considerable progress in the treatment of schizophrenia, patients with the disorder have a high suicidal risk.1 Individuals with schizophrenia commit suicide nearly 13 times more often than the general population,2 with the lifetime estimation from 4 to 10%.3–5 Suicidal attempts are fatal in 20%–40%.6,7
Repeatedly reported risk factors of suicide are male gender, greater insight into the illness, poor adherence to treatment, substance abuse or dependence, episodes of depression, and previous suicide attempts.1,8,9 Protective factors, such as cognitive decline at an early stage and having daily activities, have been reported.8 Hallucinations have been somewhat surprisingly stated to be a protective factor in one meta-analysis;1 however, other studies found the opposite results.9–11 A Finnish suicide study of patients with schizophrenia indicates that a third of the patients who commit suicide are 45 years and older.12
Despite considerable efforts, pharmacological treatment, and psychosocial interventions, the numbers of suicides in schizophrenic patients have remained unchanged for several decades.13 However, exciting work was published by Nordentoft et al,14 which showed that the suicide rate among Danish schizophrenic patients declines parallel to the general population.
Some studies showed that hopelessness and insight into the severity of psychopathology is one of the most important predictors of completed suicide in patients with psychotic disorders.15–17 The results of two later studies that focused on this problem showed that a more significant insight into the disorder significantly predicts the risk of suicide, but only if the insight leads to hopelessness.18,19 The level of self-stigma also correlated to suicide rates in patients with bipolar disorder and schizophrenia.19,20
Some symptoms of psychopathology are also associated with suicidal risk. Anxiety contributes to suicide in postpsychotic depression.21,22 Panic attacks, psychomotor agitation and restlessness, fear of psychotic breakdown of personality, akathisia, aggression, impulsivity, and poor compliance all correlate with higher suicidal risk too.22–24 About one-third of suicide victims also meet the criteria for personality disorders.25
A number of studies have shown that the acute phase of the disease and the presence of positive psychotic symptoms,8,26,27 as well as thought disorders,28,29 and imperative auditory hallucinations are linked to higher suicidality.30
A systematic review of risk factors for suicide in schizophrenic patients identified 29 relevant studies and revealed seven robust risk factors: previous depressive disorder, previous suicide attempts, drug abuse, agitation or motor agitation, fear of mental decline, adherence to treatment, and recent loss.1 Reduced suicide risk was associated with hallucinations. The authors claimed that imperative hallucinations are not an independent risk factor, but they increase the risk in those who are already susceptible to suicide.1 Overall, suicide is less associated with the underlying symptoms of psychosis and more with affective and psychomotor symptoms (restlessness), and schizophrenia-based decline in mental function.
Melle and Barrett31 found that the risk of suicide is higher among patients with schizophrenia in the early phases of the disorder and increases with the time duration of untreated psychosis. Findings of other studies have been in agreement, as the risk of suicide is twice as high at the start of treatment in comparison with later stages of the disorder.32,33
The multiple studies have recognized a positive correlation between suicide ideation and negative symptoms (assessed by the negative symptoms subscale of the Positive and Negative Syndrome Scale; PANSS).34–37 However, there have been mixed results about the role of negative symptoms and risk of suicide.38,39
The role of personality traits on suicidality was assessed in some studies. In another study, self-transcendence was shown to be a predictor of lifetime suicide attempts in 120 outpatients.41 In one more study, harm-avoidance and persistence were positively associated with suicidal behavior, while higher self-directedness and cooperativeness were negatively associated with suicidal behavior.40
According to the results of our previous studies, some demographic factors such as the earlier onset of illness and the number of hospitalizations may worsen the overall course of the disorder and its concequences.42,43 But there are a lack of studies that would point to a link between suicidality and the earlier onset of illness or the number of hospitalizations.
Aims of the study and hypotheses
The present study aims to test the relationship among suicidal ideation, self-stigma, hope, positive and negative schizophrenia symptoms, and social anxiety in stabilized patients with schizophrenia. There is lack of information about risk factors of suicidality in stabilized outpatients and factors correlated with it.
The hypotheses of the study were:
- Suicidality correlates positively with (a) positive symptoms; (b) negative symptoms; (c) self-stigma; (d) social anxiety symptoms; (e) depressive symptoms; (f) harm-avoidance and persistence; and negatively correlates with (g) hope; and (h) self-directedness and cooperativeness.
- Patients with comorbid depression or comorbid social phobia have a higher suicide risk than patients without such comorbidities.
- The early onset of the disorder, the duration of the treated disorder, number of hospitalizations, and disability pension are connected with suicidality.
Methods
Patients
Forty-eight outpatients in stable condition (without a need for a change of the treatment) entered into the study. All patients who were invited to participate accepted the invitation to the study. They were consecutive patients who fulfilled the inclusion criteria for schizophrenia without any other selection. The structured interview MINI (Mini International Neuropsychiatric Interview) was used to confirm the diagnosis.44 Inclusion criteria were:
- Age 18–65 years
- Diagnosis of the schizophrenia according to ICD-10 and the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)45,46
- The severity of the illness was determined thorough interview with a doctor, who evaluated the severity on the objective version of Clinical Global Impression – Severity (objCGI-S) scale.47
Exclusion criteria were:
- Presence of a severe physical illness
- Intellectual disability or organic mental disorder.
Nine patients did not meet inclusion criteria, because after careful assessment they met diagnostic criteria for schizoaffective disorder or delusional disorder. They were excluded because they did not meet diagnostic criteria for schizophrenia.
Assessment instruments
The following assessment tools were used:
- MINI.44 MINI is a structured interview covering diagnostic criteria for common psychiatric disorders according to the DSM-5 and ICD-10.45 The suicidal index of MINI was the primary outcome measure of suicidality.
- PANSS.37 The scale measures the positive, negative, and general symptoms of schizophrenia. The scale comprises 30 items allocated into three subgroups: 7 positive (PANSS P), 7 negative (PANSS N), and 16 general psychopathological items. The total score is the sum of all points, called PANSS total (PANSS T). The score of 58 corresponds with mild illness, 75 points correspond with moderate illness, 95 points correspond with marked illness, and 116 points correspond with severe illness.48
- CGI. The GCI evaluates the overall severity of the disorder.47 It consists of one scale with seven points. Score 1 indicates absence of illness, while score 7 indicates extreme illness. The source of the assessment in objCGI-S is a comprehensive assessment of the patient by a physician.
- BDI-II (Beck Depression Inventory-II).49 BDI measures the severity of depressive symptoms. It includes 21 items of which the patient selects one of the four defined opportunities that best matches how they have felt in the last 2 weeks. The inventory was adapted to Czech population and standardized by Ociskova et al.50,51
- ISMI (The Internalized the Stigma of Mental Illness Scale). This scale measures the level of self-stigma. The scale contains 29 items with a four-point scale, which evaluates five areas of self-stigma.52 These include feelings of alienation from society, the rate of stereotype endorsement about persons with psychiatric disorder, perceived discrimination (how the patient feels about the behavior of others toward him because of psychiatric diagnosis), social withdrawal, and the degree of stigma resistance.52–54 ISMI was standardized in the Czech Republic.55
- ADHS (Adult Dispositional Hope Scale). This scale measures the level of hope. It consists of 12 items: four assess the capability to set the adaptive pathway to the aim, four focus on effort, and four are distractors.56 The patient chooses their level of agreement with the statement on an eight-point scale. Ociskova et al57 standardized the measurement in Czech.
- LSAS (The Liebowitz Social Anxiety Scale). The questionnaire measures the level of social anxiety and avoidance behavior. The scale consists of 24 items related to different social situations.58 The present study used its self-report version.
- TCI-R (Temperament and Character Inventory – Revised). This consists of 240 items.59 The questionnaire assesses four temperamental and three character personality traits. Features of temperament include novelty seeking (NS), harm-avoidance (HA), reward dependence (RD), and persistence (PS). Characteristic features include self-directedness (SD), cooperativeness (CO), and self-transcendence (ST).60 Czech percentile standards were created by Preiss and Klose.61
- The demographic questionnaire contained the necessary information: gender, age, marital status, education, employment, disability, the age at the disorder onset, the duration of the treated disorder, the number of hospitalizations, length of the last hospitalization, number of visited psychiatrists, medications, and data on stopping the medication in the past.
Statistics and ethics
The statistical programs Prism (GraphPad PRISM version 5.0; GraphPad Software Inc., La Jolla, CA, USA; http://www.graphpad.com/prism/prism.htm) and SPSS 24.0 (IBM Corporation, Armonk, NY, USA) were used for the statistical estimation of the results. Demographic data and the average scores in the distinct questionnaires and scales were evaluated using descriptive statistics (means, medians, standard deviations, and the character of data distribution). Means were compared by using unpaired t-tests. Relations between categories have been calculated using correlation coefficients. Because of many measures, we used Bonferroni correction for multiple comparisons to reach more precise outcomes. Fisher’s exact test verified the relationship between alternative variables (gender, marital status, discontinuation of medication). Backward stepwise regression established the significance of each significant correlation coefficient. The statistical tests were reflected as satisfactory at 5% level of statistical significance.
The local ethical committee of the Faculty of Medicine and Dentistry, University Palacky in Olomouc, approved this study. The research was conducted in accordance with the latest version of the Declaration of Helsinki and recommendations for good clinical practice.62 All participants provided written informed consent.
Medication management
All 48 patients had been prescribed antipsychotics in the range of advised therapeutic doses (mean 5.53 ± 4.02 mg daily dose of the antipsychotics index; converted to the dosage of risperidone). In addition to the antipsychotic medication, 21 patients (47.3%) were also treated with antidepressants, 7 patients (14.6%) by benzodiazepine anxiolytics, and 7 patients (14.6%) by mood stabilizers. Medications were administered according to the recommended Czech guidelines for the treatment of schizophrenia.63
Results
Description of the sample
The data were collected in the period from August 2016 to October 2017. Forty-eight patients completed questionnaires. The demographic, clinical, and psychological data are described in Table 1.
Demographic data and suicidality
The suicidal index from MINI statistically significantly positively correlated with the number of the previous hospitalizations and the duration of the treated disorder and negatively with the age of the onset of the disorder (Table 2). After Bonferroni correction for multiple comparisons, only duration of the treated disorder passed the statistical significance (Table 2). The mean suicidal index did not statistically differ between sexes, level of education, employment status, marital status, and heredity, but there was a statistically significant difference between people without and with a pension (Table 3).
  | Table 3 Suicidality index and the gender, level of education, employment and partnership |
The severity of the disorder, depression, and suicidality
The suicidal index positively correlated with objective CGI and the level of the depression measured by BDI-II (Table 2).
The severity of social anxiety and suicidality
The suicidal index positively correlated with the level of the severity of social anxiety, measured by the total score LSAS (Table 2).
Positive and negative symptoms, and suicidality
PANSS total, positive, and general subscores, but not negative symptoms correlated with the suicidal index (Table 2).
Hope and suicidality
Hope measured by ADHS-total negatively correlated with the suicidal index (Table 2).
Self-stigma and suicidality
Self-stigma measured by ISMI-total positively significantly correlated with the suicidal index (Table 2).
Personality traits and suicidality
There was a statistically significant positive correlation between the suicidal index and harm-avoidance and a negative correlation between suicidal index and self-directedness (Table 2). Novelty seeking, reward dependence, persistence, cooperativeness and self-transcendence were not significantly connected with the suicidal index (Table 2).
Medication and suicidality
Antipsychotic index (daily dose of antipsychotic) did not correlate with the suicidal index, but antidepressant index (antidepressants were administrated in 21 patients) statistically, significantly, positively correlated with the suicidal index; nevertheless, after Bonferroni correction for multiple comparisons it did not pass statistical significance (Table 2).
Comorbidity and suicidality
Patients with comorbid depression had statistically significantly higher suicidal index than patients without comorbid depression (Table 3). There was no statistically significant difference in suicidal index between patients with and without any anxiety disorder, but there was a significant difference in the suicidal index between patients without and with social phobia (Table 3).
Regression analysis
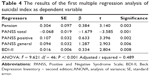
Because various factors significantly correlated with the suicidal index, a multiple regression analysis was completed to detect the most central factors associated with suicidality in patients with schizophrenia.
We made two backward regression analyses to avoid confounding between diagnosis of depression and BDI-II which measure severity of depressive symptoms, and between diagnosis of social phobia and LSAS, which measure severity of social anxiety symptoms. The dependent variable was the suicidal index according to MINI.
In the first regression analysis, the independent variables which showed significant correlations with suicidality after Bonferroni correction were: duration of the treated disorder, objCGI-S, BDI-II, LSAS-total, PANSS T, PANSS P, PANSS G, ADHS-total, ISMI-total, and harm-avoidance.
During the six steps of the backward stepwise regression pension, PANSS T, PANSS P, PANSS G, and BDI-II passed with statistical significance (Table 4).
In the second regression analysis, the independent variables were: duration of the treated disorder, objCGI-S, comorbid depressive disorder, comorbid social anxiety disorder, PANSS T, PANSS P, PANSS G, ADHS-total, ISMI-total, and harm-avoidance. Pension, harm-avoidance, PANSS T, PANSS P, and PANSS G passed with statistical significance (Table 5).
Discussion
This study aimed to explore connections between selected clinical and psychological factors in stabilized patients with schizophrenia. The results have shown that increased suicide is related to the duration of the treated disorder, nevertheless this factor did not pass regression analysis. The only demographic factor that entered and also passed regression analysis is pension. The results of larger Finnish study showed opposite results.64 The difference between the our study and the Finnish study may be due to the different populations studied; our patients had several hospitalizations in the past, while Kiviniemi et al’s study64 included patients with first episode of schizophrenia.
The suicidality is also correlated with the level of depression and social anxiety at the time of assessment. Only the severity of depressive symptoms measured by BDI-II pass the regression analysis. The most influential clinical factors are positive and general symptoms of schizophrenia measured by PANSS. Both these clinical factors and also PANSS T passed regression analysis. But PANSS N, measuring the severity of negative symptoms, did not correlate with suicidality. The results of our study are in agreement with the outcomes of other studies which showed that severity of positive symptoms is associated with high risk of suicide.1,8,26,27,65 Alternatively, our results did not confirm results of studies which found a positive correlation between suicidality and the negative symptoms.34–37 Instead, our results were in agreement with investigations which did not find a significant relationship between negative symptoms and risk for suicide.38,39 For a better understanding, however, it would be necessary to use more differentiated assessment tools, capturing specific attitudes to suicide and positive symptoms, as well as the content of those positive symptoms (eg, voices ordering the patient to attempt suicide).
Also the degree of hope, measured by ADHS scale, which is considered to be a more or less stable personality factor, significantly negatively correlated with the degree of suicidality. The hypothesis that hope is negatively related to suicidality, based on shared clinical experience, was confirmed in our study, even though the degree of hope was not such a substantial factor to pass through the regression analysis in our sample. The connection between hopelessness and suicidality is described elsewhere.65 In an interpretive phenomenological analysis of suicide in young men with the first episode of psychosis, suicide was perceived as an escape from terrifying, disturbing experiences and was associated with anger and impulsivity, without hope to future. However, keeping a hopeful state of mind was associated with sharing of one’s burden, finding a sense of belonging, and reduced suicidality.66
The study shows that self-stigma could be an essential factor influencing suicidality levels of patients with schizophrenia. The self-stigma positively correlated with suicidality. It seems that patients with higher level of self-stigma have a higher level of suicidality. The level of self-stigma was related to the suicidal rates in another study with patients who have schizophrenia and bipolar disorder.17,67 The total ISMI score was used as independent variables in regression analysis and was removed from the regression. It means that factors like psychopathology and pension are more strongly related to suicidality.
Only the temperament trait from TCI harm-avoidance correlated with suicide. Suicidality increases with higher harm-avoidance. This trait also passed regression analysis. Scores of harm-avoidance were higher in suicidal patients with schizophrenia in comparison with non-suicidal patients in one previous study.43 However, harm-avoidance has been associated with suicidal behavior in many other studies in non-schizophrenic populations.68–70 This suggests that this temperament trait relates to suicidality, no matter the population on which this relation has been studied.
Comorbidity with depressive disorder and social phobia have been shown to have a significant effect on suicidality in schizophrenic patients, although they did not pass through regression analysis, where stronger factors removed them. Depressive disorder was reported as a risk factor for suicide in several studies of patients with schizophrenia.1,8,9 Our results also confirmed the results of the current meta-analysis by Cassidy et al,65 which showed that depressive symptoms are a natural factor associated with suicide. The comorbidity with panic attacks was linked to the higher suicide rates in schizophrenia, but there was no information about the higher rate of suicidal ideation in patients with comorbid social phobia.71 Our previous study results were indirectly in agreement with the present data: social phobia was associated with higher severity of symptoms,72 and according to a review by Cassidy et al,65 a higher overall severity of symptoms is related to suicide. Social phobia is also associated with more frequent isolation of patients which increases their hopelessness.66
When returning to the hypotheses set forth at the beginning of the study, our results confirm that positive schizophrenia symptoms and general schizophrenia symptoms, level of depressive symptoms, harm-avoidance, and pension correlated with suicidality. But the connection between suicidality and negative symptoms, persistence, self-directedness, and cooperativeness was not found. Also no link was found between demographic factors and suicidality.
It is important to look for level of suicidality in patients with schizophrenia with higher depressive symptoms, especially in patients on a pension. The level of depression, social anxiety, and harm-avoidance could be influenced by psychotherapy and social skills training.73,74 Clinicians may develop a collaborative clinical focus on increasing frequency of social interactions, lessening avoidance from people, improve reciprocity in social relationships, make contributions to others, and reduce dependency or destructive behaviors in relationships. Additionally, the results of this study also indicate that assessing the functioning in social roles, as well as reducing stigma, may be beneficial when assessing suicide risk in individuals with schizophrenia.
Limitations of the study
The study has several limitations. The cross-sectional study does not allow us to explore the causality of the studies phenomena – a prospective study is needed. Another limitation is the high number of possible predictors after correlation analysis in a sample size of just 48 patients. The results of the regression analysis in such number of patients are imperfect. In addition, the stabilized outpatient population adds to less variability in suicidality in the cohort. The low scored variable of suicidality also prevented the use of other analyses that could have been more sound. Our sample was predominantly single (never married) which may limit generalizability to individuals who are married, divorced, or widowed. The stabilized outpatient sample also limits generalizability to the more symptomatic population. The participants used different psychopharmacs. Use of questionnaires based on self-evaluation presents another limitation. We cannot rule out the likelihood of social desirability bias in answering. The use of such methods is also conditioned by the capability of the introspection of the patients and readiness to be open in their reports. Potential cognitive deficits could also lower the validity of the patients’ reports.
Conclusion
Patients with schizophrenia experience a high prevalence of the suicide attempts and death. The study result suggests a possible way to recognize suicidality in schizophrenia. The first significant factor is harm-avoidance which is a mostly inherited temperament trait characterized by excessive worrying; tendency to pessimism; shyness in social contact, fears; and getting easily fatigued. If this is connected with a predisposition to psychotic illness, it can result in early onset of schizophrenia. The earlier the psychotic breakdown means worsened functioning in society and more stigmatization. That can result in suicide ideations. The results suggest the importance in detecting people with the harm-avoidance personality trait to help them change the behavior connected with it by counseling and psychotherapy. In patients with early onset of schizophrenia illness, we need to prevent stigmatization by changing the knowledge of illness in professional caregivers and the public. Our data suggest the importance of the subsequent study and longitudinal assessment of the symptoms, personality traits, demographic factors, and their influence on the subjectively perceived suicidality.
The implications of the findings in practice should be an important message for the clinicians that the severity of the disorder, social anxiety, depression and suicidality are also interrelated in stabilized outpatients with schizophrenia.
Disclosure
The authors report no conflicts of interest in this work.
References
Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9–20. | ||
Bushe CJ, Taylor M, Haukka J. Mortality in schizophrenia: a measurable clinical endpoint. J Psychopharmacol. 2010;24(S4):17–25. | ||
Miles CP. Conditions predisposing to suicide: a review. J Nerv Ment Dis. 1977;164(4):231–246. | ||
Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry. 1998;172:35–37. | ||
Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a re-examination. Arch Gen Psychiatry. 2005;62(3):247–253. | ||
Landmark J, Cernovsky ZZ, Merskey H. Correlates of suicide attempts and ideation in schizophrenia. Br J Psychiatry. 1987;151:18–20. | ||
Drake RE. Suicide attempts and completed suicides among schizophrenia patients. In: Tatarelli R, Pompili M, Girardi P, editors. Suicide in schizophrenia. New York: Nova Science Publishers Inc.; 2006. | ||
De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res. 2001;47(1–2):127–134. | ||
Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(Suppl 4):81–90. | ||
Kjelby E, Sinkeviciute I, Gjestad R, et al. Suicidality in schizophrenia spectrum disorders: the relationship to hallucinations and persecutory delusions. Eur Psychiatry. 2015;30(7):830–836. | ||
Ishii T, Hashimoto E, Ukai W, Kakutani Y, Sasaki R, Saito T. Characteristics of attempted suicide by patients with schizophrenia compared with those with mood disorders: a case-controlled study in northern Japan. PLoS One. 2014;9(5):e96272. | ||
Heila H, Isometsa ET, Henriksson MM, Heikkinen ME, Marttunen MJ, Lönnqvist JK. Suicide, and schizophrenia: a nationwide psychological autopsy study on age- and sex-specific clinical characteristics of 92 suicide victims with schizophrenia. Am J Psychiatry. 1997;154(9):1235–1242. | ||
Meltzer HY, Alphs L, Green AI, et al; International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry. 2003;60(1):82–91. | ||
Nordentoft M, Jeppesen P, Abel M, et al. OPUS study: suicidal behaviour, suicidal ideation, and hopelessness among patients with first-episode psychosis. Br J Psychiatry. 2002;181(Suppl):S98–S106. | ||
Farberow NL, Shneidman ES, Leonard CV. Suicide among schizophrenic mental hospital patients. In: Farberow NL, Shneidman ES, editors. The Cry for Help. New York: McGraw-Hill; 1961:78–109. | ||
Warnes H. Suicide in schizophrenics. Dis Nerv Syst. 1968;29(Suppl5):35–40. | ||
Drake RE, Gates C, Cotton PG. Suicide among schizophrenics: a comparison of attempters and completed suicide. Br J Psychiatry. 1986;149:784–787. | ||
Kim CH, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr Res. 2002;60:71–80. | ||
Bourgeois M, Swendsen J, Young F, et al; InterSePT Study Group. Awareness of disorder and suicide risk in the treatment of schizophrenia: results of the international suicide prevention trial. Am J Psychiatry. 2004;161(8):1494–1496. | ||
Latalova K, Prasko J, Kamaradova D, et al. Self-stigma and suicidality in patients with neurotic spectrum disorder – a cross sectional study. Neuro Endocrinol Lett. 2014;35(6):474–480. | ||
Shuwall M, Siris SG. Suicidal ideation in postpsychotic depression. Compr Psychiatry. 1994;35:132–134. | ||
Heilä H, Isometsä ET, Henriksson MM, Heikkinen ME, Marttunen MJ, Lönnqvist JK. Suicide victims with schizophrenia in different treatment phases and adequacy of antipsychotic medication. J Clin Psychiatry. 1999;60(3):200–208. | ||
Cem Atbasoglu E, Schultz SK, Andreasen NC. The relationship of akathisia with suicidality and depersonalization among patients with schizophrenia. J Neuropsychiatry Clin Neurosci. 2001;13(3):336–341. | ||
Sinclair JMA, Mullee MA, King EA, Baldwin DS. Suicide in schizophrenia: a retrospective case-control study of 51 suicides. Schizophr Bull. 2004;30(4):803–811. | ||
Wolfersdorf M, Keller F, Vogl R, Vogel R. An increase in patient suicide in Bavarian and Baden-Württemberg psychiatric and psychotherapy specialty hospitals? What are the long-term trends? Psychiatr Prax. 2003;30(Suppl 2):S181–S182. | ||
Hu WH, Sun CM, Lee CT, Peng SL, Lin SK, Shen WW. A clinical study of schizophrenic suicides. 42 cases in Taiwan. Schizophr Res. 1991;5(1):43–50. | ||
Westermeyer JF, Harrow M, Marengo J. Risk for suicide in schizophrenia and other psychotic and nonpsychotic disorders. J Nerv Ment Dis. 1991;179(5):259–266. | ||
Saarinen PI, Lehtonen J, Lönnqvist J. Suicide risk in schizophrenia: an analysis of 17 consecutive suicides. Schizophr Bull. 1999;25(3):533–542. | ||
Krupinski M, Fischer A, Grohmann R, Engel RR, Hollweg M, Moller HJ. Schizophrenic psychoses and suicide in the clinic. Risk factors, psychopharmacologic treatment. Nervenarzt. 2000;71(11):906–911. | ||
Zisook S, Byrd D, Kuck J, Jeste DV. Command hallucinations in outpatients with schizophrenia. J Clin Psychiatry. 1995;56(10):462–465. | ||
Melle I, Barrett EA. Insight and suicidal behavior in first-episode schizophrenia. Expert Rev Neurother. 2012;12(3):353–359. | ||
Nordentoft M, Madsen T, Fedyszyn I. Suicidal behavior and mortality in first-episode psychosis. J Nerv Ment Dis. 2015;203(5):387–392. | ||
Ventriglio A, Gentile A, Bonfitto I, Stella E, Mari M, Steardo L, Bellomo A. Suicide in the early stage of schizophrenia. Front Psychiatry. 2016;7:116. | ||
Tarrier N, Barrowclough C, Andrews B, Gregg L. Risk of non-fatal suicide ideation and behaviour in recent onset schizophrenia – the influence of clinical, social, self-esteem and demographic factors. Soc Psychiatry Psychiatr Epidemiol. 2004;39(11):927–937. | ||
Umut G, Altun ZO, Danismant BS, Kucukparlak I, Karamustafalioglu N, Ilnem MC. The correlation of suicide attempt and suicidal ideation with insight, depression and severity of illness in schizophrenic patients. Düşünen Adam. 2013;26(4):341–350. | ||
Yan F, Xiang YT, Hou YZ, et al. Suicide attempt and suicidal ideation and their associations with demographic and clinical correlates and quality of life in Chinese schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2013;48(3):447–454. | ||
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. | ||
McGirr A, Tousignant M, Routhier D, Pouliot L, Chawky N, Margolese HC, Turecki G. Risk factors for completed suicide in schizophrenia and other chronic psychotic disorders: a case-control study. Schizophr Res. 2006;84(1):132–143. | ||
Luckhoff M, Koen L, Jordaan E, Neihaus D. Attempted suicide in a Xhosa schizophrenia and schizoaffective disorder population. Suicide Life Threat Behav. 2014;44(2):167–174. | ||
Albayrak Y, Ekinci O, Cayköylü A. Temperament and character personality profile in relation to suicide attempts in patients with schizophrenia. Compr Psychiatry. 2012;53(8):1130–1136. | ||
Aukst Margetić B, Jakovljević M, Ivanec D, Marčinko D, Margetić B, Jakšić N. Current suicidality and previous suicidal attempts in patients with schizophrenia are associated with different dimensions of temperament and character. Psychiatry Res. 2012;30(2–3):120–125. | ||
Vrbova K, Prasko J, Holubova M, et al. Self-stigma and schizophrenia: a cross-sectional study. Neuropsychiatr Dis Treat. 2016;12:3011–3020. | ||
Vrbova K, Prasko J, Ociskova M, et al. Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr Dis Treat. 2017;13:567–576. | ||
Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. | ||
Mezinárodní klasifikace nemocí – 10. [International Clasification of Disorders - 10th revision]. revize, MKN-10 (1. vydání); Maxdorf Praha; 1996. Czech. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. DSM-5. Arlington: American Psychiatric Association; 2013. | ||
Guy W, editor. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD, USA: DHEW; 1976. | ||
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res. 2005;79(2–3):231–238. | ||
Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. | ||
Preiss M, Vacíř K. Beckova sebeposuzovací škála depresivity pro dospělé. [Beck self-rate scale for depression for adults]. BDI-II. Příručka. Brno: Psychodiagnostika; 1999. Czech. | ||
Ociskova M, Prasko J, Kupka M, et al. Psychometric evaluation of the Czech Beck Depression Inventory-II in a sample of depressed patients and healthy controls. Neuro Endocrinol Lett. 2017;38(2):98–106. | ||
Ritsher JB, Otilingam PO, Grajales M. Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Res. 2003;121(1):31–49. | ||
Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–265. | ||
Boyd JE, Adler EP, Otilingam PG, Peters T. Internalized Stigma of Mental Illness (ISMI) Scale: a multinational review. Compr Psychiatry. 2014;55(1):221–231. | ||
Ocisková M, Praško J, Kamarádová D, et al. Self-stigma in psychiatric patients – standardization of the ISMI scale. Neuro Endocrinol Lett. 2014;35(7):624–632. | ||
Snyder CR, editor. Handbook of hope: Theory, measures, and applications. New York: Academic Press; 2000. | ||
Ocisková M, Sobotková I, Praško J, Mihál V. Standardizace české verze Snyderovy škály naděje pro dospělé. [Standardization of Czech version of Snyder hope scale for adults]. Psychologie a Její Kontexty. 2016;7(1):109–123. Czech. | ||
Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987;22:141–173. | ||
Farmer RF, Goldberg LR. A psychometric evaluation of the revised Temperament and Character Inventory (TCI-R) and the TCI-140. Psychol Assess. 2008;20(3):281–291. | ||
Gillespie NA, Cloninger CR, Heath AC, Martin NG. The genetic and environmental relationship between Cloninger’s dimensions of temperament and character. Pers Individ Dif. 2003;35(8):1931–1946. | ||
Preiss M, Klose J. Diagnostika poruch osobnosti pomocí teorie C. R. Cloningera. [Diagnostics of personality disorders using theory of C.R. Cloninger]. Psychiatrie. 2001;5:226–231. Czech. | ||
EMEA. Note for guidance on clinical investigation of medicinal products in the treatment of depression. London, UK: EMEA; 2002. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003526.pdf. Accessed August 25, 2016. | ||
Češková E, Přikryl R, Pěč O. Schizofrenie u dospělých. [Schizophrenia in adults]. In: Raboch J, Uhlíková P, Hellerová P, Anders M, Šusta M, editors. Psychiatrie Doporučené postupy psychiatrické péče IV. Psychiatrická společnost ČSL JEP; 2014:44–51. Czech. | ||
Kiviniemi M, Suvisaari J, Pirkola S, Läksy K, Häkkinen U, Isohanni M, Hakko H. Five-year follow-up study of disability pension rates in first-onset schizophrenia with special focus on regional differences and mortality. Gen Hosp Psychiatry. 2011;33(5):509–517. | ||
Cassidy RM, Yang F, Kapczinski F, Passos IC. Risk factors for suicidality in patients with schizophrenia: a systematic review, meta-analysis, and meta-regression of 96 studies. Schizophr Bull. Epub 2017 Sep 23. | ||
Gajwani R, Larkin M, Jackson C. “What is the point of life?”: an interpretative phenomenological analysis of suicide in young men with first-episode psychosis. Early Interv Psychiatry. Epub 2017 Apr 18. | ||
Latalova K, Kamaradova D, Prasko J. Suicide in bipolar disorder: a review. Psychiatr Danub. 2014;26(2):108–114. | ||
Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatr Scand. 2006;113(3):180–206. | ||
Calati R, Giegling I, Rujescu D, Hartmann AM, Möller HJ, De Ronchi D, Serretti A. Temperament and character of suicide attempters. J Psychiatr Res. 2008;42(11):938–945. | ||
Mitsui N, Asakura S, Inoue T, et al. Temperament and character profiles of Japanese university student suicide completers. Compr Psychiatry. 2013;54(5):556–561. | ||
Goodwin R, Lyons JS, McNally RJ. Panic attacks in schizophrenia. Schizophr Res. 2002;58(2–3):213–220. | ||
Vrbova K, Prasko J, Ociskova M, Holubova M. Comorbidity of schizophrenia and social phobia – impact on quality of life, hope, and personality traits: a cross sectional study. Neuropsychiatr Dis Treat. 2017;13:2073–2083. | ||
Bellack AS, Mueser KT, Gingerich S, Agresta J. Social Skills Training for Schizophrenia: A Step-by-Step Guide. 2nd ed. Guilford Press: New York; 2004. | ||
Prasko J, Diveky T, Grambal A, et al. Narrative cognitive behavior therapy for psychosis. Act Nerv Super Rediviva. 2010;52(2):135–146. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.