Back to Journals » Psychology Research and Behavior Management » Volume 16
Suicidality and Its Association with Stigma in Clinically Stable Patients with Schizophrenia in Rural China
Authors Wang R , Zheng S, Ouyang X, Zhang S, Ge M, Yang M, Sheng X, Yang K, Xia L, Zhou X
Received 18 March 2023
Accepted for publication 18 May 2023
Published 29 May 2023 Volume 2023:16 Pages 1947—1956
DOI https://doi.org/10.2147/PRBM.S413070
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Ruoqi Wang,1– 3,* Siyuan Zheng,1– 3,* Xu Ouyang,1– 3 Shaofei Zhang,1– 3 Menglin Ge,1– 3 Meng Yang,1– 3 Xuanlian Sheng,1– 3 Kefei Yang,2,3 Lei Xia,2,3 Xiaoqin Zhou1– 3
1School of Mental Health and Psychological Sciences, Anhui Medical University, Hefei City, People’s Republic of China; 2Chaohu Hospital of Anhui Medical University, Hefei City, People’s Republic of China; 3Department of Psychiatry, Chaohu Hospital of Anhui Medical University, Hefei City, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoqin Zhou, Chaohu Hospital of Anhui Medical University, Hefei City, People’s Republic of China, Tel +8613865913378, Email [email protected]
Purpose: Patients with schizophrenia not only experience more stigma than those with other mental illnesses, but they also have a higher risk of committing suicide. There are, however, few research on the connection between rural individuals with clinically stable schizophrenia and suicidality when they feel stigmatized. Therefore, the purpose of this study was to look at the suicidality in clinically stable patients with schizophrenia in rural China, including the prevalence, clinical correlates, and its relationships with stigma.
Patients and Methods: From September 2022 to October 2022, we conducted a multicenter, cross-sectional study in rural Chaohu, Anhui Province, China, and A total of 821 patients with schizophrenia completed the assessment. Three standardized questions were used to assess suicidality (including suicidal ideation, suicide plan, and suicide attempt), Patient Health Questionnaire with 9 items (PHQ-9) for determining depressive state, the first two items of the World Health Organization Quality of Life Questionnaire-Brief Version (QOL), which measures quality of life, the Social Impact Scale (SIS) to assess stigma, and some other important variables (eg employment, psychiatric medication, etc.) were measured using a homemade scale.
Results: Of the 821 participants who completed the questionnaire, 19.2% of the patients were found to have suicidality, of which 19.2% (158/821) were suicidal ideation, 5.6% (46/821) were suicide plans and 4.5% (37/821) were suicide attempts. Binary logistic regression analysis showed that job status (OR=0.520, p=0.047), psychiatric medication (OR=2.353, p=0.020), number of hospitalizations (OR=1.047, p=0.042), quality of life (OR=0.829, p=0.027), PHQ-9 (OR=0.209, p< 0.001) stigma (OR=1.060, p< 0.001) and social isolation in stigma (OR=1.134, p=0.001) were associated independently with suicidality.
Conclusion: Among clinically stable schizophrenia patients in rural China, suicidality is frequent and associated with stigma. Since stigma and some risk factors have a negative impact on suicidality, we should conduct routine screening and take suicide prevention measures to clinically stable schizophrenia patients in rural areas of China.
Keywords: patients with schizophrenia, clinically stable, rural China, prevalence of suicidality, stigma
A Letter to the Editor has been published for this article.
Introduction
Around the world, suicide continues to be a serious issue, claiming 700,000 lives each year.1 However, before suicidal behavior can occur, there can be suicidality. Suicidality including suicidal ideation (SI), suicide plan (SP), suicide attempt (SA), and may ultimately lead to suicidal behavior.2 According to a meta-analysis, China has a lower rate of lifetime suicidal ideation (3.9%) and suicide attempts (0.8%) than Western nations. (S1:10%-20%; SA: 2–8%), probably because in traditional Chinese culture it is shameful to report suicidality, so these results must be considered with caution, they are likely to represent only the lowest of the SI and SA rates in China, and the potential population of SI and SA may be much larger than the survey data suggest.3 Even worse, compared to the general population, schizophrenia individuals have a 10–20-fold increased risk of suicidality,4 and hundreds of thousands of people with schizophrenia suffer from mental illness and eventually choose to commit suicide each year. According to previous studies, gender, marriage, work, depression and stigma are all associated with the development of suicidality.5 Therefore, a better understanding of the risk factors for suicidality in people with schizophrenia is necessary to manage the risk of suicide.
Due to the distinctive symptoms of the illness and outside prejudice, persons with schizophrenia frequently endure higher degrees of stigma than those with other mental diseases.6 Stigma is a disapproving or negative attitude toward a person with certain characteristic or illness that makes them appear to be at odds with others,7 and leads to social anxiety, despair, and psychotic symptoms (depression) in people with mental illness, and consequently reduces adherence to treatment.8 According to the study, 31.3% of people with SMI reported high levels of self-stigma, and the stigma often acts as a stressor,8 causing greater depression and despair in patients with internalized stigma, also resulting in more frequent suicidality9.
At the same time, people with schizophrenia in rural areas not only suffer from stigma, but may also face higher social pressure, poorer social cohesion, and less access to medical resources,10 and are therefore more likely to be suicidal. In order to better understand the frequency of suicidality among patients with schizophrenia in rural China, its relationship to stigma, and related risk factors, we performed this survey. This not only provides a new perspective on disease management and suicide prevention among clinically stable patients with schizophrenia in rural China, but also presents a realistic picture of stigma and suicidality among clinically stable patients with schizophrenia in rural China to other countries for international exchange and comparison.
Material and Methods
Participants and Procedure
During September to October 2022, a cross-sectional investigation including many centers was carried out, and the subjects are from rural areas of Chaohu City, Hefei City, Anhui Province, the ratio of the number of psychiatrists to the population in China is reported to be only 2.10 per 100,000 and the density of psychiatric beds in the region does not exceed 10 per 100,000,11 the per capita disposable income was only RMB 18,931,12 the incidence of poverty was 0.6%.13 Patients with schizophrenia in this region were registered in the database system for the management of severe mental disorders in Chaohu, Anhui Province. Over 3000 people were registered in this system, and we sent out 1101 questionnaires according to a 3:1 random stratified sample, with 821 valid returns, and all participants were screened according to the inclusion and exclusion criteria described below (Figure 1). After this survey was approved by the Ethics Committee of Chaohu Hospital, Anhui Medical University (KYXM-202212-013), we signed an informed consent form with the participants, in accordance with the Helgi Declaration, before completing the questionnaire to clarify the purpose of the survey and to ensure that patients’ personal privacy would not be disclosed.
 |
Figure 1 Flowchart of trial participation 1. |
The following eligibility requirements for inclusion and exclusion must be met by all participants. The inclusion criteria include: (1) The participant had a diagnosis of schizophrenia based on ICD-10; (2) Between the ages of 18 and 75; (3) The participants’ state right now is essentially stable: Patients in this research were deemed clinically stable if they had experienced less than a 50% change in their psychiatric medication during the previous three months;14(4) Capable of providing written information that is informed by the assessment’s objective and substance; (5) Living in rural areas of Chaohu. Exclusion criteria included: (1) Acute risk of alcohol, substance dependence, or violence; (2) Schizoaffective disorder, paranoid psychosis, bipolar disorder, mental disorders due to epilepsy, and mental retardation with mental disorders; (3) Serious physical disorders with a high risk of death; (4) Pregnant or lactating patients.
Measures
Demographic Characteristics
We refer to previous studies and use a self-made scale to evaluate demographic characteristics, including age, sex, BMI, marital status, education level, whether there is chronic disease, work status, whether smoking and drinking, number of hospitalizations, psychiatric medication use, etc. Of these, psychiatric medication use is divided into regular and irregular medication use. Those who take their medication as prescribed are considered to be taking it regularly, while those who do not take it regularly can be either intentional or unintentional, including failing to initially fill or refill a prescription, discontinuing a medication before completing the course of therapy, taking more or less of a medication than prescribed, and taking a dose at the wrong time.15 As almost all patients are accompanied by family members during this assessment, these basic information are very reliable.
Suicidality
Suicidality was evaluated by three standard questions that each required a “yes” or “no” response and inquired about suicidal ideation, suicide planning, and suicide attempts (eg, “Have you ever had any suicidal thoughts in the past year?”; “Have you ever made any preparations for suicide in the past year?”; and “Have you ever attempted suicide in the past year”). Patients are deemed “suicidal” if they respond “yes” to any one of these three questions.14 Here, recall bias was greatly decreased by only inquiring about recent suicide ideation rather than lifetime suicidal ideation.16
Stigma
The Social Impact Scale (SIS) is a labeling theory17 that incorporates four stigmatizing domains: internalized shame, financial insecurity, social isolation, and social rejection. According to the hypothesis, a lot of people form prejudice and discrimination against groups that have particular traits, which will internalize when people realize they are stigmatized and ultimately result in bad self-perceptions and life experiences.18 Each item’s score on the SIS ranged from 1 to 4, with a score of 4 denoting “strongly agree” and a score of 1 denoting “strongly disagree”. The SIS subscales’ Cronbach’s alpha values vary from 0.85 to 0.90, and the correlations between them are between 0.28 and 0.66. Greater SlS scores reflect perceived stigmatization at higher levels.
Depressive State
Patient Health Questionnaire-9 (PHQ-9): Over the course of two weeks, the PHQ-9’s nine items were used to gauge the severity of depression.19 The overall score varied from 0 to 27, while the individual item scores were 0 to 3. No or minimum depression was indicated by scores of 0–4, mild depression by scores of 5–9, moderate depression by scores of 10–14, major depression by scores of 15–19, and severe depression by scores of 20 or above. The Chinese version of the PHQ-9 has an internal consistency reliability score of 0.86 according to Cronbach’s alpha,20 and the scale is extensively used in China.21
Quality of Life
The quality of life (QOL) was assessed by summing the World Health Organization Quality of Life Questionnaire-brief version (the first two items),22 a self-assessment to understand patients’ current satisfaction with their quality of life and health status, with higher total scores indicating higher QOL.23 The Chinese version of the scale has satisfactory psychometric properties.24
Statistical Analysis
SPSS statistical software version 24.0 was used for data analysis. Chi-square test, double independent sample t-test or Mann–Whitney U-test were used to compare the differences between groups of patients with and without suicidality. For continuous variables, we use Mean ± Standard deviation (SD) to express, and for classified variables, we use percentage to describe.
The “enter” approach was used to construct a multiple factor logistic regression analysis to examine the independent correlation factors of suicidality utilizing variables with significant differences between single factor groups as the independent variable and suicidality as the dependent variable. P-values <0.05 was used as the significance threshold for all tests (two-sided).
Results
The Prevalence of Suicidality and Univariate Analysis of the Sociodemographic and Clinical Characteristics of Suicidality
In our study, which had 821 patients in total, we found that the incidence of suicidality was 19.2% (158/821), of which 19.2% (158/821) were suicidal ideation, 5.6% (46/821) were suicide plans and 4.5% (37/821) were suicide attempts. The sociodemographic and clinical characteristics of the patients are shown in Table 1. Female, married, suffering from chronic physical ailments, non-smoker, and the four stigma subscales were significantly linked with suicidality (all P values.05), according to univariate analyses.
 |
Table 1 Socio-Demographical and Clinical Characteristics of Patients |
Independent Correlates of Suicidality by Binary Logistic Regression Analysis
After adjusting for confounding variables, binary logistic regression analysis revealed that suicidality was correlated with employment (OR=0.520, p=0.047), psychiatric medication (OR=2.353, p=0.020), number of hospitalizations (OR=1.047, p=0.042), QOL score (OR=0.829, p=0.027), PHQ-9 (OR=0.209, p<0.001), stigma (OR=1.060, p<0.001) and social isolation in stigma (OR=1.134, p=0.001) (Table 2).
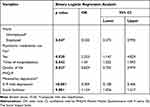 |
Table 2 Binary Logistic Regression Analysis for Associations with Suicidality |
Discussion
The province of Anhui is in the center of China, where 44.2% of the total population lives in rural areas,25 making its rural population representative throughout the country. Schizophrenia is a chronic psychotic disorder that can lead to severe disability, affect behavior, thinking and cognition, and have a huge impact on the health and lives of those affected.26 Not only that, but patients with schizophrenia can also experience a strong sense of stigma, which can lead to suicidality. This is the first time to look at the connection between stigma and suicidality among clinically stable patients with schizophrenia in rural China, and the prevalence of suicidality in this region was 19.2%. A previous meta-analysis showed that the global prevalence of suicidality among people with schizophrenia was 26.8% (95% CI 22.1–31.9%), approximately twice the prevalence of suicidality in China (14.6%, 95% CI 9.1–22.8%).27 In addition to being influenced by confounding factors, we also have to take into account the economic, political and cultural differences between countries around the world (eg in China, suicidality creates a sense of stigma for the patient, who therefore chooses to conceal it).28 The relative risk of suicidality is another three to four times higher in rural China compared to urban China, a situation that may be attributed to: a significantly higher risk of suicidality due to fewer mental health services, lack of medical knowledge, poverty, dependence on family caregivers, poor family attitudes towards relatives with schizophrenia and the strong stigma attached to mental illness in rural areas.29 Furthermore, according to the current findings, suicidal ideation was present in all patients with schizophrenia who also exhibited suicidality (19.2%), and therefore suicidal ideation may be a major predictor of suicidality in patients with schizophrenia.
According to previous meta-analyses, schizophrenia was the most common diagnosis in investigations of the impact of stigma on people with serious mental illness.30 Moreover, people with psychotic disorders often face higher levels of public stigma than people with non-psychotic disorders. Compared to Western countries, people with schizophrenia in China and India experience lower rates of stigma, but similar levels of self-stigma for people with schizophrenia.31 This may be because the actual rate is underestimated, as in the Chinese social hierarchy, face (also called “mianzi”), akin to vanity, is an important aspect of social identity, representing power and status.32 In addition, people with mental illness in rural areas often experience greater stigma and discrimination than those in urban areas,33 probably because people in rural areas are relatively isolated and do not understand the symptoms of mental illness, or even demonize them, seeing people with schizophrenia as evil like the “witches” of Western culture This may be due to the fact that people in rural areas do not understand the symptoms of mental illness and even demonize them, viewing patients with schizophrenia as evil beings like “witches” in Western culture. Furthermore, in rural China, a family member suffering from mental illness is considered to be an “invalid” and this is internalized as a sense of stigma. But all this is also due to poor education and resources.
For those who have schizophrenia and other mental diseases, stigma is a significant stressor34 that may cause severe psychological anguish and raise the risk of suicidality.35 Stigma’s impact on suicidality can be explained in a number of ways 1) In most agricultural areas of China, people with mental illness may suffer greater stigma and discrimination,36 leading to greater depression and hopelessness among patients with inherent stigma, and such depression may lead to higher prevalence of suicidality.9 In our study, the statistics of PHQ-9 also confirmed the independent correlation between depression and patients’ suicidal intention. However, whether depression mediates the relationship between schizophrenia and suicidality is worth further investigation. 2) Financial insecurity, internalized shame, social isolation, and social rejection are the four subscales of the SIS scale, and all of them can cause suicidality in patients with schizophrenia. In this study, we found that social isolation, one of the four subscales of morbidity stigma, was an independent risk factor for suicidality risk after excluding confounding factors, supporting earlier research.37 Determining the risk of those who exhibit suicidal ideation, attempt suicide, or engage in self-harm activity requires taking into account one’s experience of solitude;38 3) Research has also shown that insight is a double-edged sword, although high insight can make patients aware of the symptoms of their illness, at the same time, it can make patients with schizophrenia feel stigmatized,39,40 studies have shown that self-stigmatization mediates the relationship between insight and psychosocial outcomes in people with schizophrenia. Consequently, lowering self-stigma might aid in attenuating some of the negative effects of high insight on psychosocial outcomes in patients with schizophrenia,40 which was not explored in this study. Future research might examine this connection further.
In addition, we found a number of demographic characteristics in our study that were also associated with suicidality among the participants. 1) Women are more likely to become suicidal: According to the “gender paradox” theory, the suicide death rate of men exceeds that of women, but the incidence of suicidal ideation and behavior is higher in women than in men when it comes to suicidal intentions,41 suggesting that women may have worse mental health. 2) Married people are more likely to commit suicide: Women in rural areas of China, especially those with schizophrenia, often have poor social support and are even used as a fertility tool, thus committing suicide. Some studies have shown that marriage is a protective factor for suicidality,42 but this study found that married patients with schizophrenia have a higher prevalence of suicidality, and in Xiang,43 it was also shown that patients with suicidality are more likely to be married, which may be because among the schizophrenia group in rural areas, people with marital relationships have a lower degree of illness and more feeling of hopeless, and therefore more likely to commit suicide. In addition, negative factors in the marital relationship, such as rejection and hostility, can also become stressors, aggravating the condition of patients with schizophrenia and causing suicidality.10 3) Non-smokers are more likely to commit suicide: In this study, the suicidality rate of smokers (n=150,12.7%) was lower than that of non-smokers (n=671,20.7%), which may be because a large proportion of patients with schizophrenia are smokers. Studies have revealed44 that nicotine withdrawal can cause symptoms like irritability, depression, and anxiety. Furthermore, smoking cessation and reduction medications may interact with and impair the effectiveness of psychiatric medication routinely recommended for schizophrenia. Suicidality in these people may be a result of changes in their mental states brought on by any one of these symptoms.
After controlling for confounding factors, the following factors were independently associated with suicidality: 1) Psychiatric medication: The number of patients with schizophrenia in rural China (0.45%) was higher than that in urban areas (0.32%).45 In fact, due to factors such as family poverty and poor mental health services, many patients with schizophrenia cannot be admitted to hospital in time and receive regular psychiatric medication. However, this is an important means to prevent the suicidality of patients with schizophrenia in China. Therefore, it may have contributed to the high suicidality of the participants.29 2) Work: Nowadays, unemployment is harmful to people’s social status or self-esteem,20 and public discrimination and perceived humiliation may cause the unemployment of patients with schizophrenia.46 In our study, although they were unable to work due to the particularity of the disease itself, almost all of them expressed their desire to work, but owing to social rejection and discriminate, they were unable to work outside, which increased their stigma. Moreover, our study also confirmed that social rejection, one of the stigma subscales, was strongly correlated with suicidality in patients with refined scores. 3) Number of hospitalizations: Fleischhacker47 found that five or more hospitalizations were a significant variable in suicidality. Zhang48 also found an association between suicidality and multiple hospitalizations when assessing patients with schizophrenia. This is consistent with our findings, possibly because multiple hospitalizations not only reduce patients’ confidence in treatment, but also place a considerable burden on families in rural areas, which may also increase patients’ stigma. 4) Quality of life: Our findings, which are in part consistent with earlier research, showed that mental patients with low quality of life scores were also more likely to develop suicidality. Those with schizophrenia have lower quality of life than those with other diseases. Due to inadequate medical conditions in rural areas and the lack of attention paid by family members to patients’ physical conditions, many patients’ comorbidities are not discovered in time. However, this will further decrease the quality of life, physical and mental pain combined with the difficulty of seeking medical treatment in rural areas will finally lead to increased suicidality.36,49 Thus, a low level of quality of life can also be considered an indicator of suicidal behavior.50 5) Social isolation: Social isolation is one of the SIS subscales and is divided into subjective and objective. Either type of social isolation is a significant risk factor for the incidence of suicide and mental disorders,51 and when one is socially isolated, which means a loss of social interaction,52 one experiences social withdrawal or morbid stigma, and is more likely to become suicidal because of the isolation that comes with social isolation.53
However, there are several drawbacks that should be aware of. First of all, only schizophrenia in the clinically stable period in the Chaohu area of Anhui Province was included in this study, and it is impossible to speculate whether rural areas in other parts of Anhui Province or other provinces are consistent with this study, and for safety reasons, we only limit patients in the clinically stable period, and the study settings and samples are not fully representative of the entire population of patients with schizophrenia. Second, cross-sectional studies can only explore their correlations, which means that causality cannot be inferred like longitudinal studies, and future studies can use cohort studies to enhance the accuracy of the factors influencing this study. Third, the accuracy of the self-assessment scale for patients with schizophrenia needs to be discussed: In our evaluation process, patients with negative symptoms at present answered “NO” for most question in the scale, which may not be consistent with the real situation, and this part of data may have an impact on the research results. Fourth, this paper used the PHQ-9 to rate depression in patients with schizophrenia, but the PHQ-9 is mostly used as a screening test and lacks specificity, whereas the Calgary Depression Scale can be used to differentiate depressive symptoms from negative symptoms in schizophrenia,54 which would make the results more precise and should be assessed using a more precise scale in future studies. Fifth, whether there was an interaction between depression and stigma was not mentioned in the current study, which may have an impact on the findings and should be discussed in detail in the next study.
Conclusion
In conclusion, by investigating the relationship between suicidality and stigma among clinically stable schizophrenic patients in rural China, we found that the incidence of suicidality and the degree of stigma are lower in China than in Western countries, but this does not mean that the potential risk for schizophrenic patients in the Chinese region is small, but rather provides us with the lowest value of risk for research and comparison in different countries and cultures. At the same time, the low level of suicidality and stigma in urban areas of China compared to rural areas suggests that we need to focus on suicidality prevention for patients in rural areas. This study suggests that this group of patients bears a significant stigma burden, which not only significantly increases the risk of suicidality among people with mental disorders, but we can also speculate that a large proportion of this group may be reluctant to seek medical attention due to stigma and therefore never be diagnosed and treated. Stigma, psychiatric medication use, work status, hospitalization and quality of life are all closely related to suicidality, and therefore a series of targeted measures should be taken to reduce suicidality in this group and thus prevent suicides from occurring. 1) strengthen mental health education to reduce public discrimination and the stigma of patients themselves; 2) provide employment opportunities for people with mental illness; 3) establish a relationship with patients to prevent suicidality; 3) Establishing family alliances with patients so as to increase medication compliance and reduce hospitalization; 4) Improving patients’ quality of life by requiring psychiatrists to pay attention to patients’ physical illnesses during treatment, in addition to recommending that the government strengthen relevant family support policies; 5) Given the lack of health resources in rural areas of China, primary health care workers should receive further training in order to provide basic mental health treatment in rural 5) Given the inadequate health resources in rural areas of China, primary health care workers should receive further training to provide basic mental health treatment in rural areas.29
Abbreviations
SIS, The Social Impact Scale; PHQ-9, Patient Health Questionnaire with 9 items; QOL, Quality of life; BMI, Body Mass Index; SI, suicidal ideation; SP, suicide plan; SA, suicide attempt; SD, Standard deviations; CI, confidence interval.
Data Sharing Statement
A data set that can be obtained from the corresponding author ([email protected]) upon reasonable request.
Ethics Approval and Informed Consent
The survey strictly followed the principles of the Helsinki Declaration and was approved by the Ethics Committee of Chaohu Hospital affiliated to Anhui Medical University (KYXM-202212-013). Before filling in the questionnaire, we informed the participants of the purpose of the study and guaranteed that their personal privacy would not be disclosed, and signed an informed consent form with the participants.
Acknowledgments
The author would like to thank Mr. Ouyang Xu, Mr. Zhang Shaofei, Ms. Sheng Xuanlian, Ms. Ge Menglin and Ms. Yang Meng for their contributions to data collection.
Funding
No allowance is provided in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sarraf L, Lepage M, Sauvé G. The clinical and psychosocial correlates of self-stigma among people with schizophrenia spectrum disorders across cultures: a systematic review and meta-analysis. Schizophr Res. 2022;248:64–78. doi:10.1016/j.schres.2022.08.001
2. Li YC, Bai W, Cai H, et al. Suicidality in clinically stable bipolar disorder and schizophrenia patients during the COVID-19 pandemic. Transl Psychiatry. 2022;12(1):303. doi:10.1038/s41398-022-02045-2
3. Cao XL, Zhong BL, Xiang YT, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. 2015;49(4):296–308. doi:10.1177/0091217415589306
4. Patel V, Saxena S. Transforming lives, enhancing communities--innovations in global mental health. N Engl J Med. 2014;370(6):498–501. doi:10.1056/NEJMp1315214
5. Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15(2):127–135. doi:10.1177/026988110101500209
6. Zahid A, Best MW. Stigma towards individuals with schizophrenia: examining the effects of negative symptoms and diagnosis awareness on preference for social distance. Psychiatry Res. 2021;297:113724. doi:10.1016/j.psychres.2021.113724
7. Yuan Y, Zhao YJ, Zhang QE, et al. COVID-19-related stigma and its sociodemographic correlates: a comparative study. Global Health. 2021;17(1):54. doi:10.1186/s12992-021-00705-4
8. Jian CR, Wang PW, Lin HC, et al. Association between self-stigma and suicide risk in individuals with schizophrenia: moderating effects of self-esteem and perceived support from friends. Int J Environ Res Public Health. 2022;19(22):15071. doi:10.3390/ijerph192215071
9. Touriño R, Acosta FJ, Giráldez A, et al. Suicidal risk, hopelessness and depression in patients with schizophrenia and internalized stigma. Actas Esp Psiquiatr. 2018;46(2):33–41.
10. Luo Y, Pang L, Guo C, Zhang L, Zheng X. Association of urbanicity with schizophrenia and related mortality in China: association de l’urbanicité avec la schizophrénie et la mortalité qui y est reliée en Chine. Can J Psychiatry. 2021;66(4):385–394. doi:10.1177/0706743720954059
11. TEAM W. World health statistics 2015; 2015.
12. 中华人民共和国国务院 [The State Council, The People's Republic of China]. 2021年居民收入和消费支出情况 [Resident income and consumer spending in 2021]. Available from: http://www.gov.cn/xinwen/2022-01/17/content_5668748.htm.
13. NBo, Statistics. Statistical bulletin on national economic and social development of the people’s republic of china 2019. China Stat. 2020;459(3):8–22.
14. Liu R, Xu X, Zou S, et al. Prevalence of suicidality and its association with quality of life in older patients with clinically stable psychiatric disorders in china during the COVID-19 pandemic. J Geriatr Psychiatry Neurol. 2022;35(2):237–244. doi:10.1177/08919887221078557
15. Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. 2020;9(1):17. doi:10.1186/s13643-020-1274-3
16. Dai J, Zhong BL, Xiang YT, et al. Internal migration, mental health, and suicidal behaviors in young rural Chinese. Soc Psychiatry Psychiatr Epidemiol. 2015;50(4):621–631. doi:10.1007/s00127-014-0985-y
17. Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–190. doi:10.2307/2955424
18. Link B. Mental patient status, work, and income: an examination of the effects of a psychiatric label. Am Sociol Rev. 1982;47(2):202–215. doi:10.2307/2094963
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
20. Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. doi:10.1016/j.genhosppsych.2014.05.021
21. Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17(10):1.
22. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–558. doi:10.1017/S0033291798006667
23. Skevington SM, Tucker C. Designing response scales for cross-cultural use in health care: data from the development of the UK WHOQOL. Br J Med Psychol. 1999;72(Pt 1):51–61. doi:10.1348/000711299159817
24. Jiang XI. 青少年生命质量量表 (YQOL-R) 的汉化研究 [A study on the Chineseization of the Youth Quality of Life Scale (YQOL-R)] [Master‘s thesis]. [硕士], 浙江大学 [Zhejiang University]; 2014. Chinese.
25. Yang JJ, Cai H, Xia L, et al. The prevalence of depressive and insomnia symptoms, and their association with quality of life among older adults in rural areas in China. Front Psychiatry. 2021;12:727939. doi:10.3389/fpsyt.2021.727939
26. Srivastava A, Dada O, Qian J, et al. Epigenetics of Schizophrenia. Psychiatry Res. 2021;305:114218. doi:10.1016/j.psychres.2021.114218
27. Lu L, Dong M, Zhang L, et al. Prevalence of suicide attempts in individuals with schizophrenia: a meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2019;29:e39. doi:10.1017/S2045796019000313
28. Dong M, Wang SB, Wang F, et al. Suicide-related behaviours in schizophrenia in China: a comprehensive meta-analysis. Epidemiol Psychiatr Sci. 2019;28(3):290–299. doi:10.1017/S2045796017000476
29. Ran MS, Xiao Y, Fazel S, et al. Mortality and suicide in schizophrenia: 21-year follow-up in rural China. BJPsych Open. 2020;6(6):e121. doi:10.1192/bjo.2020.106
30. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–2161. doi:10.1016/j.socscimed.2010.09.030
31. Dubreucq J, Plasse J, Franck N. Self-stigma in serious mental illness: a systematic review of frequency, correlates, and consequences. Schizophr Bull. 2021;47(5):1261–1287. doi:10.1093/schbul/sbaa181
32. Li J, Guo YB, Huang YG, et al. Stigma and discrimination experienced by people with schizophrenia living in the community in Guangzhou, China. Psychiatry Res. 2017;255:225–231. doi:10.1016/j.psychres.2017.05.040
33. Jin Y, Zhang YS, Zhang Q, et al. Corrigendum: prevalence and socio-demographic correlates of poor mental health among older adults in agricultural areas of China. Front Psychiatry. 2021;12:664145. doi:10.3389/fpsyt.2021.664145
34. Komatsu H, Ono T, Onoguchi G, Tomita H, Kakuto Y. Mediating effects of self-stigma and depression on the association between autistic symptoms and recovery in patients with schizophrenia-spectrum disorders: a cross-sectional study. BMC Psychiatry. 2021;21(1):464. doi:10.1186/s12888-021-03472-z
35. Kudva KG, El Hayek S, Gupta AK, et al. Stigma in mental illness: perspective from eight Asian nations. Asia Pac Psychiatry. 2020;12(2):e12380. doi:10.1111/appy.12380
36. Jin Y, Zhang YS, Zhang Q, et al. Prevalence and socio-demographic correlates of poor mental health among older adults in agricultural areas of China. Front Psychiatry. 2020;11:549148. doi:10.3389/fpsyt.2020.549148
37. Lu Y, Sun M, Li Y, et al. Association of workplace bullying with suicide ideation and attempt among Chinese nurses during the COVID-19 pandemic. J Clin Psychol Med Settings. 2022;2022:1–10.
38. Farooq S, Tunmore J, Wajid Ali M, Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. 2021;306:114228. doi:10.1016/j.psychres.2021.114228
39. Lysaker PH, Vohs J, Hillis JD, et al. Poor insight into schizophrenia: contributing factors, consequences and emerging treatment approaches. Expert Rev Neurother. 2013;13(7):785–793. doi:10.1586/14737175.2013.811150
40. Mak WW, Wu CF. Cognitive insight and causal attribution in the development of self-stigma among individuals with schizophrenia. Psychiatr Serv. 2006;57(12):1800–1802. doi:10.1176/ps.2006.57.12.1800
41. Eisenlohr-Moul TA, Bowers SM, Prinstein MJ, et al. Effects of acute estradiol and progesterone on perimenstrual exacerbation of suicidal ideation and related symptoms: a crossover randomized controlled trial. Transl Psychiatry. 2022;12(1):528. doi:10.1038/s41398-022-02294-1
42. Berardelli I, Rogante E, Sarubbi S, Erbuto D, Lester D, Pompili M. The importance of suicide risk formulation in schizophrenia. Front Psychiatry. 2021;12:779684. doi:10.3389/fpsyt.2021.779684
43. Yan F, Xiang YT, Hou YZ, et al. Suicide attempt and suicidal ideation and their associations with demographic and clinical correlates and quality of life in Chinese schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2013;48(3):447–454. doi:10.1007/s00127-012-0555-0
44. Tsoi DT, Porwal M, Webster AC. Interventions for smoking cessation and reduction in individuals with schizophrenia. Cochrane Database Syst Rev. 2013;2013(2):Cd007253. doi:10.1002/14651858.CD007253.pub3
45. Liu T, Zhang L, Pang L, Li N, Chen G, Zheng X. Schizophrenia-related disability in China: prevalence, gender, and geographic location. Psychiatr Serv. 2015;66(3):249–257. doi:10.1176/appi.ps.201400032
46. Oshodi YO, Abdulmalik J, Ola B, et al. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):259–266. doi:10.1007/s00127-013-0737-4
47. Fleischhacker WW, Kane JM, Geier J, et al. Completed and attempted suicides among 18,154 subjects with schizophrenia included in a large simple trial. J Clin Psychiatry. 2014;75(3):e184–190. doi:10.4088/JCP.13m08563
48. Zhang XY, Al Jurdi RK, Zoghbi AW, et al. Prevalence, demographic and clinical correlates of suicide attempts in Chinese medicated chronic inpatients with schizophrenia. J Psychiatr Res. 2013;47(10):1370–1375. doi:10.1016/j.jpsychires.2013.05.024
49. Fässberg MM, Cheung G, Canetto SS, et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment Health. 2016;20(2):166–194. doi:10.1080/13607863.2015.1083945
50. Pîrlog MC, Alexandru DO, Popescu RE, et al. Quality of life-a goal for schizophrenia’s therapy. Curr Health Sci J. 2018;44(2):122–128. doi:10.12865/CHSJ.44.02.05
51. Andreu-Bernabeu Á, Díaz-Caneja CM, Costas J, et al. Polygenic contribution to the relationship of loneliness and social isolation with schizophrenia. Nat Commun. 2022;13(1):51. doi:10.1038/s41467-021-27598-6
52. Porcelli S, Van Der Wee N, van der Werff S, et al. Social brain, social dysfunction and social withdrawal. Neurosci Biobehav Rev. 2019;97:10–33. doi:10.1016/j.neubiorev.2018.09.012
53. Pješčić KD, Nenadović MM, Jašović-Gašić M, Trajković G, Kostić M, Ristić-Dimitrijević R. Influence of psycho-social factors on the emergence of depression and suicidal risk in patients with schizophrenia. Psychiatr Danub. 2014;26(3):226–230.
54. Porter L, Jones C, Fox A. Reliability of the Calgary depression scale for schizophrenia: a meta-analysis. Schizophr Res. 2022;240:32–45. doi:10.1016/j.schres.2021.11.040
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
