Back to Journals » Journal of Pain Research » Volume 16
Sufentanil Improves the Analgesia Effect of Continuous Femoral Nerve Block After Total Knee Arthroplasty
Authors Dong J , Jin Z, Chen H, Bao N, Xia F
Received 28 May 2023
Accepted for publication 21 October 2023
Published 7 December 2023 Volume 2023:16 Pages 4209—4216
DOI https://doi.org/10.2147/JPR.S409668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Jiaojiao Dong,* Zhousheng Jin,* Hongfei Chen, Nana Bao, Fangfang Xia*
Department of Anesthesiology, The First Affiliated Hospital, Wenzhou Medical University, Wenzhou, Zhejiang Province, 325000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fangfang Xia, Department of Anesthesiology, The First Affiliated Hospital, Wenzhou Medical University, Shangcai Village, Nanbaixiang Town, Ouhai District, Wenzhou, Zhejiang Province, 325000, People’s Republic of China, Email [email protected]
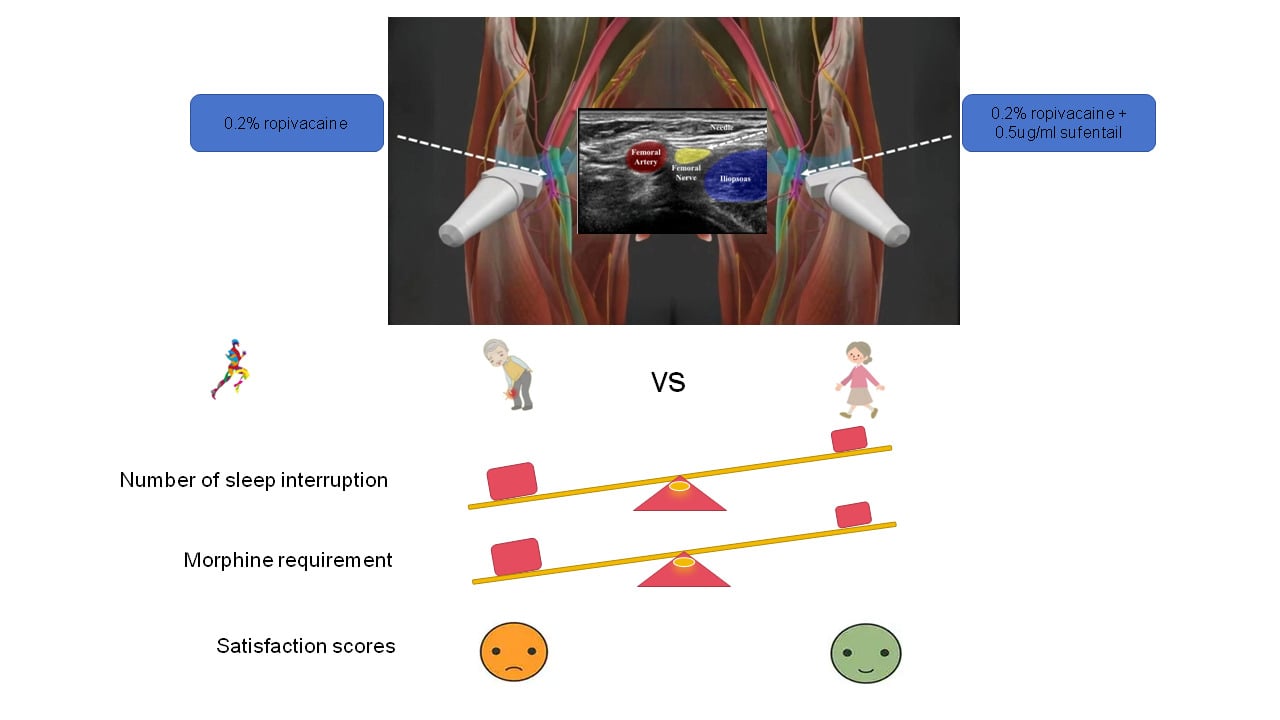
Purpose: We examined whether the addition of sufentanil to local anesthetics improves the quality of continuous femoral nerve block in patients undergoing total knee arthroplasty (TKA).
Patients and Methods: With institutional ethical approval and having obtained written informed consent from each, 35 patients scheduled for elective bilateral TKA with ASA I or II physical status were studied. Bilateral femoral perineural catheters were preoperatively inserted. Both-sided catheters were randomly assigned to receive perineural ropivacaine of 0.2% plus 0.5μg/mL sufentanil deemed as RS group or 0.2% ropivacaine alone deemed as R group at the end of surgery. Visual analogue pain scores (VAS) during activity and at rest of each lower limb were recorded at 6,12,18,24,30,36,42 and 48h after surgery. During the first 48 postoperative hours, the number and reason of patients sleep interruption at night, the number of painful compressions, patient satisfaction and morphine requirements were recorded for each lower limb of patients.
Results: Pain scores of RS group on movement were significantly lower than R group, but no difference was noted at rest. When compared to R group, RS group had a lower incidence of sleep interruption at night, fewer painful compressions, higher satisfaction scores and less morphine requirement.
Conclusion: The addition of sufentanil to ropivacaine improved analgesia quality of continuous femoral nerve block after arthroplasty.
Keywords: continuous femoral nerve block, ultrasound guidance, total knee arthroplasty, analgesia, ropivacaine
Graphical Abstract:
Introduction
Knee arthritis is a disease based on degenerative pathological changes. The main manifestations are pain, movement disorders, simultaneous involvement of both knee joints, and poor conservative treatment effect.1 The main types include osteoarthritis, rheumatoid arthritis, metabolic arthritis, and traumatic arthritis. Total knee arthroplasty (TKA) is one of the most effective surgical treatment methods for pain relief and functional recovery in patients with end-stage knee arthritis.2 With the maturity of artificial TKA, TKA has achieved good results. Strictly grasping the surgical indications for bilateral TKA can avoid two surgeries, shorten recovery time, reduce medical costs, and ensure good safety. Research has confirmed that there were no significant differences in the incidence of complications between bilateral TKA and unilateral TKA.3,4
The postoperative pain of TKA is severe, and patients need active functional exercise at an early stage. Therefore, effective postoperative analgesia is very important to improve the function of the prosthetic joint.5 At present, the analgesic methods mainly include patient controlled intravenous analgesia, epidural analgesia, postoperative analgesia of lumbar plexus, postoperative continuous analgesia of femoral nerve and so on.6–10
Due to the large side effects of intravenous opioid analgesia, patients are poorly tolerated,11 while TKA patients often receive prophylactic anticoagulant therapy, which limits the use of epidural analgesia. In recent years, continuous femoral nerve block (cFNB) has been considered as a safe and effective analgesic method,12 which can promote patients’ early activity. Low concentrations of ropivacaine may lead to insufficient postoperative analgesia.13,14 Brodner et al demonstrated that using 0.1% ropivacaine in cFNB cannot provide effective analgesic effects, even with increased volume.14 Research has shown that in order to achieve good postoperative analgesic effects, high concentrations or doses of ropivacaine are often required, but this may affect the strength of the quadriceps femoris muscle, making it difficult for patients to move effectively.15 In previous studies, 0.2% ropivacaine was most commonly used for cFNB.16–18 Previous studies have shown that opioid drugs such as fentanyl, morphine, and other composite local anesthetics can enhance the analgesic effect of low concentration local anesthetics.19–21 Scholars believe that opioids may produce local effects through peripheral receptors: increasing Ca2+ conduction and reducing K+ conduction in sensory neurons,22 reducing excitability of nociceptive neurons, and inhibiting the release of excitatory neurotransmitter P.23 Neuroplexus administration can trigger central effects: opioid binding proteins transport opioid drugs from the periphery to the dorsal horn of the spinal cord.24,25 Additionally, local absorption into the bloodstream cannot be ruled out to produce central analgesic effects. In addition, as a commonly used powerful opioid analgesic, sufentanil can quickly exert analgesic effects when administered intravenously, and its analgesic effect is superior to that of fentanyl and morphine, with fewer related side effects. However, there is little research on the use of sufentanil combined with local anesthetics for peripheral nerve block.
We hypothesized that sufentanil could act locally to improve the postoperative analgesic effect of local anesthesia in cFNB. Therefore, this study selected patients who planned to receive bilateral TKA and adopted the self-controlled study method to evaluate the effect of sufentanil on the analgesic effect of ropivacaine in cFNB, so as to clarify whether sufentanil can be used to enhance the analgesic effect of local anesthesia, so as to provide clinical reference.
Materials and Methods
Patients and Enrollment
The study protocol was approved by the independent Ethics Committee at the First Affiliated Hospital of Wenzhou Medical University (April 6, 2017/No. 2017–115). It was also registered with Chinese Clinical Trial Registry under the number ChiCTR-TRC-12002537. The study adhered to the World Medical Association’s Declaration of Helsinki. Data are presented in accordance with the Consolidated Standards. Figure 1 summarizes the design of the study. Inclusion criteria were as follows: whose age was 53~82y, weight was 47~81kg, height was 150~179cm, ASA I or II, and scheduled for bilateral TKA between June 2017 and January 2018. A total of 47 patients were assessed for eligibility for the study. Exclusion criteria were as follows: allergy to local anesthetics, chronic opioid usage, coagulopathy, presence of infection at the planned injection site, peripheral neurologic or neuromuscular disease, severe liver or renal insufficiency and an inability to comprehend study-related procedures. All patients were taught to assess the degree of pain using a visual analogue.
 |
Figure 1 Enrollment and randomization of the subject. |
Conduction of Anesthesia
All patients were sent to the nerve block preparation room one hour before the operation. Bilateral femoral perineural catheters were inserted in patients placed supine, monitored with electrocardiogram, pulse oximetry, and non-invasive blood pressure. All patients were administered oxygen by a nasal cannula (3L/min). Intravenous access was also obtained. Before anesthesia, all patients received intravenous premedication (midazolam 1 or 2mg plus fentanyl 50μg) to produce sedation while ensuring that study subjects remained responsive to verbal cues.
Using a 13–6MHz 38mm linear array transducer (HFL38, MicroMaxx; SonoSite, USA) with a sterile sleeve, the femoral nerve was identified in a transverse cross-sectional (short axis) view at the inguinal crease and adjusted to obtain the best image of the femoral nerve. A local anesthetic skin wheal was raised lateral to the ultrasound transducer. A stimulating needle [a Stimulong Plus Plexolong Catheter Set (Pajunk, Germany) was used with a 19-G × 50-mm stimulating needle and 20-G × 50-cm stimulating catheter] was inserted through the skin wheal with an in-plane technique under ultrasound guidance toward the femoral nerve. The stimulating needle was advanced with the initial stimulator current set at 0.8mA, 2Hz, and 0.3ms (Stimuplex HNS11; Braun, Germany) until quadriceps femoris muscle contractions were elicited (cephalad patellar movements). The needle was kept in place if quadriceps muscle contractions were elicited at a current of 0.3mA or less. A total of 10mL 5% dextrose (D5W) was injected to facilitate catheter insertion. With the catheter tip remaining visualized by ultrasound to ensure that its position remained fixed under femoral nerve when the needle was withdrawn over the remaining catheter, and the puncture point was sutured to fix catheter (like the fixation of the drainage tube after surgery). Adhesive tape and application were used to strengthen the fixation. 4mL of 2% lidocaine was injected through the femoral nerve catheter. After 10 min, sensory block of the femoral nerve was assessed by evaluating the presence or loss of a sharp sensation with pinprick testing (20-G needle) delivered at the central sensory region of the femoral nerve, anterior to the patella. One would be excluded from the study, if bilateral inserting was fail. After the manipulation above, patients were sent to the operating room for anesthesia and surgery.
Intraoperative Anesthesia and Study Groups
All patients took lateral position. The subarachnoid puncture was performed at the L3-L4 inter-vertebral space with hyperbaric solution including 0.5% bupivacaine 3mL (0.75% bupivacaine 2mL and 10% glucose 1mL), controlling the level at T6-8. Patients who were nervous intraoperative were given midazolam 1 or 2mg plus fentanyl 50μg. If the spinal anesthesia fail, change to general anesthesia and be excluded from the study.
The operations were performed with a tourniquet. After doing a 12cm incision in the middle of the front of the knee, TKA implant (P.F. C SIGM A Total Knee System, DePuy UK, Leeds) was placed, fixed with bone cement. A drainage tube was used and the knee joint was bandaged postoperatively. Patients were observed in a postoperative room after surgery. Patients acted as their own controls: Using a computer-generated sequence of random numbers and a sealed envelope, the right side was randomly assigned to receive ropivacaine of 0.2% plus 0.5μg/mL sufentanil deemed as RS group or 0.2% ropivacaine deemed as R group, the left catheter receiving the alternative solution deemed as R group or RS group. When the level of anesthesia declines to L1, both knees of all patients were connected to analgesia pumps (Shanghai Bo Gen Medical Equipment Co., LTD) randomly, with continuous infusion of 5mL/h. The infusion pumps were labeled as either “left” or “right” so that subjects could self-administer a bolus to the necessary side. The electronic display was covered with opaque medical tape to mask treatment assignments. All patients received patient-controlled analgesia (PCA) morphine (Shenyang first pharmaceutical factory, China), using a 2mg bolus and a 5-minute lockout period, and 1 hour maximum was 10mg. Patients had been taught to use the PCA to make the visual analogue scale (VAS) score <3 at rest. All patients were intravenous injected parecoxib 40mg postoperative, 2 times a day and enoxaparin 20mg subcutaneous once the first morning after operation.
Assessments and Data Collection
The intensity of postoperative pain was assessed using the VAS score, at 6, 12, 18, 24, 30, 36, 42, 48h after surgery, ranging from 0 (no pain) to 10 (extreme pain), both at rest and during activity (when the knee was bended 30 degrees). The number of sleep interruption because of each side of the lower limb pain during the night after surgery and the number of painful compressions of the analgesic pump connected to the femoral nerve and morphine consumption in the 48h post operation were also recorded. Patient degree of satisfaction about the analgesia of each side of the lower limb was recorded with 4 grades, very satisfied as 4, generally satisfied as 3, moderately satisfied as 2, unsatisfied as 1.
Sample Size Calculation
The primary endpoint was the VAS score for pain during activity after surgery. In the preliminary study, the VAS score for pain during activity was 1.7 ± 0.7 for limbs receiving 0.2% ropivacaine plus 0.5μg/mL sufentanil and 2.4 ± 1.0 for limbs receiving 0.2% ropivacaine alone, respectively, at 24h after surgery. Assuming a type I two-tailed error of 5% and power of 0.80, a sample size of 26 patients per group was calculated. To compensate for dropouts, 35 patients were included.
Statistical Analysis
SPSS 19.0 statistical software was used for statistical analysis. The Shapiro–Wilk test was used for normality of data distribution. The normal distribution measurement data were expressed as mean ± SD, and the skewed distribution measurement data were expressed as median (interquartile range). Morphine consumption were compared using one-way ANOVA. VAS scores and patient satisfaction scores after surgery were compared by repeated measures ANOVA. Values for the number of sleep interruption and the number of painful compression were analyzed with the Kruskal–Wallis H-test. Values of P < 0.05 were considered significant.
Results
A total of 47 patients were assessed for eligibility for the study. Twelve patients were excluded due to the exclusion criteria, and 5 patients were excluded due to unsuccessful femoral nerve catheterization. Ultimately, 30 patients were included in the experiment and followed up. A CONSORT checklist was used for patient enrollment and allocation, as shown in Figure 1.
The patient’s age, gender, height and weight, ASA score and other general indicators are shown in Table 1. At 6, 12, 18, 24, 30, 36, 42 and 48h postoperative, there was no statistical difference in the VAS scores of both sides of the lower limb at rest time, but the VAS scores of the RS group were significantly lower than those of the R group during the activity time (P < 0.05), as shown in Figure 2. At 6–48 hours after surgery, patient satisfaction with analgesia in the RS group was significantly higher than that in the R group (P < 0.05), as shown in Figure 3.
 |
Table 1 The General Situation |
Postoperative patients were treated with PCA for supplementary analgesia. The use of morphine in RS group was significantly lower than that in R group on the first and second day after surgery (P < 0.05), as shown in Figure 4A and B.
In addition, the number of sleep interruption caused by postoperative pain at night on the day of surgery was 3 (2) times in the R group and 1 (1) times in the RS group, and 0 (1) times in the RS group and 2 (3) times in the R group at night on the first day after surgery, with statistically significant differences between groups (P < 0.05).
The number of compressions of the analgesic pump connected to the femoral nerve was 6 (4) times in the R group and 2 (1) times in the RS group on the first day after surgery, 4 (2) times in the R group and 1 (0) times in the R group on the second day after surgery, and the difference between groups was statistically significant (P < 0.05).
Patients were followed up 30 days after surgery, and no neurological complications were observed in both groups.
Discussion
The purpose of this study was primarily to determine whether sufentanil could enhance the analgesic effect of ropivacaine and whether the effect could be achieved through local action. The results showed that (1) VAS score in RS group was significantly lower than that in R group; (2) The satisfaction of analgesia in RS group was significantly higher than that in R group; (3) The use of morphine in RS group was significantly lower than that in R group on the first and second postoperative days; (4) The number of sleep interruption and painful compressions on the first postoperative day in RS group was significantly lower than that in R group; (5) During follow-up 30 days after discharge, no neuro-related complications were observed.
The results showed that VAS score in RS group was significantly lower than that in R group, suggesting that sufentanil can improve the analgesic effect of ropivacaine in cFNB after TKA. This study selected patients were bilateral TKA surgery, patients with bilateral femoral nerve connections of different formulations of continuous femoral nerve analgesia pump, so that we can insight its controlled analgesia effect, eliminate sufentanil or other analgesics systemic effect of analgesic effect. This study adopts a self-controlled study that can eliminate individual differences, improve the internal validity of the study, reduce experimental errors, and provide more accurate explanations to the experimental results.
Similar to our study, Nishikawa’s study demonstrated that the addition of opioid fentanyl to lidocaine solution for axillary brachial plexus block can improve the success rate and prolong the duration of analgesia.26 Similarly, Elmawgoud27 compared the postoperative analgesia of 0.2% ropivacaine and 0.2% ropivacaine combined with 4ug/mL fentanyl for TKA, and found that the combined group could significantly enhance the analgesic effect of ropivacaine and reduce the intravenous use of opioids. However, Fanelli28 found that the addition of 0.75% ropivacaine to 1ug/mL fentanyl could not improve the nerve block characteristics of axillary brachial plexus anesthesia. In his study, patients receiving fentanyl and ropivacaine did not differ in intraoperative analgesia and the duration of the first postoperative analgesia from those receiving ropivacaine alone. Similarly, Bouaziz29 found that the addition of 1.5% mepivacaine to 5ug, 10ug or 20ug sufentanil did not accelerate the onset of axillary nerve bundle block or prolong its duration. However, we think Fanelli’s study differs from ours in that he used a higher concentration of 0.75% ropivacaine and the same Bouaziz study used a higher concentration of mepivacaine. High local anesthetic onset time, analgesic effect and maintenance time are long, which may mask the effect of fentanyl, and such concentration does not conform to the concept of quick postoperative recovery. Overall, our results suggest that opioids combined with low concentration local anesthetics are more effective for postoperative analgesia.
The results of this study showed that in the resting state, there was no statistical difference between the VAS score of RS group and R group. This was because the wound pain of patients in the resting state was not so intense, so the simple local anesthetic block effect could have a good analgesic effect, which led to no difference in analgesic effect between the two groups. However, the focus of postoperative rehabilitation after knee surgery lies in early exercise. In this experiment, the motion pain score of RS group was significantly lower than that of R group, which is more meaningful for patients undergoing knee surgery.
The results of our study were self-controlled and showed that sufentanil locally enhanced the analgesic effect of ropivacaine. This is similar to Nishikawa’s study26 which found that fentanyl enhances the analgesic effect of lidocaine through a peripheral mechanism. Previous animal experiments have demonstrated that peripheral opioid receptors exist in immune cells and primary afferent neurons.30 In addition, opioids can not only activate peripheral opioid receptors,31 but also produce analgesic effects by inhibiting sodium channels.32 These mechanisms may explain the effect of sufentanil on local analgesia.
In addition, our results showed that addition of sufentanil not only reduced intravenous morphine use but also improved analgesia satisfaction and sleep quality during activity. The study also showed no neurological complications associated with topical sufentanil use. This suggests that sufentanil may be a beneficial method for peripheral analgesia. But more research is needed.
Of course, this study also has some limitations. Firstly, the sample size of this experiment was relatively small, which was due to the small number of patients requiring bilateral TKA. However, we found significant differences between the results of the two groups during the experiment, so the experimental results are relatively reliable. Secondly, although the pain of TKA mainly originates from the femoral nerve, it also originates from some sciatic nerve branches and the lateral femoral cutaneous nerve. Therefore, the cFNB we used could not completely cover the painful nerve. In recent years, the development of iliac fascia block has been rapid, as the femoral nerve, lateral femoral cutaneous nerve, and pelvic segment of obturator nerve located below the iliac fascia. A breakthrough in this direction will significantly reduce postoperative pain and increase patient satisfaction in TKA patients. Therefore, the related research on the impact of continuous iliac fascia block on postoperative pain after TKA is the direction of our team’s future research.
Conclusion
In conclusion, compared with 0.2% ropivacaine, cFNB analgesia with 0.2% ropivacaine combined with 0.5μg/mL sufentanil can improve postoperative analgesia effect, improve patient satisfaction and reduce morphine use after TKA. At the same time, the study demonstrated that sufentanil’s effect was activated through the periphery.
Funding
Zhejiang Provincial Natural Science Foundation of China (LWQ20H310001).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Huang D, Liu YQ, Liang LS, et al. The diagnosis and therapy of degenerative knee joint disease: expert consensus from the Chinese pain medicine panel. Pain Res Manag. 2018;2018. doi:10.1155/2018/2010129
2. Krumov J, Obretenov V, Bozov H, et al. Is group-based physical therapy superior to individual rehabilitation in elderly adults after total knee arthroplasty? A prospective observational study. Eur J Transl Myol. 2022;32(4):10984. doi:10.4081/ejtm.2022.10984
3. Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty - A survival analysis. J Bone Joint Surg Am. 2003;85a(8):1532–1537. doi:10.2106/00004623-200308000-00015
4. Wang XL, Zhang L, Li HC, Bian T, Zhou YX, Li YJ. Predisposing factors for allogeneic blood transfusion in patients with rheumatoid arthritis undergoing primary unilateral total knee arthroplasty. Front Surg. 2023;10. doi:10.3389/fsurg.2023.1205896
5. Freccero DM, Van Steyn P, Joslin PMN, et al. Continuous femoral nerve block reduces the need for manipulation following total knee arthroplasty. JB JS Open Access. 2022;2022:1.
6. Fu PL, Xiao J, Zhu YL, et al. Efficacy of a multimodal analgesia protocol in total knee arthroplasty: a randomized, controlled trial. J Int Med Res. 2010;38(4):1404–1412. doi:10.1177/147323001003800422
7. Hasegawa M, Singh D, Urits I, et al. Review on nerve blocks utilized for perioperative total knee arthroplasty analgesia. Orthop Rev. 2022;14(3):37405. doi:10.52965/001c.37405
8. Davies AF, Segar EP, Murdoch J, Wright DE, Wilson IH. Epidural infusion or combined femoral and sciatic nerve blocks as perioperative analgesia for knee arthroplasty. Br J Anaesth. 2004;93(3):368–374. doi:10.1093/bja/aeh224
9. Pathonsamit C, Onklin I, Hongku N, Chaiyakit P. Randomized double-blind controlled trial comparing 0.2 mg, 0.1 mg, and no intrathecal morphine combined with periarticular injection for unilateral total knee arthroplasty. Arthroplast Today. 2021;7:253–259. doi:10.1016/j.artd.2020.11.008
10. Hadzic A, Houle TT, Capdevila X, Ilfeld BM. Femoral nerve block for analgesia in patients having knee arthroplasty. Anesthesiology. 2010;113(5):1014–1015. doi:10.1097/ALN.0b013e3181f4b43d
11. Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology. 2014;120(3):540–550. doi:10.1097/ALN.0000000000000119
12. Farag E, Atim A, Ghosh R, et al. Comparison of three techniques for ultrasound-guided femoral nerve catheter insertion: a randomized, blinded trial. Anesthesiology. 2014;121(2):239–248. doi:10.1097/ALN.0000000000000262
13. Zhang YJ, Liu L, Zheng LY, et al. Comparison of effectiveness of ropivacaine infusion regimens for continuous femoral nerve block for recovery after total knee arthroplasty: a randomized double-blind trial. J Pain Res. 2020;13:997–1005. doi:10.2147/Jpr.S247158
14. Brodner G, Buerkle H, Van Aken H, et al. Postoperative analgesia after knee surgery: a comparison of three different concentrations of ropivacaine for continuous femoral nerve blockade. Anesth Analg. 2007;105(1):256–262. doi:10.1213/01.ane.0000265552.43299.2b
15. Bauer M, Wang L, Onibonoje OK, et al. Continuous femoral nerve blocks decreasing local anesthetic concentration to minimize quadriceps femoris weakness. Anesthesiology. 2012;116(3):665–672. doi:10.1097/ALN.0b013e3182475c35
16. Gandhi HJ, Trivedi LH, Tripathi DC, Dash DM, Khare AM, Gupta MU. A randomized, controlled trial of comparison of a continuous femoral nerve block (CFNB) and continuous epidural infusion (CEI) using 0.2% ropivacaine for postoperative analgesia and knee rehabilitation after total knee arthroplasty (TKA). J Anaesthesiol Clin Pharmacol. 2019;35(3):386–389. doi:10.4103/joacp.JOACP_134_16
17. Babu SC, Menon G, Vasu BK, George M, Thilak J, Lyer S. Postoperative ultrasound guided continuous femoral nerve blockade for unilateral total knee arthroplasty: a comparison of 0.125% bupivacaine and 0.2% ropivacaine. Anesth Essays Res. 2017;11(4):1026–1029. doi:10.4103/aer.AER_155_17
18. Sztain JF, Machi AT, Kormylo NJ, et al. Continuous adductor canal versus continuous femoral nerve blocks relative effects on discharge readiness following unicompartment knee arthroplasty. Region Anesth Pain M. 2015;40(5):559–567. doi:10.1097/Aap.0000000000000279
19. Prabhakar A, Lambert T, Kaye RJ, et al. Adjuvants in clinical regional anesthesia practice: a comprehensive review. Best Prac Res-Cl Ana. 2019;33(4):415–423. doi:10.1016/j.bpa.2019.06.001
20. Axelsson K, Gupta A. Local anaesthetic adjuvants: neuraxial versus peripheral nerve block. Curr Opin Anesthesio. 2009;22(5):649–654. doi:10.1097/ACO.0b013e32832ee847
21. Candido KD, Winnie AP, Ghaleb AH, Fattouh MW, Franco CD. Buprenorphine added to the local anesthetic for axillary brachial plexus block prolongs postoperative analgesia. Region Anesth Pain M. 2002;27(2):162–167. doi:10.1053/rapm.2002.30671
22. Schroeder JE, Fischbach PS, Zheng D, McCleskey EW. Activation of mu opioid receptors inhibits transient high- and low-threshold Ca21 currents, but spares a sustained current. Neuron. 1991;6(1):13–20. doi:10.1016/0896-6273(91)90117-i
23. Yaksh TL. Substance P release from knee joint afferent terminals: modulation by opioids. Brain Res. 1988;458(2):319–324. doi:10.1016/0006-8993(88)90474-x
24. Laduron PM. Axonal transport of opiate receptors in capsaicin-sensitive neurones. Brain Res. 1984;294(1):157–160. doi:10.1016/0006-8993(84)91322-2
25. Laduron PM, Janssen PFM. Axonal transport and possible recycling of opiate receptors labelled with 3H lofentanil. Life Sci. 1982;31(5):457–462. doi:10.1016/0024-3205(82)90331-9
26. Nishikawa K, Kanaya N, Nakayama M, Igarashi M, Tsunoda K, Namiki A. Fentanyl improves analgesia but prolongs the onset of axillary brachial plexus block by peripheral mechanism. Anesth Analg. 2000;91(2):384–387. doi:10.1097/00000539-200008000-00028
27. Elmawgoud MA, Elkassem SA, Rashwan D, Rashwan D. Effect of addition of magnesium sulphate and fentanyl to ropivacaine continuous femoral nerve block in patients undergoing elective total knee replacement. J Med Sci. 2008;73(4):395–399. doi:10.3923/jms.2008.395.399
28. Fanelli G, Casati A, Magistris L, et al. Fentanyl does not improve the nerve block characteristics of axillary brachial plexus anaesthesia performed with ropivacaine. Acta Anaesthesiol Scand. 2001;45(5):590–594. doi:10.1034/j.1399-6576.2001.045005590.x
29. Bouaziz H, Kinirons BP, Macalou D, et al. Sufentanil does not prolong the duration of analgesia in a mepivacaine brachial plexus block: a dose response study. Anesth Analg. 2000;90(2):383–387. doi:10.1097/00000539-200002000-00027
30. Brejchova J, Holan V, Svoboda P. Expression of opioid receptors in cells of the immune system. Int J Mol Sci. 2020;22(1):315. doi:10.3390/ijms22010315
31. Stein C, Lang LJ. Peripheral mechanisms of opioid analgesia. Curr Opin Pharmacol. 2009;9(1):3–8. doi:10.1016/j.coph.2008.12.009
32. Haeseler G, Foadi N, Ahrens J, Dengler R, Hecker H, Leuwer M. Tramadol, fentanyl and sufentanil but not morphine block voltage-operated sodium channels. Pain. 2006;126(1–3):234–244. doi:10.1016/j.pain.2006.07.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



