Back to Journals » Journal of Inflammation Research » Volume 16
Subfatin, Asprosin, Alamandine and Maresin-1 Inflammation Molecules in Cardiopulmonary Bypass
Authors Hanbeyoglu O, Aydin S
Received 25 May 2023
Accepted for publication 11 August 2023
Published 16 August 2023 Volume 2023:16 Pages 3469—3477
DOI https://doi.org/10.2147/JIR.S422998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Onur Hanbeyoglu,1 Suna Aydin2– 4
1Department of Anesthesiology, Fethi Sekin City Hospital, Elazig, Turkiye; 2Department of Cardiovascular Surgery, Fethi Sekin City Hospital, Elazig, Turkiye; 3Department of Anatomy, School of Medicine, Firat University, Elazig, Turkiye; 4Department of Histology and Embryology, School of Veterinary Medicine, Firat University, Elazig, Turkiye
Correspondence: Suna Aydin, Department of Cardiovascular Surgery, Fethi Sekin City Hospital, No: 99, Elazig, Turkiye, Email [email protected]
Purpose: Cardiopulmonary bypass (CPB) is a nonphysiological procedure in which inflammatory reactions and oxidative stress are induced, hormones and hemodynamic parameters are affected, and circulation is maintained outside the body. This study aimed to examine the effects of CPB on blood subfatin (SUB), asprossin (ASP), alamandine (ALA) and maresin-1 (MaR-1) levels.
Materials and Methods: Controls and patients who underwent open-heart surgery with CPB and whose age and body mass indices were compatible with each other were included in the study. Venous blood samples were collected from CPB patients (n =19) before anesthesia induction (T1), before CPB (T2), 5 min before cross-clamp removal (T3), 5 min after cross-clamp removal (T4), when taken to the intensive care unit (T5), postoperative 24th hour (T6) and 72nd hour (T7) postoperatively. Venous blood was collected from the healthy controls (n =19). The amounts of SUB, ASP, ALA, and MaR-1 in the blood samples were measured using an Enzyme-Linked Immunosorbent Assay (ELISA).
Results: The amounts of SUB and MaR-1 in the control group were significantly higher than those in CPB patients, while these parameters in T1-T3 blood gradually decreased in CPB patients (p< 0.01). It was also reported that the amounts of ASP and ALA in the control group were significantly lower than those in CPB patients, whereas those parameters in the T1-T3 blood samples increased gradually in CPB patients, but started to decrease in T4-T7 blood samples.
Conclusion: These hormonal changes in the organism due to CPB demonstrate that “hormonal metabolic adaptation” mechanisms may be activated to eliminate the negative consequences of surgery. According to these data, SUB, MaR-1, anti-alamandine, and anti-asprosin could be used in CPB surgeries may come to the fore in the future to increase the safety of CPB surgeries.
Keywords: subfatin, maresin-1, asprosin, alamandine, cardiopulmonary bypass
Introduction
Cardiopulmonary bypass (CPB) is a non-physiological event in which circulation is maintained from outside the body to facilitate surgical intervention and provide a more effective intervention in cardiac surgery, leading to numerous pathophysiological changes in the body systems.1,2 In other words, systemic inflammatory and endocrine responses occur through many pathways such as cytokines, coagulation-fibrinolysis cascade, endothelium, and cellular immune system.1,3,4 The contact of blood with a non-physiological surface during CPB surgery specifically triggers systemic inflammatory reaction syndrome (SIRS).5
Subfatin (Meteorin-like= Metrnl) is a protein synthesized mainly from white adipose tissue.6 However, subfatin (SUB) has been reported to be expressed in brain tissue, activated human monocytes, liver, spleen, thymus gland, omental adipose tissue, subcutaneous adipose tissue, salivary glands, interscapular adipose tissue, muscle tissue, and heart tissues.7–9 SUB regulates glucose metabolism by reducing insulin resistance. It has been reported that insulin resistance develops when mice lacking SUB gene are fed a high-fat diet.10 In a study, it was reported that the decrease in SUB level may cause a decrease in metabolic activity, prevent adequate energy production, and therefore increase oxidative stress in patients.11 In addition, SUB is a molecule that plays a role in the elimination of inflammation.8 It has not yet been clarified how stress and inflammation due to cardiopulmonary bypass surgery are reflected in the amounts of SUB in circulation.
Maresin-1 (MaR 1 or 7R, 14S-dihydroxy-4Z,8E,10E,12Z,16Z,19Z-docosahexaenoic acid) is produced from docosahexaenoic acid (DHA) by monocyte-macrophage cell types12 In vitro and in vivo studies show that Maresin-1 (MaR-1) increases the solubility of inflammation, inhibits the inflammatory response, contributes to tissue regeneration, and accelerates wound healing.13,14 Endothelial plates of the vessels are damaged due to inflammation.15 MaR-1 administration to experimental animals has been reported to prevent tumor necrosis factor (TN) a-induced monocyte adhesion and reactive oxygen species (ROS) formation in the vascular endothelial.16 MaR-1 exerts its effects on smooth muscle cells by upregulating cyclic adenosine monophosphate (cAMP) and downregulating transcription factor nuclear transcription factor kappa B (NF-κβ).17 Vascular injuries activate the reshaping of vessels.18 This leads to inflammation in the endothelial cells and causes neointima, that is, re-occlusion of blood vessels. Systemic administration of MaR-1 reduced neointimal formation and prevented blood vessels from occlusion again.17
Asprosin (ASP) is a polypeptide hormone consisting of 140-amino acids, which are formed as the C-terminal cleavage product of profibrillin (FBN1), which was first detected in 2016 by a group of researchers19 during a study on individuals with neonatal progeria syndrome (NPS-neonatal Marfan lipodystrophy).19 Progeria disease is associated with FBN1 gene mutation (ie, asprosin deficiency), and individuals with progeria have hypophagia and their subcutaneous fat tissues are not well developed.20 ASP is secreted by white adipose tissue in response to fasting. The main function of asprosin is to increase hepatic glucose production. This hormone crosses the blood-brain barrier, causing appetite stimulation and an increase in adipocyte tissue and body weight, through the activation of agouti-related protein (AgRP+) neurons and the consequent inhibition of Pro-opiomelanocortin (POMC+) neurons.19 ASP is higher in the circulation of insulin resistant obese mice and humans compared to healthy organisms.21,22 ASP shows all these effects by activating G protein-cAMP- protein kinase A (PKA) pathway.22 ASP has been reported to also have inflammatory effects.23 It has been reported that a decrease in the level of ASP in circulation leads to a decrease in metabolic activity and induces oxidative stress in patients.22,24 Many metabolic pathways such as glucose metabolism affect cardiopulmonary bypass patients. Hence, it would be beneficial to investigate whether ASP plays a role in this surgical procedure.
Alamandine (ALA) is a heptapeptide hormone that consists of alanine (Ala), arginine (Arg), valine (Val), tyrosine (Tyr), isoleucine (Ile), histidine () and proline (Pro). This hormone is a new member of the renin-angiotensin system (RAS), which is involved in homeostasis of the cardiovascular system (water and electrolyte balance).25,26 ALA can be directly derived from angiotensin- (1–7), and can also be formed as a product of angiotensin-converting enzyme 2 (ACE2)-dependent catalytic hydrolysis of angiotensin A. ALA, similar to angiotensin- (1–7), is a hormone with vasodilation, antifibrosis, and antihypertensive effects. Different receptors have been used to demonstrate these biological effects. For instance, while ALA Mas-related G-protein-coupled receptor type D (MrgD) is used in these biological effects, angiotensin- (1–7) uses RAS, Mas, and angiotensin II type 2 receptors.27 In addition to the biological effects mentioned above, administration of ALA reduces aortic narrowing, regulates cardiac contractility, growth, and apoptosis.28 Thus, finding out the fate of ALA, which has a strict role in ensuring the homeostasis of the cardiovascular system in cardiopulmonary CPB surgery, will shed light on the response of the cardiovascular system to bypass surgery.
Hence, this study aimed to reveal how the amounts of SUB, MaR-1, ASP, and ALA are affected in blood samples taken from patients who underwent open-heart surgery with CPB at various times during surgery and postoperatively.
Materials and Methods
Study Design and Population
This case-control study focused on coronary artery bypass graft (CABG) surgery with CPB (7.6. 2022 and September 1, 2022) after obtaining the approval of the Clinical Research and Ethics Committees of Firat University (2022/08-19 issue and date 7.6-2022) and this study was conducted in accordance with the principles of the Declaration of Helsinki, and all patients provided written informed consent prior to enrolment. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines are shown in Figure 1. Patients with previously known chronic obstructive pulmonary disease (COPD) and liver disease, patients with acute MI (acute myocardial infarction: heart attack), patients with diabetes mellitus, patients with renal failure, malignancies, reoperation, preoperative steroid treatment, patients with a history of hypo-hyperthyroidism, patients with cardiac cachexia, morbid obesity (body mass index= (BMI) > 38 kg/m2), patients with a history of use of tobacco products (smoke, chew, or sniff tobacco), patients under 18 years of age and over 75 years of age, patients with active infection and patients with a history of previous cerebrovascular disease were excluded from the study. CPB patients were administered metoprolol tartrate (a beta1-selective (cardioselective) adrenergic antagonist) to treat supraventricular tachyarrhythmias, angina pectoris, cardiac arrhythmias, and hypertension. The patients (CPB) were also taking a blood-thinner drug (acetylsalicylic acid). The patients (CPB) were also taking antihypertensive medications (furosemide-diuretic or ramipril angiotensin-converting enzyme (ACE) inhibitor) until they were taking metoprolol tartrate. Hyperlipidemia was defined as fasting total serum cholesterol > 200 mg/dL, LDL cholesterol > 130 mg/dL, serum TG > 180 mg/dL, or the use of lipid-lowering drugs (atorvastatin) if necessary. Atorvastatin is a statin that lowers “bad” cholesterol. Other details are listed in Table 1.
 |
Table 1 Certain Demographic Characteristics and Biochemical Parameters of the Participants |
 |
Figure 1 Flowchart of participants’ progress through the phases of the trial. |
Anesthetic Application and Hemodynamic Parameters
For monitoring hemodynamic parameters, a central venous catheter was inserted through the jugular vein and Swan-Ganz catheter was inserted through the femoral artery before anesthetic induction in the Cardiovascular Surgery Operating Room as described before.29 Anesthetic induction and maintenance were performed as standard in all patients. The hemodynamic parameters measured in the Cardiovascular Surgery Operating Room were pulse heart rate (HR), mean arterial pressure (MAP), mean pulmonary arterial pressure (MPAP), and central venous pressure (CVP).
Anesthesia and Cardiopulmonary Bypass
Total intravenous general anesthesia with fentanyl (Fentanyl® 0.05 mg/mL, Johnson and Johnson Tic. Ltd. Sti. Beykoz, Istanbul), and propofol (PROPOFOL-PF® 1200 mg/20 mL IV, POLIFARMA Ilaç San. ve Tic. A.S, Ergene, Tekirdag) was administered to the participants and maintained (anesthetic gases were not used). After the patient relaxed with rocuronium bromide (Muscuron ® 50 mg/5 mL, Kocak Farma Ilac. San. A.S, Bagcılar, Istanbul) tracheal intubation was performed, and controlled normocapnic ventilation was initiated with an air-oxygen mixture. 200–300 IU/kg heparin dose was given to participants who underwent the operation. Cardiopulmonary bypass was performed as previously described using ascending aortic cannulation and two-stage venous cannulation in the right atrium.29 The CPB circuit consisted of pipes (Cardiovascular Cannula, Shanghai International Holding Corp. GmbH, Hamburg, Germany) without an arterial line filter, with a crystalloid-colloid mixture, heparin, membrane oxygenator, and centrifugal pump (SORIN C5 Heart Lung Machine SORIN GROUP, Munchen, Germany). During aortic cross-clamping, intermittent cold blood cardioplegia is used for myocardial protection. Protamine was administered at the end of surgery to completely reverse the effect of heparin.
Collection of Biological Samples
From the CPB patients (n = 19) who participated in the study, 5 mL of venous blood was collected as described before anesthesia induction (T1), before CPB (T2), 5 min before cross-clamping (T3), 5 min after cross-clamping (T4), when taken to intensive care (T5), at postoperative 24th hour (T6) and 72nd hour (T7) in seven periods, and 5 mL of venous blood was collected from healthy individuals (n = 19) who agreed to participate in the study, as previously described, after fasting overnight.30 These bloods were centrifuged at 4000 revolution per minute (RPM) for 5 min. The obtained plasma was divided into five equal parts and stored at −40 °C until analysis in Eppendorf tubes. Blood biochemical parameters (serum calcium, potassium, sodium, and glucose levels) were obtained from the hospital records. These (Serum) parameters were measured using an autoanalyser (AU5800; Beckman Coulter, Tokyo, Japan).
Measurements of Molecules with Enzyme Linked Immunosorbent Assay (ELISA)
Meteorin-like Protein (SUB) (SunRed, Biological Technology Co., Catalog no: SRB-T-81862 Shanghai, CHINA), ALA (SunRed, Biological Technology Co., Catalog no: DZE201125722 Shanghai, CHINA), ASP (Bioassay Technology Laboratory Catalog no: E4095Hu Shanghai, CHINA), and MaR-1 (SunRed, Biological Technology Co., Shanghai, CHINA) were studied by ELISA using an ELISA kit according to the manufacturer’s instructions. The absorbance was read spectrophotometrically at 450 nm using a ChroMate Microplate Reader P4300 (Awareness Technology Instruments, USA) ELISA reader. A Bio-TEK ELX50 (BioTek Instruments, USA) automatic washer was used to wash the plates. The measurement range of the SUB kit was 0.05–15 ng/mL, with a minimum measurable level of 0.023 ng/mL. The measurement range of the ASP kit was 0.5–100 ng/mL, and the minimum measurable level was 0.23 ng/mL. The measuring range of the ALA kit was 1.5 pg/mL and 400 pg/mL, and the minimum measurable level was 1.368 pg/mL. The measurement range for the MaR-1 kit is 0.01–1.5 ng/mL. While the intra-assay coefficient of variation (CV) of the kits was <10%, the inter-assay CV was <15%.
Statistical Analyses
All statistical analyses were performed with computer package (SSPS-22) package. Two-way analysis of variance (two-Ways) was used for intergroup comparisons of study data. Pearson’s correlation analysis was used to determine the relationships between SUB, ASP, ALA, MaR-1, and other variables. p<0.05 was considered significant at the 95% confidence interval.
Results
When the demographic characteristics of the participants included in the study were evaluated, no statistical differences were observed in terms of the mean age, BMI, glucose, calcium, potassium, and sodium levels (Table 1). The operative characteristics of the CPB patients are summarized in Table 2. Given the change in time-dependent hemodynamic data of CPB patients, the lowest CVP value was reported at T4, the lowest HR value was reported at T2, and the lowest MAP value was reported at T3, whereas no significant time-dependent changes were found in MPAP and pulmonary capillary wedge pressure (PCWP) values (Table 3). The CVP value decreased slightly in the pre-cardiopulmonary bypass interval and continued to decrease again for 5 min before the cross-clamp was placed (values were not considered because the heart was stopped with cardioplegia and reset when the cross was placed). As the pulse was zero during T3 (as the heart was stopped by cardioplegia) in cardiopulmonary bypass surgery, it was not included in the statistical analysis. When CPB patients were admitted to the intensive care unit, a horizontal course in the HR value was observed. Based on the examination of the mean MPAP changes in the patients, while the MPAP value before anesthesia induction was 20–25 mmHg, there was a slight decrease in the pre-cardiopulmonary bypass interval 5 min before the cross-clamp was placed, and the decrease stopped 5 min after the cross-clamp was performed (Table 3). When the patients’ pulmonary PCWP changes were examined preoperatively, it was observed that while the PCWP value before anesthesia induction was 15 mmHg, it decreased in the pre-CPB interval, increased again 5 min before the cross-clamp was placed, and reached the level before anesthesia induction (Table 3). History of drug use in patients with cardiopulmonary bypass (CPB) and control were also shown in Table 4.
 |
Table 2 Operative Characteristics of CPB Patients |
 |
Table 3 Change in Hemodynamic Data of Patients Over Time |
 |
Table 4 History of Drug Use in Patients with Cardiopulmonary Bypass (CPB) and Control |
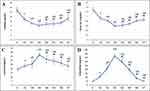
When the SUB (Figure 2A) and MaR-1 (Figure 2B) values of the control group were compared with the preoperative values of the CPB patients, SUB and MaR-1 of the control group were found to be significantly higher. The SUB (Figure 2A) and MaR-1 (Figure 2B) values of CPB patients decreased significantly from T1 to T3. The largest decreases in the SUB (Figure 2A) and MaR-1 (Figure 2B), ASP (Figure 2C) values were observed in the blood samples taken at T3. A significant increase was recorded in the blood samples collected after T3, which was between T4 and T7 including T4, a significant increase was recorded. A contrary situation was observed in ASP and ALA changes. When the ASP (Figure 2C) and ALA (Figure 2D) values of the control group were compared with the preoperative values of CPB patients, the ASP and ALA values of the control group were found to be significantly lower. The ASP (Figure 2C) and ALA (Figure 2D) values of the CPB patients gradually increased significantly from T1 to T3. The greatest increases in ASP (Figure 2C) and ALA (Figure 2D) were observed in the blood samples taken at T3. In the blood samples collected after T3, from T4 to T7 including T4, a decrease was observed.
When hemodynamic data of the CPB participants were examined, the correlations of SUB–CVP (r:0.386; p:0.01), MaR-1–CVP (r:0.394; p:0.01), SUB–MAP (r:0.413, p:0.01), and MaR-1–MAP (r:0.437, p:0.01) were observed at T3, while negative correlations of ASP–CVP (r: −0.397; p:0.01), ALA–CVP (r:0.408; p:0.01), ASP–MAP (r: −0.462, p:0.01), and ALA–MAP (r:- 0.437, p:0.01) were observed in the same period. Additionally, compared with the control group, an inverse correlation was observed between SUB–ASP (r: −0.652; p:0.01), MaR-1–ASP (r: −0.488; p:0.01), SUB–ALA (r: −0.652; p:0.01), MaR-1–ALA (r: −0.503; p:0.01).
Discussion
In this study, we evaluated the kinetics of plasma SUB, ASP, ALA, and MaR-1 levels over various periods in patients who underwent open-heart surgery via CPB. In this study, control blood subfatin values were found to be significantly higher than those in CPB patients, whereas a decrease was reported in blood SUB values taken at T1, T2, and T3 as progression from T1 to T3. In the periods after the completion of CPB, the amount of SUB increased in the blood samples collected at T4–T7. These results indicate that CPB surgery alters the circulating levels of hormones. Additionally, the decrease in SUB levels during CPB surgery shows that organisms tend to conserve energy and minimize metabolism to survive. As calorie restriction in animals leads to a decrease in the amount of SUB, it has been reported to be related to conserving energy and minimizing metabolism for survival.8
In this study, when the control blood MaR-1 values and T1 (basal) T2 and T3 values of CPB patients were compared, it was reported that the MaR-1 values gradually decreased significantly. However, the amount of MaR-1 in the blood samples increased on the 1st and 3rd day after CPB surgery, but this increase was not statistically significant. Occlusion or narrowing of coronary vessels increases inflammation.31 In other words, chronic inflammation is one of the main causes of atherosclerosis.32 The fact that the MaR-1 values of CPB patients were lower than the control values may be one of the causes of vascular occlusion in these patients. This is because physiological doses of MaR-1 have been reported to inhibit the progression of atherosclerosis by reducing the necrosis and macrophages accumulation in atherosclerosis area, as well as the fibrous thickness of smooth muscle cells.33 Again, the possible reason for the low T1 (basal) values and also the low MaR-1 values in blood samples taken at T1, T2, and T3 time periods of CPB patients, may be the increase in inflammation due to CBP surgery and the decrease in the amount of MaR-1, a potent endogenous anti-inflammatory molecule, in the circulation by being consumed by the organism to eliminate this inflammation.13 Studies have reported that administration of MaR-1 reduced inflammation.34,35 This decrease in MaR-1 amounts in response to surgical stress may also affect other physiological pathways closely. Given the available data, the use of MaR-1 may be considered in the future to eliminate inflammation due to CPB surgery or other surgical operations.
In this study, the ASP values in blood samples collected from CPB patients during and after CPB were significantly higher than the control blood values. In addition, the ASP values in the blood samples taken from T1 to T3 in CPB patients increased over time. ASP levels have been reported to increase in coronary artery disease.36,37 When the ASP levels in the early hours of ischemic heart disease and the values after coronary angiography were compared, it was reported that the ASP values also increased after coronary angiography.36 Thus, we suggesting with our current data that the restoration of blood flow at a physiological level by bypass in CPB patients may cause an increase in asprosin values. Additionally, CPB is a surgery that requires strict control of glucose homeostasis.38 ASP is a hormone that induces glucose release from the liver.39 Circulating glucose levels and reactive oxygen species partially increase due to CPB surgery stress.40 Hence, ASP might protect cardiomyocytes from apoptosis by reducing reactive oxygen species under glucose conditions above the physiological dose. In light of the available data, we suggest that this may be the likely cause of the increase in ASP levels during and after CPB in our study.
In addition, in this study, it was reported that while control blood ALA values were significantly lower than those in CPB patients, there was an increase in blood ALA values taken at T1, T2, and T3 as progression from T1 to T3. On the 1st day (T6) and 3rd day (T7) of CPB surgery, the amount of ALA decreased in the blood samples, but this decrease was not statistically significant compared to the control. Ischemia occurs due to occlusion or narrowing of the coronary vessels feeding the heart because of atherosclerosis and lack of oxygen and nutrients required by the heart. A possible reason for the high T1 (basal) values in CPB patients and the ALA values in blood samples taken at T2 and T3 may be the occlusion of the coronary vessels and the increased amount of ALA in circulation as a compensator for protecting heart tissues from ischemia-reperfusion injury due to CPB surgery. This is because in a study, it has been reported that ALA administration to rats protected the rats from myocardial ischemia-reperfusion injuries by activating C-Jun N-terminal kinase (JNK) and inhibiting nuclear factor-kappa B (NF-κβ).41 In addition, the administration of ALA caused an improvement in HR, MAP, left ventricular end-systolic pressure (LVESP), and left ventricular end-diastolic pressure (LVEDP).42 Possible main function of increased ALA during and after CPB surgery in coronary occlusion is predicted to mediate the physiologically harmonious regulation of hemodynamic events such as HR and MAP.
Although this study is the first to show how SUB, MaR-1, ASP, and ALA change during CPB surgery, it has some limitations. The most important limitation of this study is the small number of participants. The real reason for this limitation is that CPB patients did not participate in the study because of their own stress and surgical concerns. The demographic data of patients vary widely. It is extremely difficult to find participants because these variabilities were eliminated. The last limitation of this study was how the drugs used by patients affected these parameters.
Conclusion
As a result, since the physiopathology of CPB systemic inflammatory response is multifaceted, there is no consensus regarding its true mechanism. However, tissue hormones discovered in recent years are effective in inflammatory processes and surgical stress changes. This study demonstrated an inverse relationship (decreasing SUB and MaR-1, and increasing ASP and ALA) between these four neurohormonal stress factors in an acute systemic stress response scenario. Therefore, these molecules (decreased SUB and MaR-1, increased ASP and ALA), which vary in response to CPB surgery, have the potential to be used in the future in the follow-up of surgical operations for the elimination of damage from CPB, myocardial ischemia-reperfusion, or for the elimination of postoperative systemic complications that adversely affect the perioperative course of the patient after surgical myocardial revascularization.
Data Sharing Statement
Data for this study can be obtained from the corresponding authors upon reasonable request.
Ethics Approval and Informed Consent
This study was reviewed and approved by the Institutional Clinical Research and Ethics Committee of the Firat University. All patients provided written informed consent to participate in the study.
Acknowledgments
We are grateful to Cardiac Surgeon Associate Prof. Dr. Fevzi Sarper TURKER for helping us collect biological samples from his patients during cardiac surgery, Associate Prof. Dr. İbrahim SAHİN for performing statistical analysis, and Biochemist Prof. Dr. Suleyman AYDİN, who read this study with a critical eye, contributed to his constructive feedback, and assisted with the ELISA studies.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
References
1. Levy H, Tanaka KA. Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg. 2003;75(2):S715–S720. doi:10.1016/s0003-475(02)04701-x
2. Aydin S, Aydin S, Nesimi Eren M, et al. The cardiovascular system and the biochemistry of grafts used in heart surgery. Springerplus. 2013;2(1):612. doi:10.1186/2193-1801-2-612
3. Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016;118(9):1392–1408. doi:10.1161/CIRCRESAHA.116.306853
4. Mallat Z, Binder CJ. The why and how of adaptive immune responses in ischemic cardiovascular disease. Nat Cardiovascular Res. 2022;1(5):431–444. doi:10.1038/s44161-022-00049-1
5. Corral-Velez V, Lopez-Delgado JC, Betancur-Zambrano NL, et al. The inflammatory response in cardiac surgery: an overview of the pathophysiology and clinical implications. Inflamm Allergy Drug Targets. 2015;13(6):367–370. doi:10.2174/1871528114666150529120801
6. Ding X, Chang X, Wang J, et al. Serum Metrnl levels are decreased in subjects with overweight or obesity and are independently associated with adverse lipid profile. Front Endocrinol. 2022;13:938341. doi:10.3389/fendo.2022.938341
7. Ushach I, Burkhardt AM, Martinez C, et al. METEORIN-LIKE is a cytokine associated with barrier tissues and alternatively activated macrophages. Clin Immunol. 2015;156(2):119–127. doi:10.1016/j.clim.2014.11.006
8. Huang S, Cao L, Cheng H, et al. The blooming intersection of subfatin and metabolic syndrome. Rev Cardiovasc Med. 2021;22(3):799–805. doi:10.31083/j.rcm2203086
9. Mirzaoglu M, Yavuzkir S, Mirzaoglu C, et al. Use of asprosin and subfatin for differential diagnosis of serous ovarian tumors. Biotech Histochem. 2023;98(2):140–146. doi:10.1080/10520295.2022.2135763
10. Cheng JX, Yu K. New discovered adipokines associated with the pathogenesis of obesity and type 2 diabetes. Diabetes Metab Syndr Obes. 2022;15:2381–2389. doi:10.2147/DMSO.S376163
11. Akbulut T, Cinar V, Ugur K, Yardim M, Karagoz ZK, Aydin S. Effect of regular exercise on the levels of subfatin and asprosin: a trial with different types of exercise. Eur Rev Med Pharmacol Sci. 2022;26(8):2683–2691. doi:10.26355/eurrev_202204_28598
12. Deng B, Wang CW, Arnardottir HH, et al. Maresin biosynthesis and identification of maresin 2, a new anti-inflammatory and pro-resolving mediator from human macrophages. PLoS One. 2014;9(7):e102362. doi:10.1371/journal.pone.0102362
13. Tang S, Wan M, Huang W, Stanton RC, Xu Y. Maresins: specialized proresolving lipid mediators and their potential role in inflammatory-related diseases. Mediators Inflamm. 2018;2018:2380319. doi:10.1155/2018/2380319
14. Wang CW, Yu SH, Fretwurst T, et al. Maresin 1 promotes wound healing and socket bone regeneration for alveolar ridge preservation. J Dent Res. 2020;99(8):930–937. doi:10.1177/0022034520917903
15. Theofilis P, Sagris M, Oikonomou E, et al. Inflammatory mechanisms contributing to endothelial dysfunction. Biomedicines. 2021;9(7):781. doi:10.3390/biomedicines9070781
16. Chatterjee A, Sharma A, Chen M, Toy R, Mottola G, Conte MS. The pro-resolving lipid mediator maresin 1 (MaR1) attenuates inflammatory signaling pathways in vascular smooth muscle and endothelial cells. PLoS One. 2014;9(11):e113480. doi:10.1371/journal.pone.0113480
17. Saito-Sasaki N, Sawada Y, Nakamura M. Maresin-1 and inflammatory disease. Int J Mol Sci. 2022;23(3):1367. doi:10.3390/ijms23031367
18. Adachi Y, Ueda K, Nomura S, et al. Beiging of perivascular adipose tissue regulates its inflammation and vascular remodeling. Nat Commun. 2022;13(1):5117. doi:10.1038/s41467-022-32658-6
19. Romere C, Duerrschmid C, Bournat J, et al. Asprosin, a Fasting-induced glucogenic protein hormone. Cell. 2016;165(3):566–579. doi:10.1016/j.cell.2016.02.063
20. Chen ZX, Jia WN, Jiang YX. Genotype-phenotype correlations of Marfan syndrome and related fibrillinopathies: phenomenon and molecular relevance. Front Genet. 2022;13:943083. doi:10.3389/fgene.2022.943083
21. Duerrschmid C, He Y, Wang C, et al. Asprosin is a centrally acting orexigenic hormone. Nat Med. 2017;23(12):1444–1453. doi:10.1038/nm.4432
22. Yuan M, Li W, Zhu Y, Yu B, Wu J. Asprosin: a novel player in metabolic diseases. Front Endocrinol. 2020;11:64. doi:10.3389/fendo.2020.00064
23. Lee T, Yun S, Jeong JH, Jung TW. Asprosin impairs insulin secretion in response to glucose and viability through TLR4/JNK-mediated inflammation. Mol Cell Endocrinol. 2019;486:96–104. doi:10.1016/j.mce.2019.03.001
24. Wiecek M, Szymura J, Sproull J, Szygula Z. Decreased blood asprosin in hyperglycemic menopausal women as a result of whole-body cryotherapy regardless of metabolic syndrome. J Clin Med. 2019;8(9):1428. doi:10.3390/jcm8091428
25. Almeida-Santos AF, de Melo LA, Gonçalves SCA, et al. Alamandine through MrgD receptor induces antidepressant-like effect in transgenic rats with low brain angiotensinogen. Horm Behav. 2021;127:104880. doi:10.1016/j.yhbeh.2020.104880
26. Hrenak J, Paulis L, Simko F. Angiotensin A/Alamandine/MrgD Axis: another clue to understanding cardiovascular pathophysiology. Int J Mol Sci. 2016;17(7):1098. doi:10.3390/ijms17071098
27. de Carvalho Santuchi M, Dutra MF, Vago JP, et al. Angiotensin-(1-7) and Alamandine promote anti-inflammatory response in macrophages in vitro and in vivo. Mediators Inflamm. 2019;2019:2401081. doi:10.1155/2019/2401081
28. de Souza-Neto FP, Silva MME, Santuchi MC, et al. Alamandine attenuates arterial remodelling induced by transverse aortic constriction in mice. Clin Sci. 2019;133(5):629–643. doi:10.1042/CS20180547
29. Aydin S, Catak Z, Eren MN, Topal AE, Aydin S. Irisin in Coronary Bypass Surgery. Cardiovasc Hematol Disord Drug Targets. 2018;18(3):208–214. doi:10.2174/1871529X18666180511141151
30. Aydin S. A short history, principles, and types of ELISA, and our laboratory experience with peptide/protein analyses using ELISA. Peptides. 2015;72:4–15. doi:10.1016/j.peptides.2015.04.012
31. Li J, Zhang H, Zhang C. Role of inflammation in the regulation of coronary blood flow in ischemia and reperfusion: mechanisms and therapeutic implications. J Mol Cell Cardiol. 2012;52(4):865–872. doi:10.1016/j.yjmcc.2011.08.027
32. Kobiyama K, Ley K. Atherosclerosis. Circ Res. 2018;123(10):1118–1120. doi:10.1161/CIRCRESAHA.118.313816
33. Liu M, He H, Chen L. Protective potential of maresins in cardiovascular diseases. Front Cardiovasc Med. 2022;9:923413. doi:10.3389/fcvm.2022.923413
34. Cezar TLC, Martinez RM, da Rocha C, et al. Treatment with maresin 1, a docosahexaenoic acid-derived pro-resolution lipid, protects skin from inflammation and oxidative stress caused by UVB irradiation. Sci Rep. 2019;9(1):3062. doi:10.1038/s41598-019-39584-6
35. Sánchez-Fernández A, Zandee S, Mastrogiovanni M, et al. Administration of Maresin-1 ameliorates the physiopathology of experimental autoimmune encephalomyelitis. J Neuroinflammation. 2022;19(1):27. doi:10.1186/s12974-022-02386-1
36. Moradi N, Fouani FZ, Vatannejad A, Bakhti Arani A, Shahrzad S, Fadaei R. Serum levels of Asprosin in patients diagnosed with coronary artery disease (CAD): a case-control study. Lipids Health Dis. 2021;20(1):88. doi:10.1186/s12944-021-01514-9
37. Güven C, Kafadar H. Evaluation of plasma asprosin concentration in patients with coronary artery disease. Braz J Cardiovasc Surg. 2022;37(4):493–500. doi:10.21470/1678-9741-2021-0003
38. Fujii T, Hirai T, Tamura T, Suzuki S, Nishiwaki K. Effect of intensive insulin therapy on inflammatory response after cardiac surgery using bedside artificial pancreas: a propensity score-matched analysis. Artif Organs. 2023;47(6):982–989. doi:10.1111/aor.14418
39. Mazur-Bialy AI. Asprosin-a fasting-induced, glucogenic, and orexigenic adipokine as a new promising player. will it be a new factor in the treatment of obesity, diabetes, or infertility? A review of the literature. Nutrients. 2021;13(2):620. doi:10.3390/nu13020620
40. Reyes-Umpierrez D, Davis G, Cardona S, et al. Inflammation and oxidative stress in cardiac surgery patients treated to intensive versus conservative glucose targets. J Clin Endocrinol Meta. 2017;102(1):309–315. doi:10.1210/jc.2016-3197
41. Song XD, Feng JP, Yang RX. Alamandine protects rat from myocardial ischemia-reperfusion injury by activating JNK and inhibiting NF-κB. Eur Rev Med Pharmacol Sci. 2019;23(15):6718–6726. doi:10.26355/eurrev_201908_18563
42. Silva MM, de Souza-Neto FP, de Jesus ICG, et al. Alamandine improves cardiac remodeling induced by transverse aortic constriction in mice. Am J Physiol Heart Circ Physiol. 2021;320(1):H352–H363. doi:10.1152/ajpheart.00328.2020
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.