Back to Journals » Infection and Drug Resistance » Volume 16
Study on Respiratory Function and Hemodynamics of AIDS Patients with Respiratory Failure
Authors Qiu K, Lu J , Guo H, Du C, Liu J, Li A
Received 6 May 2023
Accepted for publication 27 September 2023
Published 30 October 2023 Volume 2023:16 Pages 6941—6950
DOI https://doi.org/10.2147/IDR.S376752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Kai Qiu,1,2 Jiaqi Lu,1 Hebing Guo,1 Chunjing Du,1 Jingyuan Liu,1 Ang Li3
1Department of Critical Care Medicine, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Intensive Care Medicine, Liangxiang Hospital of Beijing Fangshan District, Beijing, People’s Republic of China; 3Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Jingyuan Liu; Ang Li, Beijing Ditan Hospital, Capital Medical University, #8 Jing Shun East St Chaoyang, Beijing, 100015, People’s Republic of China, Email [email protected]; [email protected]
Objective: We performed a comparative analysis of respiratory function and hemodynamics among patients with Acquired Immunodeficiency Syndrome (AIDS)-associated respiratory failure and those with non-AIDS-associated respiratory failure.
Methods: Data were collected from critically ill patients diagnosed with Acquired Immunodeficiency Syndrome who were admitted to the Intensive Care Unit (ICU) of Beijing Ditan Hospital, affiliated with Capital Medical University, between January 1, 2019, and December 31, 2019. We simultaneously gathered data from non-AIDS patients admitted to the ICU of Beijing Liangxiang Hospital within the same timeframe. A comparative study was performed to analyze clinical data from these two patient groups, encompassing parameters related to respiratory mechanics and hemodynamic indicators.
Results: A total of 12 patients diagnosed with Acquired Immunodeficiency Syndrome (AIDS) and experiencing respiratory failure, along with 23 patients with respiratory failure independent of AIDS, were included in our study. Subsequently, a comparative analysis of clinical information was conducted between the two patient cohorts. Our findings demonstrate non-statistically significant differences between the two patient groups when assessing various indicators, encompassing peak airway pressure, plateau pressure, mean pressure, compliance, oxygenation index, and arterial partial pressure of carbon dioxide (P> 0.05). Additionally, the comparison of multiple indicators encompassing mean arterial pressure, central venous pressure, cardiac output index, intrathoracic blood volume index, global end-diastolic volume index, extravascular lung water content, and pulmonary vascular permeability index revealed no statistically significant differences between the two patient groups (P> 0.05). Ultimately, the Galileo respiratory system was utilized to assess the pressure-volume (P-V) curve of the experimental cohort, revealing a consistent and seamless trajectory devoid of noticeable points of inflection.
Conclusion: No statistically significant differences were found in the respiratory function and hemodynamic profiles between patients diagnosed with AIDS presenting respiratory failure and those experiencing respiratory failure unrelated to AIDS. Additionally, the pressure-volume curve of individuals diagnosed with AIDS presenting respiratory failure displayed a seamless and uninterrupted trajectory devoid of discernible points of inflection. Hence, there might be constraints when utilizing P-V curve-based adjustments for positive end-expiratory pressure (PEEP) during mechanical ventilation in individuals diagnosed with AIDS presenting respiratory failure.
Keywords: acquired immunodeficiency syndrome, acute respiratory failure, respiratory function, hemodynamics, pressure-volume curve
Introduction
Acquired Immunodeficiency Syndrome, commonly known as human immunodeficiency virus (HIV) infection, is caused by the presence of the HIV, which is often referred to as the AIDS virus.1 Individuals diagnosed with AIDS commonly require admission to the intensive care unit due to hypoxemic respiratory failure.2–4 Furthermore, individuals in question commonly require specific therapeutic interventions as well as supportive measures such as mechanical ventilation and oxygen therapy.5 Prior to the extensive implementation of Highly Active Antiretroviral Therapy (HAART), respiratory failure resulting from Pneumocystis Jirovecii Pneumonia (PJP) stood as the leading reason for admitting HIV-infected individuals to the Intensive Care Unit.6,7 The widespread implementation of Highly Active Antiretroviral Therapy (HAART) has resulted in a significant decrease in the prevalence of opportunistic infections linked to HIV/AIDS, consequently altering the primary causes of HIV-related mortality from opportunistic infections to non-opportunistic infections, including chronic diseases.3,8,9 Nevertheless, acute respiratory failure continues to prevail as the primary diagnosis upon admission to the ICU, especially in countries with lower and middle incomes.3,10,11 Between October 2008 and October 2013, at Beijing Ditan Hospital, pulmonary infections constituted the prevailing etiology of concurrent respiratory failure among individuals with HIV/AIDS, representing 89% of cases. Notably, Pneumocystis pneumonia accounted for 84.5% of these cases, likely associated with compromised immune function due to HIV infection and heightened vulnerability to opportunistic pathogens.2 Out of the patients who survived hospitalization, 38.9% necessitated invasive mechanical ventilation, signifying the significant impact of respiratory failure on individuals with HIV/AIDS and accompanying pulmonary infections, while underscoring the criticality of prompt intervention and treatment.2 Owing to the complex profile of individuals diagnosed with HIV/AIDS and concurrent respiratory failure, characterized by frequent immunosuppression and increased vulnerability to infections, providing respiratory support has persistently presented a formidable obstacle within the realm of clinical care. Within the domain of therapy involving invasive mechanical ventilation, attending to the concerns surrounding the reduction of pulmonary injury and the prevention of complications, such as secondary infections, assumes paramount significance, demanding meticulous focus and effective resolution. Concurrently, effectively managing respiratory failure across various stages and classifications mandates the utilization of multifaceted therapeutic strategies and approaches. For example, implementing timely interventions, tailored modifications, and periodic evaluations becomes imperative in optimizing treatment effectiveness and mitigating mortality risks.7
The pathophysiological mechanisms and distinguishing features of respiratory failure resulting from pulmonary infections in individuals diagnosed with HIV/AIDS exhibit substantial disparities compared to those induced by infectious agents in non-HIV/AIDS patients. Consequently, our research endeavors are directed towards discerning the distinct variations in respiratory failure stemming from pulmonary infections among individuals diagnosed with HIV/AIDS compared to those unaffected by the condition. Presently, there exists a dearth of research pertaining to the respiratory function and hemodynamic profiles in individuals diagnosed with HIV/AIDS who experience respiratory failure and undergo therapeutic interventions involving invasive mechanical ventilation. Hence, the primary objective of this study is to examine individuals diagnosed with AIDS who receive invasive mechanical ventilation therapy to address respiratory failure. The study aims to conduct a comprehensive investigation into the respiratory function and hemodynamic features exhibited by these patients, ultimately aiming to provide enhanced guidance for the formulation of clinical strategies pertaining to both respiratory and circulatory support.
Materials and Methods
Study Design
The primary focus of this study centers around critically ill patients receiving treatment in the Intensive Care Units (ICUs) at Beijing Ditan Hospital and Liangxiang Hospital located within the Fangshan District of Beijing. The study was conducted during the time frame spanning from January 1st, 2019, to December 31st, 2019. This study was conducted in accordance with the Declaration of Helsinki. Moreover, this study has received approval from the Ethics Committee. This study has been granted ethical approval with the reference number Department of ethics, Beijing Ditan Hospital (2018) No. (005) - 01. Due to the absence of any identifiable information within the collected clinical and laboratory data, all patient records remain anonymous, effectively eliminating the requirement for informed consent from both patients and their families.
Study Population
Sequential enrollment was conducted for all individuals aged 18 and above who were admitted to the intensive care unit with respiratory failure, irrespective of their origination from the emergency department or transfer from general wards. A positive outcome in HIV antibody testing (screening + confirmatory test) serves as the diagnostic criterion for HIV infection. HIV infections are categorized as either previously diagnosed or newly diagnosed, depending on the time of diagnosis and the receipt of antiviral treatment. Newly diagnosed HIV infection refers to cases where diagnosis occurs within 2 months prior to admission without any prior antiviral treatment. Patients diagnosed with AIDS are individuals who have advanced to the AIDS stage following HIV infection. This condition is defined by a CD4+ T lymphocyte count lower than 200 cells/µL or the manifestation of diverse opportunistic infections and tumors linked to AIDS. Respiratory failure is clinically defined by an arterial partial pressure of oxygen (PaO2) ≤ 60mmHg in the absence of supplemental oxygen, along with a PaO2/FiO2 ratio (ratio of PaO2 to inspired oxygen fraction, FiO2) ≤ 300mmHg under conditions of supplemental oxygen administration. Furthermore, respiratory failure is marked by an arterial partial pressure of carbon dioxide (PaCO2) ≤ 50mmHg. Exclude patients who do not exhibit signs of pulmonary infection, individuals who have not undergone invasive mechanical ventilation, and those with ICU stays shorter than 24 hours. Our study exclusively enrolls patients who are facing respiratory failure resulting from pulmonary infection. Diagnostic criteria for pulmonary infection include the following: (1) Presence of corresponding clinical manifestations, such as cough, sputum production, fever, dyspnea, and shortness of breath. (2) Observation of abnormal lung imaging findings, including ground-glass opacities, consolidation, patchy shadows, reticular opacities, and bronchial inflation, in computed tomography scans. (3) Collection of airway secretion specimens, such as induced sputum, lower respiratory tract aspirate, or bronchoalveolar lavage fluid, to identify pathogenic microorganisms. Bacterial and fungal cultures are performed on these collected airway secretion specimens. The specimens undergo Giemsa staining or Gomori-Grocott staining, or the application of immunofluorescence assay to ascertain the presence of Pneumocystis jirovecii. Cytomegalovirus DNA is detected through the utilization of real-time quantitative polymerase chain reaction (PCR) assay. Furthermore, our laboratory testing for atypical bacterial pathogens, including Chlamydia and Legionella, has been significantly enhanced. Data pertaining to the patients’ initial admission period in the ICU are gathered for those with recurrent ICU admissions.
Data Collection
Patients receive mechanical ventilation through the utilization of the Galileo ventilator, while continuous hemodynamic monitoring is implemented using the Pulse Index Contour Continuous Cardiac Output (PICCO) system. Neuromuscular relaxation therapy is administered to patients under the condition of stable circulatory status to induce a sedated and relaxed state without any spontaneous respiration. Expanding upon this groundwork, we obtain respiratory mechanical parameters of patients, analyze respiratory mechanics by utilizing pressure-volume curves derived from the ventilator, and concurrently carry out hemodynamic measurements.
Baseline information of patients has been gathered at the time of ICU admission, encompassing age, gender, weight, height, and pertinent indicators associated with HIV infection, such as the date of HIV diagnosis, utilization of antiviral treatment, the most recent recorded CD4+ T lymphocyte count within three months preceding ICU admission, and the HIV viral load. Disease severity upon admission to the ICU is evaluated by employing the Acute Physiology and Chronic Health Evaluation (APACHE) II score12 and the Sequential Organ Failure Assessment (SOFA) score. These scoring systems measure acute physiological and chronic health conditions, along with the progression of organ dysfunction.13
Collected respiratory mechanical parameters from patients encompass peak inspiratory pressure (Ppeak), plateau pressure (Pplat), mean airway pressure (Pmean), compliance of respiratory system (Crs), oxygenation index (PaO2/FiO2), carbon dioxide partial pressure (PaCO2) levels, and quasi-static observation of pressure-volume (P-V) curves. Collected hemodynamic parameters from patients encompass heart rate (HR), central venous pressure (CVP), mean arterial pressure (MAP), cardiac output index (CI), intrathoracic blood volume index (ITBVI), global end-diastolic volume index (GEDVI), extravascular lung water index (EVLWI), and pulmonary vascular permeability index (PVPI).
Statistical Analysis
Patients were categorized into two groups based on the presence or absence of HIV infection: the HIV-positive group and the HIV-negative group. Subsequently, clinical data and laboratory information were compared between the two groups. Metric data from the subjects with a normal distribution were presented as mean ± standard deviation. Independent sample t-tests were utilized to compare non-paired data, whereas paired sample t-tests were applied for paired data comparisons. Non-normally distributed data were represented using the median and interquartile range (IQR). For non-paired data, Mann–Whitney U-tests were conducted, and for paired data, Wilcoxon signed-rank tests were employed. Differences in all test data were deemed statistically significant when the significance level (P-value) was below 0.05. Statistical analyses were performed utilizing IBM SPSS Statistics 24.0.
Results
Patient Characteristics
Throughout a one-year duration, our study involved a cohort of 20 adult patients who suffered from respiratory failure related to HIV and were admitted to two separate hospitals. Out of the total, 8 patients (40.0%) were excluded from the study due to meeting the exclusion criteria: 1 patient (12.5%) had respiratory failure unrelated to pulmonary infection, 5 patients (62.5%) did not undergo invasive mechanical ventilation treatment, and 2 patients (25.0%) had an ICU treatment duration of less than 24 hours. Ultimately, 12 patients (60.0%) were included in the final analysis. Moreover, throughout the study period, a total of 41 adult patients without HIV infection who suffered from respiratory failure were admitted. Out of the total participants, 18 patients (43.9%) met the exclusion criteria and were subsequently excluded from the study: 5 patients (27.8%) experienced respiratory failure not associated with pulmonary infection, 10 patients (55.5%) did not receive invasive mechanical ventilation therapy, and 3 patients (16.7%) had an ICU treatment duration of less than 24 hours. Ultimately, a total of 23 patients (56.1%) were successfully included in the study. All enrolled participants shared the same ethnic background.
The clinical characteristics of patients in both the HIV-positive and non-HIV groups are presented in Table 1. The mean age of patients in the HIV-positive group was 37.50±8.45 years, primarily comprising males who constituted 91.7% of the cohort. The average age of non-HIV patients was 61.48±13.93 years, significantly higher than that of HIV-positive patients, and the difference between the two groups was statistically significant (p<0.001). No statistically significant differences were observed between the HIV-positive and non-HIV groups regarding patients’ weight, height, and BMI (p>0.05). These findings suggest a lack of substantial variation. Subsequently, we conducted an analysis of the essential clinical characteristics of the patient cohort. The findings revealed that individuals in the HIV-positive group demonstrated notably reduced APACHE II scores, SOFA scores, and CD4+ cell counts when compared to their counterparts in the non-HIV group (P<0.01).
 |
Table 1 Comparison of the Basic Characteristics of the Two Patient Groups |
Comparison of Respiratory Function Between the Two Patient Groups
The comparative analysis of respiratory function indicators between the two patient groups during mechanical ventilation can be found in Table 2. The set of parameters includes Ppeak, Pplat, Pmean, Crs, PaO2/FiO2, and PaCO2, among other relevant indicators. Regarding the airway pressure observed during mechanical ventilation, the Ppeak values were (25.34±6.71) cmH2O for patients in the HIV-positive group and (26.15±6.48) cmH2O for non-HIV patients. Although the Ppeak of non-HIV patients exceeded that of HIV-positive patients slightly, the observed disparity between the two groups did not attain statistical significance (p>0.05). In a similar vein, the Pplat values were notably greater in the non-HIV group as compared to the HIV group, with measurements of 23.36±5.62 cmH2O and 22.69±6.03 cmH2O, respectively. However, the observed disparity between the two groups did not reach statistical significance according to the determined p-value (p>0.05). Likewise, the research outcomes pertaining to Pmean exhibited comparability across both patient groups. Subsequent to the examination of pulmonary compliance among the two patient cohorts, it was found that the pulmonary resistance was higher in the non-HIV group compared to the HIV group, with measurements of 28.53±6.86 mL/cmH2O and 25.57±9.25 mL/cmH2O respectively. Nevertheless, the observed difference between the two groups did not reach statistical significance (p>0.05). The research findings regarding PaO2/FiO2 and PaCO2 in both patient groups exhibit resemblance to the previous indices, as there were no statistically significant differences observed (P>0.05).
 |
Table 2 Comparison of the Respiratory Function Indicators Between the Two Groups |
Comparison of Hemodynamic Characteristics Between the Two Groups of Patients
Table 3 displays the comparative analysis of hemodynamic indicators across the two patient groups. Among others, these parameters include HR, MAP, CVP, CI, ITBVI, GEDVI, EVLWI, and PVPI. Regarding heart rate, the HIV group demonstrated an HR of (93.52±13.06) cpm, whereas the non-HIV group exhibited an HR of (104.36±15.95) cpm. The heart rate of the non-HIV group surpassed that of the HIV group significantly with statistical significance (p=0.05). Furthermore, the non-HIV group demonstrated a greater mean arterial pressure (MAP) in comparison to the HIV group (92.53±7.75 vs 88.62±8.71 mmHg); however, this disparity did not reach statistical significance (p>0.05). Afterwards, the research findings pertaining to CVP exhibited similarity between the two patient cohorts. Subsequently, we employed PICCO to assess the variables CI, ITBVI, GEDVI, EVLWI, and PVPI in both patient groups. Furthermore, the comparative analysis of data obtained from both patient cohorts revealed that the HIV group demonstrated elevated levels of CI, ITBVI, GEDVI, EVLWI, and PVPI in comparison to the non-HIV group. Nevertheless, these observed disparities did not achieve statistical significance (p>0.05).
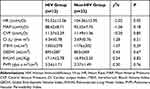 |
Table 3 Comparison of the Hemodynamic Parameters Between the Two Groups |
The P-V Curve of the HIV Group Patients Does Not Exhibit a Distinct Inflection Point
In this study, Galilean ventilators were utilized for measuring the patients’ P-V curves. The obtained P-V curves were subsequently employed to evaluate the pulmonary function and mechanical ventilation efficacy of the subjects. The P-V curve pertains to the quantification of the pressure-volume relationship within a defined temporal window, wherein the respiratory system reaches a state of relative stability characterized by negligible airflow. This graphical representation serves as an indicator of the pulmonary compliance exhibited by the patient’s alveoli alongside the resistance encountered within the respiratory system. Through the analysis of the morphology and slope of the P-V curve, one can discern the presence of restrictive or obstructive pulmonary diseases. This examination allows for the establishment of pertinent mechanical ventilation parameters aimed at optimizing the patient’s ventilatory support. The current study reveals that the P-V curve of individuals afflicted with HIV did not manifest a discernible inflection point, as indicated in Figure 1.
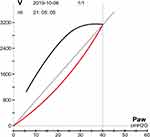 |
Figure 1 The quasi-static P-V curve. |
Discussion
This article primarily examines the clinical characteristics of individuals with HIV-associated respiratory failure in comparison to those without HIV who similarly present with respiratory failure. This study offers crucial clinical insights into the management of critically ill patients with HIV-associated respiratory failure through the identification of respiratory function and hemodynamic characteristics within the two distinct patient groups. This study represents our initial analysis, juxtaposing the clinical characteristics of patients experiencing HIV-associated respiratory failure who were admitted to the intensive care unit with those encountering respiratory failure in the absence of HIV infection.
Despite the introduction of highly active antiretroviral therapy, patients suffering from HIV-associated respiratory failure continue to face a myriad of challenges regarding their treatment and management.1 According to the study conducted by Sarkar et al, it is currently evident that 25–50% of individuals infected with the HIV are necessitated to be admitted to the ICU as a consequence of acute respiratory failure (ARF). These patients commonly necessitate intensive interventions, including mechanical ventilation, with a mortality rate soaring to 50%-68%.5 Furthermore, numerous studies have indicated that in middle- and low-income countries, there is a tendency for the diagnosis and treatment of individuals with HIV/AIDS to be delayed.14–17 Investigation findings indicate that around 80% of HIV-infected patients who were admitted to the ICU in our nation had not received a prior diagnosis of HIV infection.18–21 Mechanical ventilation is considered a crucial intervention in the comprehensive care of patients experiencing respiratory failure. Its primary goals include minimizing the occurrence of ventilator-induced lung injury (VILI) while significantly improving oxygenation.22 The mechanical ventilation strategy should be customized based on the specific condition of each patient, encompassing the selection of suitable ventilation modes and parameters to effectively mitigate additional harm to the pulmonary tissue. Moreover, the implementation of a lung-protective ventilation strategy plays a vital role in both preventing and treating VILI. This comprehensive approach encompasses strategies such as utilizing low tidal volumes, restricting plateau pressures, and ensuring sufficient positive end-expiratory pressure (PEEP) levels, alongside other relevant measures. Therefore, gaining a profound understanding of patients’ respiratory mechanics characteristics and appropriately guiding the mechanical ventilation strategy are of utmost importance.23 Throughout the course of mechanical ventilation, crucial parameters including Ppeak, Pplat, Pmean, Crs, PaO2/FiO2 ratio, and PaCO2 serve as indispensable markers to assess patients’ pulmonary function and the effectiveness of mechanical ventilation therapy. Among these parameters, Ppeak signifies the highest pressure exerted by the ventilator throughout the course of mechanical ventilation and is frequently utilized for evaluating the potential threat of ventilator-associated lung injury. Pplat denotes the airway pressure that remains constant at the conclusion of expiration and plays a crucial role in assessing alveolar pressure. Pmean signifies the average airway pressure observed during a specific time interval and embodies the mean pressure imposed on the pulmonary tissue through mechanical ventilation. Crs, a critical indicator, reflects the elasticity of the pulmonary tissue and its capacity to accommodate lung expansion. It encapsulates various elements including alveolar compliance, chest wall compliance, and respiratory muscle compliance. The PaO2/FiO2 ratio, an indicator employed to evaluate oxygenation capacity, encompasses both pulmonary function and oxygen delivery. PaCO2 functions as an essential indicator to evaluate the elimination of carbon dioxide and indicates the presence of respiratory acidosis or alkalosis. These indicators hold significant importance in the realm of mechanical ventilation therapy and pulmonary function assessment. Through diligent monitoring and analysis of these indicators, we can acquire a more profound comprehension of the influence exerted by mechanical ventilation on the pulmonary system, thus enabling the formulation of pertinent clinical treatment strategies. Concurrently, these indicators serve as pivotal benchmarks for evaluating the efficacy and safety of mechanical ventilation therapy, thereby playing a critical role in augmenting treatment success rates and mitigating the occurrence of adverse reactions. The present study involved a comparative analysis of several indicators, encompassing Ppeak, Pplat, Pmean, Crs, PaO2/FiO2, and PaCO2, between the experimental group and the control group. The findings suggest that there were no statistically significant differences (P>0.05) observed in the comparison of these indicators between the two groups. Specifically, it can be concluded that no substantial enhancement in lung compliance occurred when contrasting the AIDS group with the non-AIDS group.
Hemodynamic parameters serve as essential metrics utilized for assessing cardiovascular function and volumetric status, playing a crucial role in the monitoring and treatment of critically ill patients in clinical practice. Among these indicators, HR, MAP, CVP, CI, ITBVI, GEDVI, EVLWI, and PVPI bear substantial clinical significance. Heart rate (HR) signifies the frequency of cardiac contractions within a specified duration, conventionally quantified in beats per minute (BPM). Mean arterial pressure (MAP) denotes the average pressure encountered by arteries throughout a cardiac cycle, encompassing both systole and diastole. It serves as a crucial gauge for assessing cardiac ejection capacity and reflecting the condition of peripheral vascular resistance. Central venous pressure (CVP) pertains to the assessment of venous blood pressure within the right atrium or proximal major veins, offering valuable insights into the correlation between blood volume and cardiac preload. The cardiac index (CI) represents the cardiac output adjusted for body surface area, facilitating a more accurate assessment of a patient’s cardiac function. Indexed total blood volume (ITBVI) represents the indexed coronary artery blood flow during each cardiac cycle, indicative of the volume of blood ejected with every heartbeat. The global end-diastolic volume index (GEDVI) represents the indexed effective circulating blood volume, providing insights into the distribution state of blood volume and tissue perfusion. The extravascular lung water index (EVLWI) represents the water content within the pulmonary interstitium, facilitating the evaluation of pulmonary edema severity. The pulmonary vascular permeability index (PVPI) represents an index that characterizes the distribution of intravascular blood volume, thereby assisting in assessing a patient’s circulatory status and volume load conditions. These indicators are commonly utilized in clinical practice for monitoring and evaluating the cardiovascular function and volume status of critically ill patients. Through continuous monitoring and analysis of these indicators, a more comprehensive comprehension of the patient’s condition and treatment effectiveness can be obtained, facilitating prompt adjustments in therapeutic approaches to enhance patient survival rates. In this experiment, we utilized the PICCO technique to quantitatively assess diverse parameters including HR, MAP, CVP, CI, ITBVI, GEDVI, EVLWI, PVPI, among others. Additionally, we performed a comparative analysis between the two groups. The results indicated a lack of statistically significant differences (P>0.05) when comparing these indicators between the two groups.
Our study did not yield any statistically significant differences. This observation could potentially be ascribed to the constraints imposed by the limited sample size at our disposal. Furthermore, despite variations in the underlying primary diseases among patients, all the individuals from whom we collected data presented a shared condition of respiratory failure. Additionally, given the uniform diagnostic criteria for respiratory failure, it is plausible that there are no discernible disparities in both respiratory mechanics and hemodynamic indicators across the two patient cohorts.
The pressure-volume (P-V) curves acquired from patients with HIV/AIDS complicated by respiratory failure, who received treatment with the Galileo ventilator, underwent thorough examination, revealing the absence of any noticeable inflection point within them. This outcome is consistent with the research findings by D’Angelo et al24 D’Angelo et al utilized the constant flow inflation rapid airway occlusion technique to evaluate the comprehensive respiratory system mechanics in 12 mechanically ventilated AIDS patients with PJP. Moreover, they employed the esophageal balloon technique to partition the data into separate lung and chest wall components. The study findings indicated the absence of any inflection point on the static pressure-volume (P-V) curves within this patient population.24 This observation implies that alveolar recruitment is minimal throughout the lung inflation process. This outcome can be attributed to the distinct pathological and respiratory mechanical characteristics linked to HIV/AIDS complicated by acute respiratory failure. For example, patients with Pneumocystis pneumonia mainly exhibit interstitial changes as the predominant pulmonary lesions, featuring fibrosis within lung tissue and minimal or no edema. These pathological changes diverge from the usual manifestations observed in Acute Respiratory Distress Syndrome (ARDS).25 This finding suggests that relying solely on the P-V curve as a guide for PEEP setting in patients with AIDS and concurrent pulmonary infections has its limitations. Hence, it is imperative for clinicians to develop individualized treatment strategies tailored to the unique circumstances of each patient while considering additional influential factors. Moreover, reinforcing research efforts in the pathophysiology of this illness is crucial for enhancing clinical guidance.
In interpreting the findings, it is vital to consider the inherent limitations associated with this study. Firstly, it is important to acknowledge that this study is based on a relatively limited sample size, potentially leading to inherent biases within the collected observational data. Additionally, this suggests that our research findings may not correspond with the data derived from other research centers. Moreover, it is noteworthy that this study was conducted across two healthcare facilities, potentially leading to variations in data quality control between the two patient cohorts. As a result, there is a possibility of inherent biases in the determination criteria employed for the pertinent data. Finally, the diagnosis of bacterial pneumonia hinges solely on bacterial culture identification for confirmation, with no inclusion of blood cultures or urine antigen tests. Consequently, there exists a possibility that we have underestimated both the incidence of bacterial pneumonia and its influence on mortality rates.
Conclusions
In conclusion, there were no notable discrepancies noted in terms of respiratory function and hemodynamic characteristics between patients with HIV-related respiratory failure and those without. Furthermore, individuals experiencing respiratory failure associated with HIV infection demonstrated an absence of notable deflection points on the quasi-static P-V curve, implying limited or negligible alveolar recruitment throughout lung inflation. Consequently, sole reliance on P-V curve guidance for the establishment of PEEP settings is constrained by substantial limitations.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Declarations
The study was approved by the ethics review board of the National Center for Health Statistics; Department of ethics, Beijing Ditan Hospital (2018) No. (005) - 01.
Informed Consent Statement
The study received the consent of all patients.
Acknowledgments
We would like to thank the researchers and study participants for their contributions.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Capital Medical Development Scientific Research Fund---Optimization of respiratory support of AIDS patients complicated with acute respiratory failure (2018-1-2171).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Barbier F, Mer M, Szychowiak P, et al. Management of HIV-infected patients in the intensive care unit. Intensive Care Med. 2020;46(2):329–342. doi:10.1007/s00134-020-05945-3
2. Xiao J, Zhang W, Huang Y, et al. Etiology and outcomes for patients infected with HIV in intensive care units in a tertiary care hospital in China. J Med Virol. 2015;87(3):366–374. doi:10.1002/jmv.24063
3. Chiang HH, Hung CC, Lee CM, et al. Admissions to intensive care unit of HIV-infected patients in the era of highly active antiretroviral therapy: etiology and prognostic factors. Crit Care. 2011;15(4):R202. doi:10.1186/cc10419
4. Benito N, Moreno A, Miro JM, Torres A. Pulmonary infections in HIV-infected patients: an update in the 21st century. Eur Respir J. 2012;39(3):730–745. doi:10.1183/09031936.00200210
5. Sarkar P, Rasheed HF. Clinical review: respiratory failure in HIV-infected patients--A changing picture. Crit Care. 2013;17(3):228. doi:10.1186/cc12552
6. Nickas G, Wachter RM. Outcomes of intensive care for patients with human immunodeficiency virus infection. Arch Intern Med. 2000;160(4):541–547. doi:10.1001/archinte.160.4.541
7. Barbier F, Roux A, Canet E, et al. Temporal trends in critical events complicating HIV infection: 1999–2010 multicentre cohort study in France. Intensive Care Med. 2014;40(12):1906–1915. doi:10.1007/s00134-014-3481-7
8. Barbier F, Coquet I, Legriel S, et al. Etiologies and outcome of acute respiratory failure in HIV-infected patients. Intensive Care Med. 2009;35(10):1678–1686. doi:10.1007/s00134-009-1559-4
9. Orsini J, Ahmad N, Butala A, et al. Etiology and outcome of patients with HIV infection and respiratory failure admitted to the intensive care unit. Interdiscip Perspect Infect Dis. 2013;2013:732421. doi:10.1155/2013/732421
10. Powell K, Davis JL, Morris AM, Chi A, Bensley MR, Huang L. Survival for patients With HIV admitted to the ICU continues to improve in the current era of combination antiretroviral therapy. Chest. 2009;135(1):11–17. doi:10.1378/chest.08-0980
11. Adlakha A, Pavlou M, Walker DA, et al. Survival of HIV-infected patients admitted to the intensive care unit in the era of highly active antiretroviral therapy. Int J STD AIDS. 2011;22(9):498–504. doi:10.1258/ijsa.2011.010496
12. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
13. Dickson SJ, Batson S, Copas AJ, Edwards SG, Singer M, Miller RF. Survival of HIV-infected patients in the intensive care unit in the era of highly active antiretroviral therapy. Thorax. 2007;62(11):964–968. doi:10.1136/thx.2006.072256
14. Belay GM, Endalamaw A, Ayele AD. Late presentation of HIV positive adults and its predictors to HIV/AIDS care in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):534. doi:10.1186/s12879-019-4156-3
15. Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS One. 2017;12(3):e0173928. doi:10.1371/journal.pone.0173928
16. Ruiz GO, Herrera C, Bohórquez J, Betancur JE. Mortality in patients with acquired human immunodeficiency virus infection hospitalized in an intensive care unit during the period 2017–2019. Sci Rep. 2022;12(1):15644. doi:10.1038/s41598-022-19904-z
17. Sharafi M, Mirahmadizadeh A, Hassanzadeh J, Seif M. Prevalence of late presenters and advanced HIV disease in HIV patients and their related factors in Iran: results from 19 years of national surveillance HIV data. AIDS Res Hum Retroviruses. 2022;38(12):890–897. doi:10.1089/AID.2022.0046
18. Sun C, Li J, Liu X, et al. HIV/AIDS late presentation and its associated factors in China from 2010 to 2020: a systematic review and meta-analysis. AIDS Res Ther. 2021;18(1):96. doi:10.1186/s12981-021-00415-2
19. Jiang H, Liu J, Tan Z, et al. Prevalence of and factors associated with advanced HIV disease among newly diagnosed people living with HIV in Guangdong Province, China. J Int AIDS Soc. 2020;23(11):e25642. doi:10.1002/jia2.25642
20. Shi L, Tang W, Liu X, et al. Trends of late HIV presentation and advance HIV disease among newly diagnosed HIV cases in Jiangsu, China: a serial cross-sectional study from 2008 to 2020. Front Public Health. 2022;10:1054765. doi:10.3389/fpubh.2022.1054765
21. Tang H, Mao Y, Tang W, Han J, Xu J, Li J. “Late for testing, early for antiretroviral therapy, less likely to die”: results from a large HIV cohort study in China, 2006–2014. BMC Infect Dis. 2018;18(1):272. doi:10.1186/s12879-018-3158-x
22. Celesia BM, Marino A, Borracino S, et al. Successful extracorporeal membrane oxygenation treatment in an acquired immune deficiency syndrome (AIDS) patient with acute respiratory distress syndrome (ARDS) complicating pneumocystis jirovecii pneumonia: a challenging case. Am J Case Rep. 2020;21:e919570. doi:10.12659/AJCR.919570
23. Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319(7):698–710. doi:10.1001/jama.2017.21907
24. D’Angelo E, Calderini E, Robatto FM, Puccio P, Milic-Emili J. Lung and chest wall mechanics in patients with acquired immunodeficiency syndrome and severe Pneumocystis carinii pneumonia. Eur Respir J. 1997;10(10):2343–2350. doi:10.1183/09031936.97.10102343
25. Gwag HB, Joh HS, Kim JS, Park KM, On YK, Park SJ. Safety of mechanical lung vibrator and high-frequency chest wall oscillation in patients with cardiac implantable electronic device. Clin Cardiol. 2021;44(4):531–536. doi:10.1002/clc.23571
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
