Back to Journals » Journal of Asthma and Allergy » Volume 16
Study on Intestinal Flora and Asthma: Knowledge Graph Analysis Based on CiteSpace (2001–2021)
Authors Zheng H, Dai H, Yan X, Xiang Q
Received 29 December 2022
Accepted for publication 12 March 2023
Published 5 April 2023 Volume 2023:16 Pages 355—364
DOI https://doi.org/10.2147/JAA.S402883
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amrita Dosanjh
Hang Zheng, Huan Dai, Xiumei Yan, Qiangwei Xiang
Department of Pediatric Allergy and Immunology, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China
Correspondence: Qiangwei Xiang, Department of Pediatric Allergy and Immunology, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China, Email [email protected]
Abstract: Asthma is a common chronic inflammatory disease of the airway. Intestinal flora, a significant risk factor for asthma, has become a widespread concern in the pathogenesis of asthma. To review the literature related to intestinal flora in asthma, summarize research direction, and report trends, this study used CiteSpace to perform bibliometric statistics and analysis on the research papers of intestinal flora and asthma collected in the Web of science core collection from 2001 to 2021. Eventually, a total of 613 articles were included. The results demonstrated that research on gut flora and asthma continued to heat up, with article numbers increasing, especially in the last decade. Moreover, analysis of the keywords showed that the research topics of intestinal flora and asthma range from confirming the link between intestinal flora and asthma to investigating mechanisms and then to asthma treatment. According to the summary of research hotspots, we expand on three emerging issues that require attention in the intestinal flora and asthma research, including (regulatory T)Treg cells, probiotics, and chain fatty acid. Evidence illustrated that Treg cells play a crucial role in the pathogenesis of asthma caused by dysbiosis of the gut flora. Furthermore, in contrast to probiotic supplements, which do not reduce the risk of developing asthma, short-chain fatty acids supplements do. Overall, the research direction in the field of intestinal flora and asthma has recently evolved from macro to micro with depth broadened. As a robust scientific evaluation, our study provided a comprehensive overview of the area, particularly for research focus, which could more precisely direct scholars on future research and clinical diagnosis, therapy, and individualized prevention.
Keywords: microbiota, allergy, Treg cells, probiotics, chain fatty acid
Introduction
Asthma is a common chronic inflammatory disease of the airway induced by immune dysregulation, which affected an estimated 358 million individuals worldwide in 2015, with a significant incidence of morbidity and mortality.1 Risk factors for asthma have also gotten much attention in recent years. Noticeably, intestinal flora has so far been linked to asthma in increasing amounts of research,2,3 and it has become one of the risk factors for asthma,4,5 with the appearance of the concept of hygiene hypothesis and gut–lung axis.6 Moreover, the essential immunological role performed by intestinal flora, including regulating the proper development of the immune system and supporting immune tolerance, became a hotspot in prior years.7–9 Thus, a literature study is necessary to better understand the trajectory of research on gut flora and asthma and to direct specific studies.
Scholars can realize the visualization of discipline knowledge by drawing a scientific knowledge map based on literature data information to research the growth of research theory, the transformation of the research paradigm, the evolution of the discipline field, and the identification of discipline structure. Common information visualization analysis software includes ArnetMiner (expert retrieval system), PaperLens (data relation mining), TDA (Thomson data analysis), and CiteSpace. Compared with other software, CiteSpace software integrates cluster analysis, social network analysis, multidimensional scale analysis, and other methods, focusing on detecting and analyzing the evolution trend of the discipline research frontier, the relationship between the research frontier and its knowledge base, and the internal relationship between different research frontiers.10–12 Bibliometric techniques, however, have not been used in the field of intestinal flora and asthma. In this study, we applied CiteSpace visualization analysis software to investigate changes in research directions in the recent 20 years in the areas of intestinal flora and asthma literature.
Methods
Data Sources
The literature data used in our study was extracted from the Web of Science (WOS) core collection according to the undermentioned search parameters. After integrating duplicate references, a total of 613 English articles were finally included, covering original articles, reviews, and other sorts of publications. The ultimate choice for the literature’s time period covered the years 2001 through 2021 with 1-year time slice. Citespace (version number: 5.6.R5) software was applied to conduct the bibliometrics and visualization analysis.
Search Parameters
The keywords were set as “intestinal flora or gut flora or intestinal microflora or gut microflora or intestinal microbiota or gut microbiota or bowel microbiota or bowel flora or gut bacteria or intestinal tract bacteria or bowel bacteria” AND “asthma or bronchial asthma”. The time span is selected in “2001–2021”, the language is “English”, and the document type is “article”.
Analysis
In order to reveal the distribution and development trend of the intestinal flora and asthma field, CiteSpace (Version: 5.6.R5) was used to perform multidimensional statistics and analysis on the publishing institutes, number, research direction, and keyword co-occurrence of research papers on intestinal flora and asthma collected in the WOS core collection.
In the network graph, different nodes reflected different factors, including authors, institutions, nations, and keywords. The size of the nodes was positively correlated with the quantity or frequency. The coordination between the nodes is depicted by the connection lines between them. Additionally, centrality shows how the nodes function in the knowledge network and how one node affects other nodes. Greater centrality indicated the increased likelihood of a node becoming a network’s hub node.
Results
Publication Years
Figure 1 shows the annual number of papers on intestinal flora and asthma. According to the overall analysis, the number of papers is increasing yearly, particularly during the 2013–2017 period. It can be seen from the calculation that the number of documents issued in 2017 has increased dramatically, and the number of articles increased 3.4 times compared with 2013, and the growth rate even up to 59.9% in a single year. After 2017, there was still an endless stream of articles related to intestinal flora and asthma, indicating that in the past decade, great attention has been paid to the role of intestinal flora in the pathogenesis of asthma.
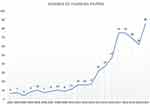 |
Figure 1 Trend chart of the number of articles published in relation to intestinal flora and asthma. |
Institutions Analysis
We applied the Network Summary Table tool to get the top 20 institutions by the number of publications (Table 1) and examined the cooperation network maps for each institution for the topic (Figure 2). As is shown in Table 1, the majority of the top 20 publications are from developed countries, and the institution with the most articles published is Univ British Columbia (21), followed by Karolinska Inst (19), Univ Alberta (15), Univ Manitoba (15), Univ Helsinki (14), and so on. The top 5 institutions with the highest number of published articles account for 40% of the total articles published by the top 20 institutions, suggesting that the top 5 institutions conduct more in-depth research and play an essential role in the field of intestinal flora and asthma. Moreover, the top 15 institutional collaboration network demonstrates that institutional collaboration already exists to some extent, but it can yet be strengthened (Figure 2).
 |
Table 1 Top 20 Institutes Publishing Research on Intestinal Flora and Asthma |
 |
Figure 2 Top 15 collaboration networks of institutions on intestinal flora and asthma. |
Authors Analysis
Table 2 shows the authors with the top number of published articles on intestinal flora and asthma from 2001 to 2021. Each of the 13 authors on the list has published five articles or more. From the perspective of the number of articles issued, the scholars with the most articles published are STURT E TURVEY (11), followed by BRETT FINLAY (10), PADMAJA SUBBARAO (9), ALLAN B BECKER (9), and MALCOLM R SEARS (8). Meanwhile, as evidenced by the author cooperation network (Figure 3), the top five authors emerged as the most prominent core in this field, laying the strong foundation for academic research. Additionally, there has good connections and close cooperation between the authors, which is conducive to the sound and solid development of the field.
 |
Table 2 Top 13 Authors with the Most Publications on Intestinal Flora and Asthma |
 |
Figure 3 Collaboration network of authors on intestinal flora and asthma. |
Keywords Distribution
Figure 4 depicts eight keyword clusters in the co-occurrence network on intestinal flora and asthma, including antibiotics, child, particle, caesarean delivery, microbiome, short-chain fatty acids, Lactobacillus rhamnosus GG, oral tolerance and microbiota. And different keyword clusters have strong symbiotic relationships. A more affluent and more thorough keyword distribution with timeline is displayed in Figure 4, including the eight keyword clusters listed above. Noticeably, “antibiotics” appeared in 2001 and generated a research boom in the subsequent years, which emerged as a keyword with the most significant long-term influence until 2021. In 2007, “microbiota” keyword first became apparent. After that, “lactobacillus” emerged as a popular keyword around 2010, and a large number of links between keywords appeared, including links within and across clusters, indicating that the bacterium played a specific role in the pathogenesis of asthma and allergic diseases. The number of connections between clusters decreased after 2016, indicating that scholars can carry out extended research in cross-cluster subject areas to serve as a new entry point for current research. By 2016, short-chain fatty acids and other keywords appear successively.
According to the development and changes in this field, the development of the keywords in the area of intestinal flora and asthma can be divided into two stages: 2001–2010 (initial research) and 2011 to now (development stage) (Figure 5). As is clear, the initial research stage mainly focused on the general direction of microbiota or allergy. During the development stage, a more intensive and subdivided pathological and physiological mechanism study with a solid theoretical foundation was conducted, with keywords including the hygiene hypothesis, airway inflammation, dysbiosis, regulatory T (Treg) cell, metabolism, and chain fatty acid. Furthermore, the presence of “metabolism” and “chain fatty acid” in the later development stage demonstrates that the research direction in this area has recently evolved towards microscopy, which may be due to the development and maturation of emerging technologies such as chromatography mass spectrometry and metabolomics.13,14
 |
Figure 5 Keyword development stages on intestinal flora and asthma. |
Hot Spot Burst Analysis
Figure 6 shows 23 prominent words such as infection, children, and prevalence. As can be observed, intestinal microflora, as the keyword with the longest duration of emergence, has a span of 12 years. In terms of allergic diseases, hay fever (2001–2006) first appeared, followed by eczema and atopic dermatitis (2005–2014 and 2007–2013, respectively), and childhood asthma (2012–2017) last, indicating that the understanding of intestinal flora and allergic diseases has altered over time. Furthermore, probiotics appeared in 2010–2014, and Treg cells presented subsequently in 2014–2018 as the hot spot. The keywords transformation suggests that research content on intestinal flora and diseases has a trend from macro to micro.
 |
Figure 6 Burstness map of keywords on intestinal flora and asthma. |
Discussion
The study performed a bibliometric analysis of the research papers on the field of intestinal flora and asthma in 2001–2021 from the WOS core collection. Especially over the past decade, research on gut flora and asthma continued to heat up with article numbers increasing. In addition, we also found that the research topics of intestinal flora and asthma range from confirming the link between intestinal flora and asthma to investigating mechanisms and then to asthma treatment.
Antibiotics appeared for the first time in 2001, and since then, they have also been emerging in research, indicating that the effect of the antibiotic application on the change of intestinal flora is a research hotspot of scholars. Antibiotics, as a powerful tool for anti-infection treatment, have attracted more and more attention, and their intervention in intestinal flora could have affected the onset of allergic diseases.15
Subsequently, around 2010, with the hygiene hypothesis appearing in the keyword line zone, scholars gradually reached an agreement that changes in gut microbiota composition might affect the maturation of the immune system and further lead to allergic diseases.16 From the keywords change, researchers early focused on whether the factors affecting intestinal flora, such as antibiotics, cesarean section, and diet, were related to allergic diseases, especially bronchial asthma. Later, the research gradually deepened, trying to clarify the specific immune mechanisms of asthma caused by changes in the intestinal flora, such as the relationship between particular flora and asthma, as well as the related treatments.
Combining with the summary of research hotspots and history mentioned above, we expand on three emerging issues that require attention in the intestinal flora and asthma research and involve mechanisms and treatments, including Treg cells, probiotics, and chain fatty acid.
First of all, Treg cells. We can see that Treg cells continued as the keyword from 2014 to 2018, which indicated that researchers started looking into the underlying mechanism after researching the connection between intestinal flora and asthma. Furthermore, numerous previous studies have shown that impaired Treg cell immunosuppressive function is one of the critical factors in the pathophysiology of asthma. In addition to being reduced in number, Treg cells in asthma patients can also not effectively suppress inflammation induced by activated effector helper T cells, eventually resulting in airway inflammation and airway remodeling correlated to asthma.17,18 However, disrupted intestinal flora tends to interfere with the immune tolerance to allergens, maintained by the Treg cells mentioned above, increasing allergy susceptibility, including asthma susceptibility.19
Second, probiotics. The onset of adult asthma symptoms might develop from childhood20; thus, it is crucial to control asthma in newborns and children early, frequently, and permanently. Meanwhile, infancy is the key period for intestinal flora establishment, which could provide the groundwork for mature intestinal flora in adulthood.21 Studies have shown that short-term early microbial ecological dysregulation might be a critical factor influencing the occurrence of subsequent asthma.22 Consistently, “children” or “child” or “childhood” or “childhood asthma” became a succession of keyword in the field of asthma and intestinal flora in the past two decades (Figures 4–6). In addition, evidence discovered that children at risk for asthma had considerably lower relative abundances of the bacterial genera Lachnospira, Veillonella, Faecalibacterium, and Rothia. Subsequently, these four bacterial taxa were administered to germ-free mice, and their adult offspring experienced reduced airway inflammation, which demonstrated the potential role of intestinal flora changes in the development of asthma.23 Therefore, many scholars suspected that the probiotic supplements played a certain role in relieving asthma. Indeed, Lactobacillus became a popular keyword around 2010, and there were many links between Lactobacillus and other keywords. The research boom on the “probiotics” keyword also continued from 2010 until 2014. Nevertheless, according to years of research advancement and study collections, it was found that probiotic supplements (including Lactobacillus), whether during pregnancy or infancy, could not reduce the risk of asthma in children at age 2 or 6 years.24–28 In recent decades, researchers have constantly been looking for efficient asthma remedies, and probiotic supplement therapy is a great and meaningful practice, even though there was no discernible link between probiotic supplements and a decreased risk of asthma.
Third, chain fatty acid. Numerous pieces of evidence have shown short-chain fatty acids (SCFAs) as the primary mediators of the lung-gut axis, effectively reducing lung pro-inflammatory reactions in asthma.29 However, long-chain n-3 fatty acid supplementation during pregnancy could lower the incidence of asthma in children with limited and low-intensity evidence, and supplementation during lactation could not.30,31 Precisely, SCFAs mainly derived from gut microbiota metabolism and were intimately related to certain foods, including butyrate, propionate, and acetate.32 Notably, the research found that fecal butyrate levels were significantly lower in asthma children compared to children without asthma. Low fecal butyrate is linked to higher levels of mite-specific IgE and an increased risk of asthma in children.33 Another prospective birth cohort study also demonstrated that children with the highest levels of butyrate and propionate (≥95th percentile) in feces at 1-year old were at lower risk of developing asthma between 3 and 6 years.34 Moreover, a slew of animal studies has established that SCFAs may improve asthma airway inflammation by suppressing airway hyperreactivity driven by group 2 innate lymphoid cells, inducing neutrophil and eosinophil apoptosis, increasing Treg numbers and activity in both the intestinal lymph nodes and the spleen, and so on.29,35,36 In conclusion, SCFAs could improve asthma. Meanwhile, dietary SCFAs are the most secure and cost-effective way to impact the large global patient population. Therefore, dietary therapy for SCFA supplementation may be a workable therapeutic option for preventing and alleviating asthma in children.
Collectively, the study of intestinal flora and asthma covers a wide range of subjects, including establishing a connection, examining the mechanisms involved, and finally developing treatments. Evidence suggests that Treg cells play a significant role in the pathogenesis of asthma caused by dysbiosis of the gut flora, and that probiotic supplements do not reduce the risk of asthma, whereas SCFA supplementation does. Additionally, a diet rich in fruits and vegetables with antioxidant vitamins may have possible anti-inflammatory qualities that reduce the chance of developing asthma.37,38 In summary, the trend and development of intestinal flora and asthma research showed a significant link between gut flora and the occurrence and treatment of asthma. The focus of the studies has gradually broadened over time, as has the depth, but there is still potential for further branched. It is expected to prevent and treat asthma through the regulation of gut flora. However, further research and experiment are required to elucidate deeper connections and more specific mechanisms between asthma and gut flora in order to achieve precision therapy.
Moreover, the study has some limitations. Firstly, we only covered English-language publications, which may result in selection bias. Secondly, the study was based only on the WOS database. Even though the WOS database was known to have a relatively reliable database, including more than 12,000 of the greatest impact and quality scientific journals,39 it will inevitably lead to bibliography omissions. Third, Citespace could provide a macro-level picture built on the concept of co-occurrence clustering, which benefited hotspot analysis and trend prediction in a field but not for less abundant investigated studies that cannot become hotspots or clusters.
Conclusion
From 2001 to 2021, the number of intestinal flora and asthma articles increased rapidly with good cooperation between different authors, countries, and institutions. The research direction in this area has recently evolved from macro to micro with depth broadened. As a robust scientific evaluation, the study provided a comprehensive overview of the field, particularly for research focus, which could more precisely direct scholars on future research and clinical diagnosis, therapy, and individualized prevention.
Acknowledgments
We are indebted to The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University for supporting the research.
Funding
This research was supported by the Wenzhou Municipal Science and Technology Bureau (Y20210006).
Disclosure
The authors declare that the study was conducted in the absence of any commercial or financial relationships that could be explained as a potential conflict of interest.
References
1. Soriano JB, Abajobir AA, Abate KH, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5(9):691–706. doi:10.1016/S2213-2600(17)30293-X
2. Hufnagl K, Pali-Schöll I, Roth-Walter F, Jensen-Jarolim E. Dysbiosis of the gut and lung microbiome has a role in asthma. Semin Immunopathol. 2020;42(1):75–93. doi:10.1007/s00281-019-00775-y
3. Salameh M, Burney Z, Mhaimeed N, et al. The role of gut microbiota in atopic asthma and allergy, implications in the understanding of disease pathogenesis. Scand J Immunol. 2020;91(3):e12855. doi:10.1111/sji.12855
4. Kuruvilla ME, Vanijcharoenkarn K, Shih JA, Lee FE. Epidemiology and risk factors for asthma. Respir Med. 2019;149:16–22. doi:10.1016/j.rmed.2019.01.014
5. Stern J, Pier J, Litonjua AA. Asthma epidemiology and risk factors. Semin Immunopathol. 2020;42(1):5–15. doi:10.1007/s00281-020-00785-1
6. Dang AT, Marsland BJ. Microbes, metabolites, and the gut-lung axis. Mucosal Immunol. 2019;12:843–850. doi:10.1038/s41385-019-0160-6
7. Gensollen T, Iyer SS, Kasper DL, Blumberg RS. How colonization by microbiota in early life shapes the immune system. Science. 2016;352(6285):539–544. doi:10.1126/science.aad9378
8. Levan SR, Stamnes KA, Lin DL, et al. Elevated faecal 12,13-diHOME concentration in neonates at high risk for asthma is produced by gut bacteria and impedes immune tolerance. Nat Microbiol. 2019;4(11):1851–1861. doi:10.1038/s41564-019-0498-2
9. Ottman N, Ruokolainen L, Suomalainen A, et al. Soil exposure modifies the gut microbiota and supports immune tolerance in a mouse model. J Allergy Clin Immunol. 2019;143(3):1198–1206.e12. doi:10.1016/j.jaci.2018.06.024
10. Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101(Suppl 1):5303–5310. doi:10.1073/pnas.0307513100
11. Dufault B, Klar N. The quality of modern cross-sectional ecologic studies: a bibliometric review. Am J Epidemiol. 2011;174:1101–1107. doi:10.1093/aje/kwr241
12. Zheng M, Fu H-Z, Ho Y-S. Research trends and hotspots related to ammonia oxidation based on bibliometric analysis. Environ Sci Pollut Res Int. 2017;24:20409–20421. doi:10.1007/s11356-017-9711-0
13. Zhang S, Wang H, Zhu M-J. A sensitive GC/MS detection method for analyzing microbial metabolites short chain fatty acids in fecal and serum samples. Talanta. 2019;196:249–254. doi:10.1016/j.talanta.2018.12.049
14. Patti GJ, Yanes O, Siuzdak G. Innovation: metabolomics: the apogee of the omics trilogy. Nat Rev Mol Cell Biol. 2012;13:263–269. doi:10.1038/nrm3314
15. Russell SL, Gold MJ, Hartmann M, et al. Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep. 2012;13:440–447. doi:10.1038/embor.2012.32
16. Brown EM, Arrieta M-C, Finlay BB. A fresh look at the hygiene hypothesis: how intestinal microbial exposure drives immune effector responses in atopic disease. Semin Immunol. 2013;25(5):378–387. doi:10.1016/j.smim.2013.09.003
17. Chen W, Cao Y, Zhong Y, Sun J, Dong J. The mechanisms of effector Th cell responses contribute to treg cell function: new insights into pathogenesis and therapy of asthma. Front Immunol. 2022;13:862866. doi:10.3389/fimmu.2022.862866
18. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45–56. doi:10.1038/ni.3049
19. Bellinghausen I, Khatri R, Saloga J. Current strategies to modulate regulatory T cell activity in allergic inflammation. Front Immunol. 2022;13:912529. doi:10.3389/fimmu.2022.912529
20. Fuchs O, Bahmer T, Rabe KF, von Mutius E. Asthma transition from childhood into adulthood. Lancet Respir Med. 2017;5(3):224–234. doi:10.1016/S2213-2600(16)30187-4
21. Milani C, Duranti S, Bottacini F, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. 2017;81. doi:10.1128/MMBR.00036-17
22. Zhuang L, Chen H, Zhang S, Zhuang J, Li Q, Feng Z. Intestinal microbiota in early life and its implications on childhood health. Genomics Proteomics Bioinformatics. 2019;17:13–25. doi:10.1016/j.gpb.2018.10.002
23. Arrieta MC, Stiemsma LT, Dimitriu PA, et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med. 2015;7(307):307ra152. doi:10.1126/scitranslmed.aab2271
24. Abrahamsson TR, Jakobsson T, Björkstén B, Oldaeus G, Jenmalm MC. No effect of probiotics on respiratory allergies: a seven-year follow-up of a randomized controlled trial in infancy. Pediatr Allergy Immunol. 2013;24(6):556–561. doi:10.1111/pai.12104
25. Matsui E. No effect of probiotics on respiratory allergies: a seven-year follow-up of a randomized controlled trial in infancy. Pediatrics. 2014;134(Suppl 3):S141–S142. doi:10.1542/peds.2014-1817P
26. Gorissen DMW, Rutten NBMM, Oostermeijer CMJ, et al. Preventive effects of selected probiotic strains on the development of asthma and allergic rhinitis in childhood. The panda study. Clin Exp Allergy. 2014;44:1431–1433. doi:10.1111/cea.12413
27. Cabana MD, McKean M, Caughey AB, et al. Early probiotic supplementation for eczema and asthma prevention: a randomized controlled trial. Pediatrics. 2017;140:e20163000.
28. Wei X, Jiang P, Liu J, Sun R, Zhu L. Association between probiotic supplementation and asthma incidence in infants: a meta-analysis of randomized controlled trials. J Asthma. 2020;57:167–178. doi:10.1080/02770903.2018.1561893
29. Ashique S, De Rubis G, Sirohi E, et al. Short chain fatty acids: fundamental mediators of the gut-lung axis and their involvement in pulmonary diseases. Chem Biol Interact. 2022;368:110231. doi:10.1016/j.cbi.2022.110231
30. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;2015:CD010085. doi:10.1002/14651858.CD010085.pub2
31. Barebring L, Nwaru BI, Lamberg-Allardt C, et al. Supplementation with long chain n-3 fatty acids during pregnancy, lactation, or infancy in relation to risk of asthma and atopic disease during childhood: a systematic review and meta-analysis of randomized controlled clinical trials. Food Nutr Res. 2022;66. doi:10.29219/fnr.v66.8842
32. Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell. 2016;165(6):1332–1345. doi:10.1016/j.cell.2016.05.041
33. Chiu C-Y, Cheng M-L, Chiang M-H, et al. Gut microbial-derived butyrate is inversely associated with IgE responses to allergens in childhood asthma. Pediatr Allergy Immunol. 2019;30(7):689–697. doi:10.1111/pai.13096
34. Roduit C, Frei R, Ferstl R, et al. High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy. 2019;74(4):799–809. doi:10.1111/all.13660
35. Lewis G, Wang B, Shafiei Jahani P, et al. Dietary fiber-induced microbial short chain fatty acids suppress ILC2-dependent airway inflammation. Front Immunol. 2019;10:2051. doi:10.3389/fimmu.2019.02051
36. Yip W, Hughes MR, Li Y, et al. Butyrate shapes immune cell fate and function in allergic asthma. Front Immunol. 2021;12:628453. doi:10.3389/fimmu.2021.628453
37. Guilleminault L, Williams EJ, Scott HA, et al. Diet and asthma: is it time to adapt our message? Nutrients. 2017;9(11):1227. doi:10.3390/nu9111227
38. Garcia-Larsen V, Del Giacco SR, Moreira A, et al. Asthma and dietary intake: an overview of systematic reviews. Allergy. 2016;71(4):433–442. doi:10.1111/all.12800
39. Shi Y, Wei W, Li L, et al. The global status of research in breast cancer liver metastasis: a bibliometric and visualized analysis. Bioengineered. 2021;12(2):12246–12262. doi:10.1080/21655979.2021.2006552
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

