Back to Journals » Journal of Asthma and Allergy » Volume 16
Prevalence and Characteristics of Self-Reported Adult Asthma in Cyprus: A Population-Based Observational Study
Authors Benidis KD, Tzortzaki E, Georgiou A, Zachariadou T, Adamidi T, Zannetos S , Bakakos P, Koulouris NG , Rovina N
Received 16 November 2022
Accepted for publication 17 January 2023
Published 22 February 2023 Volume 2023:16 Pages 215—226
DOI https://doi.org/10.2147/JAA.S397784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Kleomenis D Benidis,1 Eleni Tzortzaki,2 Andreas Georgiou,1 Theodora Zachariadou,3 Tonia Adamidi,1 Savvas Zannetos,4 Petros Bakakos,5 Nikolaos G Koulouris,5 Nikoletta Rovina5
1Respiratory Department, Nicosia General Hospital, Nicosia, Cyprus; 2Outpatient Respiratory Clinic, Heraklion, Greece; 3Health Center of Engomi, Nicosia, Cyprus; 4Department of Healthcare Management, Neapolis University Paphos, Paphos, Cyprus; 5 1st Respiratory Department, National and Kapodistrian University of Athens Medical School, “Sotiria” Chest Hospital, Athens, Greece
Correspondence: Nikoletta Rovina, Pulmonary and Critical Care Medicine, National and Kapodistrian University of Athens & ICU, First Department of Pulmonary Medicine, Sotiria Hospital, Athens, 115 27, Greece, Email [email protected]
Purpose: To estimate the prevalence of asthma in adults, by gender and age, in urban and rural areas of Cyprus.
Patients and Methods: This was a population-based, random-digit dialing, telephone nation-wide survey to recruit patients with asthma. Among 8996 random landline-telephone contacted from the five major urban and rural regions of Cyprus, 1914 were finally met the age criterion of ≥ 18 years old and 572 completed valid screening for prevalence estimation. The participants filled a short screening questionnaire in order for asthma cases to be recognized. Then, asthma cases filled the main ECRHS II questionnaire and were evaluated by a pulmonary physician. All underwent spirometry. Data on demographic characteristics, educational level, profession, smoking status, Body Mass Index (BMI), Total IgE and Eosinophil Cationic Protein levels were measured.
Results: The overall prevalence of bronchial asthma in adults in Cyprus was 5.57% (61.1% men and 38.9% women). Among the participants with self-reported bronchial asthma 36.1% were current smokers, while 12.3% were obese (BMI > 30). A total value of IgE > 115 IU and Eosinophil Cationic Protein (ECP) > 20 IU was found in 40% of the participants with established bronchial asthma. Wheezing and chest tightness were the most frequently reported symptoms in asthma patients (36.1% and 34.5%, respectively), while 36.5% experienced at least one exacerbation during the last year. Interestingly, most of the patients were under-treated (14.2% were on maintenance asthma treatment, and 18% used solely reliever medication).
Conclusion: This was the first study estimating asthma prevalence in Cyprus. Asthma affects almost 6% of the adult population, with higher prevalence in urban areas and in men compared to women. Interestingly, one-third of the patients were uncontrolled and under-treated. This study revealed that in Cyprus there is space for improvement in the management of asthma.
Keywords: asthma, allergy, prevalence, Cyprus
Introduction
Asthma is a heterogeneous lung disease with different phenotypes, characterized by airway inflammation, reversible airflow limitation1 and various respiratory symptoms. Asthma remains a major health problem world-wide affecting 1–18% of the population in different countries.1 According to GINA and the European Community Respiratory Health Survey (ECHRS) and International Study of Asthma and Allergies in children (ISAAC) studies, it is expected that 400 million people of all ages will suffer from bronchial asthma by the year 2025.1–5
ISAAC the and ECRHS, two multicenter studies, have confirmed the variations of bronchial asthma worldwide in prevalence and manifestation. Prevalence of asthma ranged from 0.7% in Macau, 2% to 3.3% in Estonia, Germany, Spain, Austria and Algeria, 8% to 11.9% in the United Kingdom, New Zealand, and Australia, and 18.4% in Scotland.2–5 Similarly, the prevalence of asthma-like symptoms varied across countries; wheeze ranged from 4.1% to 9.7% in India, Algeria and Italy, 19% in Greece, 23% to 32% in Sweden, Estonia, Denmark, USA, UK, Ireland and Australia.6–11 An additional survey, designed by the World Health Organization (WHO) in 70 countries, the World Health Survey (WHS) estimated that the global prevalence of clinical/treated asthma in adults aged 18–45 was 4.5% (178.215 participants).11
A recent population-based, random-digit dialing, telephone nationwide survey in Greece revealed that the lifetime self-reported prevalence of asthma was 9.10%.7 Up to now, limited data exist on asthma prevalence in Cyprus. The first study investigating the prevalence of asthma and allergies in children, using the ISAAC questionnaire, revealed an overall prevalence of 6.9%.12 However, little data exist on adult asthma. In 2008, the National Statistical Service of Cyprus estimated that self-reported asthma prevalence was 5.1%.13 However, this percentage is expected to be higher given the increase of asthma prevalence worldwide along with asthma diagnosis improvement.14–17 The fact that the prevalence of asthma and allergic diseases, in Cyprus is on the rise was initially shown in the paediatric population by Kolokotroni et al nearly ten years ago.18 Several risk factors for asthma development in Cyprus were acknowledged by these authors and others mainly pointing to environmental and lifestyle determinants.19–21 Furthermore, a recent study on asthma economic burden in Cyprus estimated that the mean asthma patient cost was €579.64 with indirect costs accounting for 17.92% of the overall health expenses.22 Thus, it is particularly important to estimate the prevalence of asthma in adults, as this is directly linked to the economic burden of the disease and could further guide the national policy of the Cyprus Healthcare System.
The aim of our study was to estimate the prevalence of bronchial asthma in adults by age and gender, in urban and rural areas of Cyprus. Data on demographic characteristics, educational level, profession, smoking status, asthma symptoms, total IgE levels and ECP values were collected to better recognize the main characteristics of the disease in the Greek-Cypriot population.
Patients and Methods
This two-stage report-based study covered a wide geographical range of Cyprus and a total population of more than 865,000 Greek-Cypriots, aged ≥18 years. The classification of the population by gender and region, urban and rural, was based on the geographical distribution of the population stated in the annual demographic report of the Statistical Service of Cyprus.14 The study population was allocated to the five geographical regions of the Republic of Cyprus; Nicosia Larnaca, Paphos, Limassol and Ammochostos. The Nicosia region included a total population of 336,900 people; Limassol included 241,830; Larnaca 147,200; Paphos 91,940 and Ammochostos 47,900 people. The total number of inhabitants and number of subjects that completed the first screening per geographical region are shown in Figure 1 and Table 1.
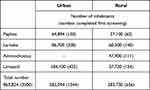 |
Table 1 The Table Shows the Total Number of Inhabitants and of Participants Completed the First Screening (in Brackets) in Urban and Rural Areas of the Five Geographical Regions of Cyprus |
Figure 2 illustrates the study consort diagram. Individuals were randomly selected using the telephone directory of Cyprus (comprises more than 90% of households-population). A random-digit telephone dialing was used, and more than 8900 telephone calls were attempted to define the final participant number. A random-digit telephone dialing was used, and more than 8900 telephone calls were attempted. Our aim was to define the final participants’ number. Phone calls were attempted between 28/9/2016 and 16/11/2016 and a total number of 1914 (21.3%) participants met the age criterion. All individuals completed an informed consent form and thereafter answered a screening questionnaire in Greek based on the ECRHS survey questionnaire (Appendix 1 and 2).23
 |
Figure 2 Study consort diagram. |
Valid screening was completed in 572 participants. Since we had a representative sample size of the population at the first stage of the survey, we matched the potential asthma patients with a control that bears the same demographic characteristics in a second stage of analysis, given the original strata we used at stage 1. The inclusion criteria for the case group were any positive answer of the first seven questions of the screening questionnaire (Appendix 1). Individuals with negative answers to the above questions were allocated to the control group of the study. Each group was comprised of 200 and 194 individuals, respectively, so as gender, urban and rural regions of Cyprus, and geographical characteristics of the five regions to be represented.
For all eligible participants (N = 394) from both groups (case and control) an appointment was fixed with a respiratory physician at the Respiratory Department of Nicosia General Hospital, or regional hospitals (Limassol, Paphos and Larnaca Pulmonary Clinics) at each participating region of Cyprus. Exclusion criteria for the second phase of the study were only pregnancy and age ≤18 years old. During this visit, each participant signed an informed consent. All individuals answered a detailed main questionnaire of 47 questions in Greek (interview with pulmonologist face to face) based on the ECRHS II survey.23 This included questions on demographics, occupational interests, asthma-like symptoms, comorbidities treated or untreated, allergy and smoking history.
Thereafter, each participant underwent lung function testing – spirometry before and after bronchodilation. All tests were performed with portable spirometers (Spirolab II), according to the American Thoracic Society (ATS) and European Respiratory Society (ERS) recommendations.24 The spirometers were calibrated with a 3-Liter syringe (calibration limits of ±3%) daily. The individuals performed up to eight forced expiratory maneuvers until achieving three acceptable lung function tests with the best values of forced expiratory volume at the first second of expiration (FEV1) and forced vital capacity (FVC).24 The post bronchodilation lung function tests were performed 15 minutes after the inhalation of 400μg salbutamol (Inh Ventolin; Glaxo Smith Kline) via a spacer device. All the participants underwent blood analyses for the measurement of total IgE and Eosinophil Cationic Protein (ECP).
The prevalence of asthma among the eligible study population was defined according to the medical history of the participants, lung function tests (spirometry, pre and post bronchodilation) and GINA criteria,1 measurement of total IgE and Eosinophil Cationic Protein levels.25,26
Statistical Analysis
For the statistical analysis of the data, all the answers were coded to proceed in statistical processing with the statistical program IBM SPSS Statistics v25. The statistical analysis of the survey data at the descriptive level included: tables of frequency distribution of the answers of the respondents when the variables were nominal and means (standard deviation) when the variables were continuous. In all cases of statistical tests, α = 0.05 was used as the minimum level of statistical significance and the value was rounded to 3 decimal places.
Results
A total of 8996 individuals were contacted by phone. Of those, 7082 subjects (78.7%) did not answer the phone at all or did not give their consent to participate in the survey. Α total of 1914 individuals (21.3%) participated in the first stage of the study (Figure 2). Most of the participants were men (62.4%). The mean age of the study population was 48.5 years old and the mean body mass index (BMI) was 27.1. Among the participants, 55.4% lived in urban areas whereas 44.6% lived in rural areas. Regarding the educational status of the participants 9.4% had completed primary school, 29.8% high school and 51% had a University degree. Regarding occupation, 8.2% were unemployed, 36.7% were employed in the private sector, 17.6% were government employees, and 17.1% were pensioners. One-third (33%) of the study population were current smokers (pack-years 29±11, mean±SD), and one-fifth (21%) were ex-smokers (pack-years 32±15, mean±SD). One out of four (24.8%) reported any type of allergies (asthma, rhinitis, dermatitis, eczema, conjunctivitis) while 327 (17.1%) reported an asthma diagnosis by a physician (Figure 3).
Respiratory Symptoms and Characteristics of the Subjects with Self-Reported Asthma (First Stage of the Survey)
Bronchial asthma prevalence was higher in men (61%) than in women (39%), and in the age group of 41–59 years (41.7%) as compared to age groups ≤40 years old (27.8%) and ≥60 years old (30.6%). Among the participants with self-reported asthma 36.1% were current smokers. Forty percent of them had IgE levels higher than 115 IU, and Eosinophil Cationic Protein (ECP) higher than 20 IU. For the participants in whom asthma was not evident, these percentages were 26.3% and 21.3%, respectively.
Self-reported respiratory symptoms in those completed the first screening (N = 1914) and those with asthma confirmed by a physician (N = 327) are shown in Figure 4. Wheezing and chest tightness were the most frequently reported symptoms in asthma patients (36.1% and 34.5%, respectively), with early morning dyspnea occurring in 25.3% and night awakenings due to respiratory symptoms occurring in 13.7%. Self-reported symptoms were statistically significantly more evident in asthma patients compared to these reported in the population of the first screening (Figure 4). Of note, although 86.5% of participants with self-reported asthma had a diagnosis by a physician, only 14.2% were on maintenance asthma treatment, and 18% used solely reliever medication. Among asthma patients, 36.5% experienced at least one exacerbation during the last year (Figure 5). Furthermore, it is interesting that the diagnosis and follow-up of asthma was made by a respiratory physician in half of the cases, while the rest were assessed by physicians of internal medicine (32.1%), general practitioners (9%), allergists (5.5%), or physicians of some other specialty (3.5%) (Figure 6).
 |
Figure 4 Self-reported respiratory symptoms in those completed the first screening (N = 1914) and those with self-reported asthma (N = 327). *Indicates statistical significant difference, p < 0.05. |
 |
Figure 5 Management of asthma in patients with self-reported asthma (N = 327). |
 |
Figure 6 Physicians handling asthma in Cyprus. |
Asthma Prevalence
The overall prevalence of bronchial asthma in adults estimated as 5.57% and was defined according to the medical history of the participants (screening and main questionnaires), lung function tests (spirometry pre and post bronchodilation, GINA criteria).1,17,18
Anthropometric characteristics and descriptive statistics of the study population (394 subjects) are shown in Table 2. The spirometric measurements, and measurements of total IgE, and ECP in the matched case-control groups (n = 394) are shown in Table 3.
 |
Table 2 Anthropometric Characteristics of the Study Population |
 |
Table 3 The Spirometric Measurements and Measurements of Total IgE, and ECP in the Study Population (394 Subjects) |
From the analysis of the matched groups (asthma and control, 394 subjects) in the second phase of the survey asthma was found more often in men than in women (63.2 versus 36.8%), in accordance to the observation from the first screening. Asthma patients had a higher percentage of unemployment compared to the control group (Table 2). Furthermore, asthma patients had significantly lower FEV1/FVC, and higher reversibility compared to the control group. No significant difference was found in IgE levels between the groups. ECP >20 IU was statistically significantly higher in the control group (Table 3).
Discussion
This is the first, two-stage population-based study, on asthma prevalence in Cyprus. The strength of this endeavor was the two stages design, comprised initially with a phone interview (first stage) followed by a face-to-face consultation by a respiratory physician, spirometry evaluation and blood test analyses (second stage). It is also the first national study that covered a wide geographical area of Cyprus and a total population of more than 865,000 Greek-Cypriots.
The overall prevalence of adult bronchial asthma in Cyprus was estimated to be 5.57%. Although there are no official data for the prevalence of adult asthma in Cyprus, a self-reported percentage was estimated at 5.1% by the National Statistical Service in 2008.27 The prevalence of adult asthma in Cyprus is estimated to be much lower than the reported in children. In 2008, the ISAAC questionnaire estimated an overall asthma prevalence in Cypriot children aged 7–8 years of 17.4%.18 Few years later, Middleton et al19 reported the prevalence of active asthma in 15–17-year-old Greek Cypriot teenagers ranging between 5% and 7.4% depending on the exposure to power plants. Although rising, the prevalence of adult asthma in Greek-Cypriots is much lower than the lifetime self-reported prevalence of asthma in Greece (9.10%)7,28 or other countries in the Mediterranean region.30,31
Our study revealed higher asthma prevalence in men compared to women in contrast to data coming from Greece and surveys in other countries.7,32,33 Although this study was not designed to investigate the causes of asthma, the difference between males and females could be attributed to social variables, and variances in indoor and outdoor environmental exposure (occupation, smoking, etc.) between sexes in this island. Interestingly, asthma was more frequent in the age range of 41–59 years. It is evident from this survey that with almost 70% of asthmatic patients belonging to the productive period of human life span (<60 years old) the economic burden of asthma may be substantial. Zannetos et al22 retrospectively estimated the economic burden of asthma in Cyprus based on a probabilistic prevalence-based cost of illness model that included direct and indirect costs. The total cost of asthma per patient was estimated at €579.64 (95% CI: €376.90–€813.68), with the highest costs referring to asthma medication accounting for 35.88% of the overall cost of the disease and 43.70% of the direct costs.22
Differences in asthma prevalence were found in the various geographical regions of Cyprus, with higher asthma prevalence reported in urban areas, such as Nicosia, as compared to Ammochostos which is a mainly rural region. These observations are in accordance with the findings of the Greek studies,6,7,28,34 but also with the reports from other areas in the Mediterranean region and other countries assessing the self-reported prevalence of asthma in adult population.11,29–31 In Greece, although in 2012 the first nation-wide, cross-sectional, community-based survey of asthma and asthma-like symptoms using a questionnaire based on the ECRHS revealed higher asthma prevalence in Athens (10.9%) with no significant difference between rural and urban areas (8.5% and 7.8%, respectively),34 in 2018 the prevalence was found higher in urban areas.7 The variability in the prevalence of asthma may be attributed to the great variability of known risk factors of asthma across countries, like smoking prevalence, indoor and outdoor air pollution, obesity index and diet. Likewise, our study revealed that 36.1% of the participants with established bronchial asthma were current smokers, whereas the overall occurrence of smoking habit in the study population was 33%. The high prevalence of smoking remains a major barrier to combating the global burden of asthma.
The higher prevalence of asthma in urban areas is associated with a continuing rise in the prevalence of allergic diseases.35,36 In our survey, one out of four (24.8%) of the participants that completed the first screening reported seasonal allergy symptoms such as rhinitis, sneezing, conjunctivitis, etc, while increased levels of IgE (>115 IU) and of Eosinophil Cationic Protein (>20IU) were found in 40% of the asthmatic participants. These findings indicate an increased percentage of atopy in asthmatic and non-asthmatic population in Cyprus.17–19 The parallel rise in asthma and allergy prevalence in Cyprus was earlier documented in the study of Kolokotroni et al.18 This study investigated temporal changes in the prevalence of asthma and allergies in children of 7–8 years old in the two main urban districts of the Republic of Cyprus (Nicosia and Limassol) based on two cross-sectional surveys eight years apart (200 and 2008). During these eight years, allergic rhinitis and eczema were doubled while wheezing increased by 25%.
An interesting finding of this study, was that more than 35% of asthma patients had uncontrolled asthma, as wheezing, chest tightness, night symptoms/awakenings, and asthma attacks. This finding is in line with other reports from Greece6,7,28,34 and other European countries.37–40 Interestingly, although 86.5% of asthma patients were diagnosed by a physician, a low percentage of patients were on maintenance treatment or referred to a physician for an asthma attack. Half of the patients were followed-up by a chest physician, while the rest were referring to other specialties, such as internists, allergists and general practitioners. It is acknowledged that gaps in patient education by the physicians affect the quality of care provided resulting in patient’s dissatisfaction and critical errors in the use of medication and in the management of asthma. In a cross-sectional multi-centered observational study conducted in Nicosia and Ammochostos state hospitals in North Cyprus patients claimed that they were not well informed and were not satisfied with the information they received from the physicians regarding potential difficulties with their asthma management and side effects.41 This has also been demonstrated in several other studies42,43 underlying the extent of the problem.
At this point, we should acknowledge the limitations that telephone surveys and self-reported questionnaires may pose. Several reports acknowledge that they may lead to non-representative results for several reasons, namely households without telephone services are automatically excluded, the response rate seems to be lower comparing to the “face to face” surveys and the information provided could be misleading.19
Conclusions
This study indicated that asthma affects almost 6% of the adult population in Cyprus. It also revealed higher asthma prevalence in urban areas and in men compared to women. Interestingly, although 86.5% of asthma patients were diagnosed by a physician a low percentage of patients were on maintenance treatment. Half of the patients were followed-up by a chest physician, while the rest were referring to other specialties. It is acknowledged that gaps in patient education by the physicians affect the quality of care provided resulting in critical errors in asthma management.
Abbreviations
GINA, Global Initiative for Asthma; ISAAC, International Study of Asthma and Allergies in children; ECRHS, European Community Respiratory Health Survey; WHS, World Health Survey; ATS, American Thoracic Society; ERS, European Respiratory Society; FEV1, Forced Expiratory Volume at the first second of expiration; FVC, Forced Vital Capacity; IgE, Immunoglobulin IgE; ECP, Eosinophil Cationic Protein.
Data Sharing Statement
The data presented in this study are available in this article.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Sotiria Thoracic Diseases General Hospital, Athens, Greece (protocol number 24510, date of approval 5/12/2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
Authors would like to thank Cyprus Ministry of Health, and the Pulmonary Clinics in Nicosia, Limassol, Paphos, and Larnaca for their co-operation. The authors would also like to thank ELPEN PHARMACEUTICAL Co. Inc. for funding the publication fees.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received external funding from Cyprus Ministry of Health.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Bateman ED, Hurd SS, Barnes PJ, et al. GINA report, global strategy for asthma management and prevention; 2020.
2. Beasley R. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998;(97):7302–7309. doi:10.1016/S0140-6736
3. International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variations in the prevalence of asthma symptoms. Eur Respir J. 1998;12:315–335. doi:10.1183/09031936.98.12020315
4. Lai CK, Beasley R, Crane J, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the international Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2009;64:476. doi:10.1136/thx.2008.106609
5. Chinn S, Luczynska C, Jarvis D, et al.Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J. 1996;9:687. doi:10.1183/09031936.96.09040687
6. Zervas E, Loukides S, Kostikas K, Bakakos P, Tzortzaki E, Gaga M; On Behalf of Asthma Working Group of the Hellenic Thoracic Society. Asthma and asthma-like symptoms in Greece. The Greece asthma national prevalence survey. Eur Respir J. 2012;40:P3936.
7. Kourlaba G, Bakakos P, Loukides S, Vellopoulou K, Solakidi A, Maniadakis N. The self-reported prevalence and disease burden of asthma in Greece. J Asthma. 2019;56(5):478–497. doi:10.1080/02770903.2018.1471704
8. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA dissemination committee report. Allergy. 2004;59:469. doi:10.1111/j.1398-9995.2004.00526.x
9. Sembajwe G, Cifuentes M, Tak SW, et al. National Income, self-reported wheezing and asthma diagnosis from the World Health Survey. Eur Respir J. 2010;35:279. doi:10.1183/09031936.00027509
10. Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226. doi:10.1056/NEJMra054308
11. To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC public Health. 2012;12:204. doi:10.1186/1471-2458-12-204
12. Mitchell EA, Stewart AW; The ISAAC Phase One Study Group. The ecological relationship of tobacco smoking to the prevalence of symptoms of asthma and other atopic diseases in children: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur J Epidemiol. 2001;17:667–673. doi:10.1023/A:1015500508261
13. Faustmann H. Statistical service of the Republic of Cyprus; Special Edition: European Health Survey; 2008.
14. Burr ML, Butland B, King S, Vaughan-Williams E. Changes in asthma prevalence: two surveys 15 years apart. Arch Dis Child. 1989;64(10):1452–1456. doi:10.1136/adc.64.10.1452
15. Åberg N. Asthma and allergic rhinitis in Swedish conscripts. Clin Exp Allergy. 1989;19(1):59–63. doi:10.1111/j.1365-2222.1989.tb02345.x
16. Ciprandi G, Vizzaccaro A, Cirillo I, Crimi P, Canonica G. Increase of asthma and allergic rhinitis prevalence in young Italian men. Int Arch Allergy Immunol. 1996;111(3):279–283. doi:10.1159/000237378
17. World Health Organization. WHO | Asthma. World Health Organization; 2016. Available from: http://www.who.int/respiratory/asthma/en/.
18. Kolokotroni O, Middleton N, Nicolaou N, et al. Temporal changes in the prevalence of childhood asthma and allergies in urban and rural areas of Cyprus: results from two cross sectional studies. BMC Public Health. 2011;11:858. doi:10.1186/1471-2458-11-858
19. Middleton N, Kolokotroni O, Lamnisos D, Koutrakis P, Yiallouros PK. Prevalence of asthma and respiratory symptoms in 15–17 year-old Greek-Cypriots by proximity of their community of residence to power plants: Cyprus 2006–07. BMC Public Health. 2014;128(3):288–296. doi:10.1016/j.puhe.2013.11.004
20. Lamnisos D, Moustaki M, Kolokotroni O, et al. Prevalence of asthma and allergies in children from the Greek-Cypriot and Turkish-Cypriot communities in Cyprus: a bi-communal cross-sectional study. BMC Public Health. 2013;13:585. doi:10.1186/1471-2458-13-585
21. Nicolaou N, Yiallouros P, Pipis S, Ioannou P, Simpson A, Custovic A. Domestic allergen exposure and allergic sensitization in Cyprus. Pediatr Allergy Immunol. 2006;17:17–21. doi:10.1111/j.1399-3038.2005.00352.x
22. Zannetos S, Zachariadou T, Zachariades A, Georgiou A, Talias MA. The economic burden of adult asthma in Cyprus; a prevalence-based cost of illness study. BMC Public Health. 2017;17(1):262. doi:10.1186/s12889-017-4184-0
23. Janson C, Anto J, Burney P, et al. The European Community Respiratory Health Survey: what are the main results so far? Eur Respir J. 2001;18:598–611. doi:10.1183/09031936.01.00205801
24. Graham BL, Steenbruggen I, Miller MR, et al. Standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi:10.1164/rccm.201908-1590ST
25. Munthe-Kaas MC, Gerritsen J, Carlsen KH, et al. Eosinophil cationic protein (ECP) polymorphisms and association with asthma, s-ECP levels and related phenotypes. Allergy. 2007;62(4):429–436. doi:10.1111/j.1398-9995.2007.01327.x
26. Sin A, Terzioğlu E, Kokuludağ A, Sebik F, Kabakçi T. Serum eosinophil cationic protein (ECP) levels in patients with seasonal allergic rhinitis and allergic asthma. Allergy Asthma Proc. 1998;19(2):69–73. doi:10.2500/108854188778607228
27. Cyprus Government. European health survey. In: Cyprus Statistical Service. Nicosia: Cyprus Government; 2010.
28. Papadopoulou A, Hadziagorou E, Matziou VN, et al. Comparison in asthma and allergy prevalence in the two major cities in Greece: the ISAAC Phase II survey. Allergol Immunopathol. 2011;39(6):347–355. doi:10.1016/j.aller.2010.10.003
29. Selcuk ZT, Demir AU, Caglar T, Caglar T. Prevalence of asthma and allergic diseases in primary school children in Edirne, Turkey, two surveys 10 years apart. Pediatr Allergy Immunol. 2010;21(4 pt 2):e711–7. doi:10.1111/j.1399-3038.2010.01008.x
30. Pearce N, Ait-Khalid N, Beasley R, et al.; the ISAAC Phase Three Study Group. Worldwide Trends in the prevalence of asthma symptoms: Phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007;62:758–766. doi:10.1136/thx.2006.070169
31. Montefort S, Ellul P, Monterort M, Caruana S, Agius Muscat H. Increasing prevalence of asthma, allergic rhinitis but not eczema in 5–8 year old Maltese children (ISAAC). Pediatr Allergy Immunol. 2009;20:67–71. doi:10.1111/j.1399-3038.2008.00746.x
32. Ebell M, Marchello C, O’Connor J. The burden and social determinants of asthma for adults in the state of Georgia. J Public Health Assoc. 2017;6(4):426–434.
33. Greenblatt R, Mansour O, Zhao E, et al. Gender-specific determinants of asthma among U.S. adults. Asthma Res Pract. 2017;3:2. doi:10.1186/s40733-017-0030-5
34. Papageorgiou N, Gaga M, Marossis C, et al. Prevalence of asthma and asthma-like symptoms in Athens, Greece. Respir Med. 1997;91(2):83–88. doi:10.1016/S0954-6111(97)90072-X
35. Anthracopoulos MB, Liolios E, Panagiotakos DB, Triantou K, Priftis KN. Prevalence of asthma among schoolchildren in Patras, Greece: four questionnaire surveys during 1978–2003. Arch Dis Child. 2007;92:209–212. doi:10.1136/adc.2006.106153
36. Ones U, Akcay A, Tamay Z, Guter N, Zencir M. Rising trend of asthma prevalence among Turkish schoolchildren. Allergy. 2006;61:1448–1453. doi:10.1111/j.1398-9995.2006.01145.x
37. Demoly P, Annunziata K, Gubba E, et al. Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev. 2012;21(123):66–74. doi:10.1183/09059180.00008111
38. Rabe KF, Vermeire PA, Soriano JB, et al. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000;16(5):802–807. doi:10.1183/09031936.00.16580200
39. Partridge MR, van der Molen T, Myrseth S-E, et al. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006;6:13. doi:10.1186/1471-2466-6-13
40. Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol. 2007;120(6):1360–1367. doi:10.1016/j.jaci.2007.09.019
41. Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis. 2016;11:2509–2517. doi:10.2147/COPD.S114576
42. Moret L, Rochedreux A, Chevalier S, Lombrail P, Gasquet I. Medical information delivered to patients: discrepancies concerning roles as perceived by physicians and nurses set against patient satisfaction. Patient Educ Couns. 2008;70:94–101. doi:10.1016/j.pec.2007.09.011
43. Olson DP, Windish DM. Communication discrepancies between physicians and hospitalized patients. Arch Intern Med. 2010;170:1302–1307. doi:10.1001/archinternmed.2010.239
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


